Abstract
Study design
A retrospective, longitudinal cohort study.
Objective
The purpose of this study was to examine whether Hounsfield units (HUs), as an alternative bone mineral density measurement to dual-energy X-ray absorptiometry and quantitative computed tomography, which lead to additional radiation exposure for patients, has an effect on the maintenance of reduction in bisegmental Cobb angle (CA) and cage subsidence in patients who receive bisegmental spine stabilization after traumatic thoracolumbar spine fractures.
Methods
A total of 81 patients with a mean follow-up of 12 months were analyzed. CAs and cage subsidence were measured intraoperatively and at follow-up. HU was measured, and patients were subsequently assigned based on HU to three HU subgroups (group 1: HU < 110 [poor bone quality (BQ)]; group 2: HU 180–110 [diminished BQ]; group 3: HU > 180 [good BQ]).
Results
Following anterior stabilization, loss of reduction and cage subsidence differed between patients with poor and diminished BQ but not significantly, and both groups showed significantly more loss of reduction and cage subsidence than patients with good BQ.
Conclusion
BQ, estimated with HU, had significant effects on cage subsidence and loss of reduction. We recommend measuring HU before surgery and applying additional treatment strategies, such as polymethylmethacrylate augmentation of endplates or anterior plates, for patients with HU < 180.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aim of providing operative treatment for spinal injuries is to enable bony healing of the injured segment in a physiological position. Injuries of the thoracolumbar spine are often accompanied by an injury to at least one vertebral motion segment. The involvement of the functional spinal unit has implications for the treatment of spinal injuries. The multicentre study (MCSII) of the Spine Section of the German Orthopaedic and Trauma Society showed that better radiological results could be achieved via additional surgical treatment of the anterior column [1]. This finding was included in the Recommendations for the Treatment of Thoracolumbar and Lumbar Spine Injuries of the Spine Section of the German Orthopaedic and Trauma Society [2].
In addition to the qualities of the implant, bone quality (BQ) and thus the bone–implant interface are important factors in the stability of the surgically treated spinal segment [3]. A high bone mineral density (BMD) is correlated with a higher stiffness of the overall construct [4,5,6] and is relevant to cage subsidence for patients with posterior lumbar interbody fusion (PLIF) [7].
The gold standard for measuring BMD is dual-energy X-ray absorptiometry (DEXA) or quantitative computed tomography (qCT), but it can also be estimated using Hounsfield units (HUs) derived from standard multidetector CT (MDCT) [8,9,10,11].
The aim of this retrospective study was to examine whether HUs have an impact on the maintenance of reduction with respect to the bisegmental Cobb angle (CA) and cage subsidence in patients with bisegmental two-step spine stabilization after traumatic thoracolumbar spine fractures (TTSFs).
We proposed that a lower HU is associated with a greater loss of reduction and more cage subsidence.
Materials and methods
Study design
This study conducted a retrospective, longitudinal analysis using prospectively collected data from a single Level 1 trauma centre.
Patients
Eighty-one patients (age: 18–70 years, 59 male and 22 female) suffering from TTSF without known osteoporosis were included. (Further information is provided in Table 1.)
Treatment protocol
Patients who were considered for the study had received a posterior stabilization (first OP—posterior reduction and bisegmental instrumentation). Sixty-eight patients received posterior open spine surgery without a fusion graft, such as a bone graft or augmentation. USS® (Synthes, N = 62) and Krypton® (Ulrich, N = 6) implants were used. Thirteen patients received percutaneous posterior reduction and instrumentation with Viper® (polyaxial, DePuy Synthes).
