Abstract
Purpose
Purpose of this study was to demonstrate that a single tunnel reconstruction of high-grade acromioclavicular (AC) joint instabilities with implants of the second generation is sufficient for stabilisation, especially in combination with an AC cerclage.
Methods
Patients with an acute AC-joint dislocation type Rockwood III-B and V were included. Besides clinical follow-up examination, radiographs were analysed. The functional outcome measures were Constant Score (CS), Taft score (TS), ACJI score and patient’s satisfaction. Horizontal instability was evaluated by clinical examination and radiological with an Alexander view.
Results
Thirty-five patients with a mean follow-up of 29 months were included. Ninety-seven per cent were satisfied with their result, with an average Subjective Shoulder Value of 90%. The CS averaged at 90 ± 10 points, TS at 11 ± 1 points and ACJI at 78 ± 18 points. Radiologically, 3 of 29 patients (10%) showed a persisting horizontal instability. The coracoclavicular (CC) distance improved from 22 preoperative to 10 mm postoperative, which was comparable to the contralateral side (10 mm, p = 0.103). At follow-up the CC distance increased to 13 mm (p = 0.0001).
Conclusion
AC-joint stabilisation with a single tunnel reconstruction using a second-generation implant results in good to excellent clinical results with high patient satisfaction. The additional AC augmentation improves stability in horizontal instable AC-joints and is recommended in all high-grade AC joint stabilisations. Nonetheless, reduction was slightly lost over time due to an elongation or suture failure of the coraco-clavicular fixation.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dislocations of the acromioclavicular (AC) joint belong to the most common injuries of the shoulder girdle and affect mainly physically active adults in the third and fourth decade of life [1]. The ideal surgical treatment of high-grade AC joint injuries remains controversial [2]. However, the introduction of arthroscopically assisted surgical techniques in recent years has been finding increasing acceptance, especially among shoulder surgeons [3]. Short to midterm results are encouraging and mainly good to excellent clinical outcomes are reported [4, 5]. The results of arthroscopically assisted flip-button techniques are comparable to classic open procedures, such as the clavicular hook plate [6]. The main advantages are a minimally invasive approach with less soft tissue damage and a high patient acceptance, no obligatory implant removal and the possibility of detection and treatment of concomitant glenohumeral injuries [6].
In the majority of the published clinical data, a double flip-button device with a block and tackle mechanism and implants of the first generation with a small clavicular washer were used (TightRope, Arthrex, Naples, Florida) [4, 5]. To date, there is no comparative clinical evidence that a double flip-button technique is superior to a single button approach [7]. Other minimally invasive fixation techniques based on a single flip-button device for coracoclavicular (CC) repair display good to excellent clinical results as well [8].
Despite rapid progress in implant and instrument development and widespread usage of the CC fixation techniques with a flip-button technique, preliminary results showed high rates of partial, recurrent horizontal AC joint instabilities, which were associated with inferior clinical results [5, 6]. An isolated CC reconstruction stabilizes predominantly in the vertical plane, allowing a persistent horizontal translation within the AC joint [9]. In high-grade AC joint dislocations (≥ Rockwood III-B), the AC joint capsule is ruptured beside the CC ligaments. The posterosuperior AC ligaments are the main restraint to posterior translation of the lateral clavicle [10]. The aim of any surgical approach to address instability of the AC joint should be an anatomic reduction and restoration of normal arthrokinetics and therefore, all components of instability should be addressed specifically [11]. The isolated CC repair should be enhanced with an AC augmentation technique, i.e. a minimally invasive suture cerclage [5]. Although the biomechanical value of an additional AC repair has already been proven [9], a lack of clinical evidence persists for this procedure.
The purpose of this study was to demonstrate that a single tunnel reconstruction with implants of the second generation with a larger supporting surface on the clavicle is sufficient for AC joint reconstruction, especially in combination with an AC cerclage. Moreover, it should be demonstrated that the addition of the minimally invasive AC augmentation is a reliable and reproducible procedure, which may lower the rate of recurrent horizontal instabilities.
