Abstract
Diabetic macular edema (DME), characterized by exudative fluid accumulation in the macula, is the most common form of sight-threatening retinopathy in patients with diabetes. The management of DME has changed considerably in recent years, especially following the development of intravitreal anti-vascular endothelial growth factor therapy which has emerged as a first-line therapy for center-involved DME. Laser treatment, intravitreal steroid therapy, and vitrectomy are also important treatment options for DME. We believe that it is important to choose the most appropriate treatment option for DME based on the clinical evidences, in addition to the careful consideration of individual patients’ general or ocular condition, DME characteristics, patients’ motivation, and compliance to the treatment in real-world clinical practice. In this review, we have summarized important clinical evidences for the main treatments for DME, presented an expert review for these evidences, and proposed a recommended therapeutic flow chart for DME. We hope that our review of the clinical evidences and the recommended therapeutic flow chart for DME will contribute to better treatment outcome for DME.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetic macular edema (DME), characterized by exudative fluid accumulation in the macula, is the most common form of sight-threatening retinopathy in patients with diabetes. DME is estimated to affect one in 15 patients with diabetes resulting in more than 20 million cases worldwide [1]. The pathogenesis of DME is multifactorial and complex, in which the hyperglycemic state caused by diabetes induces multiple pathologic abnormalities, such as angiogenic, inflammatory, hypoxic, and hemodynamic processes that lead to the breakdown of the blood-retinal barrier and leakage of the intraretinal fluid. These pathologic abnormalities ultimately lead to sight-threatening conditions of macular edema and proliferative, neovascular retinopathy [2].
The management of DME has changed significantly in recent years, especially with the emergence of intravitreal anti-vascular endothelial growth factor (VEGF) therapy that has emerged as a first-line therapy for center-involved DME [3]. Before the emergence of anti-VEGF therapy, the predominant goal of treatment was visual acuity stabilization. With the approval of anti-VEGF agents for the treatment of visual impairment caused by DME, the primary goal of therapy has now become the improvement or restoration of visual acuity, with the stabilization of vision and prevention of further vision loss as the key secondary goals [4]. However, anti-VEGF therapy has some limitations for routine use in real-world clinical practice, such as the multiple visits required for injections, the accompanying economic and time burden, and risks of the potential systemic side effects [3, 5].
Laser treatment for DME remains to be an important adjunctive therapy in real-world practice [6]. Several studies have reported the clinical usefulness of combining laser and anti-VEGF therapies. In addition, with the development of new laser technologies, such as subthreshold micropulse laser and Navilas® navigated laser (OD-OS GmbH, Germany), laser photocoagulation has again become a topic of interest [7, 8]. Inhibiting the inflammatory processes by the intravitreal application of steroids is an important pharmacotherapy for DME, as is VEGF inhibition caused by the intravitreal injection of an anti-VEGF agent [9]. Early vitrectomy may reduce treatment burden for patients with diabetes, prevent vision loss, and provide the long-term stabilization of retinopathy in patients with diabetes [10].
The main clinical treatments for DME in Japan are intravitreal anti-VEGF therapy, laser treatment, intravitreal steroid therapy, and vitrectomy. We believe that it is important to choose the most appropriate treatment option for DME based on the clinical evidences, careful consideration of the individual patients’ general or ocular condition, DME characteristics, the patients’ motivation, and compliance to the treatment in real-world clinical practice. In this review, the authors have summarized the important clinical evidences for the main treatments of DME, presented an expert review of these evidences, and have proposed a recommended therapeutic flow chart for DME. At the Retina Deep Dive, a conference held by Bayer Yakuhin, Ltd. in 2018, the authors firstly discussed about the proposal of a therapeutic flow chart for DME. The authors continued the discussion and review of clinical evidences after the conference, and have developed the proposal of this therapeutic flow chart. Bayer Yakuhin, Ltd. has not been involved in the preparation process of this proposal, and the authors have prepared this proposal neutrally based on the clinical evidences.
Anti-VEGF therapy
Focal/grid laser had been the only evidence-based treatment for DME since the 1980s [11]. Since 2010, several large trials have demonstrated that the intravitreal injection of an anti-VEGF agent yielded greater improvements in visual acuity than laser photocoagulation in patients with DME. Anti-VEGF therapy has been used increasingly for the treatment of DME in clinical practice [12, 13], and has now replaced laser photocoagulation as the standard of care for this disease. Two anti-VEGF agents, ranibizumab and aflibercept, have been approved for DME in Japan. In this section, we have summarized and reviewed the clinical evidences for these two anti-VEGF therapies, and have discussed recent updates in these evidences.
Ranibizumab
Ranibizumab is a humanized, recombinant antibody fragment of a monoclonal antibody active against all VEGF-A isoforms.
Protocol I from the DRCR.net was the first definitive phase 3 study to address the efficacy and safety of an intravitreal ranibizumab for the treatment of DME in a total of 854 study eyes of 691 participants. This study compared four treatments for DME: ranibizumab given pro re nata (PRN) with prompt laser, ranibizumab with deferred (≥ 24 weeks) laser given only for persistent DME, intraocular triamcinolone with prompt laser, and sham injections with prompt laser. Vision improved by an average of 9 letters in the ranibizumab with laser groups compared with only 3 letters in the sham injection with laser group at the 1-year primary endpoint. This study clearly showed that intravitreal ranibizumab was highly effective for the treatment of DME. The safety evaluation of ranibizumab concluded that the incidence of endophthalmitis should be considered, although ranibizumab therapy was rarely associated with endophthalmitis in this study [14]. The subsequent follow-up of the ranibizumab groups in Protocol I demonstrated sustained vision gains obtained in the first year to 5 years with little additional treatment after 3 years [15].
The RESTORE phase 3 study conducted in Europe randomized 345 subjects into 3 different groups: ranibizumab (given PRN) only, ranibizumab plus laser, and laser only. In the 1-year analysis, visual acuity improved by 6.1 letters in the ranibizumab-only group, by 5.9 letters in the ranibizumab plus laser group, and by 0.8 letters in the laser-only group. There was a statistically significant difference between both ranibizumab groups and the laser-only group, but not between the ranibizumab groups. The mean number of injections was 7.0 in the ranibizumab-only group and 6.8 in the ranibizumab plus laser group. No safety issues were observed in this study (Fig. 1) [16]. The RESTORE extension study followed up 240 patients who completed the RESTORE study and demonstrated that ranibizumab was effective for the improvement and maintenance of visual acuity outcomes with a progressively declining number of injections over 3 years of the PRN regimen. Ranibizumab was generally well tolerated, with no new safety concerns over the 3-year period [17]. The REVEAL study was a randomized controlled study with a design similar to that of the RESTORE study, and was conducted in an Asian population (including Japanese patients). The visual acuity improved by 5.9 letters in the ranibizumab-only group, by 5.7 letters in the ranibizumab plus laser group, and 1.4 letters in the laser-only group. No new ocular or non-ocular safety findings were observed and treatment was well tolerated over 1 year (Fig. 1) [18]. These 2 randomized controlled studies, RESTORE and REVEAL, have demonstrated that the general results for anti-VEGF therapy are applicable across various racial and ethnic groups.
