Abstract
Background
The purpose of this study was to characterize the adhesion characteristics of absorbable- and nonabsorbable-barrier-coated meshes and to report adhesiolysis-related complications during laparoscopic re-exploration after prior ventral hernia repair.
Methods
Under an IRB-approved protocol, patients undergoing laparoscopic re-exploration after prior intraperitoneal mesh placement were prospectively graded intraoperatively for adhesion tenacity (0-4), adhesion surface area (0 = 0%, 10 = 100%), and ratio of adhesiolysis time to mesh surface area (min/cm2). Adhesiolysis-related complications were also recorded. Data are given as mean ± SD. Statistical significance (P < 0.05) was determined using the t test and Fisher’s exact test.
Results
From March 2006 to March 2009, 69 patients underwent laparoscopic surgery after prior intraperitoneal mesh placement for ventral hernia repair. Previous meshes were absorbable-barrier-coated mesh (n = 18), permanent-barrier composite mesh [Composix® (n = 17)], permanent-barrier noncomposite mesh [DualMesh® (n = 14)], uncoated polypropylene mesh (n = 12), and biologic mesh (n = 8). Indications for laparoscopic re-exploration were recurrent ventral hernia (n = 58), chronic pain (n = 3), cholecystectomy (n = 3), parastomal hernia (n = 2), small bowel obstruction (n = 1), nephrectomy (n = 1), and Nissen fundoplication (n = 1). Adhesions to DualMesh were less tenacious (P < 0.05) compared to all other meshes. Surface area of adhesions to DualMesh were less (P < 0.05) than to Composix and to uncoated polypropylene mesh, but not to absorbable-barrier-coated and biologic meshes. Adhesiolysis time:mesh surface area was less (P < 0.05) for DualMesh compared to Composix, uncoated polypropylene, and biologic mesh, but not to absorbable-barrier-coated mesh. Adhesiolysis-related complications occurred in two (16.7%) (P = ns) patients with uncoated polypropylene mesh, one cystotomy and one enterotomy; both were repaired laparoscopically. There were two (16.7%) (P = ns) conversions to an open procedure: one converted patient had Composix (6.7%) and one had absorbable-barrier-coated mesh (5.9%). There were no adhesiolysis-related complications with these meshes. There were no adhesiolysis-related complications or conversions to open in the DualMesh or biologic mesh groups.
Conclusions
Adhesion characteristics of mesh placed intraperitoneally and adhesiolysis-related complications during laparoscopic re-exploration after ventral hernia repair are associated with unique properties of the mesh and/or barrier.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The placement of a prosthetic biomaterial in the retrorectus, preperitoneal space, as popularized by Rives et al. [1] and Stoppa [2], has reduced the recurrence rates for ventral incisional hernia repair. A prospective randomized trial comparing retrofascial, preperitoneal polypropylene mesh repair to primary repair for ventral incisional hernias reported a 10-year cumulative recurrence rate of 63% for primary suture repair and 32% for a mesh-based repair [3]. In addition, Burger et al. [3] reported that in patients with ventral incisional hernias 10 cm2 or smaller, the recurrence rates were considerably more disparate, with a 67% recurrence rate for primary suture repair compared to 17% after a mesh-based repair. This study established the basis for routine use of mesh for open ventral incisional hernia repair.
The retrorectus, preperitoneal technique described by Rives et al. [1] and Stoppa [2] was the foundation for laparoscopic ventral hernia repair as first reported by Leblanc in 1993 [4]. Laparoscopic ventral hernia repair is an intraperitoneal technique in which a prosthetic biomaterial is placed intra-abdominally against an intact peritoneum and anchored to the anterior abdominal wall with a combination of mechanical fixation devices and transabdominal sutures. The repair avoids wide fascial dissection and flap creation, minimizing postoperative wound and mesh complications [5]. Initial reports of laparoscopic ventral incisional hernia repair demonstrated its durability. Heniford et al. [6] reported a recurrence rate of 4.7% during a mean follow-up of 20 months in 744 patients available for postoperative evaluation. Despite excellent short-term results and low recurrence rates reported for laparoscopic ventral hernia repair, the placement of polypropylene and polyester mesh into the peritoneal cavity as utilized for open ventral hernia repair in the preperitoneal or retrorectus space has not been standard surgical practice since the widespread use of these macroporous meshes began several decades ago. In fact, Halm et al. [7] described a significant risk associated with subsequent abdominal surgery after intraperitoneal placement of polypropylene mesh. In comparing patients requiring abdominal surgery after intraperitoneal versus preperitoneal placement of polypropylene mesh, the small-bowel resection rate (21% vs. 0%) and surgical site infection rate (26% vs. 4%) was greater in the intraperitoneal mesh group, respectively. The overall perioperative complication rate was nearly three times greater in the intraperitoneal mesh group. Novel, adhesion-resistant composite or noncomposite biomaterials with an absorbable barrier coating or nonabsorbable barrier have been developed for laparoscopic and open ventral hernia repair to minimize or avoid the inherent problems of placing macroporous polypropylene and polyester mesh intraperitoneally.
