Abstract
Purpose
Loosening of pedicle screws is one major complication of posterior spinal stabilisation, especially in the patients with osteoporosis. Augmentation of pedicle screws with cement or lengthening of the instrumentation is widely used to improve implant stability in these patients. However, it is still unclear from which value of bone mineral density (BMD) the stability of pedicle screws is insufficient and an additional stabilisation should be performed. The aim of this study was to investigate the correlation of bone mineral density and pedicle screw fatigue strength as well as to define a threshold value for BMD below which an additional stabilisation is recommended.
Methods
Twenty-one human T12 vertebral bodies were collected from donors between 19 and 96 years of age and the BMD was measured using quantitative computed tomography. Each vertebral body was instrumented with one pedicle screw and mounted in a servo-hydraulic testing machine. Fatigue testing was performed by implementing a cranio-caudal sinusoidal, cyclic (0.5 Hz) load with stepwise increasing peak force.
Results
A significant correlation between BMD and cycles to failure (r = 0.862, r 2 = 0.743, p < 0.001) as well as for the linearly related fatigue load was found. Specimens with BMD below 80 mg/cm3 only reached 45% of the cycles to failure and only 60% of the fatigue load compared to the specimens with adequate bone quality (BMD > 120 mg/cm3).
Conclusions
There is a close correlation between BMD and pedicle screw stability. If the BMD of the thoracolumbar spine is less than 80 mg/cm3, stability of pedicle screws might be insufficient and an additional stabilisation should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vertebral fractures represent one of the most common manifestations of osteoporosis [1]. In cases of secondary kyphosis or unstable fractures as well as during deformity and tumour surgery, a posterior stabilisation is often necessary. In this regard, pedicle screw fixation is considered the gold standard [2–4]. However, loosening at the bone–screw interface is a common complication [5–7].
Several factors have been reported related to screw loosening. Stress shielding might lead to a remodelling of the bone surrounding the screw following lesser fixation [5]. Furthermore, wear debris, infections, and local high strains due to inadequate anterior support have been reported as risk factors for screw loosening [5, 8, 9]. A high incidence of loosening is reported for the elderly population [5, 10]. In this regard, osteoporosis is mentioned as a major risk factor [6, 10, 11], as the incidence of loosening ranges up to 60% in osteoporotic patients [12].
There are several biomechanical studies showing significantly reduced pull-out strength of pedicle screws in osteoporotic vertebrae [2, 6, 11, 13, 14]. However, the clinical significance of this testing method has been questioned, since withdrawing of the screws posteriorly through the pedicle has rarely been reported as a mechanism of failure in clinical reports [15–18]. Furthermore, there is rare evidence regarding a threshold of bone mineral density (BMD) which has to be assessed as being insufficient for stable screw fixation and an additional stabilisation, such as lengthening of the instrumentation or cement augmentation, should be performed. Only two studies focussed on this topic and showed that loosening might be expected at BMD measured less than 90 mg/cm3 [19] and that vertebrae with an average BMD of 95 ± 33.3 mg/cm3 (QCT) could not be stabilised anatomically by pedicle screws [20].
The goals of this biomechanical cadaver study were to evaluate the correlation of bone mineral density and pedicle screw strength using a fatigue test, to try to simulate in vivo loading conditions. Fatigue failure of the bone is believed to be more clinically relevant compared with failure due to pull-out [15, 16, 18]. Based on this, a threshold of BMD was defined from which the stability of pedicle screws is insufficient and an additional stabilisation procedure should be recommended.
Methods
We hypothesized that there is a clear correlation between BMD and pedicle screw showing a threshold of BMD from which stability of pedicle screws is insufficient. A total of 21 (eleven female, ten male) cadaveric specimens of human T12 vertebral bodies were collected from donors between 19 and 96 years of age (mean 69 years, SD 19 years). After harvesting, the specimens were sealed in plastic bags and stored at −20 °C.
Each specimen was scanned using a 16-row CT-scanner (Brilliance 16 CT; Philips Healthcare, Hamburg, Germany) with a solid calibration phantom (Bone Density Calibration Phantom; QRM, Moehrendorf, Germany) to screen for prior fractures, to measure the pedicle width, and to determine apparent volumetric trabecular bone mineral density (BMD). The BMD was determined by linearly converting the Hounsfield unit value from a defined voxel cube from the center of each T12 vertebral body to the phantom’s reference densities (Avizo 5.1, VSG Inc., Burlington, Massachusetts, USA).