Two methodologically identical phase 3 studies of ranibizumab (monthly injection), RISE, and RIDE (parallel, multicenter, double-masked, sham injection-controlled, randomized studies) were conducted in the USA and South America. RISE enrolled 377 patients with DME, and RIDE enrolled 382 patients. The main outcome measure was improvement of 15 letters or more at 2 years, and the achievement rate was 18.1%, 44.8%, and 39.2% in RISE and 12.3%, 33.6%, and 45.7% in RIDE for patients in the sham injection, 0.3-mg ranibizumab, and 0.5-mg ranibizumab groups, respectively. Similarly to other ranibizumab trials, safety findings were acceptable [19]. The main outcome measure was also evaluated at 3 years, and visual acuity gains achieved at 2 years were sustained throughout the third year [20].
The RETAIN study was a 2-year single-masked study to demonstrate non-inferiority of ranibizumab treat-and-extend (TAE) with and without laser to ranibizumab PRN for visual acuity in patients with DME. Patients with DME were randomized 1:1:1 to ranibizumab TAE with laser (n = 121), ranibizumab TAE (n = 128), and ranibizumab PRN (n = 123) groups. The TAE regimens were non-inferior to PRN based on mean average visual acuity change at 1 year (+ 6.1 and + 6.2 letters in the ranibizumab TAE and PRN groups, respectively). At 2 years, the mean average visual acuity change was similar in both the groups (+ 6.5 and + 8.1 letters, respectively). The mean number of injections was 12.8 in the TAE group and 10.7 in the PRN group. The TAE regimens led to a 46% reduction in the number of clinic visits. The RETAIN study suggested that TAE was a feasible treatment option for patients with DME, with the potential to reduce treatment burden (although slightly more injections were required compared with PRN, likely because of the specifics of the TAE regimen applied in this study) [21].
Aflibercept
Aflibercept is a recombinant fusion protein comprising the key VEGF-binding domains of human VEGF receptors 1 and 2 fused to the constant region of human immunoglobulin G1. Aflibercept acts as a soluble decoy receptor that binds VEGF-A and placental growth factor with higher affinity than naturally occurring VEGF receptors.
Two randomized controlled phase 3 studies of aflibercept, VISTA-DME, and VIVID-DME were conducted to investigate the efficacy and safety of repeated doses of intravitreal aflibercept in patients with DME. The VISTA study conducted in the USA enrolled 461 patients with DME, and the VIVID study conducted in Europe, Japan, and Australia enrolled 404 patients with DME. These patients were randomized into 3 groups: the monthly aflibercept group, the bimonthly aflibercept (after 5 initial monthly doses) group, and the laser group. The primary endpoint was the mean change in visual acuity after 1 year. The patients were scheduled for continued treatment for 3 years. After the first year, the primary results showed the superiority of the aflibercept treatments over the laser treatment. The mean change in visual acuity in the VISTA study was + 12.5 and + 10.7 versus + 0.2 letters for the monthly and bimonthly aflibercept groups versus laser group, respectively. The VIVID study showed a similar mean change in visual acuity of + 10.5 and + 10.7 versus + 1.2 letters, respectively. The overall incidences of ocular and non-ocular adverse events and serious adverse events, including the Anti-Platelet Trialists’ Collaboration-defined arterial thromboembolic events and vascular deaths, were similar across treatment groups [22]. In both the VISTA and VIVID studies, the 1-year visual superiority of aflibercept treatment over laser treatment was sustained throughout the second and third years, with similar efficacy in the monthly and bimonthly aflibercept groups. Over 3 years, the safety results in these studies were consistent with known safety profile of aflibercept [23, 24].
The recent Protocol V from the DRCR Retina Network, a randomized clinical study conducted at 91 US and Canadian sites, enrolled 702 patients with DME and a visual acuity of 20/25 or better. This study randomized patients to initial management with intravitreal aflibercept, or laser versus observation without treatment. In the laser and observation groups, patients were treated with aflibercept if vision worsened during subsequent follow-up. The primary outcome was at least a 5-letter visual acuity decrease from baseline to 2 years, and the percentage achievement of this primary outcome was 16% (33/205), 17% (36/212), and 19% (39/208) in the aflibercept, laser, and observation groups, respectively. After 1 and 2 years, the mean visual acuity was 20/20 in each group (Fig. 2) [25]. Vascular events, as defined by the Antiplatelet Trialists’ Collaboration occurred in 15 (7%), 13 (5%), and 8 (3%) patients, respectively. It was concluded that in eyes with DME and good visual acuity, there was no significant difference in vision loss at 2 years whether the eyes were initially managed with aflibercept or with laser or observation and were then managed with aflibercept if visual acuity worsened. Thus, observation without treatment, unless visual acuity worsens, may be a reasonable strategy for DME [25].
Visual acuity improvement in the DRCR.net Protocol V to compare aflibercept, laser and observation groups in DME patients with good visual acuity [25]. The figure is reprinted with the permission from the publisher of original article
Ranibizumab versus aflibercept
The DRCR.net Protocol T was a prospective, randomized, comparative effectiveness study that compared 3 anti-VEGFs, ranibizumab, aflibercept, and bevacizumab (which are not approved in Japan for the indication of DME) for the treatment of DME. In this study, given the possibility that one medication is more effective in eyes with worse vision, which is possibly associated with higher VEGF levels and more active retinopathy, a pre-specified analysis was planned to compare results from two major subgroups. No difference in the efficacy of the 3 anti-VEGF therapies in eyes with a visual acuity of 20/40 or better was found after 1 or 2 years of follow-up. However, in eyes with a visual acuity of 20/50 or worse, aflibercept was superior to ranibizumab and bevacizumab at 1 year, and at 2 years, aflibercept was no longer superior to ranibizumab but remained superior to bevacizumab (Fig. 3) [26, 27].
Visual acuity improvement in the DRCR.net Protocol T to compare the 3 anti-VEGFs, ranibizumab, aflibercept, and bevacizumab [27]. The figure is reprinted with the permission from the publisher of original article
Switching from ranibizumab to aflibercept
The body of research investigating different treatment protocols for the management of resistant DME is growing. According to the results of the DRCR.net Protocol T, switching from ranibizumab to aflibercept is suggested to be a promising strategy for the treatment of resistant DME with poor presenting vision. Some retrospective and prospective studies support this hypothesis [28,29,30]. In one such study, a prospective interventional case series study recruited 42 patients with DME with a suboptimal response to bevacizumab or ranibizumab (at least 3 consecutive monthly injections in the previous 6 months) and demonstrated that three consecutive monthly injections of aflibercept significantly improved visual acuity with a baseline logMAR visual acuity of 0.87 ± 0.23 to 0.46 ± 0.35 at 3 months [30].
Factors associated with outcomes of anti-VEGF therapy for DME
Additional or post hoc analyses of the randomized clinical study of ranibizumab suggested that baseline central subfield thickness and the presence of subretinal fluid at baseline were associated with better vision outcomes after ranibizumab therapy [31, 32]. Alternatively, a post hoc analysis of the randomized clinical study of aflibercept indicated a strong association between baseline Diabetic Retinopathy Severity Scale (DRSS) score and ≥ 2-step DRSS score improvement after 2 years for patients with DME [33]. A retrospective study that reviewed 66 eyes of 61 Japanese patients with DME who received ranibizumab suggested that the hyperreflective foci in foveal cystoid spaces at baseline were predictive of a poorer short-term (3 months) response to ranibizumab [34]. Recently, a retrospective study was conducted to investigate the factors influencing the clinical outcomes in 73 patients (94 eyes) with DME treated with ranibizumab. This study reported that younger age, better baseline visual acuity, and glycemic control were associated with better visual outcomes after treatment [35].
