Abstract
Purpose: Patients with chronic obstructive pulmonary disease (COPD) may be at higher risk for osteoporosis. The primary objective of this case-control study was to determine the prevalence of vertebral fractures among patients with COPD admitted to acute care compared with a gender- and age-matched control group. Subjects and methods: Subjects were identified by chart reviews from an acute care hospital in Hamilton, Ontario, in 1999, including patients who were over 50 years old. In total, 127 patients with ICD-9 codes specifying COPD were randomly selected and compared with 127 gender- and age-matched controls. Chest radiographs were interpreted by two radiologists who defined and graded vertebral fractures using Genant’s method. Medications taken, or prescribed at discharge, were recorded from charts. Results: The overall prevalence of at least one vertebral fracture was found to be 34/127 (26.8%) in the COPD patients compared with 30/127 (23.6%) in the controls (p=0.556). A significantly greater proportion of COPD patients had at least one severe vertebral fracture (OR=3.75, 95% CI 1.24 to 11.3). Review of hospital chest X-ray reports indicated that only 12 of 64 (18.8%) patients with vertebral fractures identified by the study radiologists actually had a vertebral fracture noted in the report. The proportion of COPD patients with vertebral fractures who were discharged on osteoporosis therapy was 5/27 (18.5%). There was a suggestion of lower lung function, as measured by forced vital capacity (FVC%), in patients with severe vertebral fractures (p=0.067). Conclusions: These data indicate that: (1) There is an increased proportion of COPD patients with severe vertebral fracture, and (2) Documentation and treatment of osteoporosis in acute care COPD patients is low. Therefore, there is a need to target this high-risk group for osteoporosis screening and potential clinical management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vertebral fractures are the most common type of osteoporotic fracture [1]. Approximately 30% of vertebral fractures are symptomatic and diagnosed, thus many vertebral fractures often go undetected [2]. However, their presence entails a fivefold increase in the risk of another vertebral fracture and a threefold increase in the risk of hip fracture within 3 years [3].
Individuals with chronic obstructive pulmonary disease (COPD) have been considered to be at a higher risk for osteoporosis which may to some extent be related to corticosteroid use [4, 5]. Oral corticosteroid use has been associated with loss of bone density and fracture [6, 7]. The effect of inhaled corticosteroids on bone is not yet clear [8, 9].
The actual prevalence of osteoporosis-related fractures in COPD patients has not been extensively studied. Moreover, research examining morbidity and health care utilization has demonstrated underrecognition and undertreatment of vertebral fractures among hospitalized patients [10]. The paucity of data on prevalence of fractures in COPD patients may contribute to undertreatment.
The primary objective of this study was to determine the prevalence of vertebral fractures among patients with COPD admitted to acute care compared with a gender- and age-matched control group. Secondary objectives were to determine the relationship between vertebral fractures and measures of lung function and the extent to which those with vertebral fractures received treatment for osteoporosis.
Methods
Study population and selection
Patients were selected using data from hospital records of those admitted between January 1, 1999, and December 31, 1999, to St. Joseph’s Healthcare, an acute care teaching hospital in Hamilton, Ontario, Canada. Patients were included if they were age 50 or older, and if a lateral chest X-ray taken during the index admission was available. Patients were excluded if their chest X-ray was prompted by physical trauma and if they had known or suspected malignancy.
In total, 331 charts were available on patients with primary diagnosis of COPD or asthma (ICD-9 codes 490–496) in 1999. After removing repeat hospital admissions and those not meeting criteria, 143 patients (i.e., cases) remained. The three main reasons for exclusion were unavailable chest X-ray, outside age range, and malignancy. Controls were selected from all those admitted over the age of 50 years, without a diagnosis of COPD/asthma (490–496). One chart was randomly selected from every 20 successive medical admissions and reviewed for inclusion/exclusion criteria. If excluded, a second chart was randomly selected from the remaining 19 until a subject met criteria. The selected subject was then initially matched to the COPD patient based on sex and closest in age. A control meeting criteria was excluded if they could not be matched within 5 years to a COPD patient. After appropriate matching, the final sample included 127 cases and 127 controls.