The purpose of this study was to characterize the adhesion characteristics of intraperitoneal absorbable- and nonabsorbable-barrier-coated meshes in patients requiring subsequent laparoscopic abdominal surgery after a prior mesh-based ventral hernia repair and to report adhesiolysis-related complications that occurred during laparoscopic re-exploration.
Methods
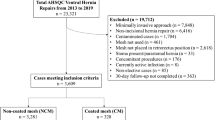
Under an IRB-approved protocol, consecutive patients undergoing laparoscopic re-exploration after prior intraperitoneal mesh placement were identified and prospectively enrolled into a clinical trial (#05-0703). Patient demographics, type of intraperitoneal mesh implanted, time interval (months) between intraperitoneal mesh implantation and laparoscopic re-intervention, and the indication for laparoscopic re-intervention were recorded. Abdominal access was obtained in an abdominal quadrant not previously operated on, utilizing an open technique to insert a 10-mm balloon tip trocar. Meshes were categorized by the material and barrier type: permanent-barrier noncomposite mesh (DualMesh®, W. L. Gore, Inc., Flagstaff, AZ), permanent-barrier composite mesh (Bard® Composix®, Davol, Inc., Cranston, RI), absorbable-barrier-coated mesh (PROCEED™, Ethicon, Inc., Somerville, NJ; Sepramesh, Davol, Inc., Warwick, RI; C-Qur™, Atrium Medical Corp., Hudson, NH; Parietex™ Composite, Covidien, Mansfield, MA), uncoated polypropylene mesh, and biologic mesh (Alloderm®, Lifecell, Inc., Branchburg, NJ; Surgisis®, Cook Biotech, West Lafayette, IN; FlexHD™, Musculoskeletal Transplantation Foundation, Edison, NJ; Bard® Collamend and Allomax, Warwick, RI; Permacol™, Covidien, Mansfield, MA). Omentum or visceral (small intestine/colon) adhesions to the mesh were recorded. Adhesion tenacity was graded (0-4) intraoperatively based on a modified version of the Garrard adhesion scale [8] (Table 1). The scale was modified to better describe patients with intraperitoneal mesh, wherein a grade “4” necessitated cutting mesh off of the abdominal wall to release adhesions. The surface area (cm2) of the mesh was calculated by measuring the cranial-caudal and transverse dimensions (cm) of the intraperitoneal mesh. The surface area of adhesions covering the mesh was estimated in 10th percentiles (0 = 0%, 10 = 100%) (Table 2). Laparoscopic adhesiolysis was performed mostly using a sharp technique with scissors. No bipolar or ultrasonic shears were used for adhesiolysis. The total time (minutes) required to perform laparoscopic adhesiolysis within the borders of the mesh was recorded and a ratio of adhesiolysis time to mesh surface area (min/cm2) was calculated. Adhesiolysis-related complications and open conversions were also recorded. Data are given as mean ± SD. Statistical significance (P < 0.05) was determined using the t test and Fisher’s exact test.
Results
From May 2006 to March 2009, 69 consecutive patients (M:F = 21:48) with a mean age of 52.8 years (range = 26–78) underwent a laparoscopic re-intervention after prior intraperitoneal mesh placement for ventral hernia repair (VHR). Previously placed intraperitoneal meshes were absorbable-barrier-coated mesh (n = 18), permanent-barrier composite mesh [Composix® (n = 17)], permanent-barrier noncomposite mesh [DualMesh® (n = 14)], uncoated polypropylene mesh (n = 12), and biologic mesh (n = 8). Biologic mesh had been placed for the following reasons: four excisions of infected mesh, ventral hernia repair (VHR), one component separation, VHR, noncontaminated case, two parastomal hernia repairs (recurrent), and one explant of mesh on postoperative day 8 at re-exploration for small bowel obstruction (SBO), VHR with biologic.