Systemic safety of anti-VEGF therapy in patients with DME
Intravitreal anti-VEGF therapy is commonly used to treat numerous retinal conditions, including DME, and appears safe; however, its systemic safety remains controversial. In a systematic review and meta-analysis reported in 2016, randomized clinical studies were selected that evaluated monthly anti-VEGF injections for DME for 2 years and reported the following outcome measures: cerebrovascular accidents, myocardial infarctions, arteriothrombotic events, and mortality. Four studies were selected for the meta-analysis that met the search criteria: 2 trials reporting the use of monthly aflibercept and 2 trials reporting the use of monthly ranibizumab. The four studies enrolled 1328 patients in total. The assessment of the highest-level exposure group (high-risk patients with DME who received monthly treatment for 2 years) revealed a potential increase in the risks of death and cerebrovascular accidents (Table 1) [36]. In addition, a recent Cochrane meta-analysis of anti-VEGF therapies (ranibizumab, aflibercept, bevacizumab, and pegaptanib) for DME analyzed 24 studies with 6007 participants. This report concluded no differences in the overall safety between the anti-VEGF therapies, but it demonstrated that the estimates were imprecise for cardiovascular events and death [37].
Expert review
The efficacy and safety of intravitreal injection of two anti-VEGFs, ranibizumab and aflibercept, for center-involved DME have been proven by many large randomized controlled studies with a high evidence level. Some studies were conducted in non-Japanese populations. However, two randomized controlled studies with similar study design, RESTORE and REVEAL, were conducted in European and Asian population (including Japanese patients) and demonstrated that the general results of anti-VEGF therapy were applicable to various racial and ethnic groups. Consequently, the intravitreal injection of the anti-VEGF agents, ranibizumab or aflibercept, is the current definitive first-line therapy for center-involved DME in the Japanese real-world clinical setting.
There are no definitive criteria for selecting ranibizumab or aflibercept for the treatment of center-involved DME. The results of the DRCR.net Protocol T suggested that aflibercept was superior to ranibizumab for the treatment of DME, and some retrospective and prospective studies have indicated the usefulness of switching from ranibizumab to aflibercept for the treatment of resistant DME associated with poor vision. These hypotheses could be explained by the different molecular structure [38], greater binding affinity [39], and/or the longer intravitreal bioavailability of aflibercept compared with other anti-VEGFs [40]. Therefore, although there is limited evidence, aflibercept is recommended especially for the treatment of severe or resistant DME.
Findings from the randomized clinical studies of anti-VEGF therapies mentioned above strongly support the use of anti-VEGF therapies for the management of center-involved DME with vision impairment. However, in the post hoc, exploratory analysis of Protocol I from the DRCR.net, less than half of the eyes treated for DME with anti-VEGF therapy, had persistent DME at 6 months after the initiation of treatment. Among these, 40% then had chronic persistent DME throughout 3 years [41]. A similar prevalence of chronic persistent DME through 2 years was also reported from the post-hoc analysis of Protocol T from the DRCR.net [42]. The identification of risk factors that can predict treatment success or failure will help investigators in making informed decisions as to which patients should be treated with each therapy. As introduced above, there are many reports suggesting the predictive factors associated with the outcomes of anti-VEGF therapy for DME. Additionally, two studies (one that was conducted in Japan) demonstrated that an early response to anti-VEGF therapy (change in visual acuity from baseline to month 3) may predict the visual outcome after 1 year in DME patients treated with anti-VEGF therapy (Fig. 4) [43, 44].
Correlation between early response to anti-VEGF therapy (change in visual acuity from baseline to month 3) and visual outcome at year 1 in Japanese DME patients treated with anti-VEGF [44]. BCVA, best-corrected visual actuity; ΔBCVAM3, logMAR BCVA change from baseline to month 3; ΔBCVAM12, logMAR BCVA change from baseline to month 12; logMAR, logarithm of the minimum angle of resolution. The figure is reprinted with the permission from the publisher of original article
In a recent retrospective study of 21 eyes in DME patients who received anti-VEGF injections, Mori et al. reported that the number of microaneurysms detected by indocyanine green angiography may be useful predictors of DME recurrence [45].
Serious ocular adverse events of intravitreal anti-VEGF injections occur at a low frequency and include endophthalmitis, uveitis, and retinal detachment; likewise, the risk of occurrence does not appear to be greater in patients with center-involved DME than in patients with AMD. The serious systemic adverse events of intravitreal anti-VEGF injections include death, myocardial infarction, and stroke. A systematic review and meta-analysis of four randomized clinical studies with 1328 patients indicated that high-risk patients with DME who received 2 years of monthly treatment may have an increased risk of death and potential cerebrovascular accidents. The risks of occurrence of these systemic adverse events appeared to be slightly higher in patients with center-involved DME than in patients with AMD. Moreover, a recent Cochrane meta-analysis of anti-VEGF therapies failed to identify issues regarding the systemic events related to intravitreal anti-VEGF injection. The risks of occurrence of serious ocular and systemic adverse events after anti-VEGF therapy are different for each patient with center-involved DME; therefore, physicians should use anti-VEGF for center-involved DME after careful consideration of the risks of these adverse events. The recent Protocol V from the DRCR Retina Network addressed the best therapeutic strategy for eyes with center-involved DME and good vision (20/25 or better). After 2 years, the visual outcomes were similar in all three groups. Given the costs and potential adverse events associated with the intravitreal injections of anti-VEGF, observation is suggested to be a reasonable initial strategy for treatment-naïve eyes with good vision, despite the presence of center-involved DME, as long as the eyes are followed closely and treated with anti-VEGF therapy if vision worsens.
Laser photocoagulation therapy
Focal/grid laser photocoagulation was the standard of care for the treatment of DME from 1985 to 2010 [11]. As intravitreal anti-VEGF injection has replaced laser photocoagulation as the standard of care for DME, laser photocoagulation therapy remains an important treatment option for DME because this therapy is cheaper and often requires significantly fewer patient visits. Moreover, it does not have the potential for systemic cardiovascular side effects, such as stroke, along with local risks, such as endophthalmitis, cataracts, and retinal tear or detachment [8].
Recently, some studies have suggested the clinical usefulness of laser and anti-VEGF therapy combination; following the development of new laser technologies such as the subthreshold micropulse laser and the Navilas navigated laser, laser photocoagulation is once again becoming an attractive therapeutic option. In this section, we have especially summarized the latest developments in laser photocoagulation therapy for DME.
Laser and anti-VEGF therapy combination
In a 5-year follow-up of the Protocol I from the DRCR.net, visual benefit and the number of ranibizumab injections were compared between ranibizumab administered PRN with prompt versus deferred (for ≥ 24 weeks) focal/grid laser treatment for DME. The mean change in visual acuity letter score from baseline to the 5-year visit tended to be superior in the ranibizumab with deferred laser group than in the ranibizumab with prompt laser group, with + 9.8 letters versus + 7.2 letters, respectively (p = 0.09). The significant difference in favor of the deferred laser group versus the prompt laser group was observed after 5 years among the subgroup of eyes with worse visual acuity at baseline (approximate Snellen equivalent less than 20/50) (p < 0.001). The median number of injections was 17 versus 13 in the deferred and prompt laser groups, respectively [15].