Materials and methods
This retrospective study was performed at a department for arthroscopic shoulder surgery between March 2010 and February 2013. After approval of the study protocol by the local ethics committee (no. 1207–2011), the electronic database was screened for the diagnosis of AC joint dislocation (ICD-10 code: S43.1). Patient’s history, documented clinical examination, and preoperative radiographs verified the diagnosis. Preoperative imaging consisted of a bilateral antero-posterior (a.p.) stress view of the AC joint with a 10 kg load to measure the CC distance. An additional axillary view of the affected shoulder and bilateral Alexander views [12] were used to detect any static or dynamic horizontal instability (Fig. 1).
Patients with an acute AC joint dislocation Rockwood type III-B (increase in the CC-distance between 25 and 100% compared to the contralateral side with additional horizontal instability in the axial view and/or dynamic horizontal instability in the Alexander view) or Rockwood type V (increase in the CC distance more than 100% compared to the contralateral side) [13, 14] were included in this study. Acute injuries were defined as a maximum interval of 21 days between trauma and surgery. Patients younger than 18 years, missing horizontal instability in Rockwood type III injuries, a disease that would preclude accurate evaluation (e.g. neuromuscular, rheumatic, significant psychiatric, and metabolic disorders), and patients with previous AC joint or shoulder injuries of both the affected and contralateral sides were excluded from the study.
All patients were invited to a single, clinical follow-up examination. After obtaining written informed consent, the follow-up examination protocol consisted of a detailed physical examination. Besides evaluating range of motion of the affected shoulder, patient outcome measures (Subjective Shoulder Value [SSV] [15], Constant–Murley score [CMS] [16], AC joint specific acromioclavicular joint instability scores [ACJIS] [5], and Taft scores [TFS] [17]) were assessed. The AC joint specific ACJI score evaluates subjective (pain, activity of daily living, cosmetic), functional and radiological parameters. It ranges from 0 to 100 points with 100 being the best result. The TFS also evaluates subjective, objective and radiological parameters with 0 points being the worst and 12 points being the best result. Furthermore, patient satisfaction of the functional and cosmetic outcomes postoperatively was evaluated using a 5-part scale (1: “excellent” to 5: “poor”). Bilateral a.p. stress views of the AC joints and Alexander views were obtained to evaluate the horizontal and vertical stability during follow-up. Radiological evaluation included measuring vertical instability due to the CC distance (1) preoperatively, (2) on the postoperative radiograph, and (3) at the follow-up examination. The horizontal instability was evaluated with the help of the Alexander view preoperatively and at the follow-up. It further distinguished between horizontal stability and instability. The clavicle was defined as “unstable” or “dislocated”, if the difference was more than one clavicle shaft width [5]. For all measurements, an unaffected contralateral side served as control. In addition, the horizontal stability was tested clinically with a horizontal shift test [6, 11, 18]. The extent of the dorsal shift of the lateral clavicle against the acromion was evaluated and determined to be either horizontally stable or unstable. A possible implant migration, either of the clavicular washer or the subcoracoidal plate was evaluated on the a.p. stress view, as well as ossification between the clavicle and coracoids. In these radiographs, the maximum diameter of the CC drill tunnels was assessed to detect a potential tunnel enlargement.
Descriptive statistical analysis for quantitative variables was presented as means, standard deviations, and ranges. The results were tested for normal distribution using the Shapiro–Wilk normality test. A t test for independent means was used for normally distributed results. If not distributed normally, the Mann–Whitney U test, as a two-way analysis of variance, for independent factors was used. A p value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS for Windows (IBM SPSS Statistics 25, Chicago, Illinois).
Surgical technique
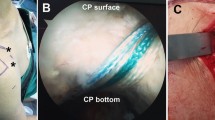
Under general anaesthesia and in the beach chair position, the arm was fixed in an arm holder. An image intensifier was integrated in the surgical setting to assure optimal placement of all drill tunnels. A standard posterior and anteroinferior portals were implemented as the main working portals. After diagnostic glenohumeral inspection and treatment of concomitant lesions, if necessary, an additional, anterolateral transtendinous viewing portal was established, which allowed a good visualisation of the coracoid base following the upper margin of the subscapular tendon as an orientation guide. The subcoracoid space and the coracoid base were exposed with a radiofrequency device. The AC joint was reduced under fluoroscopic control by means of cranialisation of the shoulder with the arm holder. A 2–3 cm skin incision was performed in line with the lateral clavicle and its surface prepared. The AC guide (Arthrex, Naples, FL, USA) allows collinear drilling through the clavicle and the coracoid base, and was placed underneath the coracoid arch, close to the base, via the low anterior portal. On the clavicle side, the guide was placed about 3–3.5 cm medial to the AC joint in the central anterior–posterior position of the clavicle. Using the single flip button technique, the desired clavicular position of the drill tunnel was between the insertion of the trapezoid and conoid ligament. The K-wire was drilled through the drill guide under fluoroscopic control. The subcoracoidal exit point was controlled arthroscopically. Subsequently, the K-wire was overdrilled with a 4 mm drill bit and the flip button device (TightRope, Arthrex) device inserted via a shuttle wire. The subcoracoid button was flipped and positioned under arthroscopic control. With the tightening of the block and tackle mechanism under fluoroscopic control, the AC joint was anatomically reduced and the flip button system was secured with 6–8 alternating half hitches (Fig. 1).
