Abstract
Osteoporosis has recently been recognized as a major comorbidity in chronic obstructive pulmonary disease (COPD). We conducted a cross-sectional study in a cohort of 136 Japanese males with COPD to evaluate the prevalence of vertebral fracture (VF) and to explore its relationship with pulmonary function parameters. VFs were present in 108 (79.4 %); multiple and severe (SQ grade 2 or 3) VFs were found in 77 (56.6 %) and 25 (18.4 %), respectively. Multivariate logistic regression analyses revealed that decrease in forced expiratory volume in one second (FEV1.0)/forced vital capacity (FVC) [odds ratio (OR) 0.963, 95 % confidence interval (CI) 0.929–998, p = 0.036] was associated with the presence of VF after adjustment for age and that FVC (OR 0.462, 95 % CI 0.220–0.968, p = 0.041) and current smoking (OR 2.992, 95 % CI 1.128–7.940, p = 0.028) were associated with VF severity (grade 2–3 vs. 1). We also found that FEV1.0 was the sole independent determinant of the number of VFs by stepwise multivariate linear regression (p < 0.001). Bone mineral density (BMD) values were available in 49 subjects. Mean T scores were −2.0 ± 1.2 in femoral neck, −1.4 ± 1.2 in total hip and −1.1 ± 1.4 in lumbar spine. Nineteen patients (38.8 %) had a BMD T score less than −2.5. BMD Z scores of all the sites showed a progressive decrease as GOLD stage of COPD advanced (p < 0.05). Our results indicate a high prevalence of osteoporosis in Japanese male COPD patients and a strong inter-relationship between the two diseases, re-emphasizing the urgent need for appropriate intervention to maintain both bone and lung health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is described as a preventable and treatable disease that is characterized by progressive airflow limitation. Although COPD is primarily caused by an abnormal response of the lung tissue to cigarette smoking and other harmful particles or gases, it is often associated with various comorbidities including atherosclerosis, muscle wasting and osteoporosis, contributing to diminished quality of life and increased mortality of the affected subjects [1].
Among such systemic features of COPD, osteoporosis is now recognized as a major comorbidity that needs clinicians’ attention and appropriate therapeutic intervention [1, 2]. Indeed, the prevalence of osteoporosis and vertebral fractures in patients with COPD has been reported to be as high as 9–69 % [3] and 24–63 % [2], respectively. Conversely, a recent report indicates that COPD is the most frequent cause of secondary osteoporosis in men, followed by corticosteroid use, hypogonadism and other disorders [4]. Although many observational studies have reported association of COPD with decreased bone mineral density (BMD) and/or vertebral fractures (VFs) [5–14], the etiological and pathophysiological link between COPD and osteoporosis has not been well understood, and whether or not particular pulmonary function parameters correlate with vertebral fractures (VFs) and bone loss in COPD patients remains controversial. In Japan, only a few studies have investigated osteoporosis in subjects with COPD [15–18].
In the present study, we thus aimed to evaluate the prevalence of vertebral fractures (VFs) and low BMD in Japanese male subjects with COPD. We also explored the association of VFs and BMD with pulmonary function parameters. The results indicate high prevalence of osteoporosis in COPD patients in Japan and illustrate a complex interactive relationship between the two diseases.
Materials and methods
Subjects
This is a cross-sectional study enrolling 136 Japanese males who were diagnosed with COPD and had a lateral spine X-ray examination. Subjects were recruited at either Teikyo University Chiba Medical Center or Yarita Hospital from April 2011 until July 2013. Diagnosis and classification of COPD was made according to the Global Initiative for Chronic Obstructive Lung Disease criteria (GOLD) [19]. We excluded patients with a secondary cause of osteoporosis such as hyperthyroidism, hyperparathyroidism, chronic renal failure (GFR less than 30 mL/min), corticosteroid use for other diseases, type 1 diabetes mellitus and bone metastatic cancer. Height and weight were measured and body mass index (BMI) was calculated. Information on medical history, smoking status and corticosteroid use was obtained from patient interviews and medical records. Smoking exposure was estimated by pack-years, calculated by multiplying the number of packs of cigarettes smoked per day by the number of years the person had smoked. The COPD assessment test (CAT) in the Japanese version was used to evaluate impairment of general health status in 30 subjects. The CAT is composed of 8 items of relevant symptoms, viz., cough, phlegm, chest tightness, breathlessness, activity limitation at home, confidence in leaving home (mental), sleep and energy (vigor) [20, 21]. The study protocol was approved by an institutional ethical committee and informed consent was obtained from all the participants.