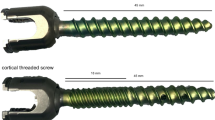
After defrosting of the specimens the night before testing, the T12 vertebral bodies were separated from the thoracolumbar spine. Specimens were sprayed with Ringer solution throughout preparation and wrapped in moist tissue prior to testing to preserve tissue constitution. Each T12 vertebral body was instrumented using commercially available 5.5 × 45 mm self-tapping, monoaxial screws (XIA3, Stryker Inc., Kalamazoo, MI, USA). Screws were inserted parallel to the vertebral end plate into one pedicle under fluoroscopic guidance. The implantation was performed alternately in the left and the right pedicle while the remaining other pedicle was not instrumented and not used for further investigation. The specimens were then embedded in a custom-made fixture using a polyurethane resin (Ureol FC53, Gößl & Paff, Karlskron, Germany). Orientation of the vertebral body was parallel to the base plate. The fixture was constructed in such way that the specimens were fixed to the posterior border of the vertebral body, but the pedicle remained completely free (Fig. 1).
Mechanical setup
The specimens were mounted on an x–y table in a servo-hydraulic testing machine (MTS 858.2, MTS Systems, Eden Praire, USA). A 6-mm rod (XIA titanium, Stryker Inc., Kalamazoo, MI, USA) was fixed to the screws using blockers (XIA Blockers, Stryker Inc., Kalamazoo, MI, USA) and linked to a custom-made connector of 8.3 cm superior to the screw. This distance corresponds approximately to the bridged distance of a fractured vertebra. A laterally orientated rotational joint in the connector allowed bending of the rod. Since the joint was positioned above the posterior border of the vertebral body, the axial actuator load from superior acted as a moment on the head of the screw (Fig. 1)—superpositioned by the axial loading. The loading of this experimental setup was similar to the loading in the ASTM F1717 norm.
Fatigue testing was performed by implementing a sinusoidal, cyclic (0.5 Hz) force. For the initial cycle the axial load ranged from 50 to 100 N, which represents the load range during physiological walking [21]. The maximum compressive force was increased stepwise by 0.05 N every cycle to accelerate failure by reducing the effects of specimen degradation (Locati test design) [18]. Testing was stopped when the caudal displacement of the connector at the testing machine exceeded 15 mm.
Output parameters
The number of cycles and the linearly related maximum force (failure load) until the end of the test were recorded. Stiffness values were determined from a linear regression slope to the load displacement curves and were measured after ten cycles of setting as well as ten cycles before failure. After the mechanical testing, the specimens were manually screened for macroscopic loosening of the pedicle screws. Loosening was assumed if significant expansion of the entry point of the screw was observed and in case of a significant movement of the screw in the vertebral body. Furthermore, additional CT scans were made to evaluate loosening. The removal torque of each screw was measured (Torsiometer 760, Stahlwille, Wuppertal, Germany) to receive a quantitative measure.
Statistical analysis
For statistical analysis (SPSS, Version 21, IBM, Armonk, USA) the type I error probability was set to α = 0.05. A linear regression analysis with stepwise reduction was performed to investigate the influence of the BMD as well as the age and pedicle width on the cycles to failure or fatigue load, respectively. Significance of the regression was tested using an ANOVA analysis. Nonparametric Kruskal–Wallis test analyses were performed to compare the cycles to failure and the fatigue force of different BMD groups. The threshold values of the different BMD groups were based on the guidelines of the American college of radiology which defined a QCT trabecular spine BMD range which is approximately equivalent to the World Health Organisation diagnostic category: normal: BMD > 120 mg/cm3; osteopenia: 80 mg/cm3 ≥ BMD ≥ 120 mg/cm3; osteoporosis: BMD < 80 mg/cm3 [22].
Results
Specimen’s age was between 19 and 96 years and the BMD ranged from 43.3 to 203.6 mg/cm3. BMD significantly decreased with age (r = −0.724, p < 0.001).