After the vertical reduction, an additional minimally invasive AC cerclage for horizontal stability was performed, according to the technique published by Jensen et al. [19]. Through the anteroinferior portal or an additional incision, a 1.2 mm drill wire was placed through the lateral clavicle in the antero-postero direction, about 1–1.5 cm medial to the AC joint. The wire was overdrilled with a 2.7 mm cannulated drill bit. A non-resorbable suture tape (FiberTape, Arthrex, Naples, FL, USA) was pulled through. Hence, the transacromial passage was prepared. The drill wire (1.2 mm) was placed percutaneously under fluoroscopic control via the incision of the anterolateral portal or a small, extra incision from caudal–lateral to medial–cranial in the acromion. The exit point was close and lateral to the AC joint. The pin was drilled with caution to avoid levering movements with a cannulated 2.7 mm drill bit (potential risk of fracture). A shuttle-wire was placed through the transacromial tunnel. The limb of the suture tape, which exited the clavicula posteriorly, was shuttled through this tunnel. The tape was returned towards the AC joint subcutaneously with a straight tissue grasper. The suture tape was tied together under tension and lateral pressure against the AC joint. Finally, the deltatrapezoid fascia was reconstructed and the clavicular incision and the portals were closed in a standard fashion.
Postoperatively, all patients were treated using a standardised protocol. The arm was placed in a sling for 6 weeks. During the first 6 weeks, only passive range of motion was allowed, gradually releasing up to a 60° angle during week 6.
After 6 weeks, a free passive range of motion was allowed and an active range of motion exercises was started. Strength training was delayed up to 3 months after surgery. A return to team and contact sport was allowed after 6 months.
Results
Between March 2010 and February 2013, 44 patients fit the inclusion criteria. Four were lost to follow-up due to migration and five refused to continue participating in the study. Therefore, 35 patients (80%) were included in this study and available for a follow-up examination with a mean follow-up of 29 months (range, 22–52 months). Thirty-four patients were male and one female. Six patients refused further follow-up radiographs due to no further complaints. Therefore, only patients completing both scoring systems (ACJIS and TFS; 29 of 35), including clinical examination and radiological results, were evaluated.
Twelve (34%) injuries were classified as Rockwood type III-B and 23 (66%) as Rockwood type V lesions. The mean age at time of injury was 40 years (range, 19–72 years). The mean time between trauma and surgery was 8 days (range, 2–20 days). In 63% of the injuries, the dominant side was affected. The injury mechanism was a direct trauma to the shoulder (n = 34) or an indirect trauma to the elevated arm (n = 1). Injuries occurred predominantly during sporting activities: cycling/motorcycling (n = 17), team sports (n = 11), alpine sports (n = 2), other trauma (n = 5). Concomitant intra-articular pathologies were identified in 14 of 35 patients (40%) during arthroscopy. In four patients (11%), these lesions were very likely related to the recent trauma: one partial articular supraspinatus tendon avulsion, one rupture of the superior glenohumeral ligament, one tear of the subscapularis tendon Lafosse type II-III and one type II SLAP lesion. Degenerative lesions were found in ten patients (29% with multiple findings in some patients). These were predominantly type I SLAP lesions (seven patients). In one patient, a superficial fraying of the subscapularis tendon was documented. Advanced humeral cartilage degeneration was detected in two cases, one with concomitant loose bodies. The surgeons described a degenerative partial rupture of the bicep tendon in two patients, which also might have been due to the acute trauma. In four of 35 patients (11%), an additional surgical treatment was necessary to address these pathologies: one reconstruction of the subscapular tendon, three tenodeses of the long head of the biceps, one removal of loose bodies and one abrasion chondroplasty.
