Abstract
Purpose
Optimal treatment of chronic unstable acromioclavicular (AC) joint dislocations (stage 3–5 according the Rockwood classification) is still debated. Anatomic coracoclavicular (CC) reconstruction is a reliable option in terms of two-dimensional radiographic reduction, clinical outcomes, and return to sports, but there remain concerns regarding anterior–posterior stability of the AC joint with CC ligament reconstruction alone. The aim of the present study was to describe the mid-term results of a new hybrid technique with CC and AC ligament reconstruction for chronic AC joint dislocations.
Methods
Twenty-two patients surgically treated for chronic AC joint dislocations (grade 3 to 5) were retrospectively reviewed. All patients were assessed before surgery and at final follow-up with the Constant–Murley score (CMS) and the American Shoulder and Elbow Surgeons (ASES) score. The CC vertical distance (CCD) and the CCD ratio (affected side compared to unaffected side) were measured on Zanca radiographs preoperatively, at 6 months postop and at final follow-up. The same surgical technique consisting in a primary fixation with a suspensory system, coracoclavicular ligaments reconstruction with a double loop of autologous gracilis and acromioclavicular ligaments reconstruction with autologous coracoacromial ligament was performed in all cases.
Results
Twenty-two shoulders in 22 patients (19 males and 3 females) were evaluated with a mean age of 34.4 ± 9 years at the time of surgery. The mean interval between the injury and surgery was 53.4 ± 36.7 days. The mean duration of postoperative follow-up was 49.9 ± 11.8 months. According to the Rockwood classification, there were 5 (22.6%) type-III and 17 (77.2%) type-V dislocations. Mean preoperative ASES and CMS were 54.4 ± 7.6 and 64.6 ± 7.2, respectively. They improved to 91.8 ± 2.3 (p = 0.0001) and 95.2 ± 3.1 (p = 0.0001), respectively at final FU. The mean preoperative CCD was 22.4 ± 3.2 mm while the mean CCD ratio was 2.1 ± 0.1. At final FU, the mean CCD was 11.9 ± 1.4 mm (p = 0.002) and the mean CCD ratio was 1.1 ± 0.1 (p = 0.009). No recurrence of instability was observed. One patient developed a local infection and four patients referred some shoulder discomfort. Heterotopic ossifications were observed in three patients.
Conclusions
The optimal treatment of chronic high-grade AC joint dislocations requires superior–inferior and anterior–posterior stability to ensure good clinical outcomes and return to overhead activities or sports. The present hybrid technique of AC and CC ligaments reconstruction showed good clinical and radiographic results and is a reliable an alternative to other reported techniques.
Level of evidence
Level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acromioclavicular (AC) joint dislocation is one of the most common shoulder injuries in the young athletic population, with an overall reported incidence of 9% to 12% [1,2,3,4]. The more severe injuries, grade 4 to 6 according to the Rockwood classification, are generally managed surgically, while grade 3 injuries have evolving surgical indications [5].
Soft tissue surgery aims to recreate the function of the disrupted coracoclavicular (CC) and AC ligaments. These include ligamentoplasty procedures, muscle transfers, and ligament reconstruction with autologous, allogeneic, or synthetic grafts [6].
Timing is important to achieve biologic healing of the disrupted tissues. Acute repair is defined as within 3 weeks from the date of injury [7]; in such a situation, AC joint stabilisation allows healing of the CC and AC ligaments, thus ensuring favourable functional outcomes [1]. Beyond this limit, biologic healing cannot be expected and reconstructive surgery with biologic augmentation should be performed in chronic symptomatic patients [8].