Additive anterior stabilization (second OP—vertebral body replacement (VBR) and fusion with an expandable cage (VLIFT® Stryker) and cancellous bone grafting) after TTSF was performed for patients with a McCormack Index of 7 or higher [12] in A, B or C injury according to the AOSpine classification [13]. For the second surgery, the ventral VBR, the criteria were as follows: intravertebral disc herniation, disturbance of the disc, subsidence, vertebral pseudarthrosis and pain. The VBR device used had removable circular endplates with a diameter of 22 or 26 mm. To fit the cage to the vertebra, angulated cage endplates (3°, 8° and 15°) were used. The endplate preparation was performed very carefully under endoscopic or direct vision to avoid damaging the endplates.
The treatment protocol included an interval of approximately 3 months from posterior to anterior procedure. The aim of our clinical standard was to assess bony healing, disc status and patient symptoms after a time period of 3 months to evaluate indications for anterior stabilization and to maintain the option of posterior implant removal after healing.
Patients with fracture-related neurological deficits, known osteoporosis or ankylosing spinal disorders were excluded due to the differing requirements of operative treatments (e.g., augmentation, kyphoplasty or multi-level instrumentation), postoperative therapies and activities.
Cobb angle
The bisegmental CAs were recorded at two time points, intraoperatively (second OP, radiographs in lateral position) and at follow-up 12 months after the second OP (radiographs in supine position), see Fig. 1.
Bisegmental CA of two patients (top: age: 19, fractured vertebra: L1, AOSpine: A3, McCormack 7, HU: 98; bottom: age: 30, fractured vertebra: Th12, AOSpine: B2 A4, McCormack 8 HU: 199) at three time points: pre 2ndOP; 2nd OP and E) follow up of fractured L1 with AOSpine classification A3. The vertebras cover- and endplate of Th12 and L2 are marked with white lines, respectively. The bisegmental CA between these lines are given in the upper right corner for each time point. The physiological bisegmental CA for L1 is supposed with 0° and for Th12 with 5°
Kyphotic CAs are denoted as negative values and lordotic CAs as positive values. The ∂CA was further used to record the change in CA and was calculated as the difference between the intraoperative and follow-up results.
The presence of cage subsidence was recorded, and its value was measured in mm at follow-up. Specifically, we measured the maximum subsidence depth of the cage into the cranial and caudal vertebra on CT scans.
Bone quality
HU values were measured according to the preoperative CT of the vertebra to be instrumented. HU values reflect BQ with high accuracy, despite the use of different devices and CT protocols [7,8,9]. We measured HU according to Schreiber et al. [9] and Mi et al. [14]. The average HU value was measured in three axial planes of the vertebral body (VB). The mean HU of the largest possible region of interest, without including sclerotic or cortical structures, within the VB was measured by a experienced surgeon (BU). The mean value of the individual HU (three axial planes) values was calculated for each patient.
To better differentiate the effects of BQ, the total population was categorized into three HU subgroups depending on their HU values (group 1: HU ≤ 110, N = 10; group 2: HU > 110 and ≤ 180, N = 43; group 3: HU > 180, N = 28), as described by Schwaiger [15] and Pickhardt [8]. Changes in BMD during the investigation period and thus an associated loss of reduction or subsidence were not expected, because the BMD as measured by DEXA decreases by less than 1% annually [16]; thus, we would not expect changes in the HU given the correlation between HU and DEXA, as indicated by Lee et al. [17].
Statistical analysis
First, differences in BMI, AOSpine classification and fractured levels between the three HU subgroups were confirmed using univariate analysis of variance (ANOVA). Variables that significantly differed between HU subgroups were chosen as covariates in the subsequent analyses of covariance (ANCOVAs). Separate ANCOVAs were performed to analyze postoperative changes in CA and the extent of subsidence. To test whether the ratio of vertebra and cage endplates differed between the HU subgroups and whether this ratio was due to an effect on subsidence, one-factorial ANOVA and bivariate Pearson correlation were performed. Effect sizes were calculated as the squared partial eta (η 2 p ). Post hoc least significant difference (LSD) tests were also performed.