The fatigue testing produced a pattern of failure with caudal displacement of the tip of the screw as well as a widening of the entrance point into the pedicle (Fig. 2). The visual screening of the specimens after testing showed a loosening of 18 screws and the removal torque was less or equal to 0.30 Nm in these cases. In three cases (BMD ≥150.00 mg/cm3), there was no visual loosening and the removal torque was higher than 2.0 Nm (Table 1). CT after testing confirmed these results. Additionally, there was a significantly decreased stiffness at the end of testing compared to the beginning, indicating failure (Start: 74.5 ± 9.6 N/mm, End: 28.4 ± 7.2 N/mm; p < 0.001).
Linear regression analyses were calculated for the dependent variables cycles to failure and fatigue load with the predictive variables BMD, age, and pedicle width. A stepwise reduction of parameters showed no significant influence of age (p = 0.423) or pedicle width (p = 0.937) on the coefficient of determination and therefore were omitted. There was a highly significant correlation between BMD and cycles to failure (r = 0.862, r 2 = 0.743, p = 0.001) and consequently also between BMD and fatigue load (r = 0.854, r 2 = 0.73, p < 0.001) (Fig. 3). Nevertheless, when the BMD is left out, there is a significant correlation between age and cycles to failure (r = 0.662, r 2 = 0.438, p = 0.001) as well as age and failure load (r = 0.662, r 2 = 0.438, p = 0.001).
Correlation between cycles to failure and BMD T12 shown with 95% confidence interval of the mean value. Different risks for osteoporotic fractures depending on the BMD are coloured according to Link [23] and mean cycles to failure of each group are marked
Specimens with bone mineral density below 80 mg/cm3, which is defined as threshold value for osteoporosis [22, 23], only reached 45% of the cycles to failure and only 60% of the fatigue load compared to the specimens with adequate bone quality (BMD > 120 mg/cm3) and accordingly there was a significant difference regarding the cycles to failure (p < 0.001) as well as the fatigue load (p < 0.001) between these two groups Table 1).
Discussion
Loosening of pedicle screws is a relevant complication in posterior spinal stabilisation, especially in osteoporotic patients [10–12]. There are different methods to improve screw stability in these cases. Augmentation of pedicle screws with bone cement is widely used and has shown good results in biomechanical as well as clinical studies [24]. Karius et al. showed that the use of radiofrequency-activated cement shows significantly increased pull-out forces in osteoporotic and non-osteoporotic vertebrae and concluded that this is a simple procedure with increased control and fewer complications like extravasation [25]. Wilke et al. investigated the biomechanical performance of a lamina hook system compared to a pedicle screw system. They showed that there are no obvious biomechanical disadvantages of the lamina hook system and inferred that it might be an alternative stabilisation method for the treatment of elderly spines [26]. Furthermore, Aycan et al. tested pedicle screws with expandable poly-ether-ether-keton shells which might be an alternative method to increase pedicle screw stability omitting the disadvantages of cement augmentation [27].
There are several factors influencing the stability of pedicle screws such as length, diameter, design, and particularly the BMD. Biomechanical pull-out tests have shown a high correlation between BMD and pedicle screw stability [7, 13, 19]. However, axial pull-out of the screw posteriorly through the pedicle is a very rare failure pattern (0.2–1%), and therefore the clinical relevance of these studies is very limited [15, 16, 28].
The current fatigue testing was utilised because of a series of forces within the physiological range [21] and an in vivo like failure pattern with cranio-caudal loosening of the screws in the vertebral bodies with a loosening zone expansion at the screw tip [29, 30]. It was based on the corpectomy model (ASTM 1717) which has been shown to be suitable to simulate a postoperative loading condition in vitro [16]. Although it has to be determined if a biomechanical fatigue testing setup is able to gather clinically relevant pedicle screw loosening parameters, this loading protocol is closer to the clinical situation compared with pull-out testing anyway. A stepwise increasing load accelerates failure to reduce specimen degradation. A significantly decreased stiffness during testing, indicating damage to the trabecular bone as shown by Kiner et al. [31], as well as a very low removal torque after testing is consistent with the loosening of the screws during testing. The measurement of the BMD using QCT is a standard clinical method, and therefore the results of this study can be transferred into clinical routine [23, 32]. Bredow et al. measured the Hounsfield units in a preoperative CT scan and showed that determination of the bone density using this data can predict the risk of screw loosening [33]. Furthermore, Popp et al. showed that the vertebral trabecular bone score (TBS) alone or in addition to BMD predicted incident clinical fracture risk in a representative population-based sample of elderly postmenopausal women, which also highlights the importance of preoperative measurement of bone quality to assess the risk of screw loosening [34].