The use of biologic grafts to stabilise the AC joint was first reported by Jones et al. who used an autogenous semitendinosus tendon graft [9]. In 2010, Carofino and Mazzocca described their technique for anatomic AC joint reconstruction with a semitendinosus allograft [10]. This procedure aimed at restoring both the conoid and trapezoid ligaments at their anatomical attachment sites through double tunnels in the clavicle to address instability of the AC joint in both vertical and horizontal planes. Subsequently, the other authors modified this technique to achieve anatomic reconstruction of CC and AC ligaments [11, 12]. Ultimately, more than 160 surgical techniques have been described so far, indicating that no gold standard has yet emerged. Aim of the present study is to describe the efficacy of a new technique for anatomic CC and AC ligaments reconstruction in chronic AC joint dislocations.
The hypothesis of the study was that the present technique was effective in achieving stable joint reduction and good functional results in patients with chronic symptomatic AC joint dislocations.
Materials and methods
The present study was designed as a retrospective study without control group performed on prospectively collected data. The local institutional review board approved the study protocol (IRB NO:M26 15.02.2019).
Patients
A consecutive series of patients operated for AC joint dislocation were enrolled for the present study. Inclusion criteria were: chronic AC joint dislocation (grade 3 to 5 according to Rockwood) surgically treated for persistent pain and functional impairment after at least 2 months of conservative treatment, surgical treatment performed using the index procedure under investigation, and minimum 2-year follow-up. Exclusion criteria were: previous surgeries and/or fractures on the affected limb, and concomitant or previous untreated rotator cuff tears (preoperative shoulder ultrasound was performed in all cases).
Surgical procedure
The procedure was performed under general anaesthesia in the beach chair position by a single shoulder surgeon. Gracilis tendon autograft was harvested through a small longitudinal incision with a non-sterile tourniquet positioned at the proximal thigh. The graft was prepared and tubularised at the two free ends with #2 Vicryl sutures. Local infiltration with tranexamic acid (1 gr) was used in all cases at the autograft donor site. The skin incision was closed with absorbable sutures or fibrin glue. Attention was then turned to the AC joint reconstruction. A slightly oblique incision started just lateral to the AC joint and run distally and medially over the coracoid process.
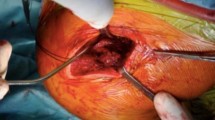
The deltotrapezial fascia was identified and incised horizontally, between the trapezius insertion onto the posterior aspect of the clavicle and the deltoid origin on the anterior clavicle, to expose the distal clavicle. The AC joint was identified and opened; scar tissue removed. The coracoid was reached through a deltoid split along the residual CC. Once identified, the coracoacromial (CA) ligament was detached from the lateral aspect of the coracoid taking care of preserving all its length until its acromial insertion. The CA ligament was then tubularised with #2 Vicryl suture. The tubularised CA ligament was ultimately utilised as local autograft for AC ligament reconstruction (Fig. 1).
The clavicle was prepared to have complete exposition of its anterior ant posterior margins. A 4-mm tunnel was drilled almost vertical from the clavicle to match with the coracoid process. The tunnel was performed around 20 mm from the lateral aspect of the clavicle and right in the middle of the anterior–posterior width of the clavicle. The coracoid tunnel was performed just distal to its knee, and right in the middle of the coracoid width. In some cases, when it was not possible with the dedicated instrumentations, the two tunnels were drilled independently to achieve the desired position. Both the clavicle and the coracoid were prepared to a suspensory fixation device (Tightrope; Arthrex, Naples, FL, USA). A double shuttle with #2 Vicryl was passed below the coracoid with a curved hook from the medial aspect of the coracoid and retrieved laterally. The gracilis tendon autograft was then passed under the coracoid process from medial to lateral. The medial end was passed over the clavicle from posterior to anterior. Conversely, the lateral end of the gracilis autograft was passed around the clavicle from the anterior aspect in a figure-of-eight configuration. This configuration allows the graft to be crossed in its passage from the coracoid to the clavicle. The length of the graft allowed for an almost complete double looping in all patients. This resulted in a double loop of at least 5 mm in diameter. The AC joint was reduced under direct visualisation using the Tightrope system by pushing downward the clavicle (Arthrex, Naples, FL, USA) (Fig. 2). The free ends of the gracilis autograft were pulled together and sutured to the underlying loop with #2 Vicryl stitches (Fig. 3).