Radiology review
Two radiologists (authors L.P. and E.J.) blinded to group status, reviewed each lateral chest X-ray according to a semiquantitative technique adapted by Genant et al. [11]. Radiologists evaluated all the visible vertebrae on the lateral radiograph. If the end-plates of a vertebra could not be clearly visualized, it was not included in the assessment. Radiologic exclusion criteria included abnormality due to conditions other than osteoporosis. Deformity was graded as: normal, grade 1 (mild), grade 2 (moderate), or grade 3 (severe) [12].
Chest X-ray reports during index hospital admission were also abstracted. Chest X-rays performed prior to the current admission were also reviewed. The number and type of vertebral fractures, and occurrence of osteopenia was noted and compared with the radiology review of chest X-rays.
Interrater reliability was completed by the two radiologists on 46 independent chest X-ray films prior to the study. Raters were compared with respect to their assessment of whether there were any fractures present and for the number of fractures present. These analyses were completed for each grade of fracture. When discrepancy was found, radiologists reviewed films together and arrived at a consensus.
Outcome variables
Data were abstracted on the following variables: age, sex, weight, height, admitting diagnoses, current oral and inhaled corticosteroid use (dose, duration, frequency), medication use during hospital admission, and pulmonary function including, forced expiratory volume (FEV1; FEV%) and forced vital capacity (FVC; FVC%). When data on a variable were recorded in charts more than once, those values closest to hospital admission were used. Discharge records were reviewed to ensure that osteoporosis treatment reflected the patient’s status upon leaving the hospital. Osteoporosis treatment was defined as receiving one or more of calcium with or without vitamin D, hormone replacement therapy, raloxifene, bisphosphonates, and calcitonin.
Data analysis
The reliability of the radiologic assessments was examined by κ statistics for both the presence of fractures and the grade of fracture. McNemar test for matched pairs was used to test for associations between case-control status and fracture status. Multivariate conditional logistic regression models were also used to identify risk factors for fractures as well as to examine whether there were subgroups of patients for whom the association between case-control status and fracture status was different. Simple linear regression was used to examine the relationship between vertebral fracture status and measures of lung function including FVC% and %FEV1. Differences in the distribution of duration of hospitalization were assessed using Cox regression models.
Results
A total of 127 COPD patients with a mean (±SD) age of 71.6 (±9.2) years and 127 control patients with a mean age of 71.1 (±9.7) years were included in this study. There were a total of 126 (49.6%) men. For COPD patients, the average predicted FVC% was 47.4% (±16.7) and the predicted %FEV1 was 32.5% (±16.9) upon admission. The most common responsible diagnoses for the control patients included congestive heart failure, pneumonia, and chest pain/angina.
Prevalence of vertebral fractures
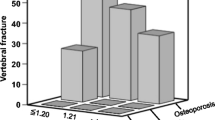
Review of chest X-rays was completed for 127 matched pairs. The overall prevalence of at least one vertebral fracture was found to be 34/127 (26.8%) in the COPD patients compared with 30/127 (23.6%) in the controls (p=0.556).
Univariate conditional logistic regression suggested that a significantly greater proportion of COPD patients had at least one severe (grade 3) vertebral fracture (OR=3.75, 95% CI 1.24 to 11.3). However, there were no significant differences in the proportion of mild (grade 1) (p=0.538) or moderate (grade 2) (p=0.258) vertebral fractures between the COPD patients and controls (Tables 1 and 2).
Multivariate conditional logistic regression analysis showed that age was an independent predictor of vertebral fractures (p=0.002). In total, 31/126 (24.6%) men and 33/128 (25.8%) women were found to have at least one vertebral fracture. There were no differences in association between vertebral fractures and COPD status found between men and women (p=0.378). The Cox regression model of the duration of hospitalization did not reveal any association with vertebral fracture status.