Indications for laparoscopic re-exploration were a recurrent ventral hernia (n = 58), chronic pain (n = 3), cholecystectomy (n = 3), parastomal hernia (n = 2), small-bowel obstruction (n = 1), nephrectomy (n = 1), and Nissen fundoplication (n = 1). Findings at reoperation for chronic pain revealed recurrent hernia with incarcerated omentum (pain resolved after a redo laparoscopic ventral hernia repair [LVHR]), adhesions to flipped portion of mesh with exposed polypropylene (pain resolved after piece of mesh excised), and no cause of pain (pain unresolved). Both parastomal hernias had been repaired previously with primary closure and biologic mesh reinforcement. The patient with small-bowel obstruction had pelvic adhesions away from the mesh; obstruction resolved after laparoscopic adhesiolysis. Table 3 summarizes the distribution (%) of recurrent hernias and mean time interval between intraperitoneal mesh implantation and laparoscopic re-intervention for each mesh group. The percentage of recurrent hernias was equal for all mesh groups. However, there was a significantly (P < 0.05) shorter time interval between mesh implantation and laparoscopic re-intervention for absorbable-barrier-coated mesh. Mesh size was significantly larger (P < 0.05) for absorbable-barrier-coated mesh and uncoated polypropylene mesh compared to all other mesh types (Table 4). The majority of patients in each group had small intestine or colon adherent to the mesh (P = ns).
The mean adhesion tenacity, surface area (cm2) of mesh covered with adhesions, and the ratio of adhesiolysis time to mesh surface area is summarized in Table 5. Adhesions to the permanent-barrier noncomposite mesh (DualMesh) were less tenacious (P < 0.05) compared to all other mesh groups. Surface area of adhesions to DualMesh were less (P < 0.05) than that to the permanent-barrier composite mesh (Composix) and uncoated polypropylene mesh, but not (P = ns) to absorbable-barrier-coated and biologic meshes. The ratio of adhesiolysis time to mesh surface area was less (P < 0.05) for DualMesh compared to Composix, uncoated polypropylene, and biologic meshes, but not (P = ns) to absorbable-barrier-coated mesh.
Adhesiolysis-related complications occurred in two (18%) (P = ns) patients with uncoated polypropylene mesh: a cystotomy and a small-bowel enterotomy. Both hollow viscus injuries were repaired laparoscopically. The patient with the cystotomy had an uneventful perioperative recovery after laparoscopic ventral hernia repair. The patient with the small-bowel enterotomy underwent an interval laparoscopic ventral hernia repair 4 months after the index operation. There were two (18%) (P = ns) conversions to an open procedure in the uncoated polypropylene mesh group: one patient with Composix (6.7%) and one with absorbable-barrier-coated mesh (6.7%). The reason for conversion was a failure to progress with the adhesiolysis; however, there were no adhesiolysis-related complications. Adhesiolysis-related complications or conversions to open did not occur in the DualMesh or biologic mesh groups.
Discussion
The challenges associated with adhesiolysis and the risks such as bowel, bladder, or solid organ injury and surgical site infection after intraperitoneal mesh placement have been described and should be considered in the clinical decision-making of reoperative surgery [7, 9]. Although adhesions are a natural consequence of abdominal surgery and occur in more than 90% of patients after a laparotomy, an increased foreign body reaction to prosthetic mesh with ensuing tenacious adhesion formation is most likely responsible for the difficulties experienced in repeat surgical interventions after intraperitoneal mesh placement [10]. A recent Veterans Affairs Medical Center review utilizing the National Surgical Quality Improvement Program (NSQIP) database revealed that the incidence of enterotomy or unplanned bowel resection increased approximately fourfold for recurrent incisional hernias during elective incisional hernia repair after prior mesh repair compared to a recurrent hernia previously repaired primarily [11]. Unfortunately, the mesh type was not specified or classified in that study. The occurrence of an enterotomy or unplanned bowel resection was associated with an increased rate of postoperative complications, reoperation within 30 days, and development of enterocutaneous fistula. Innovative, adhesion-resistant biomaterials should minimize the risks associated with subsequent abdominal surgery, but there is an insignificant amount of clinical data to characterize the effectiveness of the absorbable-barrier- or nonabsorbable barrier-coated meshes.