Overall, 34 of 35 patients (97%) were satisfied with their results (Table 1). The mean satisfaction regarding the functional result was 1.6 out of 5. The cosmetic result was evaluated to be 1.9 out of 5. All patients reached a full range of motion. The subjective shoulder value (SSV) averaged at 90% (75–100%). The Constant score was good or excellent in 91% of the patients with a mean of 90 ± 10 points (range, 53–100). The Taft score averaged at 11 ± 1 points (range, 7–12) and the ACJI score at 78 ± 18 points (range, 23–100). AC joint specific scores as Taft score (p = 0.006) and ACJI score (p = 0.026) showed significantly better results for type Rockwood III-B than type V lesions. Analysing the subgroups for the Taft score and ACJI score for both, mainly the radiological results, were responsible for the difference in both groups (Taft score: objective parameters: p = 0.68; subjective parameters: 0.20; radiographic parameters: p = 0.056. ACJI score: pain: p = 0.14; activities of daily living: p = 0.63; cosmesis: p = 0.02; function: p = 0.67; radiographs: p = 0.01).
The CC distance improved significantly from 22 mm preoperatively (range, 16–30 mm) to 10 mm postoperatively (range, 3–15 mm) (p < 0.0001) (Table 2). Comparing the postoperative result to the contralateral side with a CC distance of 10 mm (range, 6–13 mm) no statistically significant difference was observed (p = 0.103). However, the Rockwood type III-B group showed an over-reduction regarding the postoperative CC distance (p = 0.0081). At the follow-up, the CC distance increased to 13 mm (range, 8–18). This resulted in a p value of 0.0001 compared to the contralateral side. The subgroup analysis showed no difference for the Rockwood type III-B group (12 mm; range, 8–15 mm; p = 0.409), but for the Rockwood type V group (14 mm; range, 9–18; p < 0.0001) compared to the contralateral side at the follow-up.
At the time of follow-up, four patients had a horizontal instability in the clinical examination. Three of the 29 patients (10%), who were evaluated radiologically, showed a horizontal instability in the Alexander view. The widest diameter of the clavicular drill hole was 7 ± 2 mm (range, 4–13 mm). No migration of the clavicular or coracoidal button was observed. Fourteen of 29 patients (48%) had an ossification within the area of the CC ligaments.
Discussion
The purpose of this study was to demonstrate sufficient AC joint stabilisation with a single tunnel reconstruction using a second generation implant in high-grade AC joint dislocations. Moreover, an additional, minimally invasive AC joint augmentation was expected to improve horizontal stability. Our data showed a high patient satisfaction (97%) with a SSV of 90%. The functional results were good to excellent regarding a Constant score of 90 points, Taft score of 11 points and ACJI score of 78 points. Due to the increased contact area of the second-generation implant, no migration of the clavicular or coracoidal buttons was observed. Furthermore, additional AC cerclage improved horizontal stability, as observed clinically and radiologically compared to preoperative state. The radiological evaluation showed a slight loss of vertical reduction over time (Fig. 2). This might result out of an elongation of the flip button device or a suture failure. Although the functional result was not influenced by this loss of reduction in the mid-term follow-up, some initial over-reduction or the use of a more stable construct for the CC stabilisation needs to be considered evaluating this technique.
Although there is no hard evidence in the literature, low-grade AC joint dislocations, type Rockwood I and II, are typically treated non-operatively [20]. The treatment for Rockwood type III lesions is still controversial. Young patients with aspirations of high functionality or workers who regularly do heavy lifting are more likely to be treated operatively. Furthermore, the Rockwood classification was extended in 2014. Type III lesions were sub-classified as type III-A and III-B [14, 21]. Besides the vertical instability, type III-A lesions were defined as horizontally stable, while type III-B lesions show a dynamic horizontal instability. An additional horizontal instability in the Alexander view was identified as a negative predictor for inferior functional results [5]. While indication for surgery is commonly accepted in type V lesion, type III lesions are still discussed. In countries like the US type III dislocations are initially treated non-operatively and surgery is only pursued after failure. Since allografts are not as easily available for us as in the US and horizontal instabilities are identified as negative outcome predictors, we differentiate between type III-A and III-B lesion with type III-B lesions being indication for surgery.