A retrospective study compared a group of 19 eyes with DME treated with ranibizumab injections plus subthreshold micropulse laser versus a matched control group of 19 eyes with DME treated with ranibizumab injections without the laser. At 12 months, the subthreshold micropulse laser with ranibizumab was a safe and effective treatment for DME, and achieved comparable improvement in visual acuity, along with a significant reduction in the burden of ranibizumab injections compared with the control group (1.7 ± 2.3 versus 5.6 ± 2.1) [46]. Recently, precise focal laser photocoagulation using Navilas combined with ranibizumab therapy (PRN) was shown to have promising efficacy while reducing the burden of the ranibizumab injections in a 1-year prospective study (Table 2) [47]. In addition, a retrospective study also determined the long-term visual gains and injection requirements in the 3-year follow-up period. The combination of Navilas navigated laser and ranibizumab achieved the best corrected visual acuity gains equivalent to ranibizumab monotherapy at year 1, and the results were maintained through to year 3. The required injections were 2.0 times fewer in year 1 and a further 1.3 times fewer in years 2 and 3, in the combination group compared with the monotherapy group [48].
A multicenter prospective randomized clinical study, the TREX-DME study, was conducted to compare monthly dosing versus a TAE algorithm using ranibizumab with and without Navilas navigated laser photocoagulation for DME. In total, 150 eyes from 116 patients were randomized in this study, and the TAE dosing of ranibizumab with and without Navilas significantly decreased the number of injections given and provided similar visual and anatomic outcomes compared with monthly dosing. The addition of Navilas to this dosing algorithm did not significantly improve outcomes at 1 and 2 years [49, 50]. More recently, Inagaki et al. reported that the combination of intravitreal anti-VEGF and minimally invasive laser therapy, including Navilas navigated laser photocoagulation improves the visual acuity, alleviates DME, and may decrease the required number of anti-VEGF injections in a retrospective 1-year study [51].
A 6-month randomized controlled study was conducted in Japan to investigate whether targeted retinal photocoagulation (TRP) for nonperfused areas (NPAs) could have a preventive effect on the recurrence of DME after the intravitreal injection of bevacizumab (not approved in Japan for the indication of DME) in 52 patients with DME. Combination therapy with TRP and bevacizumab for NPAs was more effective for the maintenance of reduced central retinal thickness after grid/focal photocoagulation for patients with DME [52]. Further, in a 3-year randomized controlled study, DAVE to evaluate the effect of TRP on visual and anatomic outcomes and treatment burden in 40 eyes with DME, it was shown that there was no evidence that combination therapy of ranibizumab and TRP improved visual outcomes or reduced treatment burden compared with ranibizumab alone treatment [53].
Navigated laser treatment
The Navilas laser system, developed recently for the navigated laser treatment, is a computer-based system combined with a wide-angle imaging camera that has become of current interest. The Navilas has eye-tracking laser delivery system that achieves greater accuracy than conventional focal laser therapy for DME [54, 55]. For safety and patient comfort, the main theoretical advantages lie in retinal navigation, and the device offers retinal navigation owing to computerized image and target assistance systems, resulting in high precision and reproducibility, theoretically of < 60–110 μm. Another difference to slit lamp-based laser devices is the touch screen monitor used for imaging, planning, and treating fundus changes. This allows the retina surgeon to plan laser spots on the screen and then apply automated patterns and single spots, as appropriate [56].
In 2013, Neubauer et al. reported the comparison of clinical outcomes and retreatment rates when using the Navilas navigated macular laser compared with conventional macular laser for the treatment of DME. The best corrected visual acuity after 3 months was significantly superior in the Navilas group (n = 46) than in the conventional laser group (n = 28), with fewer retreatments in the Navilas group than in the conventional laser group within the first 8 months (18% versus 31%, respectively) [57]. A retrospective cohort series of 7 patients with DME indicated that focal Navilas was safe and effective for the treatment of DME with improvements in visual acuity and macular edema on optical coherence tomography over 12 months [58]. In 2018, Kato et al. reported that focal photocoagulation using Navilas was effective for the treatment of 25 eyes with refractory DME with improvement in macular edema on optical coherence tomography (OCT) over 6 months. The Navilas navigated laser photocoagulation was delivered to the microaneurysms using indocyanine green angiography (ICGA) in 21 of 25 eyes, fluorescein angiography (FA) guided in 3 eyes, and OCT angiography guided in 1 eye. Navilas was beneficial for navigated laser photocoagulation based on three modalities of ICGA, FA, and OCT angiography [59]. More recently, Nozaki et al. prospectively evaluated the efficacy of ICGA-guided navigated focal laser photocoagulation using Navilas for 8 eyes with DME. After 6 months, ICGA-guided Navilas had significantly reduced the central retinal thickness, the primary endpoint (Fig. 5), and the macular volume, with a significant improvement in the best corrected visual acuity. They also reported that 5 out of the 8 eyes (63%) underwent additional ICGA-guided Navilas focal laser photocoagulation owing to remnants of microaneurysms that had been confirmed by ICGA at 3 months, and there was no observed recurrence of edema after the photocoagulation during the 6-month follow-up [60].
Change in central retinal thickness after the treatment with ICGA-guided Navilas focal laser photocoagulation in 8 eyes with DME [60]. The figure is reprinted with the permission from the publisher of original article
Subthreshold micropulse laser therapy
Conventional laser photocoagulation therapy has a risk of retinal pigment epithelium atrophy, which may potentially induce central scotoma or scar enlargement. However, recently developed subthreshold micropulse laser therapy has fewer such side effects as it delivers laser energy below the threshold required for permanent tissue destruction. Laser parameters, such as wavelength, power, spot size, and pulse duration, can be altered to decrease the amount of thermal energy delivered to reduce permanent tissue damage [61]. A schematic explanation of the difference between the mode of action of conventional and subthreshold micropulse laser is presented in Fig. 6 [62].
Schematic explanation of the difference between the mode of action of conventional and subthreshold micropulse laser [62]. The figure is reprinted with the permission from the publisher of original article
Subthreshold micropulse laser for the treatment of DME has been investigated in some small clinical studies, including randomized controlled studies [63]. It is reported that patients with DME can attain equal, or even better, visual acuity, as well as better preservation of electrophysiologic function after micropulse laser treatment compared with conventional laser therapy [64, 65]. Subthreshold micropulse laser was demonstrated to be effective for the treatment of DME without causing any adverse treatment effects or complications [66, 67]. A prospective case study of 220 patients with DME demonstrated that subthreshold micropulse laser was an effective minimal intensity therapy that offered the clear advantage of minimizing or avoiding laser-induced visible retinal burn/scarring while reducing the foveal thickness in the management of DME [68]. In 2018, Vujosevic et al. reported prospective assessment results for the changes in OCT angiography in 35 eyes with DME treated with subthreshold micropulse laser over a period of 6-month period. Subthreshold micropulse laser led to a reduction in the foveal avascular zone area at the level of the deep capillary plexus, and a reduced number of microaneurysms and area of cysts in both superficial capillary plexus and deep capillary plexus [69]. A recent prospective study was conducted on 10 patients with DME treated with a subthreshold micropulse laser to evaluate changes in the individual retinal layers and to correlate with functional changes. The increase in best corrected visual acuity was significantly and inversely correlated to central retinal thickness, and inner and outer nuclear layer thickness [70].