Pulmonary function test
Pulmonary function tests were performed under stable condition in all patients. Vital capacity (VC), forced vital capacity (FVC) and forced expiratory volume in one second (FEV1.0) were measured by spirometry and the FEV1.0/FVC ratio was determined. Patients with FEV1.0/FVC less than 0.7 were diagnosed as having COPD, and classified into four stages by FEV1.0 expressed as percent of predicted values (FEV1.0 %predicted) according to the GOLD criteria [19]: stage 1 (equal to or more than 80 % of predicted), stage 2 (50–80 % of predicted), stage 3 (30–50 % of predicted) and stage 4 (less than 30 % of predicted).
Assessment of vertebral fractures (VFs)
The number of VFs was evaluated using thoracic and lumbar spine X-rays. Lumbar spine images were unavailable in 50 subjects. Six subjects had only a lumbar spine X-ray examination. The severity of vertebral fractures was morphologically assessed according to the semi-quantitative method of Genant et al. [22], and classified into 3 grades: grade 1 (20–25 % reduction in anterior, middle and/or posterior height and 10–20 % reduction of the projected vertebral area), grade 2 (25–40 % reduction in heights and 20–40 % reduction of the projected vertebral area) and grade 3 (equal to or more than 40 % reduction in heights).
BMD measurement
Bone mineral density was measured at lumbar spine (L1–4), femoral neck and total hip using dual energy X-ray absorptiometry (Discovery W: Hologic Inc., Bedford, MA, USA). BMD was expressed as an absolute value, T scores (standard deviations from a young, sex-specific reference mean BMD) and Z scores (standard deviations from age- and sex-specific reference mean BMD). For lumbar spine BMD measurement, we excluded vertebrae that were affected by local structural change or artifact. According to the WHO criteria, T score less than −2.5, between −2.5 and −1.0, and more than −1.0 was defined as osteoporosis, osteopenia and normal BMD, respectively [23].
Statistical analysis
All statistical analyses were performed using SPSS Version 21(IBM Inc., Tokyo, Japan). To compare continuous variables, analysis of variance (ANOVA) with post-hoc Tukey HSD test or Student’s t test were performed as appropriate. Discrete variables were presented as percentages and compared with Pearson’s Chi-squared test. Multivariate logistic regression analyses were performed to identify the determinants of the presence and the severity of fractures (grade 2 or 3 compared with grade 1). Spearman’s correlation tests were used to examine correlates of the number of vertebral fractures or FEV1.0, and multivariate linear regression analyses were performed to identify independent determinants. A p value less than 0.05 was considered significant.
Results
Patient characteristics
Characteristics of the 136 study subjects are shown in Table 1. There was no significant difference in age among GOLD stages, whereas height and BMI were significantly lower in stage 4. As expected, all the parameters of respiratory function decreased as the stages advanced, and more patients in advanced stages were receiving home oxygen therapy and had been exposed to corticosteroids. The proportion of current smokers was the lowest in GOLD 3, but there was no significant difference in pack-years smoked. Of the 136 patients, only 4 had been treated for osteoporosis with alendronate alone or in combination with alfacalcidol. A diagnosis of osteoporosis had never been made in any of the other subjects. As for non-traumatic, non-vertebral fractures, the medical record and patient interview revealed a history of one hip, one forearm and seven rib fractures.
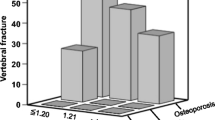
Vertebral fracture (VF)
The overall prevalence of VFs was 79.4 % (108/136), and two or more VFs were observed in 77 subjects (56.6 %) (Table 1). More than half of the VFs occurred at Th7, Th8, Th11, Th12 and L1. Severe fractures with SQ Grade 2 or 3 were present in 25 (18.4 %) subjects. Neither VF prevalence nor the average per person-number of VFs was statistically different among GOLD stages. Grade 2 or 3 VFs tended to increase as GOLD stage advanced, without statistical significance.