The existing evidence regarding the question from which BMD the fixation of pedicle screws in the vertebral body is insufficient is rare. Wittenberg et al. performed a biomechanical study with pull-out and cyclic loading in human and calf vertebral bodies. They concluded that loosening may be expected at BMD measured less than 90 mg/cm3 (QCT) [19]. Furthermore, they described that under physiologic loads, screw loosening occurred in spines with BMD below 74 mg/cm3. Okuyama et al. investigated the pull-out force, tilting and cut-up of pedicle screws. They showed that vertebrae with an average BMD of 95 ± 33.3 mg/cm3 (QCT) could not be stabilised anatomically by pedicle screws [20]. A clinical study by Okuyama et al. also showed a close relation between BMD and the stability of pedicle screws and the authors conclude that patients with a mean BMD less than 0.674 ± 0.104 g/cm2 (DEXA) have an increased risk for screw loosening [35]. Contrary, Kumano et al. described in their clinical study of patients with one level fusion, that the rate of non-union, screw loosening and screw breakage did not differ significantly between a group with a BMD more than 100 mg/cm3 and a group with a BMD less than 100 mg/cm3. However, patients with severe osteoporosis were excluded from surgeries preoperatively [36].
Regarding the measurement of bone quality in vertebral bodies using qCT there are threshold values which are approximately equivalent to the World Health Organisation diagnostic categories. Osteoporosis is defined as a BMD below 80 mg/cm3 while a BMD between 80 and 120 mg/cm3 is defined as osteopenia [22, 23].
The results of this study showed a highly significant correlation between the BMD and the cycles to failure as well as the fatigue load during fatigue testing. This clearly supports the studies mentioned above, and shows that it is possible to predict the stability of pedicle screws by measuring the preoperative BMD. The osteoporotic specimens with a BMD below 80 mg/cm3 finished significantly lesser cycles to failure (45%) and resisted a significantly lower fatigue load (60%) compared to the specimens with a BMD higher than 120 mg/cm3. Thus, due to a decrease of the cycles to failure by 55% and a decrease of the fatigue load by 40% it can be assumed that pedicle screw fixation is insufficient in osteoporotic vertebrae with a BMD below 80 mg/cm3.
Due to the use of human specimens, this study is limited with regard to sample size and the variation of the vertebral bodies. Variations in the angle, direction and entry point of the introduction of the screws may also have influenced the results. Furthermore, a biomechanical cadaver model is not able to simulate in vivo conditions. Reducing the individual variations by introducing the pedicle width did not show a significant influence. In three cases with very high BMD the implanted screws showed no loosening in the post-testing CT. Thus, the failure occurred at the rod or the fixation. Therefore, the values for fatigue load and cycles to failure would be even higher without this limitation. Due to the testing setup with stepwise increasing load, the measured failure loads are higher than loads occurring in patients during physiological activities.
In summary, there is a close correlation between BMD and pedicle screw stability and therefore the stability of pedicle screws might be insufficient in osteoporotic vertebrae. Accordingly, an additional stabilisation procedure, such as lengthening of the instrumentation or cement augmentation, might be considered in patients with a BMD below 80 mg/cm3.