The efficacy of FDA-approved absorbable-barrier-coated meshes and nonabsorbable-barrier composite and noncomposite meshes to minimize adhesion formation has been evaluated in multiple animal models [12–14]. Despite some of the disparities between the results from these animal studies evaluating adhesions to absorbable- and nonabsorbable-barrier meshes placed intraperitoneally, the studies are consistent in demonstrating that barrier meshes are superior to nonbarrier macroporous mesh in reducing adhesion tenacity and amount (surface area). The clinical translation has not been validated in a human trial. Koehler et al. [15] reported minimal adhesions to expanded polytetrafluoroethylene (PTFE) mesh (DualMesh) after laparoscopic ventral hernia repair in 65 reoperative cases, with a mean mesh implantation time of 420 days (range = 2-1739). Utilizing abdominal ultrasound to evaluate adhesion formation to Parietex™ Composite and macroporous polyester meshes placed intraperitoneally, Arnaud et al. [16] demonstrated a reduction in adhesions from 77% in the uncoated polyester mesh group to 18% in the Parietex Composite group. In 4 years follow-up after intraperitoneal placement of Parietex Composite mesh, Balique et al. [17] reported that only one of seven patients had adhesions to the mesh at a repeat surgical intervention.
The metrics developed for this study attempt to characterize the effectiveness of absorbable-barrier-coated meshes and permanent-barrier meshes at reducing adhesion tenacity and improving surgeon efficiency during a laparoscopic reintervention. The ultimate goal of these barriers is patient safety through a reduction in mesh-related complications and long-term stability of the ventral hernia repair. Adhesion surface area scores do not provide a measure of the barrier’s effectiveness. However, the tenacity score, adhesiolysis time, and ratio of adhesiolysis time to mesh surface area are surrogates of operative complexity in laparoscopic re-exploration after intraperitoneal mesh placement. The tenacity score is dependent on the action of the surgeon to perform the adhesiolysis. There is some subjectivity based on the judgment of the surgeon to manage the adhesions between the mesh and viscera. As this was a single-surgeon study, individual surgeon variability was not a confounding factor in the outcomes. The overriding intent in this cohort of patients and in all reoperative situations is the completion of a safe procedure. In the situation of an adhesion tenacity score of “4,” it is up to the operating surgeon to determine the safety of continuing with sharp dissection in a plane between the mesh and viscera or to actually remove a section of the mesh from the abdominal wall, leaving a medallion of the mesh attached to the intestine. The ratio of adhesiolysis time to mesh surface area defines the overall difficulty in performing an adhesiolysis. It characterizes the technical challenges with increasing adhesion tenacity and a larger surface area of the mesh covered with adhesions. Although the majority of patients had a recurrent hernia, the operative indication for laparoscopic re-exploration could potentially alter the adhesion characterization scores.
An unplanned enterotomy did not occur in any of the patients with an absorbable-barrier-coated or nonabsorbable-barrier mesh. Nevertheless, there appears to be some differentiation in the adhesion characteristics of the absorbable-barrier-coated meshes (PROCEED™, Sepramesh, C-Qur™, Parietex™ Composite) after intraperitoneal placement in a human trial (Table 6). Whether this is due to the proprietary, absorbable barrier coating or the polymer of the mesh or a combination is not known. We noticed a similar increase in the adhesion tenacity score of PROCEED in a preclinical study of intraperitoneal placement of absorbable-barrier-coated meshes in a rabbit model [12]. Unfortunately, in the current study the numbers of patients in each absorbable-barrier-coated mesh subgroup were too small to make definitive conclusions. Continuing this study as a multicenter trial will facilitate a more critical evaluation of these novel materials. In contrast, there was a clear difference between DualMesh and Composix favoring the permanent-barrier noncomposite material (Table 5). In most instances, the complexity of adhesiolysis with Composix was related to mesh eversion at the periphery of the biomaterial, exposing the bare polypropylene of this composite mesh. Appropriate fixation techniques may have minimized this problem.
Conclusions
Adhesion characteristics of absorbable-barrier-coated meshes and nonabsorbable composite and noncomposite meshes and adhesiolysis-related complications during laparoscopic re-exploration after ventral hernia repair are associated with the unique properties of the barrier and/or mesh. The potential morbidity of a laparoscopic re-exploration after intraperitoneal mesh placement should be considered in operative planning. A multicenter patient safety trial in evaluating these unique biomaterials is needed to define their effectiveness.