For the treatment of high-grade AC joint instabilities, the temporary hook-plate stabilisation and arthroscopic-assisted CC stabilisation are competing treatments. Mostly retrospective studies or meta-analyses showed comparable results in regard to functional results, complication rates and loss of reduction [6, 22,23,24,25]. Stein el al. were the first to compare those treatments prospectively with partially being randomised (64%), and 36% being treated by patient selection [26]. Their data showed significantly better results regarding the clinical scores for the arthroscopically assisted CC stabilisation. Further benefits from the arthroscopic treatment are the detection of concomitant glenohumeral pathologies, which are identified in up to 53% of the patients, with the rotator cuff or the bicep tendon complex being the most common and 12% requiring additional repair procedures [27,28,29]. Furthermore, this minimally invasive technique improves cosmetics and does not require a revision surgery for hardware removal. Therefore, the arthroscopic-assisted techniques are growing in volume.
In the scientific literature, arthroscopic-assisted techniques yield good to excellent results. Scheibel et al. [5] evaluated 28 patients treated with a double TightRope of the first generation without additional acromioclavicular cerclage. Clinical results averaged at a Constant score of 92 points, Taft score of 11 points and ACIJ score of 80 points. The range of motion did not differ from the contralateral side with a mean flexion of 179° and abduction of 178°. Patient satisfaction was high with a SSV of 95%. These results were comparable to our findings. The radiological evaluation showed a good postoperative reduction, comparing both shoulders with a CC difference of 0.5 mm (range, − 3 to 3 mm). Nonetheless, the CC distance increased at the operated side from 9 postoperatively to 10 mm after 3 months, 13 mm after 6 months and 14 mm at the final follow-up, which differed significantly compared to the uninjured side. Furthermore, 43% of the patients were evaluated as horizontally unstable in the Alexander view at follow-up. Patients with a stable situation achieved superior clinical results in all evaluated scores. We observed a comparable increase in the CC distance over time with the single tunnel technique. AC joint specific scores, as the Taft score or ACJI score, include a radiological evaluation. Due to the increase in the CC distance with time, an initial over-reduction resulted in significantly better results at follow-up than an initially optimal reduction in those scores. Since the Constant score as a clinical parameter and the subjective results were not influenced by this elevation of the clavicle in either case, the radiological evaluation might be overvalued in those scores.
Furthermore, Scheibel et al. [5] concluded that their technique needs further improvement due to a high rate of horizontal instabilities, which were associated with inferior results. The biomechanical testing by Saier et al. [9] showed that besides CC reconstruction, an additional AC-joint augmentation assures an adequate horizontal stability. Dyrna et al. [30] evaluated different techniques for an additional AC augmentation to restore stability against posterior rotational forces and horizontal translation. All five tested techniques (anterior, posterior, superior, O-frame, X-frame) restored stability regarding translation and rotation, which was comparable to the native states. However, none of the five tested techniques was superior over another. Based on the biomechanical findings of Theopold et al., [31] a CC reconstruction with a double tunnel technique both with or without additional AC augmentation showed significantly higher stability regarding the horizontal plane compared to a single tunnel technique with AC augmentation. Furthermore, double tunnel techniques with and without AC augmentation showed comparable horizontal stability. Therefore, in contrast to the previous mentioned literature, the authors questioned the effect of an additional AC augmentation at least for double tunnel techniques.
Multiple studies evaluated the clinical results of arthroscopically assisted CC stabilisation in acute AC joint dislocations. Some authors recommend a double tunnel technique to “anatomically” replace the CC ligaments [4, 26, 32, 33]. Although good to excellent clinical results are documented, the risk for clavicle or coracoid fractures is increased [34, 35], which can be reduced by using a single tunnel technique [36,37,38,39]. Furthermore, a “truly anatomical” reconstruction of the CC ligaments, using a collinear drilling technique for both ligaments, is simply not possible, which has been shown in several cadaveric and virtual 3D-CT scan-based studies [40,41,42]. Despite good to excellent clinical results, some patients fail or the outcome is unsatisfying. A persisting horizontal instability might be one reason [5]. Biomechanical studies prove an increase in horizontal stability by using an additional AC cerclage [9, 30]. So far, there are only two studies evaluating the clinical effect of an additional AC cerclage. A prospective multicentre study for chronic AC joint dislocations found an additional AC stabilisation as a favourable prognostic factor [43]. In contrast to our treatment 92% of those patients were treated with a double button technique and 88% were reinforced with a tendon graft due to the chronic situation. Furthermore, Hann et al. evaluated an AC joint stabilisation with a second-generation double TightRope and AC cerclage, which reduced dynamic horizontal instability. Our study is the first to evaluate the clinical and radiological results of a second generation single TightRope with additional AC augmentation. Comparable to Hann et al., our data showed an improved horizontal stability.