References
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475. doi:10.1359/jbmr.061113
Cho W, Cho SK, Wu C (2010) The biomechanics of pedicle screw-based instrumentation. J Bone Jt Surg Br 92:1061–1065. doi:10.1302/0301-620X.92B8.24237
Gaines RW Jr (2000) The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Jt Surg Am 82-A:1458–1476
Wood KB, Li W, Lebl DR, Ploumis A (2014) Management of thoracolumbar spine fractures. Spine J 14:145–164. doi:10.1016/j.spinee.2012.10.041
Galbusera F, Volkheimer D, Reitmaier S, Berger-Roscher N, Kienle A, Wilke HJ (2015) Pedicle screw loosening: a clinically relevant complication? Eur Spine J 24:1005–1016. doi:10.1007/s00586-015-3768-6
Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS 3rd, Cook SD (1994) Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976) 19:2415–2420
Soshi S, Shiba R, Kondo H, Murota K (1991) An experimental study on transpedicular screw fixation in relation to osteoporosis of the lumbar spine. Spine (Phila Pa 1976) 16:1335–1341
Hallab NJ, Cunningham BW, Jacobs JJ (2003) Spinal implant debris-induced osteolysis. Spine (Phila Pa 1976) 28:S125–S138
Villa T, La Barbera L, Galbusera F (2014) Comparative analysis of international standards for the fatigue testing of posterior spinal fixation systems. Spine J 14:695–704. doi:10.1016/j.spinee.2013.08.032
Wu ZX, Gong FT, Liu L, Ma ZS, Zhang Y, Zhao X, Yang M, Lei W, Sang HX (2012) A comparative study on screw loosening in osteoporotic lumbar spine fusion between expandable and conventional pedicle screws. Arch Orthop Trauma Surg 132:471–476. doi:10.1007/s00402-011-1439-6
Paxinos O, Tsitsopoulos PP, Zindrick MR, Voronov LI, Lorenz MA, Havey RM, Patwardhan AG (2010) Evaluation of pullout strength and failure mechanism of posterior instrumentation in normal and osteopenic thoracic vertebrae. J Neurosurg Spine 13:469–476. doi:10.3171/2010.4.SPINE09764
El Saman A, Meier S, Sander A, Kelm A, Marzi I, Laurer H (2013) Reduced loosening rate and loss of correction following posterior stabilization with or without PMMA augmentation of pedicle screws in vertebral fractures in the elderly. Eur J Trauma Emerg Surg 39:455–460. doi:10.1007/s00068-013-0310-6
Coe JD, Warden KE, Herzig MA, McAfee PC (1990) Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine (Phila Pa 1976) 15:902–907
Cook SD, Salkeld SL, Stanley T, Faciane A, Miller SD (2004) Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J 4:402–408. doi:10.1016/j.spinee.2003.11.010
Kueny RA, Kolb JP, Lehmann W, Puschel K, Morlock MM, Huber G (2014) Influence of the screw augmentation technique and a diameter increase on pedicle screw fixation in the osteoporotic spine: pullout versus fatigue testing. Eur Spine J 23:2196–2202. doi:10.1007/s00586-014-3476-7
Schulze M, Gehweiler D, Riesenbeck O, Wahnert D, Raschke MJ, Hartensuer R, Vordemvenne T (2016) Biomechanical characteristics of pedicle screws in osteoporotic vertebrae—comparing a new cadaver corpectomy model and pure pull-out testing. J Orthop Res. doi:10.1002/jor.23237
Bostelmann R, Keiler A, Steiger HJ, Scholz A, Cornelius JF, Schmoelz W (2015) Effect of augmentation techniques on the failure of pedicle screws under cranio-caudal cyclic loading. Eur Spine J. doi:10.1007/s00586-015-3904-3
Weiser L, Dreimann M, Huber G, Sellenschloh K, Puschel K, Morlock MM, Rueger JM, Lehmann W (2016) Cement augmentation versus extended dorsal instrumentation in the treatment of osteoporotic vertebral fractures: a biomechanical comparison. Bone Jt J 98-B:1099–1105. doi:10.1302/0301-620X.98B8.37413
Wittenberg RH, Shea M, Swartz DE, Lee KS, White AA 3rd, Hayes WC (1991) Importance of bone mineral density in instrumented spine fusions. Spine (Phila Pa 1976) 16:647–652
Okuyama K, Sato K, Abe E, Inaba H, Shimada Y, Murai H (1993) Stability of transpedicle screwing for the osteoporotic spine. An in vitro study of the mechanical stability. Spine (Phila Pa 1976) 18:2240–2245