To detect HU-dependent general effects on the ∂CA and cage subsidence, the Pearson correlation coefficient was used. To confirm whether the level of reduction affected the extent of subsidence, Pearson correlation was performed. The significance level for all tests was set at a P of 0.05. SPSS 24 (SPSS Inc., Chicago IL) software was used for statistical analyses.
Results
An overview of our cohort (HU, age, sex, fractured VB, AOSpine classification, loss of reduction and cage subsidence) is provided in Table 1.
The univariate ANOVA showed significant differences between the HU subgroups in BMI (P = 0.014) and AOSpine classification (P = 0.015) but not fractured VB (P = 0.523). Thus, BMI and AOSpine classification were used as covariates in the ANCOVAs, but no significant effects (loss of reduction: BMI P = 0.592, AOSpine P = 0.414; subsidence: BMI P = 0.600, AOSpine: P = 0.294) were observed.
The ANCOVA for ∂CA showed significant effects for HU subgroups (P = 0.05, F2,79 = 3.121, η 2 p = 0.078). Pairwise comparisons showed a significantly higher loss of reduction for groups with poor and diminished BQ (group 1: P = 0.043, group 2: P = 0.028) than in the group with good BQ (group 3, Fig. 2). The loss of reduction did not significantly differ between group 1 and group 2 (P = 0.575). ANOVA was used to examine the effects of vertebral-to-cage endplate ratio on subsidence and showed no significant differences between the three HU subgroups nor for the cranial or caudal vertebral-to-cage endplate ratio (cranial: P = 0.69, F2,78 = 0.376; caudal: P = 0.78, F2,78 = 0.251). The Pearson correlation between the vertebral-to-cage endplate ratio and the amount of subsidence showed a significant correlation for the caudal endplates, with r = 0.307 (P < 0.01), but not for the cranial endplates (P = 0.07). With a r2 of 0.09, this correlation can be described as low.
The correlation between the amount of reduction and the extent of subsidence was assessed, and the Pearson correlation was not significant (P = 0.68).
For cage subsidence, the ANCOVA showed a significant effect for HU subgroups (P < 0.001, F2,80 = 10.721, η 2 p = 0.222). Pairwise comparisons showed a significantly higher cage subsidence for group 1 (P < 0.001) and group 2 (P < 0.001) than for group 3. Furthermore, group 1 and group 2 did not significantly differ (P = 0.287, Fig. 2). Overall, the frequency of cage subsidence at follow-up was 100, 90 and 70% in groups 1, 2 and 3, respectively (Table 1).
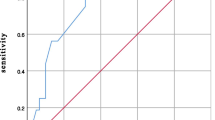
The Pearson correlation coefficient showed significant effects of HU on ∂CA (P = 0.018, r = 0.266) and cage subsidence (P < 0.001, r = − 0.412, Fig. 3).
Discussion
In this study, we showed that HU (derived from MDCT) had significant effects on cage subsidence and loss of reduction after a two-step posterior-anterior spinal stabilization for TTSFs. Loss of reduction and cage subsidence did not significantly differ between patients with poor and diminished BQ, but these patients presented a significantly greater loss of reduction and more frequent cage subsidence than patients with good BQ. These results were consistent with our hypotheses. Thus, the preoperative determination of bone quality assumes an important meaning also in the case of assumed good bone quality, because most of our patients had no good bone quality, even in patients were we expected good bone quality.
However, even patients with good BQ showed a loss of reduction and cage subsidence.
A significant difference in the loss of reduction was found between the HU subgroups after the second OP. Both group 1 (poor BQ) and group 2 (diminished BQ) had a significantly greater loss of reduction than group 3, which had HU values over 180.
Despite the use of expandable cages, which minimize the risk of cage subsidence due to the use of wedges between VBs and thus the improved/enlarged implant-to-bone contact [6, 18], we found cage subsidence in all HU subgroups in an unexpected percentage of patients when compared with the results obtained by Spiegl et al. [19]. This finding warrants further examination. One reason may be alterations in endplates despite the careful preparation. Assuming that reduced BQ increases the risk of altering the endplates during preparation, low BQ may be an explanation for the high frequency of intraoperative cage subsidence. In addition, we had no “force control” for cage expansion. It would be desirable to have cages with “force control” and referential values for expansion power.