The articular cartilage of the distal clavicle was removed, and two small tunnels were drilled obliquely (from inferior and lateral to superior and medial) with a 1.4 mm K-wire. The sutures from the CA ligament were passed into the small tunnels and tied together (Fig. 4).
Finally, the deltotrapezial fascia was closed to reinforce the AC joint stability. Local infiltration with tranexamic acid (2 gr) was used in all cases.
The patients wore a sling for 6 weeks postoperatively. Gradual recovery of the passive range of motion (ROM) was then initiated and continued until full passive elevation was achieved. Active ROM and muscle strengthening exercises were allowed once the passive ROM was fully recovered to avoid scapula-thoracic imbalance. Return to sports was allowed 6 months after surgery following a radiographic and clinical assessment.
Outcome measurements
All patients were routinely assessed as per standard protocol of our institution preoperatively and at final follow-up. Primary outcome measure was the American Shoulder and Elbow Surgeons (ASES) score. Secondary outcomes included the Constant–Murley score (CMS) and the radiographic evaluation of AC joint dislocation.
Radiographic assessment was performed on Zanca views as per standard protocol of our institution preoperatively, at 6 months postoperatively and at final follow-up. Measurements were carried out on digital X-rays using a DICOM medical image viewer (Horos Project; Purview, Annapolis, MD, USA). Vertical displacement of the AC joint was estimated by measuring the coracoclavicular distance (CCD), which is the distance between the superior border of the coracoid process and the inferior clavicular surface. The displacement was then calculated as a ratio between the CCD of the healthy side and the CCD of the affected side (CCD ratio). The CCD and CCD ratio were considered as secondary outcome measures. Intraoperative and postoperative complications and return to sports activities were also recorded. All data were retrieved retrospectively from the electronic charts and images available on the database of the hospital.
Statistical analysis
Statistical analysis was performed using statistical software (SPSS v24.0; IBM, Armonk, NY, USA). Data were assessed for normal distribution by use of the Kolmogorov–Smirnov test. Continuous variables were expressed by mean ± standard deviation (SD) for normally distributed data, otherwise median and range were used. Categorical variables were expressed as frequencies and percentages. Significance tests were run to analyse differences between pre- and postoperative clinical data. A paired t-test was used for normally distributed data, otherwise the Wilcoxon signed-rank test was considered. For radiographic measurements, repeated measures ANOVA was used to assess within-group differences across repeated observations. Alternatively, Friedman test was considered for non-normally distributed data. Repeated paired t-test or Wilcoxon signed-rank tests were run for multiple pairwise comparisons to assess differences between time intervals. Significance was considered for p value < 0.05.
Sample size was calculated according to the primary outcome. Since no current metrics are available to estimate clinical relevance of change in the ASES score for patients with AC joint injuries, we based our calculation on a previous study by Muench et al. [13], which was similar to the present one for study population, intervention and outcome measures and we accepted as minimal clinically important difference (MCID) an 11-point change in the ASES score. According to Muench et al. [13], preoperative mean ASES score was 52.1 ± 19.9. On considering 11-point difference from preoperative ASES score as MCID an effect size of 0.55 was obtained and sample size was then estimated to be 22, given alpha equal to 0.05 and power of 80%.
Results
Twenty-two patients were selected from a consecutive series of patients operated with the index procedure according to eligibility criteria. Flowchart of the study is reported in Fig. 5. Descriptive statistics for baseline characteristics is reported in Table 1. The mean duration of postoperative follow-up was 49.9 ± 11.8 months (range, 26–64 months). Clinical and radiographic results are summarised in Table 2.