Limitations of our study are the retrospective design, small number of patients, although it is comparable to other clinical studies, and the lack of a comparative group.
In conclusion, the treatment of acute high-grade AC joint dislocation, using a second generation implant, results in good to excellent clinical results with high patient satisfaction. The additional AC augmentation improved stability in horizontal instable AC joints and is recommended in all high-grade AC joint stabilisations. Nonetheless, reduction was slightly lost over time due to an elongation or suture failure of the coracoclavicular single TightRope, which did not influence the clinical outcome. Nonetheless, some over-reduction or the use of a more stable construct, e.g. using two FiberTapes, needs to be considered for further treatment.
Data availability
The data that support the findings of this study are available from the corresponding author, [G.J.] upon reasonable request.
References
Mazzocca AD, Arciero RA, Bicos J (2007) Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med 35:316–329. https://doi.org/10.1177/0363546506298022
Beitzel K, Cote MP, Apostolakos J et al (2013) Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy 29:387–397. https://doi.org/10.1016/j.arthro.2012.11.023
Balke M, Schneider MM, Shafizadeh S et al (2015) Current state of treatment of acute acromioclavicular joint injuries in Germany: is there a difference between specialists and non-specialists? A survey of German trauma and orthopaedic departments. Knee Surg Sport Traumatol Arthrosc 23:1447–1452. https://doi.org/10.1007/s00167-013-2795-2
Venjakob AJ, Salzmann GM, Gabel F et al (2013) Arthroscopically assisted 2-bundle anatomic reduction of acute acromioclavicular joint separations: 58-month findings. Am J Sports Med 41:615–621. https://doi.org/10.1177/0363546512473438
Scheibel M, Dröschel S, Gerhardt C, Kraus N (2011) Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med 39:1507–1516. https://doi.org/10.1177/0363546511399379
Jensen G, Katthagen JC, Alvarado LE et al (2014) Has the arthroscopically assisted reduction of acute AC joint separations with the double tight-rope technique advantages over the clavicular hook plate fixation? Knee Surg Sport Traumatol Arthrosc 22:422–430. https://doi.org/10.1007/s00167-012-2270-5
Patzer T, Clauss C, Kühne C, a, et al (2013) Arthroscopically assisted reduction of acute acromioclavicular joint separations: comparison of clinical and radiological results of single versus double TightRope™ technique. Unfallchirurg 116:442–450
Schliemann B, Roßlenbroich SB, Schneider KN et al (2015) Why does minimally invasive coracoclavicular ligament reconstruction using a flip button repair technique fail? An analysis of risk factors and complications. Knee Surg Sport Traumatol Arthrosc 23:1419–1425. https://doi.org/10.1007/s00167-013-2737-z
Saier T, Venjakob AJ, Minzlaff P et al (2015) Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: a biomechanical study. Knee Surg Sport Traumatol Arthrosc 23:1498–1505. https://doi.org/10.1007/s00167-014-2895-7
Klimkiewicz JJ, Williams GR, Sher JS et al (1999) The acromioclavicular capsule as a restraint to posterior translation of the clavicle: a biomechanical analysis. J Shoulder Elbow Surg 8:119–124
Jensen G, Katthagen JC, Alvarado L et al (2013) Arthroscopically assisted stabilization of chronic AC-joint instabilities in GraftRope™ technique with an additive horizontal tendon augmentation. Arch Orthop Trauma Surg 133:841–851. https://doi.org/10.1007/s00402-013-1745-2
Alexander O (1949) Dislocation of the acromioclavicular joint. Radiography 15:260
Rockwood CJ (1984) Injuries in the acromioclavicular joint – subluxations and dislocations about the shoulder. In: Rockwood CJ, Green D (eds) Fractures in adults. Lippincott, Philadelphia, pp 890–910