Consistent with the loss of reduction due to HU, we found significant differences between HU subgroups in cage subsidence. Even in group 3 (with good BQ), we found 70% cage subsidence. This finding led us to the assumption that the VBR device we used was unable to maintain reduction as a stand-alone technique for cases of diminished and poor BQ. We did not find screw loosening in any of our patients.
One reason for the loss of reduction and the progression in subsidence over time could be an excessive (over-) correction during the second surgery, with the reduction compensating over time. We could not show a correlation in our patients between the amount of reduction and the extent of subsidence. The amount of reduction did not differ between the HU subgroups. Due to the posterior instrumentation, the two levels were already stabilized. We suspect that it will not be possible to overcorrect the spine for a relevant amount, due to the limited mobility in this segment, which is caused by the posterior fixator.
The cages were used according to the optimal configuration that was technically feasible. Nevertheless, a mismatch of the vertebra and cage endplates cannot be excluded, and this mismatch may affect subsidence. The ratio of vertebral and cage endplates did not differ between HU subgroups, but we found significant correlations between the ratio and the extent of subsidence. We found that the larger the mismatch between the endplates was, the greater the subsidence. Moreover, the cages did not have to tower over the edge of the vertebrae. To minimize the risk of subsidence, the endplate of the vertebra and cage should be as equal as possible. Nevertheless, this effect is described as low in our patients.
In 2011, Schreiber et al. found significant correlations between HUs and BMD, age, and T-scores and between HUs and compressive strength (P < 0.001) in a case series of 25 patients [9]. Schreiber and colleagues concluded that these data may have utility for the diagnosis and treatment of osteoporosis.
In addition, in 2011, Pickardt et al. [20] investigated the ability to assess BMD derived from screening computed tomographic colonography (CTC) in correlation with DEXA as the reference standard in 252 adults. They analyzed a phantomless qCT-technique and HU in regard to sensitivity and specificity to detect osteoporosis and concluded that phantomless qCT and HU of the lumbar spine were effective for BMD screening with high sensitivity for osteoporosis, as defined by the DEXA T-score. Pickardt et al. analyzed BQ in 2013 in 1867 patients with HU, using the technique described by Schreiber et al. (the same technique was also used in our study). They compared HU with DEXA for the identification of osteoporosis [8, 9] and found that a threshold of 160 HU had a sensitivity of 90% and that a threshold of 110 HU had a specificity of 90% for diagnosing osteoporosis. They concluded that HUs were an appropriate tool for identifying patients with osteoporosis or normal BMD. This topic was further investigated by Choi et al. [21], and their results support the strong correlation between DEXA and HU.
Considering that (1) BMD can be closely estimated with HU values (confirmed using correlation analysis of DEXA and qCT values to HU values) [8, 9]; (2) a correlation between BMD and cage subsidence is present, as indicated by Oh et al. [7]; and (3) BMD is correlated with mechanical properties of the bone [4, 6], we think that the main cause of the loss of reduction and cage subsidence is the diminished BQ of the studied cohort.
This finding is consistent with the results of Schwaiger et al. [15] and Meredith et al. [22]. They were able to determine in 62 prospectively collected cases that screw loosening, existing fractures and fractures that occurred during the course of treatment (patients with instrumented spinal fusion due to degenerative indications) were observed only in patients who had a significantly lower HU. These results were confirmed by Bredow et al. [23]. Another study determined a threshold of 132 HU with a sensitivity of 83.3% and a specificity of 61.1 for cage subsidence following PLIF and unilateral fixation [14].