Panretinal photocoagulation for proliferative diabetic retinopathy associated with DME
The severity of diabetic retinopathy associated with DME is an important factor in deciding a therapeutic strategy. In 1981, the Diabetic Retinopathy Study Research Group reported that panretinal photocoagulation (PRP) for proliferative diabetic retinopathy (PDR) reduced the risk of severe vision loss by 50% or more and that it definitively proved the benefit of PRP for the treatment of PDR [71]. In Japan, the subcommittee of the Japanese Society of Ophthalmic Diabetology conducted a multicenter randomized clinical study of selective PRP for nonperfusion areas in 69 patients with pre-PDR. The incidence of PDR was significantly lower in the PRP treated group than in the non-PRP treated group, and the PRP was shown to be effective for the prevention of PDR development [72].
Intraocular levels of pro-angiogenic factors, particularly VEGF, were reported to be elevated in patients with active PDR, and VEGF plays a major part in the mediation of active intraocular neovascularization of PDR [73]. Recently, some randomized controlled studies have investigated the efficacy of intravitreal anti-VEGF injection in the patients with PDR compared with the efficacy of PRP. The DRCR.net Protocol S showed that ranibizumab therapy was non-inferior to PRP therapy in terms of visual acuity after 2 and 5 years (Fig. 7) [74, 75]. The extent of visual field loss was lower in the ranibizumab group than in the PRP group, but continuing visual field loss was seen in both groups for up to 5 years [75].
Mean change in visual acuity from baseline up to 5 years in the DRCR.net Protocol S [75]. The figure is reprinted with the permission from the publisher of original article
A multicenter, single-blinded randomized controlled study (CLARITY) recruited 232 patients with PDR, and confirmed the non-inferiority of aflibercept compared with PRP. The primary outcome was defined as a change in best-corrected visual acuity at 1 year. Aflibercept was non-inferior and superior to PRP (mean best corrected visual acuity difference 3.9 letters), with no safety concerns [76]. The PROTEUS study, a prospective randomized multicenter open-label phase 2/3 study, compared the efficacy of ranibizumab plus PRP versus PRP alone in regressing the neovascularization area in patients with high-risk PDR over a 1-year period. After 1 year, 92.7% of patients in the ranibizumab plus PRP group presented a significant total reduction of neovascularization versus 70.5% of patients in the PRP alone group, and the mean best corrected visual acuity was 75.2 letters versus 69.2 letters, which was not significantly different. This study demonstrated that the treatment of ranibizumab plus PRP was more effective than PRP alone for neovascularization regression in patients with high-risk PDR over 1 year (Table 3) [77].
As mentioned above, some randomized controlled studies recently demonstrated that intravitreal anti-VEGF injection provided comparable or potentially even superior outcomes to PRP in patients with PDR. However, both therapies required close follow-up to reassess response to therapy, disease progression, and the need for additional treatment to optimize outcomes; therefore, loss to follow-up (LTFU) may contribute to vision loss in patients with active PDR. Obeid et al. determined and compared the rates of LTFU in 1718 patients with PDR receiving anti-VEGF or PRP over approximately 4 years and reported that a large proportion of patients with PDR were LTFU after receiving both therapies [78]. The authors also compared anatomic and functional outcomes in 76 eyes of 59 patients with PDR that were LTFU for more than 6 months after treatment with either anti-VEGF injection or PRP. Eyes with PDR that received only intravitreal anti-VEGF demonstrated worse anatomic and functional outcomes following LTFU compared with eyes that received PRP (Fig. 8) [79].
Change in visual acuity after being LTFU in eyes with PDR receiving either intravitreal anti–VEGF or PRP [79]. LTFU, lost to follow-up. p values on the line graphs represent statistical comparisons with the visit before being LTFU. p values above the designated visits represent statistical comparisons between the treatment arms at the given time points. The figure is reprinted with the permission from the publisher of original article
Expert review
For the laser and anti-VEGF therapy combination, a 5-year follow-up of the Protocol I from the DRCR.net suggested that ranibizumab with deferred (for ≥ 24 weeks) focal/grid laser treatment for DME was superior to ranibizumab with prompt focal/grid laser treatment, especially among the subgroup of eyes with worse visual acuity at baseline (approximate Snellen equivalent less than 20/50) [15]. There was no other evidence to support this finding; however, this finding was considered as a high-quality evidence, and we therefore can refer this finding when selecting the combination treatment strategy in real-world clinical practice.
Hirano et al. reported that eyes with perifoveal leaking microaneurysms required a larger number of anti-VEGF injections, even when combined with focal/grid laser treatment, owing to the fact that the focal/grid laser can only be applied to the outside of the fovea [80]. The utilization of a precise focal laser with Navilas is useful for the treatment of perifoveal microaneurysms, and this hypothesis is supported by the evidence that the additional ICGA-guided Navilas focal laser photocoagulation for the remnants of microaneurysms was effective for preventing the recurrence of edema after photocoagulation [60].
It has been reported that the efficacy of subthreshold micropulse laser for the treatment of DME was influenced by pretreatment central foveal thickness (CFT) [81]. This report suggested that subthreshold micropulse laser treatment was less effective in DME patients with a baseline CFT of > 400 μm. Therefore, we recommend the therapeutic option of subthreshold micropulse laser and anti-VEGF therapy combination in DME patients with a baseline CFT of > 400 μm in clinical practice.
Some recent randomized controlled studies have demonstrated that intravitreal anti-VEGF injection provides comparable or even potentially superior outcomes to PRP in patients with PDR. However, as Obeid et al. reported [78, 79], given the potential sequelae of being LTFU, the choice of treatment for PDR must be considered carefully.
With the development of these new technologies, laser photocoagulation therapy has become more efficient and effective with less pain and fewer adverse events. We believe that the further accumulation of evidence for utilizing these new technologies may contribute to continuing innovations in laser technology. Additionally, the progress in understanding laser-tissue interactions make us believe that laser therapy will continue to play a critical role in the treatment of retinal disease for many years to come.
Steroid therapy
The use of the intravitreal injection of triamcinolone acetonide for the treatment of DME was first reported in 2001 [82]. This therapy was effective for the treatment of DME, but the complications of intravitreal triamcinolone therapy included secondary ocular hypertension in approximately 40% of the injected eyes, cataracts, and postoperative infectious or noninfectious endophthalmitis. After the introduction of anti-VEGF therapy into clinical practice for DME, intravitreal triamcinolone has lost its prime position as the drug most often injected intravitreally [83]. However, owing to its widespread biological effects as a steroid, the relatively large therapeutic window, and cost-effectiveness, triamcinolone therapy has remained essential for clinical use in patients with DME [83]. In this section, we have summarized the evidences for the steroid therapy, with a particular focus on the evidences important for the real-world management of DME.
Intravitreal steroid therapy for pseudophakic eyes with DME
A subgroup analysis of Protocol I from the DRCR.net demonstrated that by limiting the analysis to 273 eyes that were pseudophakic at baseline, the pseudophakic eyes at baseline in the triamcinolone with prompt laser group, visual acuity results appeared comparable with those of the pseudophakic eyes in the ranibizumab with prompt laser groups, and superior to that of the pseudophakic eyes in the sham with prompt laser group after 2 years (Fig. 9) [14].
