Abstract
Background
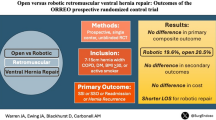
Laparoscopic ventral hernia repair (LVHR) demonstrates comparable recurrence rates, but lower incidence of surgical site infection (SSI) than open repair. Delayed complications can occur with intraperitoneal mesh, particularly if a subsequent abdominal operation is required, potentially resulting in bowel injury. Robotic retromuscular ventral hernia repair (RRVHR) allows abdominal wall reconstruction (AWR) and extraperitoneal mesh placement previously only possible with open repair, with the wound morbidity of LVHR.
Methods
All LVHR and RRVHR performed in our institution between June 2013 and May 2015 contained in the Americas Hernia Society Quality Collaborative database were analyzed. Continuous bivariate analysis was performed with Student’s t test. Continuous nonparametric data were compared with Chi-squared test, or Fisher’s exact for small sample sizes. p values <0.05 were considered significant.
Results
We compared 103 LVHR with 53 RRVHR. LVHR patients were older (60.2 vs. 52.9 years; p = 0.001), but demographics were otherwise similar between groups. Hernia width was similar (6.9 vs. 6.5 cm, p = 0.508). Fascial closure was achieved more often with RRVHR (96.2 vs. 50.5 %; p < 0.001) and aided by myofascial release in 43.4 %. Mesh was placed in an intraperitoneal position in 90.3 % of LVHR and extraperitoneal in 96.2 % of RRVHR. RRVHR operative time was longer (245 vs. 122 min, p < 0.001). Narcotic requirement was similar between LVHR and RRVHR (1.8 vs. 1.4 morphine equivalents/h; p = 0.176). Seroma was more common after RRVHR (47.2 vs. 16.5 %, p < 0.001), but SSI was similar (3.8 vs. 1 %, p = 0.592). Median length of stay was shorter after RRVHR (1 vs. 2 days, p = 0.004). Direct hospital cost was similar (LVHR $13,943 vs. RRVHR $19,532; p = 0.07).
Conclusion
RRVHR enables true AWR, with myofascial release to offset tension for midline fascial closure, and obviates the need for intraperitoneal mesh. Perioperative morbidity of RRVHR is comparable to LVHR, with shorter length of stay despite a longer operative time and extensive tissue dissection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic ventral hernia repair (LVHR) was first introduced in 1993 by LeBlanc and Booth [1], building on previously described laparoscopic techniques for inguinal hernia repair and bringing minimally invasive surgery to the forefront of a common general surgical disease. Adoption of this technique is fairly widespread, but has peaked at around 20–27 % of all ventral hernia repairs (VHR) [2, 3]. Laparoscopic VHR has been associated with shorter length of stay, earlier return to work, comparable recurrence rates, and, most significantly, a reduction in surgical site infection (SSI) when compared with open VHR (OVHR) [4–7]. Pain is variably reported, with several studies indicating greater acute and chronic pain after LVHR [8–10]. There is potential for delayed complications associated with intraperitoneal placement of prosthetic mesh, particularly if a subsequent abdominal operation (SAO) is required. Incidence of enterotomy or bowel resection during SAO with intraperitoneal mesh is as high as 21 % [11, 12]. Secondary mesh infection can also occur, and SAO was implicated in 60 % of patients treated for mesh infection at our institution [13]. Additionally, LVHR typically involves wide mesh overlap of the hernia without closure of the defect, which may lead to eventration of the mesh through the unclosed defect, particularly with larger hernias [14, 15].
Mesh reinforcement for VHR is a well established [16], and OVHR typically involves closure of the defect, which has been shown to decrease the risk of recurrence [17, 18]. The addition of any of the various myofascial releases can decrease abdominal wall tension and aid in reapproximation of the defect. Wound morbidity is a significant deterrent to open repair, specifically the fear of mesh infection, which may require complex wound therapy or mesh explantation. Retromuscular repair of ventral hernias, as described by Rives [19], shows more favorable rates of SSI and hernia recurrence [20–22] and is our preferred open technique, though its adoption is low in the USA [21].