There was a significant improvement in ASES score and CMS from preoperative to final follow-up. (p = 0.0001 and 0.0001, respectively). In addition, radiographic outcomes showed a significant improvement from baseline values. At 6-month follow-up, a significant reduction in CCD distance and CCD ratio was observed (p = 0.001 and 0.001, respectively). At final follow-up, a small increase in CCD and CCD ratio was observed when compared to 6-month follow-up, albeit the difference was not significant (p = 0.86 and 0.11, respectively), and they were both significantly reduced respect to preoperative values (p = 0.002 and 0.009, respectively). No difference in CCD was observed on the healthy side from preoperative value (10.2 ± 3.3) to final FU (10.3 ± 3.2) (n.s.). Nineteen out of 22 patients (86%) returned to their sport activities at the same level.
No intraoperative complications were recorded. One patient (4.5%) had a local infection, which developed in the early postoperative period (7 days after surgery) and required oral antibiotics to resolve. Radiographs showed heterotopic ossification around the CC ligaments in 3 (13.1%) cases. One of these patients (4.5%) showed additional cutout of the coracoid button while the reduction was stable. The button was stable on radiographs evaluations, the patient was not symptomatic, and therefore, it was not removed (Fig. 6).
Discussion
The most important finding in the present study is the good functional outcomes related to the technique of combined AC and CC ligament reconstruction for chronic AC joint dislocations.
There was a significant improvement of Constant and ASES scores at last FU (p = 0.0001 for both) and significant reduction of CCD and CCD ratio (p = 0.002 and 0.009, respectively). Moreover, 86% of patients returned to their sport activities at the same level. These outcomes are comparable to those of previous studies in literature. Carofino and Mazzocca reported the outcomes of their anatomic reconstruction in 16 patients at an average FU of 21 months [10]. At final FU, the mean ASES was 92 ± 5, SST 11.8 ± 4, CM 94.7 ± 5 and SANE score 94.4. Virtanen et al. reviewed 25 patients after a mean of 4.2 years after ligament reconstruction with autogenous semitendinosus and gracilis; mean CS was 83 and mean DASH was 14 [14]. In the past, the combination of coracoclavicular (CC) and acromioclavicular (AC), ligament reconstruction has become popular in the hope of decreasing complication rates and improving patient outcomes associated with non-anatomic repairs [15, 16]. The successful outcomes of anatomic CC ligament reconstruction rely on graft choice, bone tunnels and horizontal stability.
The hamstring tendons are the most used grafts; however, palmaris longus [17], flexor carpi radialis, peroneus longus [18] and tibialis anterior tendons [19] have been used as well. Gracilis tendon autograft was chosen because it has been demonstrated that isolated gracilis tendon harvesting is not associated with loss of strength in knee flexion, internal tibial rotation and thigh adduction [20]. In addition, preserving the native semitendinosus may be beneficial especially in young patients to keep a strong graft for any possible further surgeries. In the present series, gracilis had sufficient length to perform a double looping around clavicle and coracoid with at least 5 mm width in all patients. To protect the gracilis tendon autograft, which is less strong than semitendinosus, and allow its incorporation, the primary stabilisation of the AC joint was ensured with the Tightrope system (Arthrex, Naples, FL, USA).
Bone tunnels are the weak aspect of anatomic CC ligaments reconstruction with reported loss of reduction, fractures and hardware cutout. Martetschlager et al. reported an overall complication rate of 27% in patients after CC ligament reconstruction and no difference between cortical fixation versus tendon graft loop procedure [21]. Others have reported 80% complication rate, and 20% of coracoid fractures, when a tunnel is drilled into the coracoid compared to 35% complication rate when the graft is looped around the coracoid [22]. In the present study, one patient (4.5%) showed button cutout from the coracoid and no cases of clavicular or coracoid tunnel fracture. The risk of coracoid fracture can be mitigated by downsizing the diameter of the tunnel and improving accuracy its placement particularly in the centre–centre or medial–centre position of the coracoid [23]. Similar to coracoid fractures, multiple tunnel drilling in the clavicle also increases the risk of fractures [22, 24]. Minimising clavicular tunnel diameter as well as adequate tunnel spacing of 20 to 25 mm between clavicular tunnels and 10 to 15 mm between the lateral tunnel and the distal edge of the clavicle may reduce the incidence of clavicle fractures [10]. In the present hybrid technique, initial CC fixation was achieved with a Tightrope button (Arthrex, Naples, FL, USA) which required a 4 mm tunnel in the clavicle and coracoid. Biomechanical studies have shown that #5 FiberWire has a biomechanical strength of 485 N as compared to the native CC ligament complex of 589 N [25].