Only 12 of 64 (18.8%) patients with vertebral fractures had these fractures identified on the hospital chest X-ray report. In total, the study radiologists and hospital chest X-ray reports agreed that 185 patients did not have a vertebral fracture. The hospital chest X-ray reports noted that “osteopenia” was present for 7/127 (5.5%) of the COPD patients and 8/127 (6.3%) of the controls. In particular, for those with vertebral fractures, 4/64 (6.3%) had hospital chest X-rays that noted “osteopenia.”
Interrater reliability
The interrater reliability (κ statistic) for the detection of one or more fractures was very good (0.626, 95% CI 0.367 to 0.885) for any type of fracture and for the number of fractures (0.862, 95% CI 0.755 to 0.969). Good interrater reliability was found for the presence of one or more grade 1 fractures (0.425, 95% CI 0.129 to 0.721) and for the number of grade 1 fractures (0.507, 95% CI 0.159 to 0.855). There was perfect concordance on the presence of grade 2 fractures and the presence of grade 3 fractures, though they arose in only 8.7% and 4.3% of the patients, respectively.
Diagnosis and treatment of osteoporosis
Among COPD patients found by the study radiologists to have vertebral fractures, 8/34 (23.5%) had a diagnosis of osteoporosis in their medical records. In total, of the 127 matched pairs, 15/254 (5.9%) patients had a diagnosis of osteoporosis. The proportion of COPD patients with vertebral fractures who were discharged on at least one osteoporosis therapy was 5/27 (18.5%). This is in contrast to 7/93 (7.5%) of COPD patients without a vertebral fracture who were also given at least one osteoporosis medication at discharge. Of the control patients, 2/20 (10.0%) with vertebral fractures were discharged on osteoporosis therapy.
Lung function and vertebral fractures
Linear regression analyses suggest a trend toward lower lung function, as measured by FVC%, among patients with one or more grade 3 vertebral fractures. Neither grade 1 nor grade 2 vertebral fractures were associated with poor lung function. There was also a suggestion of an association between poor lung function and grade 3 vertebral fractures when the lung function was measured by the predicted %FEV1 (Table 3).
Corticosteroid exposure
In the matched COPD patients, a large proportion were reported as taking oral (74.7%) or inhaled (86.6%) corticosteroids at the time of index hospital admission. This is in contrast to the control group, where only four (3.5%) patients were taking oral and four (3.5%) were taking inhaled corticosteroids. There was no significant association between oral corticosteroid use at index hospital admission and vertebral fracture status (odds ratio (OR)=1.29, 95% CI 0.43 to 3.85). Similarly, there was also no association between inhaled steroid use and vertebral fracture status (OR=2.31, 95%CI 0.47 to 11.36).
Discussion
We found a fourfold higher prevalence of severe vertebral fractures among COPD patients, compared with age- and gender-matched controls. We found a trend towards lower percent FVC among patients with severe vertebral fractures. A care gap clearly exists in diagnosing patients with vertebral fractures as only 18% of patients found to have vertebral fractures actually had these fractures identified on their hospital chest X-ray report. Further, only 18% of patients with vertebral fractures were given osteoporosis therapy at discharge.
Previous studies in patients with lung disease have found a prevalence of vertebral fractures ranging from 4% to 63%. One cross-sectional study of patients with lung disease (i.e., asthma, COPD, alveolitis) found an overall prevalence of fractures of 23% for those taking oral corticosteroids for a median duration of 5.5 years. Vertebral fractures (4.1%) were more likely than other fracture types, however these were self-reported which may have decreased the prevalence [13]. Another cross-sectional study of men over 50 years of age with COPD found a much higher prevalence of vertebral fractures in men taking oral corticosteroids (63.3%) (mean duration = 163 weeks), followed by those in the inhaled corticosteroid group (57.1%) and those who never used corticosteroids (48.7%) [14]. In contrast, Riancho et al. [15] conducted a cross-sectional study in 44 men with COPD and did not find a high prevalence of vertebral fractures (5.3%) (using lateral spine X-rays). Small sample size and lack of corticosteroid use may be possible reasons for the negative findings of this particular study.
