Abstract
The aim of this clinical study was to evaluate the efficiency of in-office bleaching systems with different light sources for color change and possible side effects such as tooth sensitivity and gingival irritations. Forty healthy volunteers aged 18 years and older (average age 27.3 years), having all their natural healthy teeth in shade A3 or darker on the Vita shade guide, with no restorations on the buccal surfaces and no tooth sensitivity, participated in this study. Participants were randomly assigned to four groups of ten volunteers. Group 1 received bleaching without light activation (Opalescence Xtra Boost, Ultradent); group 2 received bleaching (Laser White 10, Biolase) with a diode laser (810 nm, 10 W/ Laser Smile, Biolase) activation; group 3 received bleaching treatment (Remewhite, Remedent) with a plasma arc lamp (400–490 nm, 2800 mV/cm2, Remecure CL15), and group 4 received bleaching with a light emitting diode (LED) lamp (By White accelerator, Ensodent) according to the manufacturers’ recommendations. The shade was assessed with a classical Vita shade guide (Vita Zahnfabrik) and a digital spectrophotometer (Vita Easy Shade, Vident). The color of teeth was scored at baseline and 1 week after bleaching. Any side effects on teeth or gingiva was recorded by visual analog scale. Results were analyzed statistically, by one-way analysis of variance (ANOVA), Kruskal–Wallis, and Mann–Whitney U tests with Bonferroni correction. All the bleaching techniques resulted in shade change. No significant differences were found in the color change among the four groups with shade guide assessment (P > 0.05), but spectrophotometer readings exhibited significant differences among the groups (P < 0.05). The overall shade change values expressed as ΔL, Δa, Δb, ΔE for group 2 was significantly higher than those for the other groups (P < 0.05). Group 2 also showed lower tooth and gingival sensitivity scores than those of the other groups (P < 0.05). All techniques resulted in shade change. Although the shade guide evaluation did not exhibit any differences among the bleaching treatment groups, spectrophotometer readings showed different findings. The results obtained by the two methods of evaluation of shade change used in this study were different from each other. Bleaching with diode laser resulted in less tooth and gingival sensitivity than the other bleaching systems. Clinical relevance: in-office bleaching systems used with or without light, lead to a shade change. As bleaching with diode laser resulted in less tooth and gingival sensitivity, it might be preferred among in-office bleaching systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bleaching is an effective method for restoring or lightening tooth color, and it can be accomplished by a variety of methods or systems, which can be generally categorized as in-office (professionally administered), at-home (professionally dispensed) or over-the- counter (self- administered).
Owing to an increased demand for whiter teeth in a short period of time, in-office bleaching is a popular option available to patients desiring a whiter and more attractive smile, and it can be performed by a dental professional the same day a patient walks into the dental office. This method of tooth whitening has been around for many years and remains popular, because results can be seen after the first appointment. The main advantages of an in-office whitening procedure over an at-home bleaching system include dentist control, avoidance of soft-tissue exposure and material ingestion, reduced total treatment time, and greater potential for immediate results that may enhance patient satisfaction and motivation [1].
Contemporary in-office bleaching systems are based primarily on hydrogen peroxide or one of its precursors, notably carbamide peroxide, and these materials are often used in combination with an activating agent such as heat or light. There are several different types of light activation sources, and among the newest light sources are lasers, light emitting diodes (LEDs), plasma arc lamps (PAC) and halogen lamps. The theoretical advantage of a light source is its ability to heat the hydrogen peroxide, thereby increasing the rate of decomposition of oxygen to form oxygen free radicals and enhancing the release of stain-containing molecules [2, 3].
There have been claims that some bleaching agents are more effective with light sources, while others are not [4, 5]. On the other hand, many articles have been published that show that light energy has no clinical effect on tooth whitening [6].
Evaluation of the efficacy and safety of tooth whitening systems has received considerable attention. Concern has been expressed about efficacy and safety limitations, including tooth sensitivity and soft-tissue irritation [7–11]. A few studies on the efficacy and safety of light used as an adjunctive tooth bleaching agent have been investigated in a controlled clinical trial [5].
As the observations regarding effectiveness and adverse effects are still controversial, the aim of this in vivo study was to evaluate the efficacy of three in-office bleaching systems with different light sources and one system without light activation and to investigate possible side effects such as tooth sensitivity and gingival irritation.