Compared with subjects without VFs, those with VFs were slightly older and shorter in height (Table 2). Among pulmonary parameters, only FEV1.0/FVC was significantly lower in the fracture group. Multivariate logistic regression analysis revealed that FEV1.0/FVC was the only independent determinant of the presence of VFs after adjustment for age (Table 3). The contribution of FEV1.0/FVC, however, became insignificant after further adjustment for height. The results remained basically unchanged after an adjustment for FVC and FEV1.0.
As for the severity of VFs, the subject group with grade 2 or 3 VFs had a shorter stature and lower FVC, and included more current smokers, compared with the group with grade 1 VFs. No other parameters were significantly different between the two groups (data not shown). Multivariate logistic regression with these parameters as covariables indicated that FVC and current smoking were independently associated with severe VFs (Table 4).
As shown in Table 5, age and pulmonary function parameters correlated with the number of VFs. Multivariate linear regression analysis revealed that FEV1.0 (β = −0.279, p = 0.001) was the sole independent determinant of the number of VFs after stepwise variable selection excluding age, body mass index, height, FEV1.0/FVC, inhaled corticosteroid use, current oral or past oral and/or intravenous corticosteroid use, current smoking, pack-years smoked and home oxygen therapy. FVC was significant when included instead of FEV1.0, but significance disappeared when included simultaneously with FEV1.0 (data not shown), suggesting that FEV1.0 was the predominant determinant of the number of VFs. Conversely, among correlates of FEV1.0 (Table 6), the number of VFs was an independent determinant of FEV1.0 in addition to height and home oxygen therapy, as shown in Table 7.
Bone mineral density
The number (%) of subjects whose BMD was available at each GOLD stage was 15 (30.6 %), 19 (38.8 %), 11 (22.4 %) and 4 (8.2 %), respectively, with the sum being 49 subjects. Mean T scores were −2.0 ± 1.2 in femoral neck, −1.4 ± 1.2 in total hip and −1.1 ± 1.4 in lumbar spine. In this subpopulation, BMI was significantly lower in stage 4, and all the pulmonary parameters were worse in advanced stages (data not shown), as observed in the whole cohort. Compared to the whole cohort of 136 subjects, these 49 subjects tended to be at earlier GOLD stage with a significantly higher mean value of FEV1.0 %predicted (66 vs. 56 %, p = 0.02). There was no difference in any other parameter. According to the WHO criteria, 19 (38.8 %) had osteoporosis, 21 (42.9 %) had osteopenia, and 9 (18.4 %) had normal BMD. According to the 2012 Japanese diagnostic criteria for osteoporosis [24], 41 subjects (83.7 %) were diagnosed as having osteoporosis. The higher value with the Japanese criteria is due to an extremely high prevalence of VFs in our subjects. Only five subjects were diagnosed with osteoporosis by BMD without fragility fractures.
We then examined whether or not GOLD stages were associated with BMD. As shown in Fig. 1, BMD Z scores at all sites measured showed a progressive decrease as GOLD stage became advanced, with values in GOLD 3 or 4 subjects being significantly lower than those in GOLD 1. Femoral neck BMD was significantly correlated negatively with age, and positively with height, BMI and pulmonary function parameters (data not shown). In multivariate linear regression analysis, FEV1.0 and BMI were significant predictors of femoral neck BMD after stepwise variable selection excluding height, FEV1.0/FVC, home oxygen therapy, current smoking, inhaled corticosteroid use, current oral and past oral and/or intravenous corticosteroid use (data not shown). However, the significance of the association between femoral neck BMD and FEV1.0 disappeared after adjustment for age (p = 0.074). Lumbar BMD gave no significant results, probably reflecting imprecision of the measurement caused by VFs.
BMD Z scores at lumbar spine, femoral neck and total hip in each GOLD stage. BMD at three sites was measured in 49 subjects, and Z scores in each GOLD stage were compared. Error bars indicate standard deviations. ANOVA with a post-hoc analysis by Tukey’s HSD test was used to determine statistical significance. *p < 0.05 compared with GOLD 1
Interestingly, CAT scores also showed a weak but significant negative correlation with total hip and femoral neck BMD Z scores (Fig. 2 and data not shown), illustrating a potential impact of general health status on BMD in COPD patients. No other anthropometric, bone or pulmonary parameter showed a significant correlation with CAT scores.