The biological conditions (quality of bone) cannot be influenced in the case of injury. If this could be adequately assessed preoperatively (HU measurement), BQ could then be appropriately considered through specific selection of the implant and surgical technique. Larger and more rectangular cage footprints improve the mechanical coupling of the cage to bone [24]. The use of additional anterolateral plates improves mechanical stability [25]. Cages with bone-like mechanical properties present an option for reducing the mechanical impedance step at the bone–implant interface [26, 27].
Different augmentation techniques are used to improve screw anchorages [28], and these techniques could be applied to avoid loss of reduction following posterior stabilization (first OP). To avoid cage subsidence after anterior stabilization, direct augmentation of endplates is possible, as described by Geiger et al. in 2010 [29].
Consistent with the previously described studies above and our findings, we revised our treatment protocol. HU measurements have become routine in patients with spinal fractures. In patients with an HU < 110, qCT is initially performed to plan for surgery. For patients with HU between 110 and 180, we are using cages with rectangular and larger footprints adapted to the patient’s individual anatomy. Additional anterior plate instrumentation is also performed.
In cases of severe osteoporosis on qCT, we use PMMA augmentation of screws and vertebroplasty of the fractured VB.
A higher degree of traumatic instability could be expected to result in a higher amount of loss of reduction. Group 3, which had HU values greater than 180, had the highest degree of AOSpine injury. This group had the lowest loss of reduction. As there were no correlations between AOSpine classification and ∂CA, we propose that BQ has a greater effect on CA than does the severity of injury described by AOSpine classification.
However, in the analysis of our cohort, we found poorer HU than we expected. Even young patients and patients who were expected to have good BQ based on gender and age demonstrated a significant loss of reduction, more cage subsidence than expected and low HU values.
Mi et al. [14] showed that cage subsidence was associated with low preoperative HU values for single-level (L4/5) transforaminal lumbar interbody fusion (TLIF) and recommended preoperative planning by including HU measurement as a predictor of cage subsidence.
Our work, based on a larger cohort, confirms this recommendation, which was also proposed by Hendrickson et al. and Spruit et al.[11, 29]. HU measurement enables us to detect BQ reduction before surgery and to optimize our surgical planning. We recommend classifying patients after VB fractures into two groups according to BQ, as estimated by HU: patients with healthy BQ, or HU > 180, and patients with weak BQ, or HU < 180.
Limitations of the study
There are some limitations of this study that should be considered. First, there is potential for selection bias because we analyzed only cases with VBR.
The data were determined by only one investigator (BU).
There was no power control for the expandable cage used, and thus, we do not know the force applied on the cage–bone interface, which is dependent on cage positioning (e.g., angulation and endplate fitting). However, differences in cage-fitting to the endplates (due to modular end caps of 3°, 8° or 15°) can lead to greater forces at the bone–implant interface and promote cage subsidence, and this possibility should not be excluded.
We have no data on postoperative patient activity. It would be useful for future investigations to collect these data, e.g., with a fitness tracker.
Conclusion
-
Only patients with the best bone quality (group 3, HU > 180) (35% of our cohort) achieved our expectations of the treatment (maintenance of reduction).
-
In all groups, we found subsidence and loss of reduction at a higher rate than expected (subsidence rate: good BQ: 69%, diminished BQ: 95% and poor BQ: 100%).
-
The HU appears to be an appropriate tool to estimate, for surgical purposes, BQ in trauma patients. We found HU-dependent effects on cage subsidence and loss of reduction.
-
Preoperative HU measurements offer additional information and should be taken into account to optimize the planning of surgical spine trauma treatment.
-
Considering our study results, we revised our treatment protocols for spinal fractures. HU measurements are now routinely used to detect patients with diminished or poor BQ.