Systemic corticosteroid use has been shown to be associated with increased risk of osteoporosis and fractures, particularly of the spine. One study of 86 white men with COPD [12] determined that osteoporosis of the lumbar spine was most frequent in patients receiving greater than 1,000 mg of oral prednisolone cumulatively for the treatment of COPD exacerbations. Inhaled corticosteroid exposure has not been consistently linked with osteoporosis where one systematic review demonstrated that in patients with asthma or COPD, inhaled steroids do not increase vertebral fractures or reduce bone density [9]. The association between COPD and a decrease in bone mineral density has been argued to involve other variables in addition to corticosteroid use, such as decreased activity levels, nutritional deficiencies, presence of inflammatory disease, and lower levels of circulating anabolic steroids such as testosterone [4].
Our results showed a higher prevalence of severe vertebral fractures in COPD patients compared with controls. However, the overall prevalence of all vertebral fracture was not significantly different (i.e., 26.8% COPD and 23.6% controls). The prevalence of vertebral fracture in our study is similar to other reported studies [16, 17]. Thus, perhaps it is only the severity of vertebral fractures that is truly affected by COPD status, rather than overall prevalence. Second, given that the control population includes hospitalized patients with comorbid illnesses, the prevalence rate may be overestimated for a nonhospitalized, non-COPD population, due to other illnesses that might contribute to osteoporosis. Finally, the small sample size may have underestimated the true prevalence of vertebral fractures in COPD patients.
Our results also showed there was a trend towards lower lung function in patients with severe vertebral fractures compared with those without fracture. It has been estimated that each vertebral fracture in the thoracic spine results in a 9% decrease in predicted FVC [18]. In addition, vertebral fractures may themselves impact lung function by changing the configuration of the chest wall [19]. Further, one large study showed that women with radiographic evidence of vertebral fracture have an increased mortality rate, particularly from pulmonary disease and cancer [20].
Only 18% of patients found to have vertebral fractures actually had these fractures identified on their hospital chest X-ray report. Underreporting of vertebral fractures on lateral chest radiographs is likely to reflect the fact that radiologists generally report these studies in light of the clinical history, usually one of a respiratory complaint. As a result, most attention is directed to the thoracic viscera rather than the bony thorax. Furthermore, radiologists generally focus on what is considered to be a significant finding and as there was no satisfactory treatment for osteoporotic fractures in the past, these lesions were frequently ignored.
Our study has some important limitations. Certain potential confounding variables (e.g., serum testosterone levels) could not be adequately assessed due to the nature of the study design. Also, we may have actually underestimated the number and severity of vertebral fractures. Use of chest X-rays, as opposed to lateral spine X-rays, may not have allowed accurate detection of all possible vertebral fractures. McEvoy et al. [13] assessed vertebral fractures using spine X-rays with the Genant semiquantitative technique and found a higher prevalence of vertebral fractures. However, chest X-rays are commonly completed in COPD patients and represent a possible quick screening option for detection of vertebral fractures in the acute care setting. Further, although our sample size was initially larger, it was decreased due to the restrictions of appropriately matching cases and controls which limits generalizability to the larger non-COPD and COPD populations. Finally, we did not conduct an outpatient investigation of past use and total cumulative use of oral and inhaled corticosteroids. The study finding of no association between corticosteroid use and vertebral fracture likely demonstrates that steroid use at admission may be a biased/inadequate estimate of history of steroid use. Given that corticosteroid use data were lacking, we cannot attribute steroid use as a possible causative factor for the higher rate of severe fractures in the COPD patients.
Given the findings of this study, efforts need to be made to increase awareness and to develop improved interdisciplinary models for the assessment of osteoporosis risk and vertebral fractures in COPD patients. Research is needed to determine the underlying mechanisms causing higher mortality in patients with vertebral fractures which needs to be assessed in more depth.