Methods and materials
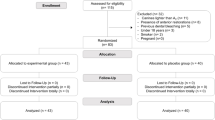
Forty patients (29 women and 11 men) with an average age of 27.3 years (range 18–30 years) and in good oral and general health participated in this study. The Ethics Committee of Hacettepe University, Ankara, Turkey, reviewed and approved the research protocol and informed consent form.
All subjects were 18 years old or older and had anterior tooth shade A3 or darker on the Vita shade guide (Vitapan Classic, VITA Zahnfabrik, Bad Sackingen, Germany) [12]. Inclusion criteria were the presence of all natural dentition, the absence of caries and restoration on the maxillary anterior teeth, no periodontal disease, no previous tooth whitening treatment, the absence of smoking habits, and compliance with procedures to avoid staining from food and beverages during the treatment period.
Study design
Participants submitted their written consent and completed medical history forms prior to the start of the study. All patients received a professional dental prophylaxis 2 weeks before the start of bleaching treatment and were asked to brush their teeth twice a day in order to standardize tooth cleaning during the study.
Before the bleaching application, all teeth were cleaned with pumice and a slow-speed rotary brush/prophy cup. Each bleaching agent was applied to both maxillary and mandibulary arches, according to the manufacturer’s recommendations. Characteristics of the office bleaching systems are given in Table 1. Participants were randomly assigned to four groups of ten volunteers:
In group 1, Opalescence Xtra Boost (Ultradent Dental GmbH, Cologne, Germany), containing 38% hydrogen peroxide, was used without a light source. To ensure protection of the gingiva, we applied a brush-on isolation material (Opaldam, Ultradent Products, South Jordan, Utah, USA), extending approximately 1.0 mm onto all tooth surfaces in the treatment area and cured with a standard curing light (Elipar Free Light, 3 M Espe, St Paul, MN, USA). The gel was provided with two syringes: one syringe contained the activator, while the other contained hydrogen peroxide. Before use, the activator was mixed with the bleaching agent, and the mixture was expressed directly onto the involved teeth in a 0.5–1.0 mm-thick layer. All the facial surfaces of the incisors, canines, and premolars were fully covered to ensure a uniform effect. After 15 min, the barrier was removed and the treated teeth were thoroughly rinsed with air–water spray. The procedure was repeated twice.
In group 2, LaserWhite 10 (37% hydrogen peroxide) was used in conjunction with a diode laser (LaserSmile, Biolase Technology Inc. San Clemente, CA, USA) with a spectral wavelength in the near infra-red region of 815 nm and an output of 10 W. After Vaseline had been applied to protect the lips and a cheek retractor had been inserted to isolate the treatment area, a suction device was connected to the retractors to help remove the excess saliva and water. Bite blocks were used as a jaw rest, and a liquid dam (White 10, Biolase) was applied along the gingival margin and cured with a standard curing light (Elipar Free Light, 3 M Espe). The upper and lower arches were then divided into four treatment sites consisting of as many as five teeth. A uniform layer of bleaching gel (1 mm thick) was applied to all four quadrants. The whitening headpiece of the laser device that was designed to treat one full quadrant at a time was placed in close proximity to the gel and activated for 15 s. The same procedure was applied to the other quadrants, and, after 1 min, the procedure was repeated for all four quadrants seven more times. Then the gel was removed with high-speed suction, the teeth were flushed with an air and water spray to remove any residual gel, and a second and third gel application with four laser activation procedures for each quadrant was completed. After all three sessions, the teeth were wiped with gauze and rinsed with water. At the completion of the treatment, the liquid dam was removed and the teeth were cleaned of gel. The operator, patient and the assistant wore laser-protective eyewear specific to the LaserSmile wavelength before starting, and during, the laser treatments.
In group 3, RemeWhite (35% hydrogen peroxide, Remedent Inc. Deurle, Belgium), designed to produce optimal results when used in combination with a plasma arc lamp (400–490 nm, 2,800 mV/ cm2, Remecure CL15, Remedent Inc.) was used without the need for any gingival protection, as this system provided a gel that did not require isolation of the gingival tissues. After a 1–2 mm-thick layer of whitening gel had been applied over the labial surfaces, with the gel kept 1 mm away from the gingiva, the Remecure full-arch tip was applied approximately 1 cm away from the patient’s mouth in whitening mode. For 10 min, the lamp lighted for 1 min and stopped for 30 s. After the 20-min session, the gel was removed and this procedure was repeated three times, so that the total bleaching time was 60 min.