References
Reinhold M, Knop C, Beisse R, Audige L, Kandziora F, Pizanis A, Pranzl R, Gercek E, Schultheiss M, Weckbach A, Buhren V, Blauth M (2010) Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, Internet-based multicenter study of the Spine Study Group of the German Association of Trauma Surgery. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 19(10):1657–1676. https://doi.org/10.1007/s00586-010-1451-5
Verheyden AP, Holzl A, Ekkerlein H, Gercek E, Hauck S, Josten C, Kandziora F, Katscher S, Knop C, Lehmann W, Meffert R, Muller CW, Partenheimer A, Schinkel C, Schleicher P, Schnake KJ, Scholz M, Ulrich C (2011) Recommendations for the treatment of thoracolumbar and lumbar spine injuries. Unfallchirurg 114(1):9–16. https://doi.org/10.1007/s00113-010-1934-1
Weiser L, Huber G, Sellenschloh K, Viezens L, Püschel K, Morlock MM, Lehmann W (2017) Insufficient stability of pedicle screws in osteoporotic vertebrae: biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur Spine J 26(11):2891–2897
Rohl K, Ullrich B, Huber G, Morlock MM (2009) Biomechanical analysis of expansion screws and cortical screws used for ventral plate fixation on the cervical spine. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 18(9):1335–1341. https://doi.org/10.1007/s00586-009-1087-5
Lund T, Oxland TR, Jost B, Cripton P, Grassmann S, Etter C, Nolte LP (1998) Interbody cage stabilisation in the lumbar spine: biomechanical evaluation of cage design, posterior instrumentation and bone density. J Bone Joint Surg Br 80(2):351–359
Knoller SM, Meyer G, Eckhardt C, Lill CA, Schneider E, Linke B (2005) Range of motion in reconstruction situations following corpectomy in the lumbar spine: a question of bone mineral density? Spine 30(9):E229–E235
Oh KW, Lee JH, Lee JH, Lee DY, Shim HJ (2016) The correlation between cage subsidence, bone mineral density, and clinical results in posterior lumbar interbody fusion. Clin Spine Surg. https://doi.org/10.1097/bsd.0000000000000315
Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N (2013) Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med 158(8):588–595
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am 93(11):1057–1063. https://doi.org/10.2106/JBJS.J.00160
Budoff MJ, Malpeso JM, Zeb I, Gao YL, Li D, Choi TY, Dailing CA, Mao SS (2013) Measurement of phantomless thoracic bone mineral density on coronary artery calcium CT scans acquired with various CT scanner models. Radiology 267(3):830–836. https://doi.org/10.1148/radiol.13111987
Hendrickson NR, Pickhardt PJ, del Rio AM, Rosas HG, Anderson PA (2018) Bone mineral density T-scores derived from CT attenuation numbers (hounsfield units): clinical utility and correlation with dual-energy X-ray absorptiometry. Iowa Orthop J 38:25
McCormack T, Karaikovic E, Gaines RW (1994) The load sharing classification of spine fractures. Spine 19(15):1741–1744
Reinhold M, Audige L, Schnake KJ, Bellabarba C, Dai LY, Oner FC (2013) AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22(10):2184–2201. https://doi.org/10.1007/s00586-013-2738-0
Mi J, Li K, Zhao X, Zhao CQ, Li H, Zhao J (2016) Vertebral body hounsfield units are associated with cage subsidence after transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Clin Spine Surg. https://doi.org/10.1097/bsd.0000000000000490
Schwaiger BJ, Gersing AS, Baum T, Noel PB, Zimmer C, Bauer JS (2014) Bone mineral density values derived from routine lumbar spine multidetector row CT predict osteoporotic vertebral fractures and screw loosening. AJNR Am J Neuroradiol 35(8):1628–1633. https://doi.org/10.3174/ajnr.A3893
Warming L, Hassager C, Christiansen C (2002) Changes in bone mineral density with age in men and women: a longitudinal study. Osteoporo Int J Establ Result Coop Between Eur Found Osteoporo Natl Osteoporo Found USA 13(2):105–112. https://doi.org/10.1007/s001980200001