Discussion
In this cross-sectional study, we demonstrated an extremely high prevalence of VF (79.4 %) in Japanese men with COPD. The prevalence of osteoporosis in subjects whose BMD was available was 38.8 % according to the WHO criteria, and was much higher (83.7 %) according to the Japanese diagnostic criteria for osteoporosis [24]. The substantial difference observed here is due to the fact that the WHO criteria depend solely on BMD and do not take prevalent fractures into account. We found that, besides age, FEV1.0/FVC was the sole predictor of the presence of VF in COPD, and that lower FVC was associated with the presence of grade 2 or 3 VF. Moreover, FEV1.0 was significantly negatively associated with the number of VFs. Conversely, the number of VFs was among the independent predictors of FEV1.0, together with height and use of home oxygen therapy, and BMD was associated with CAT scores reflecting health status impairment in COPD. We believe that our findings indicate a strong inter-relationship between COPD and osteoporosis.
The prevalence of vertebral fracture in COPD
The prevalence of VF (79.4 %) observed in this study is markedly higher than in previous studies (24–63 %) [2, 7, 10–12, 14]. Compared with previous studies, subjects in this study were leaner and slightly older, with the average BMI and age being 21.5 and 71.6 years, respectively. Furthermore, a high proportion of patients were receiving home oxygen therapy, especially in GOLD 3 or 4. These differences could account for the high prevalence of VF in the present study. Ethnic differences may also be involved, although the true incidence of COPD-associated osteoporosis in Japan is currently unknown.
Decreased BMD in COPD
The present study confirmed that COPD is associated with decreased BMD. The Z score of BMD at any site showed a progressive decrease as GOLD stage became advanced. FEV1.0 was associated with femoral neck BMD, but BMI and age, well-established risk factors of bone loss, seemed to contribute more strongly to femoral neck BMD. Previous studies reported that BMD in COPD patients was lower than in healthy subjects [13, 25, 26], and that progression of GOLD stage was associated with lower BMD [8, 13]. There are, however, some conflicting reports showing negative results in terms of dependency on GOLD stages [7] and association with pulmonary function parameters [27]. In our study, BMI was significantly lower in advanced GOLD stages, whereas no pulmonary function parameter remained to be an independent predictor of BMD after adjustment for BMI and other confounders. These results suggest that weight loss is a major contributor to BMD decrease in advanced COPD. It is also notable that BMD was not correlated with the number or severity of VFs with or without adjustment for age and BMI (data not shown), implying that not only BMD decline but also deterioration of bone quality may be involved in COPD-associated fractures [17]. The discrepancy between lumbar spine BMD and VF prevalence should, however, be interpreted with caution due to possible over-estimation of lumbar spine BMD. At least 34 fractures of lumbar vertebrae were observed in 49 subjects whose BMD was measured. Indeed, if we took the lowest T score among L1–4 instead of the mean, the average lumbar spine BMD T score decreased from −1.1 to −2.6, suggesting fracture or deformation-related over-estimation (data not shown). In addition, the sample number may have been insufficient to detect the contribution of BMD to VF. Thus, the issue of bone quality remains an open question.
Association between vertebral fracture and pulmonary function
Vertebral fracture and COPD stage
We found that FEV1.0/FVC and age, but not GOLD stage, were associated with the presence of VF. Some previous studies indicated increased prevalence of VF [11, 17] and vertebral deformities [9] with advanced GOLD stage, while others found no significant correlation between COPD stages or pulmonary function and the presence of VF [7, 14, 28]. The lack of such association in the current study may be due the fact that the subjects were relatively older, showing extremely high fracture prevalence. It seems plausible that VF occurs in early stages of COPD, in part independently of BMD decrease.