Mean change in visual acuity at follow-up visits among eyes that were pseudophakic at baseline in the Protocol I from the DRCR.net [14]. The figure is reprinted with the permission from the publisher of original article
Steroid and anti-VEGF therapy combination
The Cochrane database of systematic review published in 2018 reported that the combination of intravitreal anti-VEGF plus intravitreal steroid did not appear to offer additional visual benefits compared with monotherapy for DME; at present, the evidence for this is of low certainty. There was an increased rate of cataract development and increased intraocular pressure in eyes treated with anti-VEGF plus steroid versus anti-VEGF alone (Fig. 10) [84].
Forest plot of comparison for the adverse events: intravitreal anti-VEGF plus intravitreal steroid versus intravitreal anti-VEGF alone for the treatment of DME in a Cochrane database of systematic review [84]. The figure is reprinted with the permission from the publisher of original article
Some studies have demonstrated that subtenon injection of triamcinolone is effective for the reduction DME [85,86,87]. Shimura et al. treated 124 eyes with DME with subtenon injection of triamcinolone, and investigated the influence of triamcinolone reflux after the injection on the regression of DME and postoperative intraocular pressure. They demonstrated that triamcinolone reflux after subtenon injection was a risk factor not only for the insufficient reduction of edema but also for the postoperative intraocular pressure elevation in eyes with DME [87]. In 2016, Shimura et al. also reported that the adjunctive subtenon injection of triamcinolone to intravitreal anti-VEGF injection for the treatment of DME not only improved the morphological and functional regression but also reduced the frequency of intravitreal anti-VEGF therapy (Fig. 11) [88].
Visual acuity and frequency of intravitreal anti-VEGF treatments after adjunctive subtenon injection of triamcinolone to intravitreal anti-VEGF versus intravitreal anti-VEGF alone for the treatment of DME [88]. IVB, intravitreal bevacizumab; STTA, subtenon injection of triamcinolone. *Statistically significant difference between two treatment groups at each time point. The figure is reprinted with the permission from the publisher of original article
Expert review
Serial injections of anti-VEGF therapy are the first-line therapy for DME, and the intravitreal injection of triamcinolone has a secondary role in particular cases. We believe that DME patients with pseudophakic eyes may be treated with intravitreal injections of triamcinolone because as described above, a subgroup analysis of Protocol I from the DRCR.net suggested that intravitreal injection of triamcinolone may have similar effects for improving visual acuity compared with anti-VEGF in pseudophakic eyes with DME. There is no obvious evidence for supporting the usefulness of intravitreal triamcinolone and anti-VEGF combination therapy for DME. Some evidences support the usefulness of subtenon injection of triamcinolone for DME, as described above. In addition, a prospective study was conducted to evaluate the efficacy of subtenon injection of triamcinolone against PRP-induced macular thickening and visual disturbance in 20 eyes of patients with severe diabetic retinopathy and good vision. As a pretreatment for PRP, a single subtenon injection of triamcinolone had beneficial effects for the prevention of PRP-induced foveal thickening and visual dysfunction in patients with severe diabetic retinopathy and good vision (Fig. 12) [89]. Subtenon injection of triamcinolone may also be useful for the prevention of PRP-induced macular thickening and visual disturbance in PDR associated with DME.
Efficacy of subtenon injection of triamcinolone against panretinal photocoagulation-induced macular thickening and visual disturbance in eyes with severe diabetic retinopathy and good vision [89]. STTA, subtenon injection of triamcinolone. *Statistically significant difference between the STTA injected and control eyes at each time point. The figure is reprinted with the permission from the publisher of original article
Recently, Protocol U from the DRCR.net enrolling patients with persistent DME demonstrated that the addition of an intravitreal dexamethasone sustained release device (Ozurdex®) to a regimen of intravitreal ranibizumab injection did not improve visual acuity outcomes after 6 months, although macular thinning was greater than that with intravitreal ranibizumab injection alone [90]. Although this was a phase 2 study with a relatively small number of patients, it was decided that additional therapeutic studies on this topic were not indicated because of the difficulty in recruitment, and because of the continued improvement of many eyes after 6 months of treatment with anti-VEGF therapy alone [91]. In Japan, Ozurdex is not approved, but a preservative-free formulation of triamcinolone acetonide (MaQaid® 40 mg/vial; Wakamoto Pharmaceutical, Tokyo, Japan) has been approved for intravitreal and subtenon injections.
Pars plana vitrectomy
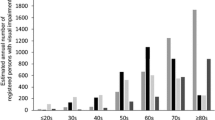
Pars plana vitrectomy for DME was first reported by Lewis et al. in 1992, and they reported that vitrectomy was effective in 10 eyes with DME and traction associated with a thickened and taut premacular posterior hyaloid [92]. Tachi et al. first showed that vitrectomy with posterior vitreous detachment was effective in eyes with diffuse DME without posterior vitreous detachment [93]. Although the precise mechanism by which vitrectomy exerts the efficacy remains to be unclear, many reports indicate that vitrectomy was effective for the improvement of macular edema and visual acuity in patients with DME [94,95,96,97,98,99,100,101]. In 2010, a prospective observational study performed by the DRCR.net was reported, and vitrectomy for DME was evaluated in 87 DME eyes with at least moderate vision loss and vitreomacular traction. At 6 months, visual acuity improved by ≥ 10 letters in 38% of the DME patients and deteriorated by ≥ 10 letters in 22% of the DME patients (Fig. 13). Median OCT central subfield thickness significantly decreased by 160 μm from baseline, with 43% of patients having central subfield thickness of < 250 μm and 68% of patients having at least a 50% reduction in thickening. Eyes with greater central subfield thickness at baseline had a significantly greater reduction in thickness after vitrectomy for DME (Fig. 14). Postoperative complications through 6 months included vitreous hemorrhage (5 eyes), elevated intraocular pressure requiring treatment (7 eyes), retinal detachment (3 eyes), and endophthalmitis (1 eye). Similar results were also observed at 1 year [102].
Distribution of change in visual acuity from baseline in the DRCR.net study [102]. The figure is reprinted with the permission from the publisher of original article
Distribution of change in optical coherence tomography central subfield thickness in categories according to baseline thickness in the DRCR.net study [102]. The figure is reprinted with the permission from the publisher of original article
A systematic review and meta-analysis from 11 randomized controlled studies concluded that there was little evidence to support vitrectomy as an intervention for DME in the absence of the epiretinal membrane or vitreomacular traction. Although vitrectomy appeared to be superior to laser in its effects on retinal structure at 6 months, no such benefit was proved at 12 months. There was no evidence to suggest the superiority of vitrectomy over laser in terms of functional outcomes (Fig. 15) [103].
A systematic review and meta-analysis for the effects of vitrectomy versus laser therapy on structural (a) and functional (b) outcomes at 6 months [103]. a Trans pars plana vitrectomy (TPPV) versus laser. Structural (reduction in foveal thickness) outcomes at 6 months (positive values better). b TPPV versus laser. Functional (likelihood of achieving ≥ 2 lines improvement in acuity) outcomes at 6 months. The figure is reprinted with the permission from the publisher of original article
The European Vitreo-Retinal Society (EVRS) conducted the EVRS Macular Edema Study, a non-randomized multicenter study in which a total of 86 retina specialists from 29 countries provided information on 2603 patients with macular edema including 870 patients with DME, with a follow-up of at least 6 months. In this study, the efficacy of different therapies for DME was compared. Treatment with vitrectomy and internal limiting membrane peeling alone resulted in better visual improvement than with other therapies, including intravitreal triamcinolone monotherapy, treatment with threshold or subthreshold grid laser, and intravitreal anti-VEGF monotherapy (Fig. 16) [104].