In group 4, By White (38% hydrogen peroxide) was used in combination with an LED lamp (BioWhite accelerator, BioWhite, Ensodent, Italy). After a liquid dam had been applied along the gingival margins and cured with a standard curing light (Elipar Free Light, 3 M Espe), the gel was applied to the buccal surfaces of the teeth. The gel was removed after 20 min and the mouth was rinsed with abundant water. The procedure was repeated two times, so that the total bleaching time was 40 min.
Shade evaluation
Shade determination was always performed under the same conditions. For each subject, the shade was measured on the facial surfaces of the ten maxillary teeth (central and lateral incisors, cuspids and premolars) by one experienced and qualified examiner using a shade guide (Vita Classic shade guide, Vitapan Classic, VITA Zahnfabrik) and a spectrophotometer (Vita Easy Shade, Vident, Brea, CA, USA), at baseline and 1 week after each bleaching treatment. The examiner responsible for measuring color was required to leave the room during the treatment and to return for the post-treatment color measurements, so that she was unaware of the actual treatment administered.
The tabs of the shade guide were arranged from B1 (lightest color) to C4 (darkest color), corresponding to a grade of whitening from 1 to 16, in which a smaller number means the tooth was lighter.
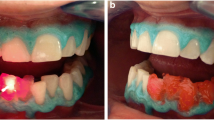
Three spectrophotometer measurements were made, with the active point of the instrument focused on the middle third of each tooth. A mean color from three measurements was calculated. The spectrophotometer measures the color of teeth based on the Commission Internationale de I’Eclairage’s CIELAB color space system. The image of the tooth is automatically transformed to derive a set of numerical values in terms of the L* a* b* system. The L* a* b* system allows color specification within a three dimensional space. The L* axis represents the degree of lightness within a tooth and ranges from 0 (black) to 100 (white). The a* plane represents the degree of green–red, while the b* plane represents the degree of blue–yellow in the teeth. ΔE is the total color difference or the distance between two colors. We computed ΔL, Δa, Δb, ΔE by subtracting the baseline measurements for the appropriate shade tabs from the follow-up measurements [12], and determined the color change by comparing each after bleaching to baseline. We took intraoral photographs (DSC-D770, Sony, Tokyo, Japan) to record the tooth shade for documentation of the baseline shade and to compare after treatment.
Evaluation of tooth and gingival sensitivity
To monitor tooth and gingival sensitivity, we asked the participants to mark a standardized 100 mm visual analog scale (VAS) ranging from 0 to 10. One end was labeled ‘no discomfort’ or ‘best acceptance’ (0), whereas the other end was labeled ‘severe discomfort’ or ‘no acceptance’ [10]. After each bleaching treatment, the patients were asked to mark the position that best indicated their current opinion. The marked point was measured in millimeters and documented accordingly. Differences, means and standard errors were calculated on the basis of this numeric assignment.
The data were evaluated by one-way analysis of variance (ANOVA), Kruskal–Wallis test, and Mann Whitney U test with Bonferroni correction.
Results
All 40 participants completed the study. The results of shade changes are shown in Tables 2 and 3. The results obtained by the two evaluation methods (the shade guide and the spectrophotometer evaluation) used in this study were different. The shades of the four groups did not differ significantly at baseline. Their values ranged from grades 9–16. There were no significant differences among the groups for shade guide rank scores (P = 0.997) (one-way ANOVA). All techniques proved to be effective at whitening, with a mean value of 8.70 ± 3.19 in group 1, 8.60 ± 3.59 in group 2, 8.40 ± 2.98 in group 3 and 8.50 ± 2.32 in group 4. The differences between baseline and after bleaching were statistically significant for the four groups (P < 0.05). On the other hand, spectrophotometer readings exhibited significant differences among the groups (P < 0.05). The ΔL value for group 2 was significantly higher than that for the other groups (P < 0.05). The differences among all the groups for Δa values were statistically different (P < 0.05). Group 2 exhibited the highest Δa values, whereas group 4 showed the lowest. The Δb values of groups 2 and 4 were significantly higher than those of groups 1 and 3. The ΔE values of group 2 were statistically higher than those of all the other groups (P < 0.05).
