Abstract
Chronic obstructive pulmonary disease (COPD) is an independent risk factor for osteoporosis. Oral glucocorticoids are deleterious to bone; however, the impact of inhaled glucocorticoids (ICS) remains unclear. Our objective was to determine whether ICS contribute to osteoporosis and fragility fractures. Sixty-one COPD patients, 35 current users of ICS and 26 who had never received glucocorticoids, were evaluated for bone mineral density (BMD) and body composition and underwent vertebral fracture assessment (VFA). The risk factors for bone disease considered for analysis were age, gender, ICS use, body mass index (BMI), muscle mass index (MMI), and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) category. The Fracture Risk Assessment Tool (FRAX) calculation tool for the Brazilian population was also employed. The groups did not differ regarding gender, BMI, MMI, GOLD class, lowest values of the BMD T-score and Z-score, prevalence of osteoporosis, or low BMD for age. Vertebral fractures were identified via VFA in seven patients using ICS and in none of those not receiving glucocorticoids (p = 0.02). There was a trend for an association between MMI and osteoporosis (p = 0.05) and for a progressive decrease in the BMD Z-score according to the COPD severity assessed via the GOLD score (p = 0.08). Vertebral fractures were not associated with osteoporosis (p = 0.69) or low MMI (p = 0.12). The fracture risk was not estimated by FRAX. ICS may lead to bone fragility before a significant decrease in BMD. Low muscle mass and COPD severity may contribute to bone disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality worldwide, and the burden of the disorder will continue to increase during the next 20 years. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) has defined COPD as a preventable and treatable disease that is primarily characterized by a progressive airflow limitation. This airflow limitation is not fully reversible and is associated with an abnormal inflammatory response of the lungs to noxious particles or gases, most often cigarette smoke [1]. COPD is often associated with comorbidities and systemic consequences that increase mortality, including osteoporosis.
Osteoporosis is a skeletal systemic disease characterized by low bone mass and micro-architectural changes in bone tissue that lead to increased bone fragility and thereby an increased fracture risk. The prevalence of osteoporosis in COPD patients varies from 4% to 59%, depending on the diagnostic methods used, the population studied, and the severity of the underlying respiratory disease [2,3,4]. The etiology of osteoporosis in COPD is very complex: the risk factors include age, gender, ethnicity, malnutrition, low body mass index (BMI), decreased free-fat mass/sarcopenia, lung disease severity, hypercapnia, progressive physical disability, physical inactivity, systemic inflammation, vitamin D deficiency, tobacco exposure, hypogonadism, use of glucocorticoids (GC), or a combination of these factors. COPD is an independent predictor of bone mineral density (BMD) reduction and an increased risk of fractures [5,6,7,8,9,10].
COPD patients frequently receive prescriptions for GCs, oral or inhaled, to control their disease. Oral GCs are associated with low bone density and osteoporosis [11, 12], but the effects of inhaled glucocorticoids (ICS) on bone remain controversial [13,14,15].
The occurrence of fractures as a consequence of osteoporosis may contribute to the disability and mortality of COPD patients. Thoracic vertebral fractures are a major concern because these fractures not only cause back pain but also decrease pulmonary performance by reducing lung volume, with consequent overlap of a restrictive ventilatory defect [16,17,18]. Thus, the early prevention of osteoporotic fractures in COPD patients is very important.
In postmenopausal women and elderly men, bone densitometry is not an ideal predictor because these patients may exhibit fragility fractures with minimal decreases in BMD [19, 20]. This issue is also true for patients who receive GCs and develop fragility fractures before significant decreases in BMD [21]. More recently, bone fragility has also been estimated by an integrated risk assessment tool, FRAX (Fracture Risk Assessment Tool) [22].
In the present study, we aimed to estimate the prevalence of osteoporosis and fractures in COPD patients who were not receiving pharmacological treatment and patients receiving ICS. We also evaluated the association of these findings with age, gender, low BMI, low muscle mass index (MMI), COPD severity assessed via the GOLD score, and FRAX.