Given the limitations and risks of both the laparoscopic and open approaches to VHR, we developed a robotic technique to reconstruct the abdominal wall in a Rives–Stoppa retromuscular fashion using a minimally invasive approach. Robotic retromuscular ventral hernia repair (RRVHR) is enabled by the flexibility and dexterity of robotic instrumentation, allowing us to perform an extensive musculofascial dissection, complete abdominal wall reconstruction (AWR), and extraperitoneal mesh placement previously only possible with open repair, but with the expected wound morbidity of LVHR. We present early outcomes of a consecutive series of RRVHR compared with consecutive LVHR.
Materials and methods
All consecutive LVHR and RRVHR performed in our institution between June 2013 and May 2015 were included. Patient and operative data were contained within the Americas Hernia Society Quality Collaborative (AHSQC), a prospective, audited database. Demographic data, patient comorbidities, hernia characteristics, operative details, and patient outcomes were compared between the two techniques. Additional retrospective data not contained within the AHSQC were obtained by chart review to evaluate postoperative pain control and narcotic requirement. Average pain scores and narcotic requirement, converted to morphine equivalents, for postoperative day (POD) 0 and 1 were recorded. Continuous bivariate analysis was performed using Student’s t test. Continuous nonparametric data were compared with Chi-squared test, or Fisher’s exact for small sample sizes (n < 5). p values <0.05 were considered statistically significant. All analysis was completed using R statistical software, version 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria). The Greenville Health System Institutional Review Board approved this study.
Surgical technique
Laparoscopic ventral hernia repair
Intraperitoneal access is obtained using an optical trocar, preferentially below the right costal margin. Additional trocars are placed laterally, typically using 4–5 trocars in total, with at least 1 trocar in the contralateral abdomen. Adhesiolysis is completed, hernia contents reduced, and the defect measured intracorporeally with a metric ruler using spinal needles placed transabdominally at the superior, inferior, and lateral extents of the defect. If defect closure is performed, a series of stab incisions are created over the defect and large-gauge monofilament sutures placed in a figure-8 fashion using a suture passer. Defect closure during LVHR was not attempted in every case and was left to the discretion of the operating surgeon. “Swiss cheese” defects and larger defects, which, in the surgeons’ judgment would require excessive tension for reapproximation, were typically not closed. Pneumoperitoneum is released in order to secure the sutures and then reestablished for mesh placement. Appropriate overlap of at least 5 cm in all directions is measured intracorporeally, again using spinal needles, and a barrier-coated permanent mesh placed into the peritoneal cavity and secured to the anterior abdominal wall using a double crown of permanent tacks, variably combined with 2–4 permanent transfascial sutures. For some smaller hernias, a preperitoneal (PP) repair can be performed, with placement of an uncoated mesh in the PP space, followed by closure of the peritoneum to exclude the mesh from the viscera.
Robotic retromuscular ventral hernia repair
For larger hernia defects, a double-dock robotic technique is employed. Intraperitoneal access is obtained in similar fashion to LVHR, placing three trocars along the right lateral abdomen, any necessary adhesiolysis is completed, and hernia contents are reduced. The defect is measured in similar fashion. Retromuscular (RM) dissection is started by incising the contralateral posterior rectus sheath along the entire length of the hernia defect, separating the rectus muscle from the posterior fascia, and extending at least 5 cm above and below the hernia to allow adequate mesh overlap. RM dissection is continued laterally to the semilunar line, followed by transversus abdominis release (TAR) and dissection of the lateral PP space to approximately the anterior axillary line. Three mirror-image trocars are placed on the left side, the dissected space is measured, and uncoated polypropylene mesh is cut to size, placed into the PP space, and affixed just lateral to the nascent trocars. The robot is re-docked on the left side and the RM dissection and TAR performed on the right side. Closure of the posterior sheath is accomplished with running, absorbable self-fixating suture, followed by deployment of the mesh across the closed posterior sheath. The final step is closure of the anterior fascia defect using a running, absorbable, self-fixating suture (Fig. 1).