Another critical aspect of anatomic reconstructions is the restoration of horizontal stability. It is crucial to avoid posterior abutment of the clavicle and scapular spine, with significant clinical disability. The CC ligaments are the primary restraint to superior migration of the clavicle, with the conoid ligament providing around 60% of the strength in this direction [26]. Conversely, the superior AC ligament provides 56% of the resistance to posterior translation, and the posterior ligament contributes to 25% [26]. Dawson et al. confirmed the role of the AC ligaments (anterior, posterior, superior, and inferior) to confer three times more stability in the anteroposterior and torsional plane than in the superior-inferior plane [27]. These findings confirm that the horizontal stability is primarily mediated by the AC ligaments while vertical stability is primarily mediated by the CC ligaments [28]. It is, therefore, reasonable to incorporate surgical techniques to reconstruct both the CC and AC to improve horizontal stability of the AC joint, as clearly demonstrated in a biomechanical study by Dyrna et al. [29] and in several clinical studies [11, 18, 30]. In the present study, the coracoacromial (CA) ligament was used to reconstruct the AC ligaments, allografts were excluded for their costs and gracilis autograft, which was used as biologic augmentation for CC ligaments did not have enough length for the additional reconstruction of AC joint. CA ligament seemed ideal choice for several reasons.
Finally, the decision to retain the distal clavicle is somewhat controversial. Although it is considered a pain generator, historic and recent clinical studies have not shown clear clinical improvements after distal clavicle excision (DCE) [10]. In the present study, the cartilage layer of the distal clavicle was removed to achieve a bleeding surface to increase the healing of the transferred CA ligament.
The present technique is innovative since it is a reconstruction of both the coracoclavicular and acromioclavicular ligaments with potential positive effects on the horizontal stability. Second, the transposition of the coracoacromial ligament to reconstruct the acromioclavicular ligaments (with similar direction of the native ligament) improves the visualisation of the pericoracoid area, making it easier the passage of the gracilis tendon beneath the coracoid, and allows to use the gracilis tendon to reconstruct the coracoclavicular ligaments with a double figure 8 loop. The semitendinosus tendon is, therefore, left in place as a potential graft for further surgeries. Finally, the use of autologous gracilis reduces the costs on health system compared to allografts which is of great relevance in several countries. Beside these aspects, the present study has several limitations. First, the lack of a control group prevents from the precise efficacy of the modifications of the original technique. Second, the present cohort is homogenous but limited to 22 patients. Moreover, the length of the follow-up does not allow for definitive conclusion concerning the onset of degenerative changes to the AC joint.
Conclusions
The reported hybrid technique of AC and CC ligaments reconstruction is be an alternative to other reported techniques. Good clinical outcomes comparable to previous reports with no re-dislocations or clavicular and coracoid fractures were observed. One patient showed asymptomatic button cutout. Further biomechanical studies are required to assess the role of AC ligament transposition on the horizontal stability of the AC joint.