Lee JH, Oh HS, Choi JG (2016) Comparison of the posterior vertebral column resection with the expandable cage versus the nonexpandable cage in thoracolumbar angular kyphosis. Clin Spine Surg. https://doi.org/10.1097/bsd.0000000000000236
Knop C, Lange U, Bastian L, Oeser M, Blauth M (2001) Biomechanical compression tests with a new implant for thoracolumbar vertebral body replacement. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 10(1):30–37
Spiegl UJ, Jarvers JS, Heyde CE, Glasmacher S, Von der Hoh N, Josten C (2016) Delayed indications for additive ventral treatment of thoracolumbar burst fractures: what correction loss is to be expected. Unfallchirurg 119(8):664–672. https://doi.org/10.1007/s00113-015-0056-1
Pickhardt PJ, Lee LJ, Muñoz del Rio A, Lauder T, Bruce RJ, Summers RM, Pooler BD, Binkley N (2011) Simultaneous screening for osteoporosis at CT colonography: bone mineral density assessment using MDCT attenuation techniques compared with the DXA reference standard. J Bone Miner Res 26(9):2194–2203
Choi MK, Kim SM, Lim JK (2016) Diagnostic efficacy of Hounsfield units in spine CT for the assessment of real bone mineral density of degenerative spine: correlation study between T-scores determined by DEXA scan and Hounsfield units from CT. Acta Neurochir 158(7):1421–1427
Meredith DS, Schreiber JJ, Taher F, Cammisa FP Jr, Girardi FP (2013) Lower preoperative Hounsfield unit measurements are associated with adjacent segment fracture after spinal fusion. Spine 38(5):415–418
Bredow J, Boese CK, Werner CM, Siewe J, Lohrer L, Zarghooni K, Eysel P, Scheyerer MJ (2016) Predictive validity of preoperative CT scans and the risk of pedicle screw loosening in spinal surgery. Arch Orthop Trauma Surg 136(8):1063–1067. https://doi.org/10.1007/s00402-016-2487-8
Mundis GM, Eastlack RK, Moazzaz P, Turner AW, Cornwall GB (2015) Contribution of Round vs. rectangular expandable cage endcaps to spinal stability in a cadaveric corpectomy model. Int J Spine Surg 9:53. https://doi.org/10.14444/2053
Shimko DA, Shimko VF, Sander EA, Dickson KF, Nauman EA (2005) Effect of porosity on the fluid flow characteristics and mechanical properties of tantalum scaffolds. J Biomed Mater Res B Appl Biomater 73(2):315–324. https://doi.org/10.1002/jbm.b.30229
Levine BR, Sporer S, Poggie RA, Della Valle CJ, Jacobs JJ (2006) Experimental and clinical performance of porous tantalum in orthopedic surgery. Biomaterials 27(27):4671–4681. https://doi.org/10.1016/j.biomaterials.2006.04.041
Elder BD, Lo SF, Holmes C, Goodwin CR, Kosztowski TA, Lina IA, Locke JE, Witham TF (2015) The biomechanics of pedicle screw augmentation with cement. Spine J Off J North Am Spine Soc 15(6):1432–1445. https://doi.org/10.1016/j.spinee.2015.03.016
Geiger F, Kafchitsas K, Rauschmann M (2010) Sintering prophylaxis of a vertebral body replacement: anterior cement augmentation of vertebral end plates. Der Orthopade 39(7):699–703. https://doi.org/10.1007/s00132-010-1604-6
Spruit M, Meijers H, Obradov M, Anderson PG (2004) CT density measurement of bone graft within an intervertebral lumbar cage: increase of hounsfield units as an indicator for increasing bone mineral content. J Spinal Disord Techn 17(3):232–235
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ullrich, B.W., Schenk, P., Spiegl, U.J. et al. Hounsfield units as predictor for cage subsidence and loss of reduction: following posterior-anterior stabilization in thoracolumbar spine fractures. Eur Spine J 27, 3034–3042 (2018). https://doi.org/10.1007/s00586-018-5792-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5792-9