Materials and methods
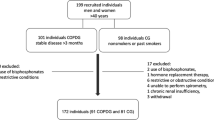
Study population
We recruited outpatients from the ambulatory of Pneumology from two institutions: University Hospital Clementino Fraga Filho and Newton Bethlem Medical Assistance Center, which are both located in Rio de Janeiro. Patients of both genders, 50 years and older, were selected from January 2014 to June 2015. The diagnosis of COPD was confirmed via spirometry, which indicated a forced expiratory volume in 1 s (FEV1)/forced capacity vital ratio less than 70% [1]. The patients were classified as stage I–IV in accordance with the GOLD criteria [1]. The selected patients had received either ICS for at least 3 months or no pharmacological treatment. The exclusion criteria were as follows: patients who received systemic GC for any cause during the preceding year, premenopausal women, individuals who exhibited alcohol abuse (>400 g/week), users of illicit drugs and other medications known to influence bone density and quality (such as anticonvulsants and antiosteoporosis drugs), as well as chronic diseases, such as diabetes mellitus and cancer, that may interfere with the parameters evaluated.
Methods
The protocol was approved by the ethical committee of UNISUAM under number 868,800, and informed consent was obtained from all individual participants included in the study. Each patient was interviewed by a physician using a structured questionnaire that addressed the history of previous fragility fractures, parental history of hip fracture, smoking, all drugs used for the treatment of COPD, including the type and dosage of ICS, when the medication was initiated or discontinued, the natural history of COPD, and concomitant health conditions. A physical examination was performed the same day. Height was measured by stadiometer and weight was measured by a balance-beam scale to calculate the body mass index (BMI) = weight/height2.
The International Physical Activity Questionnaire (IPAQ) Short Form was used to assess physical activity. This instrument estimates the time spent performing several levels of physical activity during the previous week. Energy expenditure is calculated by determining the number of minutes per week spent in each activity and estimated as a metabolic equivalent of task (MET). The IPAQ Short Form is composed of four domains, and each domain is divided into two items. The results of all items are summed to provide a total physical activity score [23].
Bone mineral density (BMD) was measured at the lumbar spine (LS), femoral neck (FN), and total femur (TF) by dual-energy X-ray absorptiometry (DEXA, DXA) (Prodigy Advance; GE Healthcare, Madison, WI, USA). According to the (Inorganic Crystal Structure Database (ISCD) criteria [24], all postmenopausal women and men 50 years and older were identified as having a low bone density (previously referred to as osteopenia) or osteoporosis when the lowest BMD T-score was between <−1 and >−2.5 SD or ≤−2.5 SD, respectively. Values of the BMD Z-score ≤−2 SD at any site were also considered a lower than expected BMD for age. The variability coefficients of the BMD values were estimated at 1.5% at the lumbar spine and 2.3% at the femur.
Body composition and vertebral fracture assessment (VFA) were also performed using the same device. The fat mass and fat-free mass (lean mass) were evaluated at the total body. The MMI was calculated as the sum of lean mass in the arms and legs/height2, and it was considered low if <5.67 kg/m2 in women and <7.25 kg/m2 in men [25].
A fan-bean DXA system with appropriate software installed is required to perform VFA. We used a dual-energy mode, with the patient in a lateral decubitus position and a C-arm that does not rotate. The same experienced physician manually placed six point markers at the anterior, middle, and posterior margins of the vertebral endplates to measure the body heights (anterior, middle, and posterior) and ratios (anterior/posterior and middle/posterior). Using Genant semi-quantitative methodology [26], vertebral fractures (VFs) were classified as moderate or grade 2 (25–40% loss of vertebral height) and severe or grade 3 (more than 40% loss of vertebral height). We did not consider mild or grade 1 (20–25% loss of vertebral height). The measurements were conducted at the same time as the BMD assessment, and the vertebrae from T7 to L4 were analyzed.
The FRAX calculation tool for the Brazilian population was used to assess the fracture risk for major osteoporotic fractures and hip fractures.