Table 4 shows the mean sensitivity scores, as measured from the 100 mm VAS scale from baseline to after bleaching. Mean tooth sensitivity values were 3.37 ± 1.94 for group 1, 0.59 ± 0.92 for group 2, 3.80 ± 1.29 for group 3, and 2.90 ± 1.4 for group 4, and the average was 2.66 ± 1.88. Mean gingival sensitivity values were 1.11 ± 0.845 for group 1, 0.1 ± 0.316 for group 2, 1.07 ± 1.14 for group 3, and 1.11 ± 0.912 for group 4, and the average was 0.82 ± 0.94. Group 2 showed significantly lower tooth and gingival sensitivity scores than did the other groups (P < 0.001) (Kruskal–Wallis test). No significant differences were observed among group 1, group 3 or group 4 in their tooth and gingival sensitivities (P > 0.05) (Mann–Whitney U test with Bonferroni correction).
Discussion
The auxiliary lights recommended by some manufacturers to be used in the in office bleaching treatment were believed to be capable of catalyzing hydrogen peroxide decomposition and therefore were used to accelerate the action of the bleach [13]. This study described the comparison of three different bleaching systems used clinically with different light and bleaching protocols and one system used without light. The four systems differed in many aspects, such as treatment method, treatment duration, application devices, and ingredients. The protocol for applying the light sources was based on the manufacturers’ directions for the three hydrogen peroxide bleaches that prescribed the use of light.
Tooth shade, which is the result of diffuse reflectance from the dentin through the translucent enamel layer, is believed to be one of the most important factors in patients’ perception of dental attractiveness [13]. A number of methods are available for evaluating the efficacy of bleaching. Shade guides, photography, colorimeter spectrophotometer or computer digitization can be used to assess tooth color changes. One of the most common methods is the simultaneous comparison of the tooth with standard shade guides [14–16]. The value-oriented shade guide gives clinically relevant results, because successful bleaching calls for a perceivable difference in tooth color. However, the selection of the matching shade tab is subjective, not predictably reproducible, and is influenced by such factors as lighting and eye fatigue. The use of a spectrophotometer also has its advantages and drawbacks; it gives more objective results than shade tabs, but it is affected by tooth translucency, tooth contour, tooth texture and difficulties in repeatable tooth repositioning [4].
In this study the shade guide and a spectrophotometer were used together to measure whitening efficacy. Photographs were also taken with a digital camera with matching shade tabs before and after bleaching to document the tooth color under standardized lighting conditions and away from strong light absorbers such as dark-colored walls. To evaluate the degree of color change an experienced and trained examiner recorded the shades.
It is difficult to compare the results of this study with data from the literature, as there are no published studies available where these four systems were compared with another. In our study all techniques with or without the use of additional light sources resulted in significant tooth lightening, and, although the group without light activation had the highest mean value of shade change, 8.70 ± 3.19, with shade guide evaluation, the difference was not significantly different. The magnitude of the shade change in the study was similar to those in previous clinical studies. Deliperi et al. [17] reported a mean change of 8.5 units after bleaching with 38% hydrogen peroxide, and Papathanasiou et al. [18] reported similar findings with 35% hydrogen peroxide activated by a halogen curing light. In contrast to these findings, Auschill et al. [19] reported higher values (11.4) with chemically activated 38% hydrogen peroxide (Opalescence Xtra Boost). Spectrophotometer readings were also in line with those in previous reports [20]. Shade changes evaluated with the spectrophotometer showed that there was a significant difference in the overall color (ΔE), with the group bleached with the diode laser as a light source showing the greatest change, whereas shade guide evaluations revealed no differences among the groups. There were differences in the results when the two methods of shade evaluation were compared, which corresponded with findings in other studies [20].
Two of the key factors in determining overall tooth whitening efficacy from peroxide-containing products are the concentration of the peroxide and the duration of application. The bleaching agents tested in this study contained hydrogen peroxide in higher concentrations (35–38%), but they all had different durations of application.