References
Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, Ziegler CG, Edgar CM, Imhoff AB, Arciero RA, Mazzocca AD (2013) Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy 29:387–397
Pallis M, Cameron KL, Svoboda SJ, Owens BD (2012) Epidemiology of acromioclavicular joint injury in young athletes. Am J Sports Med 40:2072–2077
Rothenberg A, Gasbarro G, Chlebeck J, Lin A (2017) The Coracoacromial Ligament: anatomy, follow-up function, and clinical significance. Orthop J Sports Med 5(4):2325967117703398
Skjaker SA, Enger M, Engebretsen L, Brox JI, Bøe B (2020) Young men in sports are at highest risk of acromioclavicular joint injuries: a prospective cohort study. Knee Surg Sports Traumatol Arthrosc 29(7):2039–2045
Frank RM, Cotter EJ, Leroux TS, Romeo AA (2019) Acromioclavicular Joint Injuries: evidence-based treatment. J Am Acad Orthop Surg 27(17):775–778
Zhu Y, Hsueh P, Zeng B, Chai Y, Zhang C, Chen Y, Wang Y, Maimaitiaili T (2018) A prospective study of coracoclavicular ligament reconstruction with autogenous peroneus longus tendon for acromioclavicular joint dislocations. J Shoulder Elbow Surg 27(6):178–188
Rosso C, Martetschläger F, Saccomanno MF, Voss A, Lacheta L, Beitzel K, Milano G (2021) High degree of consensus achieved regarding diagnosis and treatment of acromioclavicular joint instability among ESA-ESSKA members. Knee Surg Sports Traumatol Arthrosc 29(7):2325–2332
Sircana G, Saccomanno MF, Mocini F, Campana V, Messinese P, Monteleone A, Salvi A, Scaini A, Megaro A, Milano G (2020) Anatomic reconstruction of the acromioclavicular joint provides the best functional outcomes in the treatment of chronic instability. Knee Surg Sports Traumatol Arthrosc 29(7):2237–2248
Jones HP, Lemos MJ, Schepsis AA (2001) Salvage of failed acromioclavicular joint reconstruction using autogenous semitendinosus tendon from the knee. Surgical technique and case report. Am J Sports Med 29(2):234–237
Carofino BC, Mazzocca AD (2010) The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg 19:37–46
Kibler WB, Sciascia AD, Morris BJ, Dome D (2017) Treatment of symptomatic acromioclavicular joint instability by a docking technique: clinical indications, surgical technique, and outcomes. Arthroscopy 33(4):696–708
Saccomanno MF, Marchi G, Mocini F, Vismara V, Campana V, Salvi AG, Scaini A, Milano G (2020) Anatomic reconstruction of the coracoclavicular and acromioclavicular ligaments with semitendinosus tendon graft for the treatment of chronic acromioclavicular joint dislocation provides good clinical and radiological results. Knee Surg Sports Traumatol Arthrosc 29(7):2356–2363
Muench LN, Kia C, Jerliu A, Murphy M, Berthold DP, Cote MP, Arciero RA, Mazzocca AD (2019) Functional and radiographic outcomes after anatomic coracoclavicular ligament reconstruction for type III/V acromioclavicular joint injuries. Orthop J Sports Med 7(11):2325967119884539
Virtanen KJ, Savolainen V, Tulikoura I, Remes V, Haapamäki V, Pajarinen J, Björkenheim JM, Paavola M (2014) Surgical treatment of chronic acromioclavicular joint dislocation with autogenous tendon grafts. Springerplus 3:420. https://doi.org/10.1186/2193-1801-3-420
Huang FT, Lin KC, Lin CY, Chang WN (2021) Concomitant acromioclavicular and coracoclavicular ligament reconstruction with a duo-figure-8 autogenic graft wrapping technique for treating chronic acromioclavicular separation. Clin Orthop Surg 13(3):366–375
Xará-Leite F, Andrade R, Moreira PS, Coutinho L, Ayeni OR, Sevivas N, Espregueira- Mendes J (2019) Anatomic and non-anatomic reconstruction improves post-operative outcomes in chronic acromio-clavicular instability: a systematic review. Knee Surg Sports Traumatol Arthrosc 27(12):3779–3796