For smaller to mid-sized defects, a single-dock approach is used. Mesh is placed either in the PP space using an essentially identical technique to PP LVHR described above, or in the retromuscular space. For RM repair, the lateral aspect of the right rectus sheath is incised and dissection carried out to separate the rectus muscle from the posterior fascia from lateral to medial, until the linea alba is reached. The posterior sheath is then incised along the midline to enter the midline PP space, preserving the linea alba. Dissection is carried across the midline, including excision of the hernia sac if possible, and reenters the contralateral rectus sheath as described above. The hernia defect is closed anteriorly with a running, absorbable self-fixating suture, followed by mesh placement against the anterior abdominal wall and closure of the posterior sheath along the initial ipsilateral incision.
Results
One hundred and three LVHR and 53 RRVHR were performed between June 2013 and May 2015. There was no difference between race, sex, comorbidities, smoking status, or American Society of Anesthesiology score, though patients undergoing LVHR were older (60.2 ± 13.4 vs. 52.9 ± 12.3 years; p = 0.001). There was no difference in history of prior abdominal infection, or the presence of mesh from a prior repair (Table 1). There was no difference in Center for Disease Control (CDC) wound classification between groups, with 96.1 % of LVHR and 98.1 % of RRVHR being class 1 wounds and the remainder being class 2; no class 3 or 4 cases were repaired in either group. Mean hernia width and area were similar (6.9 vs. 6.5 cm, p = 0.508; 88 vs. 82 cm2, p = 0.685; range 2–19 cm for LVHR and 2–13 cm for RRVHR). The fascial defect was more likely to be closed after RRVHR than after LVHR (96.2 vs. 50.5 %; p < 0.001), though our practice of transcutaneous closure of defects during LVHR varies and is not attempted for every patient. The size of the mesh placed was significantly larger with RRVHR (435 vs. 339 cm2, p = 0.014). Mesh was placed in an intraperitoneal position in 90.3 % of laparoscopic repairs and in an extraperitoneal position in 96.2 % of robotic repairs. In the RRVHR group, mesh was placed in the retromuscular position in 37 (69.8 %) of cases, in a preperitoneal position in 14 (26.4 %) of cases, and combined with a myofascial release (transversus abdominis release; TAR) in 23 (43.4 %) of patients. Operative time was significantly longer for RRVHR (245.6 ± 98.5 vs. 122 ± 57.2 min, p < 0.001) [Table 2].
Seroma was the most common postoperative surgical site occurrence (SSO), with an incidence of 38.5 % overall, and was more frequently seen after RRVHR (47.2 vs. 16.5 %, p < 0.001). Other SSOs included cellulitis (1), infected seroma (1), hematoma (2), and unspecified (3), with no difference between groups. Procedural intervention (SSOPI) was required in only two patients after RRVHR, one with a percutaneous drainage of a large symptomatic seroma and one with percutaneous drainage for an infected seroma. One patient required percutaneous drainage of a seroma after LVHR. Incidence of SSI was similar between groups, occurring in one patient (0.97 %) after LVHR and two patients (3.77 %) after RRVHR (p = 0.592). One patient after RRVHR developed both a deep and organ space SSI. Intraoperatively recognized bowel injury occurred significantly more often after LVHR than after RRVHR (8.7 vs. 1.9 %; p = 0.011). Of the nine patients with bowel injury after LVHR, six were serosal injuries and three were full-thickness bowel injuries. In all three patients will full-thickness bowel injuries, the hernia was repaired with suture closure of the defect without mesh. One full-thickness gastric injury occurred in the RRVHR group at the site of a prior gastrostomy. This was repaired and the procedure completed as planned.
Four patients were converted to open after attempted LVHR. Three were a result of full-thickness bowel injury. A fourth patient required conversion from LVHR to open RM repair due to difficult adhesiolysis and a large defect. No robotic cases were converted to open. Two patients in each group required reoperation. In the LVHR group, the indication in both instances was small bowel obstruction (SBO) that failed to resolve with non-operative management. In the robotic group, one patient had a missed bowel injury and developed intraabdominal sepsis, requiring exploration, mesh removal, and management with an open abdomen. The second developed an interparietal hernia and presented with SBO due to bowel entrapment between the disrupted posterior sheath and the intact mesh and anterior fascia, requiring laparoscopic reduction and repair.