References
Rives J, Pire JC, Flament JB, Palot JP, Body C (1985) Treatment of large eventrations. New therapeutic indications apropos of 322 cases. Chirurgie 111:215–225
Stoppa RE (1989) The treatment of complicated groin and incisional hernias. World J Surg 13:545–554
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3:39–41
Pierce RA, Spitler JA, Frisella MA, Matthews BD, Brunt LM (2006) Pooled data analysis of laparoscopic vs. open ventral hernia repair: 14 years of patient data accrual. Surg Endosc 21:378–386
Heniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias: nine year experience with 850 consecutive hernias. Ann Surg 238:391–400
Halm JA, de Wall LL, Steyerberg EW, Jeekel J, Lange JF (2007) Intraperitoneal polypropylene mesh hernia repair complicates subsequent abdominal surgery. World J Surg 31:423–429
Garrard CL, Clements RH, Nanney L, Davidson JM, Richards WO (1999) Adhesion formation is reduced after laparoscopic surgery. Surg Endosc 13(1):10–13
Van Der Krabben AA, Dijkstra FR, Niewenhuijzen M, Reijnen MM, Schaapveld M, Van Goor H (2000) Morbidity and mortality of inadvertent enterotomy during adhesiotomy. Br J Surg 87(4):467–471
Luijendijk RW, de Lange DC, Wauters CC, Hop WC, Duron JJ, Pailler JL, Camprodon BR, Holmdahl L, van Geldorp HJ, Jeekel J (1996) Foreign material in postoperative adhesions. Ann Surg 223:242–248
Gray SH, Vick CC, Graham LA, Finan KR, Neumayer LA, Hawn MT (2008) Risk of complications from enterotomy or unplanned bowel resection during elective hernia repair. Arch Surg 143(6):582–586
Pierce RA, Perrone JM, Nimeri A, Sexton JA, Walcutt J, Frisella MM, Matthews BD (2009) 120-day comparative analysis of adhesion grade and quantity, mesh contraction, and tissue response to a novel omega-3 fatty acid bioabsorbable barrier macroporous mesh after intraperitoneal placement. Surg Innov 16:46–54
van’t Riet M, van Steenwijk PJ, Bonthuis F, Marquet RL, Steyerberg EW, Jeekel J, Bonjer HJ (2003) Prevention of adhesion to prosthetic mesh: comparison of different barriers using an incisional hernia model. Ann Surg 237:123–128
Matthews BD, Mostafa G, Carbonell AM, Joels CS, Kercher KW, Austin C, Norton HJ, Heniford BT (2005) Evaluation of adhesion formation and host tissue response to intra-abdominal polytetrafluoroethylene mesh and composite prosthetic mesh. J Surg Res 123(2):227–234
Koehler RH, Begos D, Berger D, Carey S, LeBlanc K, Park A, Ramshaw B, Smoot R, Voeller G (2003) Minimal adhesions to ePTFE mesh after laparoscopic ventral hernia incisional hernia repair: re-operative findings in 65 cases. JSLS 7:335–340
Arnaud JP, Hennekinne-Mucci S, Pessaux P, Tuech JJ, Aube C (2003) Ultrasound detection of visceral adhesion after intraperitoneal ventral hernia treatment: a comparative study of protected versus unprotected meshes. Hernia 7:85–88
Balique JG, Benchetrit S, Bouillot JL, Flament JB, Gouillat C, Jarsaillon P, Lepère M, Mantion G, Arnaud JP, Magne E, Brunetti F (2005) Intraperitoneal treatment of incisional and umbilical hernias using an innovative composite mesh: four-year results of a prospective multicenter clinical trial. Hernia 9:68–74
Disclosures
Dr. Jenkins, Dr. Melman, Ms. Yom, and Mrs. Frisella have no conflicts of interest or financial ties to disclose. Dr. Eagon has received consultant fees from Ethicon Endosurgery. Dr. Brunt has received an honorarium for speaking/teaching, supplies for skills training, and grant support for clinical fellowship salary support from Ethicon Endosurgery; an honorarium for speaking/teaching and supplies for skills training from Covidien; grant support for education and training from both Stryker Endoscopy and Karl Storz Endoscopy; and grant support for research from Lifecell Corp. Dr. Matthews has received consulting fees from Atrium Medical, Ethicon EndoSurgery, and Muskuloskeletal Transplant Foundation, and an honorarium for speaking from W.L. Gore.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jenkins, E.D., Yom, V., Melman, L. et al. Prospective evaluation of adhesion characteristics to intraperitoneal mesh and adhesiolysis-related complications during laparoscopic re-exploration after prior ventral hernia repair. Surg Endosc 24, 3002–3007 (2010). https://doi.org/10.1007/s00464-010-1076-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1076-0