Data analysis
The statistical analysis was performed using SPSS version 20.0 for MacOS (SPSS, Chicago, IL, USA). Most variables, with the exception of FRAX (hip fractures) and FRAX (major osteoporotic fractures), followed a normal distribution using the Kolmogorov–Smirnov test. For the descriptive analysis, categorical variables were expressed as percentages and frequencies, and numerical variables were expressed as mean ± SD or medians (minimum–maximum) according to their distribution pattern. Student’s t tests or Mann–Whitney U tests were performed to compare the numerical variables between the two groups according to their distributions. Analysis of variance (ANOVA) or Kruskal–Wallis tests were applied to compare the numerical variables among the three groups according to their distributions, followed by Tukey and Bonferroni post hoc analyses, respectively. A p value <0.05 was considered statistically significant.
Results
Sixty-one COPD outpatients were included. The participants were followed in two institutions that used the same criteria for treatment with ICS, which was established by GOLD guidelines. These guidelines recommend ICS for all patients with severe and very severe airflow limitations, patients with frequent exacerbations, and patients who are not adequately controlled by long-acting bronchodilators. According to the IPAQ Short Form, all patients were considered to be sedentary or irregularly active. The characteristics of the total population are shown in Table 1.
Thirty-five patients were current users of ICS, and 26 patients did not use GCs. Age ranged from 52 to 84 years, with no significant difference between men (65.0 ± 6.42 years) and women (65.25 ± 5.42 years). Nine men and 3 women were current smokers, and 36 men and 13 women were former smokers. Five patients (8.2%) were underweight (BMI <20 kg/m2), 34 patients (55.73%) had a normal BMI (20–27), and 22 patients (36.06%) were overweight/obese, with no gender difference. No patient reported a previous low-impact fracture.
The patients on ICS had used this medication for at least 3 months before the study. The most commonly used ICS was Budesonide 400 µg twice daily. Among men, 19 patients were using the combination Formoterol plus Budesonide 12/400 µg twice daily, 5 patients were using Beclomethasone 50–250 µg twice daily, and only 1 patient was using Formoterol plus Beclomethasone 250 µg twice daily. In the female group (n = 10), 8 patients were using the combination Formoterol plus Budesonide 12/400 µg twice daily, 1 patient was using Salmeterol plus Fluticasone 50/250 µg twice per day, and 1 patient was using Beclomethasone 200 µg twice daily.
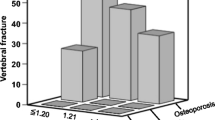
Comparisons between the patients using ICS and the patients not using GCs are shown in Table 2 (supplemental data). Only four patients were classified at GOLD IV; thus, the patient stages III and IV were considered together for statistical analysis. The distribution according to COPD severity was not different between the groups. Although the GC users were older, they did not differ regarding gender distribution, BMI, MMI, or lowest values of the BMD T-score and BMD Z-score. However, vertebral fractures were only identified in the patients using GC (p = 0.02).
Considering the type of ICS, 27 patients were on Budesonide 800 µg/day (5 patients had fractures); 7 patients were on Beclomethasone 50–500 µg/day (1 patient with a fracture was receiving 100 µg/day); and 1 patient on Fluticasone 500 µg/day had a fracture.
According to DXA scans, 22 patients (16 men and 6 women) were diagnosed with osteoporosis, which corresponded to 3 of 7 patients (42.85%) with vertebral fractures (6 men and 1 woman) and 19 patients (35.18%) without fractures. There was no association between osteoporosis by DXA and gender (p = 0.89) or age (p = 0.76).
Low MMI values were identified in 26 patients (13 patients with osteoporosis via DXA). However, only 9 of 35 patients with a normal MMI exhibited osteoporosis. The association between MMI and osteoporosis almost reached significance (p = 0.051).
No significant difference was identified between the patients with and without vertebral fractures detected by VFA, even considering the FRAX values, as shown in Table 3. Fractures were not associated with osteoporosis via DXA (p = 0.69) or a low MMI (p = 0.12).
There was a trend toward progressive decrease in the lowest BMD Z-score according to COPD severity assessed by the GOLD score (p = 0.08). All other comparisons were not significantly different, including the number of patients with vertebral fractures detected by VFA in each category (Table 4).