Readmission was required in five patients (4.8 %) after LVHR and four patients (7.5 %) after RRVHR (p = 0.836). Other medical complications occurred with similar frequency in each group and included ileus, pneumonia, urinary tract infection, acute renal failure, C. difficile colitis, and stroke. One death occurred after LVHR in an elderly patient who was converted to an open suture repair after enterotomy. The patient developed pneumonia, requiring prolonged intubation, and support was later withdrawn. Median length of stay was significantly shorter after RRVHR (1 day) compared with LVHR (2 days; p = 0.004). There was no difference in narcotic requirement between LVHR and RRVHR (1.9 vs. 1.6 morphine equivalents/h; p = 0.176) through POD 1. Mean direct hospital cost was also no different between LVHR and RRVHR ($13,943 vs. $19,532; p = 0.07). Table 3 summarizes our perioperative outcomes.
Discussion
Superior outcomes of robotic assisted surgery have been clearly demonstrated for some procedures, most notably prostatectomy, but its applicability to general surgery remains a contentious issue. Cost is a frequently cited deterrent to the application of robotics to general surgery, which is primarily related to the initial capital expense and maintenance of the robotic system. The literature on robotic colorectal, foregut, thoracic, solid organ, and other digestive tract surgery demonstrates the safety of the robotic approach. However, current evidence of clear clinical benefit over laparoscopy is lacking for most procedures. Robotic surgery may be advantageous for more complex cases in high-volume centers [23] and may prove beneficial in increasing minimally invasive surgery in areas of low laparoscopic penetrance, such as colorectal surgery [24]. A procedure that cannot be otherwise routinely performed in a minimally invasive fashion, but can be accomplished using the robotic platform, is an ideal candidate for the application of this emerging technology.
Retromuscular ventral hernia repair is one such procedure. Complex adhesiolysis is often required, and extensive musculofascial dissection, placement of a large mesh prosthesis, and abdominal wall closure preclude it from being performed laparoscopically for all but the most skilled minimally invasive surgeons. The ergonomics of a difficult anterior abdominal wall dissection are dramatically improved with the robotic platform, and the ease of intracorporeal suturing is a significant advantage. The feasibility of RRVHR was first demonstrated by Abdalla et al. [25] who used the robot to perform a retromuscular repair of small umbilical hernias with associated diastasis rectus. This led us to develop and refine a technique for robotic RM hernia repair, including posterior component separation (TAR) when indicated. As we have gained experience with this approach, we have been able to apply it to increasingly large defects along the entirety of the midline, provide complete reconstruction of the abdominal wall under minimal tension, and wide reinforcement with mesh (Fig. 1).
A Incision of the posterior sheath to enter the RM retromuscular space; B retromuscular dissection completed to the semilunar line, and transversus abdominis release (TAR; white arrow) started medial to lateral perforators (black arrow); C mesh deployed lateral to contralateral trocars; D closure of the posterior sheath after completion of contralateral RM dissection and TAR; E deployment of mesh across the closed posterior sheath; F closure of hernia defect
Wound morbidity can be expected to decrease with RRVHR compared with OVHR, approximating that achieved with LVHR. When evaluating our initial 21 patients repaired robotically, no SSIs occurred. In contrast, in 21 OVHR, matched in a 1:1 fashion for wound classification, hernia width, and body mass index (BMI), SSI occurred 9.5 % of the time [26]. This did not reach statistical significance due to small sample size, but does highlight the potential benefit of a minimally invasive approach. Despite the longer operative times and more extensive dissection involved with RRVHR, the rate of SSI remained similar to LVHR and lower than most reported series of OVHR. The rate of SSO is significantly higher after RRVHR, which were almost exclusively seromas. Other authors have noted a decrease in seroma formation after transcutaneous closure of the hernia defect when performed during LVHR [27]. Though we achieved fascial closure in 96.2 % of cases performed robotically, we still noted a significantly higher rate of seroma after RRVHR. It is likely that this higher rate is a result of the more extensive dissection required for this technique. Importantly, the clinical impact is minimal, and only two patients required percutaneous drainage for their seroma. We have modified our technique during its development, and now routinely imbricate the hernia sac along with the anterior fascial closure. It is currently unknown what impact this may have on seroma formation.