A small number of clinical studies has demonstrated the efficacy of light-activated peroxide tooth bleaching systems [21–26]. Tavares et al. [5] conducted a clinical study to compare 15% hydrogen peroxide gel illuminated with a gas plasma light source, 15% hydrogen peroxide alone, and placebo gel plus light, all treatments lasting 1 h. The change in Vita shade from baseline for peroxide plus light, peroxide alone, and placebo plus light, were 8.35, 5.88 and 4.93, respectively, with peroxide plus light being significantly different from the other two groups.
Hein et al. [6] demonstrated that there was no additional effect of any of the three bleaching lights (LumaArch, Optilux 500, and Zoom) tested over the bleaching gel alone for three commercial products, in a split-mouth clinical design.
Generally, bleaching is accompanied by some sort of increased tooth or gingival sensitivity [19]. Researchers and clinicians may be reluctant to adopt bleaching therapies because of the tooth sensitivity issue, which has been reported to be a common side effect when hydrogen peroxide is used. It was shown that the higher the concentration of a bleaching agent, the higher the risk of tooth sensitivity [20].
In this study some of the participants reported no tooth sensitivity and some experienced very little gingival sensitivity during the bleaching treatment. This may have been the result of the close professional control in application and protection of surrounding tissues, which were also an integral part of the procedure, and to the improved formulation of the bleaching agent. A significant difference was observed in tooth sensitivity between the group treated with the use of diode laser and the other groups. It has been reported that irradiation with infrared laser light can produce some beneficial effects on sensitivity [27]. The laser has been proven to be the most valuable energy source for in-office bleaching, with simple and short application in the office [27–30]. Many patients are interested in saving time, obtaining quicker results, and avoiding responsibility for the treatment, so they opt for in-office treatments if available, to expedite the whitening effect. For this situation, bleaching with laser irradiation is more advisable. The laser system used in the study demonstrated a shorter exposure time, with a total treatment time of 8–24 min including the 2–4 min of laser exposure, than of the other groups.
Tooth lightening associated with bleach exposure, as opposed to light exposure or temporary tooth dehydration, comes from a decrease in the level of tooth colorization rather than an increase in tooth brightness. Tooth dehydration is a probable cause of immediate tooth lightening, and, presumably, it is greater with increased tooth heating [1]. The observed immediate tooth lightening that is attributable to tooth dehydration appeared to be more an increase in tooth brightness than a decrease in the level of tooth colorization. For this reason the color assessments in this study were all done 1 week following the bleaching treatments.
Conclusion
-
1.
In-office bleaching systems used in this study, with or without light, were effective for the whitening of teeth.
-
2.
The results obtained by the two methods of evaluation of shade change (visual evaluation with the Classic Vita shade guide and spectrophotometric evaluation) used in this study were different.
-
3.
As bleaching with the use of diode laser resulted in less time with less tooth and gingival sensitivity, it might be preferred among in-office bleaching systems.