Change in visual acuity (in lines) after different monotherapies for DME in the EVRS Macular Edema Study [104]. The figure is reprinted with the permission from the publisher of original article
Expert review
As described above, many studies have indicated that pars plana vitrectomy is effective for the treatment of DME. However, serial injections of anti-VEGF therapy are the first-line therapy for DME at present, and the target patients of vitrectomy are limited to patients with DME that have vitreomacular traction and/or epiretinal membrane detected by OCT in current practice in Japan [105]. The efficacy and safety of vitrectomy for the treatment of DME with vitreomacular traction were reported in a prospective observational study performed by the DRCR.net described above [102]. Thirty-four eyes with resistant DME treated with vitrectomy were investigated for the predictors of visual improvement using spectral-domain OCT in a retrospective manner. This study indicated that the evaluation of epiretinal membrane preoperatively predicted the vision improvement more accurately than the photoreceptor inner segment/outer segment junction and central macular thickness in eyes with DME treated with vitrectomy [106]. These two studies support the use of vitrectomy for the treatment of DME especially with a vitreomacular traction and/or epiretinal membrane.
Preoperative factors on the foveal thickness following vitrectomy for DME were investigated, and the decrease in foveal thickness was reported to be related to the preoperative glycemic control [95]. Yamada et al. also reported that improvement for the best corrected visual acuity and central subfield macular thickness after the vitrectomy was significantly associated with postoperative glycemic control and that glycemic control was important for ocular outcomes after vitrectomy for DME [107]. We think that vitrectomy may be a suitable treatment option for DME patients who did not respond to anti-VEGF therapy or had multiple relapses after the anti-VEGF therapy with sufficient glycemic control. A sub-analysis of Protocol I from the DRCR.net demonstrated that a larger visual acuity treatment benefit of anti-VEGF therapy for DME was associated with younger age, less severe diabetic retinopathy, and the absence of surface wrinkling retinopathy [31]. Therefore, vitrectomy may also be a treatment option for DME patients with older age, more severe diabetic retinopathy, and the presence of surface wrinkling retinopathy. Anti-VEGF therapy can also be a treatment option, even for vitrectomized DME eyes, because the difference in the effectiveness of anti-VEGF therapy between DME eyes with and without previous vitrectomy was reported to be not significant in the prospective study [108]. This is also supported from an exploratory post hoc assessment of 3-year data from eyes with and without vitrectomy before randomization in a DRCR.net trial [109].
In a multicenter, prospective, controlled clinical trial, the benefits and potential complications of the use of triamcinolone acetonide (TA) in vitrectomy were evaluated in 774 patients from 8 Japanese hospitals: 391 patients underwent TA-assisted vitrectomy and 383 control patients underwent conventional vitrectomy. The incidence of both retinal breaks and intraoperative retinal detachment was significantly lower in TA-assisted vitrectomy than in conventional vitrectomy, and there were no serious adverse events related to the intraoperative use of TA [110]. This evidence suggested the benefits of using TA in vitrectomy, although more careful control of intraocular pressure is required than for conventional vitrectomy.
A standard protocol for pars plana vitrectomy has not been established. In a prospective observational study performed by the DRCR.net described above, general guidelines for pars plana vitrectomy included (1) three pars plana sclerotomies, (2) the removal of the vitreous gel with peeling of the posterior hyaloid, if attached, and removal of the peripheral vitreous leaving only a small residual vitreous skirt, (3) engagement and peeling of epiretinal membranes judged visually significant, and (4) examination of the peripheral retina at the close of the procedure and treatment of peripheral breaks with laser or cryotherapy [102]. These general guidelines may provide a reference for performing vitrectomy in clinical practice.
Recommendation for a therapeutic flow chart for DME
In this chapter, we have proposed the recommended therapeutic flow chart for DME (Fig. 17), after consideration of the recent clinical evidences reviewed in Chapters I to IV.
Recommended therapeutic flow chart for DME. *Microaneurysm related to macular edema. NPDR, non PDR; CI, center-involved DME; Non-CI, non-center-involved DME; VMT, vitreomacular traction; EPM, epiretinal membrane; IOL, intraocular lens. The figure is reprinted with the permission from the publisher of original article
Intravitreal injection of anti-VEGF agents, ranibizumab or aflibercept, should generally be the first-line therapy for center-involved DME (see Expert review of Chapter I). For the selection of ranibizumab or aflibercept, there are currently no definitive criteria. With the presence of perifoveal leaking microaneurysms related to macular edema, focal laser photocoagulation is recommended as an additional therapeutic option to anti-VEGF therapy (see Expert review of Chapter II). Furthermore, depending on the patient’s condition of DME, such as the existence of PDR and vitreomacular traction/epiretinal membrane, and non-center-involved DME, additional and/or alternative treatments for anti-VEGF therapy should be considered, with the aim of effective disease control and function improvement (see Expert review of Chapters II to IV).
PDR, as well as DME, is a vision-threatening diabetic retinopathy. For patients with both PDR and DME, simultaneous interventions for these two disease conditions are needed to prevent vision loss. Instead of conventional PRP monotherapy, the combination of pharmacotherapy and PRP has become the predominant therapy for PDR along with the advent of anti-VEGF agents or steroids (see Expert review of Chapter II). The DRCR.net Protocol S showed that anti-VEGF therapy was non-inferior to PRP therapy in terms of the improvement of visual acuity and the prevention of PDR-related complications (see 4th section of Chapter II). However, poor prognosis has also been reported in some dropout cases. Based on these evidences, anti-VEGF therapy combined with PRP at the appropriate timing for achieving vision improvement and for lowering the risk of serious complications accompanying PDR was a rational therapeutic approach for DME patients with PDR. Moreover, the benefits of anti-VEGF therapy combined with PRP for patients with high-risk PDR have been addressed by the PROTEUS study. With regard to the combination of the subtenon injection of triamcinolone and PRP treatment, this is less evidence for its long-term effectiveness. In our clinical experience, PRP monotherapy often induces severe inflammation, and therefore, the subtenon injection of triamcinolone is believed to be useful for the suppression of PRP-induced inflammation (see Expert review of Chapter III). Further prospective studies to investigate the long-term efficacy of subtenon injection of triamcinolone and PRP treatment are expected in the future.
Non-center-involved DME without PDR should be treated by photocoagulation, as clinically significant macular edema. Among non-center-involved DME, photocoagulation is reported to be highly effective in patients with circinate retinopathy from the finding that the circinate complex was eliminated in 23 of the 24 treated eyes (96%) [111]. For the presence of perifoveal leaking microaneurysms related to macular edema, focal laser photocoagulation is recommended. The utilization of a precise focal laser with Navilas is expected to be useful for the treatment of perifoveal microaneurysms; however, more prospective studies are necessary to verify the efficacy of this new therapy (see Expert review of Chapter II).
For cases of diffuse macular edema without obvious microaneurysms related to macular edema, conventional grid laser photocoagulation treatment has been employed. However, the laser photocoagulation of the retinal pigment epithelium has a risk of the possible development of atrophic creep during a long course of therapy. New technologies, including subthreshold and micropulse laser therapy, is expected to be useful for the treatment of diffuse macular edema without obvious microaneurysms, although further assessments are needed to confirm their potential efficacy and safety (see 3rd section of Chapter II).