Perioperative complications were similar between RRVHR and LVHR, confirming the safety of the robotic approach. There were significantly more bowel injuries after LVHR in this cohort, which is much higher than our overall rate over 10 years of just 1.3 %. The reason for this is uncertain and may reflect our patient selection, as increasingly complex, recurrent, and multiply recurrent hernia patients are still offered laparoscopic repair. Loss of all haptic feedback is frequently cited as a disadvantage and possible safety concern in robotic surgery. This is countered by the enhanced three-dimensional high-definition optics of the robotic system. Ultimately, the safety of the robotic platform for hernia repair lies with the surgeons’ expertise in reconstructive techniques and recognition of both the benefits and limitations of the technology.
Closure of the fascia is an important factor in OVHR. Several studies have shown that failure to close fascia results in higher rates of hernia recurrence [17, 18], though this may simply be a surrogate marker indicating the complexity of these cases. Whether the restoration of a functional abdominal wall has any relevant clinical impact is not clear. Traditional LVHR involves placing mesh against the posterior abdominal wall to essentially bridge the hernia defect. This may result in eventration or pseudorecurrence, particularly for larger defects, as intraabdominal pressure causes the mesh to bulge through the unclosed hernia defect [14, 15]. Currently, there is a trend toward transcutaneous closure of the hernia defect during LVHR, with promising early results showing a decrease in seroma formation and recurrence [27]. The relative ease of intracorporeal suturing on the robot is appealing for hernia repair, and early reports on the feasibility of robotic VHR noted this as a potential benefit of this approach [28, 29]. However, simple transcutaneous closure fails to offset the tension along the defect closure, which is an important factor in the development of recurrence [30]. Using additional transfascial buttressing sutures may offload midline tension, dispersing the tension along the greater area of the mesh [31]. Addition of an endoscopic component separation can facilitate midline closure as well [31, 32], but is not a routine part of our practice. By releasing the posterior rectus sheath and/or the transversus abdominis (TA) muscle and fascia, we are able to significantly decrease the tension of the midline closure and apply this technique to larger defects.
We used a TA myofascial release in nearly half of cases. The TA essentially acts as an internal girdle, creating circumferential tension to the abdominal wall and providing stability to the lumbosacrum [33]. The implications of division of the TA are largely unknown. Weakness or dysfunction of the TA has been associated with lower back pain and spinal instability [34]. However, there is currently no evidence of deleterious effects of TAR. Computed tomography imaging after TAR demonstrates compensatory hypertrophy of the rectus, external, and internal obliques, which may alleviate the potential negative effects of division of the TA [35].
In this study, TAR is performed at a higher rate than might be predicted based simply on the size defects repaired. During OVHR, a TAR is typically employed only if additional myofascial release is required for fascial closure, or to create additional lateral overlap for off-midline defects. For small- and moderate-sized defects, typically <8 cm, the PP or single-dock approach described above allows repair without using a TAR. However, for larger defects where a double-dock technique is used, because of the necessity of lateral trocar placement, a TAR is required to create working space for the contralateral dissection, posterior sheath closure, and mesh placement. Avoiding a TAR in these cases requires more difficult management of the posterior sheath flaps, reintroducing the laparoscope to assist in mesh fixation anteriorly, and a more difficult closure of the posterior sheath in a limited intraabdominal working space. As our technique has evolved, we have been able to repair increasingly large hernia defects using the double-dock technique with bilateral TAR described above.
Using the robotic approach, a much large mesh size is typically used. The mesh is sized to fill the dissected space rather than based on lateral overlap of the defect. It is unknown what affect the larger mesh size has on recurrence. Vertically, the retromuscular space is dissected at least 5 cm superior and inferior to the defect to allow adequate mesh overlap.