Beitzel K, Mazzocca AD, Bak K et al (2014) ISAKOS upper extremity committee consensus statement on the need for diversification of the rockwood classification for acromioclavicular joint injuries. Arthroscopy 30:271–278. https://doi.org/10.1016/j.arthro.2013.11.005
Fuchs B, Jost B, Gerber C (2000) Posterior-inferior capsular shift for the treatment of recurrent, voluntary posterior subluxation of the shoulder. J Bone Joint Surg Am 82:16–25
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Taft TN, Wilson FC, Oglesby JW (1987) Dislocation of the acromioclavicular joint. An end-result study of the Acromioclavicular. J Bone Joint Surg Am 69:1045–1051
Irlenbusch U (2012) Examination techniques of the shoulder - expert’s evaluation based on literature analysis. Obere Extrem 7:61
Jensen G, Katthagen C, Voigt C, Lill H (2014) Arthroscopically assisted treatment of lateral clavicular fractures and acute instability of the acromioclavicular joint. Arthroskopie 27:255–264. https://doi.org/10.1007/s00142-014-0842-8
Pogorzelski J, Fritz EM, Godin JA et al (2018) Nonoperative treatment of five common shoulder injuries: a critical analysis. Obere Extrem 13:89–97. https://doi.org/10.1007/s11678-018-0449-1
Kraus N, Hann C, Gerhardt C, Scheibel M (2018) Dynamic instability of the acromioclavicular joint: a new classification for acute AC joint separation. Obere Extrem 13:279–285. https://doi.org/10.1007/s11678-018-0469-x
Helfen T, Siebenbürger G, Ockert B, Haasters F (2015) Therapy of acute acromioclavicular joint instability. Meta-analysis of arthroscopic/minimally invasive versus open procedures. Unfallchirurg 118:415–426. https://doi.org/10.1007/s00113-015-0005-z
Gowd AK, Liu JN, Cabarcas BC et al (2019) Current concepts in the operative management of acromioclavicular dislocations: a systematic review and meta-analysis of operative techniques. Am J Sports Med 47:2745–3758. https://doi.org/10.1177/0363546518795147
Metzlaff S, Rosslenbroich S, Forkel PH et al (2016) Surgical treatment of acute acromioclavicular joint dislocations: hook plate versus minimally invasive reconstruction. Knee Surg Sport Traumatol Arthrosc 24:1972–1978. https://doi.org/10.1007/s00167-014-3294-9
Andreani L, Bonicoli E, Parchi P et al (2014) Acromio-clavicular repair using two different techniques. Eur J Orthop Surg Traumatol 24:237–242. https://doi.org/10.1007/s00590-013-1186-1
Stein T, Müller D, Blank M et al (2018) Stabilization of acute high-grade acromioclavicular joint separation: a prospective assessment of the clavicular hook plate versus the double double-button suture procedure. Am J Sports Med 46:2725–2734. https://doi.org/10.1177/0363546518788355
Pauly S, Kraus N, Greiner S, Scheibel M (2013) Prevalence and pattern of glenohumeral injuries among acute high-grade acromioclavicular joint instabilities. J Shoulder Elbow Surg 22:760–766. https://doi.org/10.1016/j.jse.2012.08.016
Jensen G, Millett PJ, Tahal DS et al (2017) Concomitant glenohumeral pathologies associated with acute and chronic grade III and grade V acromioclavicular joint injuries. Int Orthop 41:1633–1640. https://doi.org/10.1007/s00264-017-3469-3
Arrigoni P, Brady PC, Zottarelli L et al (2014) Associated lesions requiring additional surgical treatment in grade 3 acromioclavicular joint dislocations. Arthroscopy 30:6–10. https://doi.org/10.1016/j.arthro.2013.10.006
Dyrna F, Imhoff FB, Haller B et al (2018) Primary stability of an acromioclavicular joint repair is affected by the type of additional reconstruction of the acromioclavicular capsule. Am J Sports Med 46:3471–3479. https://doi.org/10.1177/0363546518807908
Theopold J, Schöbel T, Fischer J-P et al (2019) Acromioclavicular joint reconstruction: an additional acromioclavicular cerclage does not improve horizontal stability in double coraco-clavicular tunnel technique. Knee Surg Sport Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05674-1
Salzmann GM, Walz L, Buchmann S et al (2010) Arthroscopically assisted 2-bundle anatomical reduction of acute acromioclavicular joint separations. Am J Sports Med 38:1179–1187. https://doi.org/10.1177/0363546509355645