Rohlmann A, Bergmann G, Graichen F (1997) Loads on an internal spinal fixation device during walking. J Biomech 30:41–47
American College of Radiology (2014) ACR–SPR–SSR practice parameter for the performance of quantitative computed tomography (QCT) bone densitometry. https://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/QCT.pdf.In. Accessed 17 Oct 2016
Link TM (2012) Osteoporosis imaging: state of the art and advanced imaging. Radiology 263:3–17. doi:10.1148/radiol.12110462, 10.1148/radiol.2633201203
Hoppe S, Keel MJ (2017) Pedicle screw augmentation in osteoporotic spine: indications, limitations and technical aspects. Eur J Trauma Emerg Surg 43:3–8. doi:10.1007/s00068-016-0750-x
Karius T, Deborre C, Wirtz DC, Burger C, Prescher A, Folsch A, Kabir K, Pflugmacher R, Goost H (2016) Radiofrequency-activated PMMA-augmentation through cannulated pedicle screws: a cadaver study to determine the biomechanical benefits in the osteoporotic spine. Technol Health Care. doi:10.3233/THC-161273
Wilke HJ, Kaiser D, Volkheimer D, Hackenbroch C, Puschel K, Rauschmann M (2016) A pedicle screw system and a lamina hook system provide similar primary and long-term stability: a biomechanical in vitro study with quasi-static and dynamic loading conditions. Eur Spine J 25:2919–2928. doi:10.1007/s00586-016-4679-x
Aycan MF, Tolunay T, Demir T, Yaman ME, Usta Y (2017) Pullout performance comparison of novel expandable pedicle screw with expandable poly-ether-ether-ketone shells and cement-augmented pedicle screws. Proc Inst Mech Eng H 231:169–175. doi:10.1177/0954411916687792
Yuan HA, Garfin SR, Dickman CA, Mardjetko SM (1994) A historical cohort study of pedicle screw fixation in thoracic, lumbar, and sacral spinal fusions. Spine (Phila Pa 1976) 19:2279S–2296S
Tokuhashi Y, Matsuzaki H, Oda H, Uei H (2008) Clinical course and significance of the clear zone around the pedicle screws in the lumbar degenerative disease. Spine (Phila Pa 1976) 33:903–908. doi:10.1097/BRS.0b013e31816b1eff
Choma TJ, Frevert WF, Carson WL, Waters NP, Pfeiffer FM (2011) Biomechanical analysis of pedicle screws in osteoporotic bone with bioactive cement augmentation using simulated in vivo multicomponent loading. Spine (Phila Pa 1976) 36:454–462. doi:10.1097/BRS.0b013e3181d449ec
Kiner DW, Wybo CD, Sterba W, Yeni YN, Bartol SW, Vaidya R (2008) Biomechanical analysis of different techniques in revision spinal instrumentation: larger diameter screws versus cement augmentation. Spine (Phila Pa 1976) 33:2618–2622. doi:10.1097/BRS.0b013e3181882cac
Johanson NA, Litrenta J, Zampini JM, Kleinbart F, Goldman HM (2011) Surgical treatment options in patients with impaired bone quality. Clin Orthop Relat Res 469:2237–2247. doi:10.1007/s11999-011-1838-6
Bredow J, Boese CK, Werner CM, Siewe J, Lohrer L, Zarghooni K, Eysel P, Scheyerer MJ (2016) Predictive validity of preoperative CT scans and the risk of pedicle screw loosening in spinal surgery. Arch Orthop Trauma Surg 136:1063–1067. doi:10.1007/s00402-016-2487-8
Popp AW, Meer S, Krieg MA, Perrelet R, Hans D, Lippuner K (2016) Bone mineral density (BMD) and vertebral trabecular bone score (TBS) for the identification of elderly women at high risk for fracture: the SEMOF cohort study. Eur Spine J 25:3432–3438. doi:10.1007/s00586-015-4035-6
Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K (2001) Influence of bone mineral density on pedicle screw fixation: a study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J 1:402–407
Kumano K, Hirabayashi S, Ogawa Y, Aota Y (1994) Pedicle screws and bone mineral density. Spine (Phila Pa 1976) 19:1157–1161
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Rights and permissions
About this article
Cite this article
Weiser, L., Huber, G., Sellenschloh, K. et al. Insufficient stability of pedicle screws in osteoporotic vertebrae: biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur Spine J 26, 2891–2897 (2017). https://doi.org/10.1007/s00586-017-5091-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5091-x