References
Joiner A (2006) The bleaching of teeth: a review of the literature. J Dent 34:412–419
Sulieman M, MacDonald E, Rees JS, Addy M (2005) Comparison of three in office bleaching systems based on 35% hydrogen peroxide with different light activators. Am J Dent 18:194–197
Joiner A (2004) Tooth colour: a review of the literature. J Dent 32 (Suppl. 1):3–12
Luk K, Tam L, Hubert M (2004) Effect of light energy on peroxide tooth bleaching. J Am Dent Assoc 135:194–201
Tavares M, Stultz J, Newman M, Smith V, Kent R, Carpino E, Goodson JM (2003) Light augments tooth whitening with peroxide. J Am Dent Assoc 134:167–175
Hein DK, Ploeger BJ, Hartup JK, Wagstaff RS, Palmer TM, Hansen LD (2003) In-office vital tooth bleaching—what do they add? Compend Contin Educ Dent 24:340–352
Ziebolz D, Helms K, Hannig C, Attin T (2007) Efficacy and oral side effects of two highly concentrated tray-based bleaching systems. Clin Oral Investig 11:267–275
Leonard RH, Smith LR, Garland GE, Tiwana KK, Zaidel LA, Pugh G, Lin NC (2007) Evaluation of side effects and patients perceptions during tooth bleaching. J Esthet Restor Dent 19:355–364
Sulieman M (2004) An overview of bleaching techniques: history, chemistry, safety and legal aspects. Dent Update 31:608–616
Mokhlis GR, Matis BA, Cochran MA, Eckert GJ (2000) A clinical evaluation of carbamide peroxide and hydrogen peroxide whitening agents during daytime use. J Am Dent Assoc 131:1269–1277
Clinical Research Associates (2000) Vital tooth bleaching, in-office. CRA Newsletter 24:1–3
Commission Internationale de I’Eclairage (1978) Recommendations on uniform color spaces, color difference equations, psychometric color terms. Bureau Central de la CIE, Paris
Zhang C, Wang X, Kinoshita J-I, Zhao B, Toko T, Kimura Y, Matsumoto K (2007) Effects of KTP laser irradiation, diode laser and LED on tooth bleaching: a comparative study. Photomed Laser Surg 25:91–95
Mohan N, Westland S, Brunton P, Ellwood R, Pretty IA, Luo W (2008) A clinical study to evaluate the efficacy of a novel tray based tooth whitening system. J Dent 36:21–26
van der Burgt TO, ten Bosch JJ, Borsboom PCF, Kortsmit PM (1990) A comparison of new and conventional methods for quantification of tooth color. J Prosthet Dent 63:155–162
Rosenstiel S, Gegauff A, Johnston W (1991) Duration of tooth color change after bleaching. J Am Dent Assoc 122:54–9
Deliperi S, Bardwell DN, Papathanasiou A (2004) Clinical evaluation of a combined in-office and take home bleaching system. J Am Dent Assoc 135:628–634
Papathanasiou A, Kastali S, Perry RD, Kugel G (2002) Clinical evaluation of a 35% hydrogen peroxide in-office whitening system. Compend Contin Educ Dent 23:335–338
Auschill TM, Hellwig E, Schmidale S, Sculean A, Arweiler NB (2005) Efficacy, side-effects and patients’ acceptance of different bleaching techniques (OTC, in-office, at-home). Oper Dent 30:156–163
Marson FC, Sensi LG, Vieira LCC, Araujo E (2008) Clinical evaluation of in-office dental bleaching treatments with and without the use of light-activation sources. Oper Dent 33:15–22
Smigel I (1996) Laser tooth whitening. Dent Today 32–36.
Reyto R (1998) Laser tooth whitening. Dent Clin North Am 42:755–762
Lu AC, Margiotta A, Nathoo SA (2001) In-office tooth whitening: current procedures. Compend Contin Educ Dent 22:798–805
Hanosh N, Hanosh GS (1992) Vital bleaching: a new light-activated hydrogen peroxide system. J Esthet Dent 4:90–95
Nakamura T, Saito O, Ko T, Maruyama T (2001) The effects of polishing and bleaching on the colour of discoloured teeth in vivo. J Oral Rehabil 28:1080–1084
Nash W (1999) In-office bleaching system for quick esthetic change. Compend Contin Educ Dent 20:986–990
Wetter NU, Barroso MCS, Pelino JEP (2004) Dental bleaching efficacy with diode laser and LED irradiation: an in vitro study. Lasers Surg Med 35:254–258
Dostalova T, Jelinkova H, Housova D, Sulch J, Nemec M, Miyagi M, Brugnera A, Zanin F (2004) Diode laser-activated bleaching. Braz Dent J 15:SI-3–SI-8
Cesar ICR, Redigolo ML, Lıporoni PCP, Munin E (2005) Analyses by photoreflectance spectroscopy and Vickers hardness of conventional and laser-assisted tooth bleaching. Am J Dent 18:219–222
Jones A, Diaz-Arnold A, Vargas M, Cobb D (1999) Colorimetric assessment of laser and home bleaching techniques. J Esthet Dent 11:87–94
Acknowledgement
This research was supported by Hacettepe University Research Center (HüBAB Project No: 07 A 201001).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gurgan, S., Cakir, F.Y. & Yazici, E. Different light-activated in-office bleaching systems: a clinical evaluation. Lasers Med Sci 25, 817–822 (2010). https://doi.org/10.1007/s10103-009-0688-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-009-0688-x