Vertebral fracture and FEV1.0/FVC
It is of note that among pulmonary function parameters lower FEV1.0/FVC was the only independent predictor of VF in our study. In both COPD and healthy subjects, an association between FEV1.0/FVC and VF has never been reported. Previous studies focused on GOLD stage defined by FEV1.0 %predicted or absolute value of FEV1.0 and paid little attention to FEV1.0/FVC. Although FEV1.0/FVC is decreased by definition in COPD, progression of COPD is accompanied by decrease in FVC, resulting in a further decline in the absolute amount of FEV1.0 but relatively preserved FEV1.0/FVC. Thus, FEV1.0 %predicted is considered to reflect clinical progression of COPD more precisely than FEV1.0/FVC, and is used for staging. The exact pathological process of the disease progression is, however, incompletely understood. COPD involves both small airway obstruction and parenchymal destruction, and recent reports have suggested that narrowing and loss of terminal bronchioles precedes emphysematous destruction [29]. In addition, a subset of subjects with COPD is known to exhibit concomitant bronchial inflammation of larger airways and fibrotic changes [30–32]. The former would further increase airway resistance while the latter would preferentially cause FVC loss with minimal changes in FEV1.0/FVC. Such variations in spatial and temporal patterns of disease progression will determine the course of changes in respiratory mechanics and may also distinctively affect bone metabolism. The role of FEV1.0/FVC in COPD-associated osteoporosis requires further investigation.
Fracture severity and pulmonary function
In our study, lower FEV1.0 was significantly associated with multiple fractures. Conversely, the number of VFs and home oxygen therapy use were independent predictors of FEV1.0. Moreover, lower FVC was associated with the presence of grade 2 or 3 VF. These findings indicate a close relationship between impaired pulmonary function and progression of osteoporosis. One obvious explanation for this relationship would be the possibility that multiple and/or severe fractures result in thoracic deformity and fragility, ultimately disturbing pulmonary function. However, few reports have demonstrated this seemingly simple concept [33], and in these studies pulmonary diseases were excluded. Low thoracic muscle mass and/or strength could also disturb respiratory function in fragile elderly subjects with severe fractures. Thus, the direct impact of VF on respiratory function still remains an open question. Less clear is the etiological significance of decreased FEV1.0 and FVC in osteoporosis progression. One prospective study [34] reported that patients who developed osteoporosis during the 3-year follow-up showed a significant decrease in FEV1.0 whereas those who did not become osteoporotic showed no significant changes in FEV1.0. Another recent report in Japan has demonstrated that COPD patients with a history of acute exacerbations exhibited more progressive BMD decrease than those without exacerbation [16]. Further studies will be necessary to establish a causal link between COPD and osteoporosis progression.
General health status and osteoporosis in COPD
Staging of the disease does not necessarily reflect general performance and daily activities of COPD patients. In fact, it has been reported that osteoporosis was associated with higher MRC (Medical Research Council) dyspnea scores [35], although there are also conflicting reports demonstrating that MRC dyspnea scores of patients who developed osteoporosis did not change significantly during a 3-year follow-up period [34]. Recently, CAT scores have come to be used globally instead of the MRC dyspnea scale as a tool for assessment of the health status impairment of COPD. We found that CAT scores negatively correlated with total hip BMD Z scores after adjustment for BMI. Severe pulmonary symptoms of COPD would restrict physical activity, which may account for reduced BMD in weight-bearing bones. As far as we know, this is the first report demonstrating an association of CAT scores with bone loss.
Study limitations
The current study has several limitations. First, due to the cross-sectional study design and the small sample size, we were unable to determine the actual fracture incidence. We need large-scale prospective studies to examine the incidence of vertebral fracture. Second, non-COPD controls were not enrolled. Third, spine X-ray for fracture survey as well as BMD measurement was incomplete. The number of VFs may therefore have been underestimated. Finally, although we defined COPD by the standard spirometric test, it was not based on post-bronchodilator examination, raising a concern that a small minority of subjects diagnosed as having COPD may have had asthma.
Conclusion
In conclusion, our study demonstrated an extremely high prevalence of VF in Japanese males with COPD. Distinct pulmonary function parameters were found to be associated with the presence, severity and number of VFs, and BMD decline, suggesting a complex bidirectional interaction between COPD and osteoporosis. Despite the high prevalence of VF and strong inter-relationship between COPD and osteoporosis, only a few patients were treated for osteoporosis in our study, as well as in previous studies in other countries [5, 7]. Thus, emphasis should be put on the urgent need for an appropriate and timely intervention for COPD-associated osteoporosis, which would protect against fractures and might also improve the prognosis of pulmonary function in patients with COPD. Large-scale longitudinal studies will be necessary to define the exact condition and timing of treatment initiation for osteoporosis in COPD subjects, and such knowledge of COPD-associated osteoporosis should be widely publicized to raise the awareness of physicians treating COPD.