Placement of mesh in an extraperitoneal position is another benefit of RRVHR. Once the RM dissection and TAR are completed, the posterior sheath is closed to completely exclude the visceral sac. This allows mesh to be placed without direct bowel contact. This affords the use of less expensive uncoated mesh, as there is no need to use a barrier-coated prosthesis. All robotic repairs in this study were performed with large-pore mid-weight polypropylene mesh, in the preperitoneal or retromuscular position, with the exception of two patients that required a tissue separating mesh due to intraperitoneal placement. Additionally, delayed complications associated with intraperitoneal mesh must be considered. As many as 25 % of patients may require a SAO after index hernia repair [36, 37]. Adhesions to intraperitoneal mesh can significantly complicate reoperation, leading to enterotomy or other visceral injury in up to 21 % of cases [11, 12, 38], prolonged operative time [36, 38], and secondary mesh infection [11, 13]. We previously reported a 10-year experience with management of mesh infections and found that 60 % of all cases had an intervening abdominal operation after their index hernia repair prior to development of the infection. We also found that 70 % of the cases involved intraperitoneal mesh and were unable to be salvaged, compared with RM mesh, which was salvaged 70 % of the time [13]. Delayed mesh infections and enteroprosthetic fistulae, though uncommon, can occur even in the absence of intervening operations, often several years removed from the index VHR (Fig. 2).
Even with the short LOS associated with LVHR, patients were discharged a full day earlier after RRVHR, with a median LOS of just 1 day compared with 2 days after LVHR. The exact reason for this difference is not clear. Extensive tissue dissection and myofascial releases performed during RRVHR might be anticipated to be more painful and prolong the hospital stay, compared with the simple mesh placement during standard LVHR, making this difference in LOS even more striking. In contrast to most operations performed laparoscopically, LVHR does not necessarily reduce postoperative pain or improve short-term quality of life when compared to OVHR [5, 9]. This may be related to fixation technique. In our study, mesh for RRVHR was typically secured with a few interrupted absorbable sutures, securing the periphery of the mesh to the anterior abdominal wall above the peritoneum. For LVHR, a double crown of permanent tacks, affixing the mesh to the abdominal wall through the peritoneum, with or without additional transfascial suture fixation, was used, which potentially causes increased postoperative pain and prolonged LOS. We attempted to explain this difference in LOS by assessing pain scores and narcotic requirement. No meaningful assessment of the pain scores could be obtained due to high variability in their documentation in the medical record. After conversion to morphine equivalents, there was no difference seen in narcotic use per hour for RRVHR compared with LVHR through the first POD.
When comparing direct hospital costs of LVHR to RRVHR, we did not show a statistical difference. However, these data are inadequate to make any definitive statement to actual cost of RRVHR. A more complex cost analysis is needed to have a more complete economic picture. Prolonged operative time clearly increases the cost of RRVHR, though use of uncoated polypropylene mesh, minimizing the number of robotic instruments used, using suture rather than tacks for mesh fixation, and shorter LOS are important in limiting cost.
Recurrence was not a primary endpoint of this study due to short follow-up in our early experience. To date, only two patients in the RRVHR group have recurred: the index patient that had a recurrence superior to the robotically placed mesh and the patient that required mesh explantation due to missed bowel injury and intraabdominal sepsis. We expect that recurrence will be similar to the open RM technique, which is 10.6 % using mid-weight polypropylene mesh [39], but longer follow-up is necessary before making this determination.
This study is limited by the non-randomized nature of the two groups and selection bias of patients in each group. This, however, is tempered by the fact that most of the LVHR cases during the study time period were performed consecutively by one of the authors who does not perform robotic surgery. Additionally, during the initial development of the RRVHR technique, many of the patients had smaller, less complex defects than those later in the study. The patients most likely to benefit from a robotic approach are those with the highest risk of wound complications and larger defects. Further study is needed in order to determine the most clinically effective and cost-efficient method for VHR for a given patient.
Conclusion
The benefit of RRVHR over LVHR is the complete AWR enabled by this procedure. Anatomic reconstruction of the abdominal wall and myofascial release to offset tension along the midline fascia closure are well-established principles of OVHR, and placement of mesh in the retromuscular rather than intraperitoneal space may decrease the risks associated with future operations and mesh-related complications. Despite the more extensive dissection and myofascial release performed with robotic RRVHR, it compares favorably with the standard laparoscopic repair with the benefit of a shorter hospital length of stay, and no difference in direct hospital costs.