Hann C, Kraus N, Minkus M et al (2018) Combined arthroscopically assisted coraco- and acromioclavicular stabilization of acute high-grade acromioclavicular joint separations. Knee Surg Sport Traumatol Arthrosc 26:212–220. https://doi.org/10.1007/s00167-017-4643-2
Martetschläger F, Horan MP, Warth RJ, Millett PJ (2013) Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med 41:2896–2903. https://doi.org/10.1177/0363546513502459
Milewski MD, Tompkins M, Giugale JM et al (2012) Complications related to anatomic reconstruction of the coracoclavicular ligaments. Am J Sport Meds 40:1628–1634. https://doi.org/10.1177/0363546512445273
Banffy MB, van Eck CF, ElAttrache NS (2018) Clinical outcomes of a single-tunnel technique for coracoclavicular and acromioclavicular ligament reconstruction. J Shoulder Elbow Surg 27:S70–S75. https://doi.org/10.1016/j.jse.2017.11.032
Flinkkilä TE, Ihanainen E (2014) Results of arthroscopy-assisted tightrope repair of acromioclavicular dislocations. Shoulder Elbow 6:18–22. https://doi.org/10.1111/sae.12040
Fahmy FS, Fathi H, ElAttar M (2019) Clinical outcomes of arthroscopic assissted fixation of acute high grade acromioclavicular joint disruption. J Orthop 16:133–136. https://doi.org/10.1016/j.jor.2019.02.005
Rosslenbroich SB, Schliemann B, Schneider KN et al (2015) Minimally invasive coracoclavicular ligament reconstruction with a flip-button technique (MINAR): clinical and radiological midterm results. Am J Sports Med 43:1751–1757. https://doi.org/10.1177/0363546515579179
Coale RM, Hollister SJ, Dines JS et al (2013) Anatomic considerations of transclavicular-transcoracoid drilling for coracoclavicular ligament reconstruction. J Shoulder Elbow Surg 22:137–144. https://doi.org/10.1016/j.jse.2011.12.008
Koh KH, Shon MS, Choi NH, Lim TK (2018) Anatomic tunnel placement is not feasible by transclavicular-transcoracoid drilling technique for coracoclavicular reconstruction: a cadaveric study. Arthroscopy 34:2012–2017. https://doi.org/10.1016/j.arthro.2018.01.028
Xue C, Zhang M, Zheng T-S et al (2013) Clavicle and coracoid process drilling technique for truly anatomic coracoclavicular ligament reconstruction. Injury 44:1314–1320. https://doi.org/10.1016/j.injury.2013.06.022
Barth J, Duparc F, Baverel L et al (2015) Prognostic factors to succeed in surgical treatment of chronic acromioclavicular dislocations. Orthop Traumatol Surg Res 101:S305–S311. https://doi.org/10.1016/j.otsr.2015.09.002
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
AE, GJ, JCK and R-ODH were responsible for conception and design of the study. AE, GJ, R-ODH and JCK were responsible for analysis and interpretation of data. AE and GJ drafted the article. HL, MA, KS, AE, GJ, JCK and R-ODH were responsible for final approval of the version to be submitted. MA and KS were responsible for acquisition of data. JCK, R-ODH and HL were responsible for revising the article critically for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
Helmut Lill is consultant for Arthrex. Jan Christoph Katthagen and Alexander Ellwein received speaker’s honorarium from Arthrex. All other authors declared that they have no conflict of interest.
Consent for publication
All patients signed informed consent regarding publishing their data.
Consent to participate
All patients approved the study with written informed consent.
Ethical approval
The study was performed in accordance with the ethical standards of the local ethics committee (Ethikkommission der MHH, No 1207–2011) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jensen, G., Dey Hazra, RO., Al-Ibadi, M. et al. Arthroscopically assisted single tunnel reconstruction for acute high-grade acromioclavicular joint dislocation with an additional acromioclavicular joint cerclage. Eur J Orthop Surg Traumatol 33, 1185–1192 (2023). https://doi.org/10.1007/s00590-022-03271-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03271-6