References
Decramer M, Janssens W, Miravitlles M (2012) Chronic obstructive pulmonary disease. Lancet 379:1341–1351
Lehouck A, Boonen S, Decramer M, Janssens W (2011) COPD, bone metabolism, and osteoporosis. Chest 139:648–657
Graat-Verboom L, Wouters EF, Smeenk FW, van den Borne BE, Lunde R, Spruit MA (2009) Current status of research on osteoporosis in COPD: a systematic review. Eur Respir J 34:209–218
Ryan CS, Petkov VI, Adler RA (2011) Osteoporosis in men: the value of laboratory testing. Osteoporos Int 22:1845–1853
Carter JD, Patel S, Sultan FL, Thompson ZJ, Margaux H, Sterrett A, Carney G, Murphy N, Huang Y, Valeriano J, Vasey FB (2008) The recognition and treatment of vertebral fractures in males with chronic obstructive pulmonary disease. Respir Med 102:1165–1172
Graat-Verboom L, Spruit MA, van den Borne BE, Smeenk FW, Martens EJ, Lunde R, Wouters EF (2009) Correlates of osteoporosis in chronic obstructive pulmonary disease: an underestimated systemic component. Respir Med 103:1143–1151
Graat-Verboom L, van den Borne BE, Smeenk FW, Spruit MA, Wouters EF (2011) Osteoporosis in COPD outpatients based on bone mineral density and vertebral fractures. J Bone Miner Res 26:561–568
Kjensli A, Mowinckel P, Ryg MS, Falch JA (2007) Low bone mineral density is related to severity of chronic obstructive pulmonary disease. Bone 40:493–497
Kjensli A, Falch JA, Ryg M, Blenk T, Armbrecht G, Diep LM, Ellingsen I (2009) High prevalence of vertebral deformities in COPD patients: relationship to disease severity. Eur Respir J 33:1018–1024
McEvoy CE, Ensrud KE, Bender E, Genant HK, Yu W, Griffith JM, Niewoehner DE (1998) Association between corticosteroid use and vertebral fractures in older men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 157:704–709
Nuti R, Siviero P, Maggi S, Guglielmi G, Caffarelli C, Crepaldi G, Gonnelli S (2009) Vertebral fractures in patients with chronic obstructive pulmonary disease: the EOLO Study. Osteoporos Int 20:989–998
Papaioannou A, Parkinson W, Ferko N, Probyn L, Ioannidis G, Jurriaans E, Cox G, Cook RJ, Kumbhare D, Adachi JD (2003) Prevalence of vertebral fractures among patients with chronic obstructive pulmonary disease in Canada. Osteoporos Int 14:913–917
Sin DD, Man JP, Man SF (2003) The risk of osteoporosis in Caucasian men and women with obstructive airways disease. Am J Med 114:10–14
Jorgensen NR, Schwarz P, Holme I, Henriksen BM, Petersen LJ, Backer V (2007) The prevalence of osteoporosis in patients with chronic obstructive pulmonary disease: a cross sectional study. Respir Med 101:177–185
Katsura H, Kida K (2002) A comparison of bone mineral density in elderly female patients with COPD and bronchial asthma. Chest 122:1949–1955
Kiyokawa H, Muro S, Oguma T, Sato S, Tanabe N, Takahashi T, Kudo M, Kinose D, Kondoh H, Kubo T, Hoshino Y, Ogawa E, Hirai T, Mishima M (2012) Impact of COPD exacerbations on osteoporosis assessed by chest CT scan. COPD 9:235–242
Ogura-Tomomatsu H, Asano K, Tomomatsu K, Miyata J, Ohmori N, Kodama M, Ueda S, Takihara T, Tanaka K, Kamiishi N, Suzuki Y, Fukunaga K, Oguma T, Sayama K, Betsuyaku T (2012) Predictors of osteoporosis and vertebral fractures in patients presenting with moderate-to-severe chronic obstructive lung disease. COPD 9:332–337
Ohara T, Hirai T, Muro S, Haruna A, Terada K, Kinose D, Marumo S, Ogawa E, Hoshino Y, Niimi A, Chin K, Mishima M (2008) Relationship between pulmonary emphysema and osteoporosis assessed by CT in patients with COPD. Chest 134:1244–1249
Global Initiative for Chronic Obstructive Lung Disease (updated 2013). http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf
Tsuda T, Suematsu R, Kamohara K, Kurose M, Arakawa I, Tomioka R, Kawayama T, Hoshino T, Aizawa H (2012) Development of the Japanese version of the COPD Assessment Test. Respir Investig 50:34–39
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N (2009) Development and first validation of the COPD Assessment Test. Eur Respir J 34:648–654
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Kanis JA (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int 4:368–381
Soen S, Fukunaga M, Sugimoto T, Sone T, Fujiwara S, Endo N, Gorai I, Shiraki M, Hagino H, Hosoi T, Ohta H, Yoneda T, Tomomitsu T (2013) Diagnostic criteria for primary osteoporosis: year 2012 revision. J Bone Miner Metab 31:247–257
Dam TT, Harrison S, Fink HA, Ramsdell J, Barrett-Connor E (2010) Bone mineral density and fractures in older men with chronic obstructive pulmonary disease or asthma. Osteoporos Int 21:1341–1349
Duckers JM, Evans BA, Fraser WD, Stone MD, Bolton CE, Shale DJ (2011) Low bone mineral density in men with chronic obstructive pulmonary disease. Respir Res 12:101
Dennison EM, Dhanwal DK, Shaheen SO, Azagra R, Reading I, Jameson KA, Sayer AA, Cooper C (2013) Is lung function associated with bone mineral density? Results from the Hertfordshire Cohort Study. Arch Osteoporos 8:115
Majumdar SR, Villa-Roel C, Lyons KJ, Rowe BH (2010) Prevalence and predictors of vertebral fracture in patients with chronic obstructive pulmonary disease. Respir Med 104:260–266
McDonough JE, Yuan R, Suzuki M, Seyednejad N, Elliott WM, Sanchez PG, Wright AC, Gefter WB, Litzky L, Coxson HO, Pare PD, Sin DD, Pierce RA, Woods JC, McWilliams AM, Mayo JR, Lam SC, Cooper JD, Hogg JC (2011) Small-airway obstruction and emphysema in chronic obstructive pulmonary disease. N Engl J Med 365:1567–1575
Washko GR, Hunninghake GM, Fernandez IE, Nishino M, Okajima Y, Yamashiro T, Ross JC, Estepar RS, Lynch DA, Brehm JM, Andriole KP, Diaz AA, Khorasani R, D’Aco K, Sciurba FC, Silverman EK, Hatabu H, Rosas IO (2011) Lung volumes and emphysema in smokers with interstitial lung abnormalities. N Engl J Med 364:897–906
Novosad SA, Barker AF (2013) Chronic obstructive pulmonary disease and bronchiectasis. Curr Opin Pulm Med 19:133–139
Tomiyama H, Okazaki R, Koji Y, Usui Y, Hayashi T, Hori S, Yamashina A (2005) Elevated C-reactive protein: a common marker for atherosclerotic cardiovascular risk and subclinical stages of pulmonary dysfunction and osteopenia in a healthy population. Atherosclerosis 178:187–192
Harrison RA, Siminoski K, Vethanayagam D, Majumdar SR (2007) Osteoporosis-related kyphosis and impairments in pulmonary function: a systematic review. J Bone Miner Res 22:447–457
Graat-Verboom L, Smeenk FW, van den Borne BE, Spruit MA, Jansen FH, van Enschot JW, Wouters EF (2012) Progression of osteoporosis in patients with COPD: a 3-year follow up study. Respir Med 106:861–870
Miller J, Edwards LD, Agusti A, Bakke P, Calverley PM, Celli B, Coxson HO, Crim C, Lomas DA, Miller BE, Rennard S, Silverman EK, Tal-Singer R, Vestbo J, Wouters E, Yates JC, Macnee W (2013) Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Respir Med 107:1376–1384
Acknowledgments
We would like to thank Yoshie Fujita for her technical assistance.
Conflict of interest
All authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Watanabe, R., Tanaka, T., Aita, K. et al. Osteoporosis is highly prevalent in Japanese males with chronic obstructive pulmonary disease and is associated with deteriorated pulmonary function. J Bone Miner Metab 33, 392–400 (2015). https://doi.org/10.1007/s00774-014-0605-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-014-0605-7