References
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3:39–41
Vorst AL, Kaoutzanis C, Carbonell AM, Franz MG (2015) Evolution and advances in laparoscopic ventral and incisional hernia repair. World J Gastrointest Surg 7:293–305
Tsui C, Klein R, Garabrant M (2013) Minimally invasive surgery: national trends in adoption and future directions for hospital strategy. Surg Endosc 27:2253–2257
Ramshaw BJ, Esartia P, Schwab J (1999) Comparison of laparoscopic and open ventral herniorrhapy. Am Surg 65:827–832
Pierce RA, Spitler JA, Frisella MM, Matthews BD, Brunt LM (2007) Pooled data analysis of laparoscopic vs. open ventral hernia repair: 14 years of patient data accrual. Surg Endosc 21:378–386
Halabi WJ, Jafari MD, Carmichael JC, Nguyen VQ, Mills S, Phelan M, Stamos MJ, Pigazzi A (2013) Laparoscopic versus open repair of parastomal hernias: an ACS-NSQIP analysis of short-term outcomes. Surg Endosc 27:4067–4072
Itani KMF, Hur K, Kim LT, Anthony T, Berger DH, Reda D, Neumayer L, Veterans Affairs Ventral Incisional Hernia Investigators (2010) Comparison of laparoscopic and open repair with mesh for the treatment of ventral incisional hernia: a randomized trial. Arch Surg 145:322–328
Muysoms F, Vander Mijnsbrugge G, Pletinckx P, Boldo E, Jacobs I, Michiels M, Ceulemans R (2013) Randomized clinical trial of mesh fixation with “double crown” versus “sutures and tackers” in laparoscopic ventral hernia repair. Hernia 17:603–612
Colavita PD, Tsirline VB, Belyansky I, Walters AL, Lincourt AE, Sing RF, Heniford BT (2012) Prospective, long-term comparison of quality of life in laparoscopic versus open ventral hernia repair. Ann Surg 256:714–722
Liang MK, Clapp M, Li LT, Berger RL, Hicks SC (2013) Patient satisfaction, chronic pain, and functional status following laparoscopic ventral hernia repair. World J Surg 37:530–537
Halm JA, De Wall LL, Steyerberg EW, Jeekel J, Lange JF (2007) Intraperitoneal polypropylene mesh hernia repair complicates subsequent abdominal surgery. World J Surg 31:423–429
Gray SH, Vick CC, Graham LA, Finan KR, Neumayer LA, Hawn MT (2008) Risk of complications from enterotomy or unplanned bowel resection during elective hernia repair. Arch Surg 143:582–586
Shaver M, Cobb WS, Carbonell AM (2016) A 10-year experience with periprosthetic mesh infections. Hernia Supp 1:S66
Carter SA, Hicks SC, Brahmbhatt R, Liang MK (2014) Recurrence and pseudorecurrence after laparoscopic ventral hernia repair: predictors and patient-focused outcomes. Am Surg 80:138–148
Kurmann A, Visth E, Candinas D, Beldi G (2011) Long-term follow-up of open and laparoscopic repair of large incisional hernias. World J Surg 35:297–301
Burger JWA, Luijendijk RW, Hop WCJ, Halm JA, Verdaasdonk EGG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
Booth JH, Garvey PB, Baumann DP, Selber JC, Nguyen AT, Clemens MW, Liu J, Butler CE (2013) Primary fascial closure with mesh reinforcement is superior to bridged mesh repair for abdominal wall reconstruction. J Am Coll Surg 217:999–1009
Itani KMF, Rosen M, Vargo D, Awad SS, Denoto G, Butler CE, RICH Study Group (2012) Prospective study of single-stage repair of contaminated hernias using a biologic porcine tissue matrix: the RICH study. Surgery 152:498–505
Rives J, Pire JC, Flament JB, Convers G (1977) Treatment of large eventrations (apropos of 133 cases). Minerva Chir 32:749–756
Jin J, Rosen MJ (2008) Laparoscopic versus open ventral hernia repair. Surg Clin N Am 88:1083–1100
Albino FP, Patel KM, Nahabedian MY, Sosin M, Attinger CE, Bhanot P (2013) Does mesh location matter in abdominal wall reconstruction? a systematic review of the literature and a summary of recommendations. Plast Reconstr Surg 132:1295–1304
Israelsson LA, Smedberg S, Montgomery A, Nordin P (2006) Incisional hernia repair in Sweden 2002. Hernia 10:258–261