Discussion
Our data strongly suggest that ICSs are related to vertebral fractures in COPD patients before alterations in bone densitometry. Decreased muscle mass and lung disease severity may contribute to bone disease in these patients.
Oral GCs increase the risk of vertebral fractures by twofold and osteoporosis by ninefold [27, 28]. However, the role of ICS therapy in the genesis of bone thinning is controversial. Patients with COPD frequently receive ICS for several years; however, long-term, prospective studies of conventional high-dose ICS therapy are lacking, with reports only of up to 3 years duration [28,29,30,31]. A Cochrane database review indicated there was no evidence of an effect of ICS on BMD or vertebral fracture in patients with mild COPD or asthma, when used at a conventional dose for 2 or 3 years [29]. According to Iqbal et al. [27] and McEvoy et al. [28], the effect of ICS in COPD on vertebral fractures was small; however, the severity of loss of BMD was similar between ICS and OCS therapies. In patients administered a standard dose of budesonide (800 µg/day), there was no accelerated bone loss compared with placebo treatment in the EUROSCOPS study [32]. In a large, case-controlled study, which included more than 100,000 cases from the United Kingdom General Practice Research Database, De Vries et al. [33] determined that the association between ICS at daily doses equivalent to greater than 1600 µg Beclomethasone and the increased fracture risk disappeared after adjustment for disease severity; these findings suggest that in COPD, disease severity rather than ICS increases the fracture risk. More recently, Watanabe et al. [10] demonstrated association between vertebral fractures and deterioration of pulmonary function. In a 4-year study with 251 men with COPD, Mathioudakis et al. [34] reported that low-dose ICS did not aggravate bone loss; furthermore, it decelerated the osteoporosis in bronchitic patients. Elmståhl et al. [35] also reported no difference in BMD between postmenopausal women exposed to ICS and unexposed controls; moreover, there was no dose–response relationship between ICS therapy and BMD.
The majority of our patients had mild or moderate lung disease, and no patients had previously received oral GC; however, approximately one third of the patients had osteoporosis via bone densitometry, and 11% of the patients had nonclinical vertebral fractures via VFA. In accordance with the previously described studies, we also determined there was no difference between GC users and non-users regarding the absolute BMD values, the prevalence of low bone mass for age, and osteoporosis evaluated by DXA. We did not evaluate physical activity, inflammation markers, vitamin D, or sex-steroid serum levels; however, there was no association with age, gender, or BMI. The differences among the three groups of GOLD scores were not statistically significant; however, there was a trend toward progressive decrease in the BMD Z-score with the severity of lung disease. Furthermore, there was an association between low muscle mass and osteoporosis. Thus, both MMI and GOLD score appeared to contribute to bone disease.
Importantly, although no patient reported a previous low-impact fracture, VFA identified nonclinical vertebral fractures in seven patients, all of whom had received ICS; i.e., 20% of the patients on ICS had fragility fractures. In a systematic review and meta-analysis of 16 randomized controlled trials, Loke et al. indicated that ICS were associated with a 27% increase in fracture risk [36].
The BMD T-score and BMD Z-score values and osteoporosis via DXA did not discriminate the patients with vertebral fractures confirmed by VFA.
BMD assessment, although specific, may not be sensitive for predicting fracture risk. The addition of clinical risk factors that are able to predict fractures independent of BMD may improve our ability to predict fracture risk.
FRAX is a web-based algorithm designed to calculate the 10-year probability of major osteoporosis-related fractures (clinical vertebral, hip, forearm, or humerus) and hip fractures in men and women based on easily obtained clinical risk factors (and the femoral neck BMD, if available). The average dose of GC considered a risk factor is prednisolone 5 mg/day or higher or equivalent doses of other GC [22]. Patients on ICS are not considered GC users in the FRAX model, and we adopted this criterion in the present study. There was no difference in the FRAX values between patients with and without fractures, which suggests that FRAX may underestimate the fracture probability in ICS users.