Kocaoglu B, Ulku TK, Gereli A, Karahan M, Turkmen M (2017) Palmaris longus tendon graft versus modified Weaver-Dunn procedure via dynamic button system for acromioclavicular joint reconstruction in chronic cases. J Shoulder Elbow Surg 26(9):1546–1552
Saier T, Venjakob AJ, Minzlaff P, Föhr P, Lindell F, Imhoff AB, Vogt S, Braun S (2015) Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 23(5):1498–1505
Lee B, Acevedo DC, Mirzayan R (2014) Reconstruction of the acromioclavicular joint, its superior capsule, and coracoclavicular ligaments using an interpositional acellular dermal matrix and tibialis tendon allograft. Tech Shoulder Elbow Surg 15(3):79–86
Flies A, Scheibel M, Kraus N, Kruppa P, Provencher MT, Becker R, Kopf S (2020) Isolated gracilis tendon harvesting is not associated with loss of strength and maintains good follow-up functional outcome. Knee Surg Sports Traumatol Arthrosc 28(2):637–644
Martetschlager F, Horan MP, Warth RJ, Millett PJ (2013) Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med 41:2896–2903
Milewski MD, Tompkins M, Giugale JM, Carson EW, Miller MD, Diduch DR (2012) Complications related to anatomic reconstruction of the coracoclavicular ligaments. Am J Sports Med 40:1628–1634
Ferreira JV, Chowaniec D, Obopilwe E, Nowak MD, Arciero RA, Mazzocca AD (2012) Biomechanical evaluation of effect of coracoid tunnel placement on load to failure of fixation during repair of acromioclavicular joint dislocations. Arthroscopy 28:1230–1236
Turman KA, Miller CD, Miller MD (2010) Clavicular fractures following coracoclavicular ligament reconstruction with tendon graft: a report of three cases. J Bone Joint Surg Am 92:1526–1532
Imhoff AB, Chernchujit B (2004) Arthroscopic anatomic stabilization of acromioclavicular joint dislocation. Oper Tech Sports Med 12:43–48
Fukuda K, Craig EV, An KN, Cofield RH, Chao EY (1986) Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am 68:434–440
Dawson PA, Adamson GJ, Pink MM et al (2009) Relative contribution of acromioclavicular joint capsule and coracoclavicular ligaments to acromioclavicular stability. J Shoulder Elbow Surg 18:237–244
Hislop P, Sakata K, Ackland DC, Gotmaker R, Evans MC (2019) Acromioclavicular joint stabilization: a biomechanical study of bidirectional stability and strength. Orthop J Sports Med 7(4):2325967119836751
Dyrna F, Imhoff FB, Haller B, Braun S, Obopilwe E, Apostolakos JM, Morikawa D, Imhoff AB, Mazzocca AD, Beitzel K (2018) Primary stability of an acromioclavicular joint repair Is affected by the type of additional reconstruction of the acromioclavicular capsule. Am J Sports Med 46(14):3471–3479
Barth J, Duparc F, Baverel L, Bahurel J, Toussaint B, Bertiaux S, Clavert P, Gastaud O, Brassart N, Beaudouin E, De Mourgues P, Berne D, Duport M, Najihi N, Boyer P, Faivre B, Meyer A, Nourissat G, Poulain S, Bruchou F, Ménard JF, d’Arthroscopie SF (2015) Prognostic factors to succeed in surgical treatment of chronic acromioclavicular dislocations. Orthop Traumatol Surg Res 101:S305-311
Acknowledgements
We gratefully thank Paola Santangelo for having supported us in the realisation of the drawings.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
All the authors listed above made a significant contribution to the study or manuscript completion.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was exempt from institutional approval.
Informed consent
Informed consent was collected from all included subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cerciello, S., Corona, K., Morris, B.J. et al. Hybrid coracoclavicular and acromioclavicular reconstruction in chronic acromioclavicular joint dislocations yields good functional and radiographic results. Knee Surg Sports Traumatol Arthrosc 30, 2084–2091 (2022). https://doi.org/10.1007/s00167-021-06790-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06790-7