References
Genant HK, Cooper C, Poor G et al (1999) Interim report and recommendations of the World Health Organization task-force for osteoporosis. Osteoporos Int 259–264
Cooper C, Melton LJ (1992) Vertebral fractures, how large is the silent epidemic? BMJ 304:793–794
Klotzbeucher CM, Ross PD, Landsman PB et al (2000) Patients with prior fracture have an increased risk of future fracture: summary of literature and statistical synthesis. J Bone Miner Res 15:721–727
Gross NJ (2001) Extrapulmonary effects of chronic obstructive pulmonary disease. Curr Opin Pulm Med 7:84–92
Manolagas SC, Weinstein RS (1999) New developments in the pathogenesis and treatment of steroid-induced osteoporosis. J Bone Miner Res 14:1061–1066
Likert BP, Raiaz LG (1990) Glucocorticoid-induced osteoporosis: pathogenesis and management. Ann Intern Med 112:352–364
Ruegsegger P, Medici TC, Anliker M (1983) Corticosteroid-induced bone loss. A longitudinal study of alternate day therapy in patients with bronchial asthma using quantitative computed tomography. Eur J Clin Pharmacol 25:615–620
Goldstein MF, Fallon JJ, Harning R (1999) Chronic glucocorticoid therapy-induced osteoporosis in patients with obstructive lung disease. Chest 116:1733–1749
Jones A, Fay JK, Burr M et al (2002) Review: Inhaled corticosteroids for asthma or chronic osbstructive pulmonary disease do not increase bone loss. Cochrane Database Syst Rev 1
Papaioannou A, Adachi JD, Parkinson W, Stephenson G, Bedard M (2001) Lengthy Hospitalization Associated with Vertebral Fractures Despite Control for Comorbid Conditions. Osteoporos Int 12(10):870–874
Genant HK, Jergas M, Palermo L et al (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis. J Bone Miner Res 11:984–996
Dubois EF, Roder E, Dekhuijzen R, Zwinderman AE, Schweitzer DH (2002) Dual energy x-ray absorptiometry outcomes in male COPD patients after treatment with different glucocorticoid regimens. Chest 121:1456–1463
Walsh LJ, Wong CA, Oborne J et al (2001) Adverse effects of oral corticosteroids in relation to dose in patients with lung disease. Thorax 56:279–284
McEvoy CE, Ensrud KE, Bender E et al (1998) Association between corticosteroid use and vertebral fractures in older men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 157:704–709
Riancho JA, Gonzalez Macias J, Delarco C et al (1987) Vertebral compression fractures and mineral metabolism in chronic obstructive lung disease. Thorax 42:962–966
Jackson SA, Tenenhouse A, Robertson L et al (2000) Vertebral fracture definition from population-based data: preliminary results from the Canadian Multicenter Osteoporosis Study (CaMos). Osteoporos Int 11:680–687
Melton LJ III, Kan SH, Frye MA et al (1989) Epidemiology of vertebral fractures in women. Am J Epidemiol 129:1000–1011
Leech JA, Dulberg C, Kellie S, Pattee L, Gay J (1990) Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis. 141:68–71
Schlaich C, Minne HW, Bruckner T et al (1998) Reduced pulmonary function in patients with spinal osteoporotic fracture. Osteoporos Int 8:261–267
Kado DM, Browner WS, Palermo L et al (1999) Vertebral fractures and mortality in older women: a prospective study. Arch Intern Med 159:1215–1220
Acknowledgements
We would like to thank Sonny Olatunji and Neil Hannigan for their assistance with data collection for the study and Bethany Giddings for her assistance with the project. We would also like to thank Procter & Gamble Pharmaceuticals for an educational grant-in-aid.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by a research grant from Procter & Gamble Pharmaceuticals.
Rights and permissions
About this article
Cite this article
Papaioannou, A., Parkinson, W., Ferko, N. et al. Prevalence of vertebral fractures among patients with chronic obstructive pulmonary disease in Canada. Osteoporos Int 14, 913–917 (2003). https://doi.org/10.1007/s00198-003-1449-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1449-5