This study has several limitations. First, the study sample was relatively small, considering the prevalence of COPD. Second, a double-blind, controlled trial may be more useful to detect the real impact of ICS on BMD; however, we believe that our results have similar reliability because our patient groups did not differ in nearly all variables. Third, we did not measure inflammatory factors in the circulation; thus, a longitudinal study may identify a positive relationship between ICS and the systemic inflammation caused by COPD, as well as facilitate an understanding of the association between systemic inflammation and the extra-pulmonary manifestations of COPD.
In conclusion, the present study demonstrated that ICS is associated with bone fragility in COPD patients. Low muscle mass and COPD severity may contribute to bone disease. DXA scan and FRAX were not predictive of fragility fractures.
References
Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C et al (2013) Global strategy for the diagnosis management and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 187:347–365
Law MR, Hackshaw AK (1997) A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: recognition of major effect. BMJ 315:841–846
Gan WQ, Man SF, Senthilselvan A, Sin DD (2004) Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax 59:574–580
Bolton CE, Ionescu AA, Shields KM, Pettit RJ, Edwards PH (2004) Associated loss of fat-free mass and bone mineral density in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 170:1286–1293
Jorgensen NR, Schwarz P, Holme L, Henriksen BM, Petersen LJ, Backer V (2007) The prevalence of osteoporosis in patients with chronic obstructive pulmonary disease: a cross-sectional study. Respir Med 101:177–185
Graat-Verboom L, Wouters EF, Smeenk FW, van den Borne BE, Lunde R, Spruit MA (2009) Current status of research on osteoporosis in COPD: a systematic review. Eur Respir J 34:209–218
Maggi S, Siviero P, Gonnelli S, Schiraldi C, Malavolta N et al (2009) Osteoporosis risk in patients with chronic obstructive pulmonary disease: the EOLO Study. J Clin Densitom 12:345–352
Majumdar SR, Villa Roel C, Lyons KJ, Rowe BH (2010) Prevalence and predictors of vertebral fracture in patients with chronic obstructive pulmonary disease. Respir Med 104:260–266
Gonnelli S, Caffarelli C, Maggi S, Guglielmi G, Siviero P et al (2010) Effect of inhaled glucocorticoids and beta2 agonists on vertebral fracture risk in COPD patients: the EOLO study. Calcif Tissue Int 87:137–143
Watanabe R, Tanaka T, Aita K, Hagiya M, Homma T (2015) Osteoporosis is highly prevalent in Japanese males with chronic obstructive pulmonary disease and is associated with deteriorated pulmonary function. J Bone Miner Metab 33:392–400
Dubois EF, Roder E, Dekhuijzen R, Zwinderman AE, Schweitzer DH (2002) Dual X-ray absorptiometry outcomes in male COPD patients after treatment with different glucocorticoid regimens. Chest 121:1456–1463
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. National Osteoporosis Foundation. Osteoporos Int 25:2359–2381
Johnell O, Pauwels R, Löfdahl CG, Laitinen LA, Postma DS et al (2002) Bone mineral density in patients with chronic obstructive pulmonary disease treated with budesonide Turbuhaler. Eur Respir J 19:1058–1063
Richy F, Bousquet J, Ehrlich GE, Meunier PJ, Israel E et al (2003) Inhaled corticosteroids effects on bone in asthmatic and COPD patients: a quantitative systematic review. Osteoporos Int 14:179–190
Wilkie M, Finch S, Schembri S (2015) Inhaled corticosteroids for chronic obstructive pulmonary disease: the shifting treatment paradigm. COPD 12:582–590
Papaioannou A, Parkinson W, Ferko N, Probyn L, Ioannidis G et al (2003) Prevalence of vertebral fractures among patients with chronic obstructive pulmonary disease in Canada. Osteoporos Int 14:913–917
Schlaich C, Minne HW, Bruckner T, Wagner G, Gebest HJ et al (1998) Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos Int 8:261–267
Carter JD, Patel S, Sultan FL, Thompson ZJ, Margaux H et al (2008) The recognition and treatment of vertebral fractures in males with chronic obstructive pulmonary disease. Respir Med 102:1165–1172