Rodríguez-Sanjuán JC, Gómez-Ruiz M, Trugeda-Carrera S, Manuel-Palazuelos C, López-Useros A, Gómez-Fleitas M (2016) Laparoscopic and robot-assisted laparoscopic digestive surgery: present and future directions. World J Gastronterol 22:1975–2004
Altieri MS, Yang J, Telem DA, Zhu J, Halbert C, Talamini M, Pryor AD (2016) Robotic approaches may offer benefit in colorectal procedures, more controversial in other areas: a review of 168,248 cases. Surg Endosc 30:925–933
Abdalla RZ, Garcia RB, Costa R, Luca C (2012) Procedimento de Rives/Stoppa modificado robô-assistido para correção de hérnias ventrais da linha média. ABCD Arq Bras Cir Dig 25:129–132
Warren J, Cobb W, Ewing J, Carbonell A (2015) Prospective observational cohort study of robotic vs open Rives-Stoppa retrorectus incisional hernia repair. Hernia 19:S177–S186
Banerjee A, Beck C, Narula VK, Linn J, Noria S, Zagol B, Mikami DJ (2012) Laparoscopic ventral hernia repair: does primary repair in addition to placement of mesh decrease recurrence? Surg Endosc 26:1264–1268
Allison N, Tieu K, Snyder B, Pigazzi A, Wilson E (2012) Technical feasibility of robot-assisted ventral hernia repair. World J Surg 36:447–452
Gonzalez AM, Romero RJ, Seetharamaiah R, Gallas M, Lamoureux J, Rabaza JR (2015) Laparoscopic ventral hernia repair with primary closure versus no primary closure of the defect: potential benefits of the robotic technology. Int J Med Robot 11:120–125
Dragu A, Klein P, Unglaub F, Polykandriotis E, Kneser U, Hohenberger W, Horch RE (2009) Tensiometry as a decision tool for abdominal wall reconstruction with component separation. World J Surg 33:1174–1180
Orenstein SB, Dumeer JL, Monteagudo J, Poi MJ, Novitsky YW (2011) Outcomes of laparoscopic ventral hernia repair with routine defect closure using “shoelacing” technique. Surg Endosc 25:1452–1457
Harth KC, Rosen MJ (2010) Endoscopic versus open component separation in complex abdominal wall reconstruction. Am J Surg 199:342–346
Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ (2012) Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg 204:709–716
Willard FH, Vleeming A, Schuenke MD, Danneels L, Schleip R (2012) The thoracolumbar fascia: anatomy, function and clinical considerations. J Anat 221:507–536
De Silva GS, Krpata DM, Hicks CW, Criss CN, Gao Y, Rosen MJ, Novitsky YW (2014) Comparative radiographic analysis of changes in the abdominal wall musculature morphology after open posterior component separation or bridging laparoscopic ventral hernia repair. J Am Coll Surg 218:353–357
Snyder CW, Graham LA, Gray SH, Vick CC (2011) Effect of mesh type and position on subsequent abdominal operations after incisional hernia repair. J Am Coll Surg 212:496–504
Liang MK, Li LT, Nguyen MT, Berger RL, Hicks SC, Kao LS (2014) Abdominal reoperation and mesh explantation following open ventral hernia repair with mesh. Am J Surg 208:670–676
Jenkins ED, Yom V, Melman L, Brunt LM, Eagon JC, Frisella MM, Matthews BD (2010) Prospective evaluation of adhesion characteristics to intraperitoneal mesh and adhesiolysis-related complications during laparoscopic re-exploration after prior ventral hernia repair. Surg Endosc 24:3002–3007
Cobb WS, Warren JA, Ewing JA, Burnikel A, Merchant M, Carbonell AM (2015) Open retromuscular mesh repair of complex incisional hernia: predictors of wound events and recurrence. J Am Coll Surg 220:606–613
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Warren and Carbonell are speakers for Intuitive Surgical. Drs. Warren, Cobb, and Carbonell are consultants for Ethicon, W.L. Gore, and Maquet Surgical. Joseph Ewing has no financial disclosures.
Rights and permissions
About this article
Cite this article
Warren, J.A., Cobb, W.S., Ewing, J.A. et al. Standard laparoscopic versus robotic retromuscular ventral hernia repair. Surg Endosc 31, 324–332 (2017). https://doi.org/10.1007/s00464-016-4975-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4975-x