Siris ES, Miller PD, Barrett-Connor E, Faulkner KG, Wehren LE et al (2001) Identification and fracture outcomes of undiagnosed low mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA 286:2815–2822
Schuit SC, van der Klift M, Weel AE, de Laet CE, Burger H et al (2004) Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone (NY) 34:195–202
Canalis E, Mazziotti G, Giustina A, Bilezikian JP (2007) Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos Int 18:1319–1328
Kanis JA, Johnell O, Oden A, Dawson A, De Laet C, Jonsson B (2001) Ten-year probabilities of osteoporotic fractures according to BMD and diagnostic thresholds. Osteoporos Int 12:989–995
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML et al (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35:1381–1395
Lewiecki EM, Watts NB, McClung MR, Petak SM, Bachrach LK et al (2004) Official positions of the International Society for clinical densitometry. J Clin Endocrinol Metab 89:3651–3655
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T et al (2010) Sarcopenia: European consensus on definition and diagnosis. Age Ageing 39:412–423
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS et al (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fracture in osteoporosis. J Bone Miner Res 11:984–996
Iqbal F, Michaelson J, Thaler L, Rubin J, Roman J, Nanes MS (1999) Declining bone mass in men with chronic obstructive pulmonary disease: contribution of glucocorticoids treatment, body mass index, and gonadal function. Chest 116:1616–1624
McEvoy CE, Ensrud KE, Bender E, Genant HK, Yu W et al (1998) Association between corticosteroid use and vertebral fractures in older men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 157:704–709
Jones A, Fay JK, Burr M, Stone M, Hood K, Roberts G (2002) Inhaled corticosteroid effects on bone metabolism in asthma and mild chronic obstructive pulmonary disease. Cochrane Database Syst Rev. doi:10.1002/14651858.CD003537
Graat-Verboom L, Smeenk FW, van den Borne BE, Spruit MA, Jansen FH et al (2012) Progression of osteoporosis in patients with COPD: a 3-year follow-up study. Respir Med 106:861–870
Fergusson GT, Calverley MA, Anderson JA, Jenkins CR, Jones PW et al (2009) Prevalence and progression of osteoporosis in patients with COPD: results from the Towards a Revolution in COPD Health Study. Chest 136:1457–1465
Pauwels RA, Lofdahl GC, Laitinen LA, Schouten JP, Postma DS et al (1999) Long term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. European Respiratory Society Study on Chronic Obstructive Pulmonary Disease. N Engl J Med 340:1948–1953
De Vries F, van Staa TP, Bracke MS, Cooper C, Leufkens HG, Lammers JW (2005) Severity of obstructive airway disease and risk of osteoporotic fracture. Eur Respir J 25:879–884
Mathioudakis AG, Amanetopoulou SG, Gialmanidis IP, Chatzimavridou-Grigoriadou V, Siasos G et al (2013) Impact of long-term treatment with low-dose inhaled corticosteroids on the bone mineral density of chronic obstructive pulmonary disease patients: aggravating or beneficial? Respirology 18:147–153
Elmståhl S, Ekström H, Johnell O, Gerhardsson de Verdier M, Norjavaara E (2006) No association between inhaled corticosteroids and whole body DXA in postmenopausal women. Pharmacoepidemiol Drug Saf 15:527–535
Loke YK, Cavallazzi R, Singh S (2011) Risk of fractures with inhaled corticosteroids in COPD: systematic review and meta-analysis of randomised controlled trials and observational studies. Thorax 66:699–708
Acknowledgements
The authors thank the Division of Pneumology at the Hospital Universitario Clementino Fraga Filho HUCFF-UFRJ for the collaboration.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Appendix
Appendix
See Table 5.
About this article
Cite this article
Gonçalves, P.A., dos Santos Neves, R., Neto, L.V. et al. Inhaled glucocorticoids are associated with vertebral fractures in COPD patients. J Bone Miner Metab 36, 454–461 (2018). https://doi.org/10.1007/s00774-017-0854-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-017-0854-3