Vitrectomy is recommended for the treatment of DME especially with vitreomacular traction and/or epiretinal membrane, and it is the only way to treat complicated vitreoretinal disorders (see Expert review of Chapter IV). The DRCR.net Protocol D confirmed the beneficial result of the vitrectomy with epiretinal membrane peeling for visual improvement. In a subgroup analysis of the DRCR.net Protocol I, no statistically significant differences have been observed between the vitrectomized eyes and the non-vitrectomized eyes with regard to vision improvement and the decreased number of injections related to anti-VEGF therapy. Therefore, it is reasonable to perform vitrectomy before anti-VEGF treatment for patients with vitreomacular abnormalities. Postoperative treatment with anti-VEGF or triamcinolone should also be considered when DME persists after vitrectomy.
Anti-VEGF therapy is the first-line treatment for general DME without PDR. When obvious microaneurysms related to macular edema are present, deferred focal laser photocoagulation should be added to anti-VEGF therapy; the anti-VEGF therapy can first be used to gain an overall improvement, and then additional focal laser photocoagulation can be used to improve persistently leaking microaneurysms. Two evidences support this therapy procedure. One is that the occlusion of microaneurysms or the suppression of microaneurysms leakage in response to anti-VEGF therapy has often been observed. The other is the long-term outcome of deferred focal laser photocoagulation superior to that of prompt focal laser photocoagulation in the DRCR.net Protocol I (see Expert review of Chapter II). Further studies are expected to help develop a useful method for the identification of the microaneurysms related to macular edema and optimize the timing of the addition of focal laser photocoagulation.
For DME patients with pseudophakic eyes, triamcinolone could be considered as an alternative treatment of anti-VEGF agents, of which the socioeconomic burden is great. According to the post hoc analysis of the DRCR.net Protocol I, there was no statistically significant difference in the effect on improving visual acuity between the intravitreal injections of triamcinolone and the anti-VEGF agent combined with laser photocoagulation in pseudophakic eyes with DME. The socioeconomic burden is low in triamcinolone treatment; however, close attention should be paid to the occurrence of adverse events, such as glaucoma and ocular hypertension. Although remarkable progress has taken in microincision glaucoma surgery (MIGS), appropriate informed consent is of great significance (see Expert review of Chapter III). The identification of the prognostic factors for pharmacotherapy is expected to optimize the selection of an appropriate pharmacotherapy for individual patients with DME.
Conclusions
It is our strong desire that the treatment outcome of DME in real-world clinical practice is further improved by the selection and performance of the most appropriate therapies for individual patients with DME based on high-quality and most recent clinical evidences. We believe that our review of clinical evidence and the recommended therapeutic flow chart for DME will help for achieving better treatment outcomes for DME.
References
Tan GS, Cheung N, Simó R, Cheung GC, Wong TY (2017) Diabetic macular oedema. Lancet Diabetes Endocrinol 5:143–155
Miller K, Fortun JA (2018) Diabetic macular edema: current understanding, pharmacologic treatment options, and developing therapies. Asia Pac J Ophthalmol (Phila) 7:28–35
Kodjikian L, Bellocq D, Bandello F, Loewenstein A, Chakravarthy U, Koh A, Augustin A, de Smet MD, Chhablani J, Tufail A, García-Layana A, Sudhalkar A, Mathis T (2019) First-line treatment algorithm and guidelines in center-involving diabetic macular edema. Eur J Ophthalmol 29:573–584
Bandello F, Cunha-Vaz J, Chong NV, Lang GE, Massin P, Mitchell P, Porta M, Prünte C, Schlingemann R, Schmidt-Erfurth U (2012) New approaches for the treatment of diabetic macular oedema: recommendations by an expert panel. Eye (Lond) 26:485–493
Kim EJ, Lin WV, Rodriguez SM, Chen A, Loya A, Weng CY (2019) Treatment of diabetic macular edema. Curr Diab Rep 19:68
Crosson JN, Mason L, Mason JO (2017) The role of focal laser in the anti-vascular endothelial growth factor era. Ophthalmol Eye Dis 21:1179172117738240
Blindbaek SL, Peto T, Grauslund J (2019) How do we evaluate the role of focal/grid photocoagulation in the treatment of diabetic macular edema? Acta Ophthalmol 97:339–346
Li J, Paulus YM (2018) Advances in retinal laser therapy. Int J Ophthalmic Res 4:259–264
Haritoglou C, Maier M, Neubauer AS, Augustin AJ (2020) Current concepts of pharmacotherapy of diabetic macular edema. Expert Opin Pharmacother 21:467–475
Berrocal MH, Acaba LA, Chenworth ML (2019) Surgical innovations in the treatment of diabetic macular edema and diabetic retinopathy. Curr Diab Rep 19:106
Early Treatment Diabetic Retinopathy Study research group (1985) Photocoagulation for diabetic macular edema. Early treatment diabetic retinopathy study report number 1. Arch Ophthalmol 103:1796–1806
Dugel PU, Layton A, Varma RB (2016) Diabetic macular edema diagnosis and treatment in the real world: an analysis of Medicare claims data (2008 to 2010). Ophthalmic Surg Lasers Imaging Retina 47:258–267
Jiang S, Barner JC, Park C, Ling YL (2015) Treatment patterns of anti-vascular endothelial growth factor and laser therapy among patients with diabetic macular edema. J Manag Care Spec Pharm 21:735–741
Diabetic Retinopathy Clinical Research Network, Elman MJ, Aiello LP, Beck RW, Bressler NM, Bressler SB, Edwards AR, Ferris FL 3rd, Friedman SM, Glassman AR, Miller KM, Scott IU, Stockdale CR, Sun JK (2010) Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 117:1064–1077
Elman MJ, Ayala A, Bressler NM, Browning D, Flaxel CJ, Glassman AR, Jampol LM, Stone TW, Diabetic Retinopathy Clinical Research Network (2015) Intravitreal ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: 5-year randomized trial results. Ophthalmology 122:375–381
Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO, Sutter F, Simader C, Burian G, Gerstner O, Weichselberger A, RESTORE study group (2011) The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology 118:615–625
Schmidt-Erfurth U, Lang GE, Holz FG, Schlingemann RO, Lanzetta P, Massin P, Gerstner O, Bouazza AS, Shen H, Osborne A, Mitchell P, RESTORE Extension Study Group (2014) Three-year outcomes of individualized ranibizumab treatment in patients with diabetic macular edema: the RESTORE extension study. Ophthalmology 121:1045–1053
Ishibashi T, Li X, Koh A, Lai TY, Lee FL, Lee WK, Ma Z, Ohji M, Tan N, Cha SB, Shamsazar J, Yau CL, REVEAL Study Group (2015) The REVEAL study: ranibizumab monotherapy or combined with laser versus laser monotherapy in Asian patients with diabetic macular edema. Ophthalmology 122:1402–1415
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, Gibson A, Sy J, Rundle AC, Hopkins JJ, Rubio RG, Ehrlich JS, RISE and RIDE Research Group (2012) Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 119:789–801
Brown DM, Nguyen QD, Marcus DM, Boyer DS, Patel S, Feiner L, Schlottmann PG, Rundle AC, Zhang J, Rubio RG, Adamis AP, Ehrlich JS, Hopkins JJ, RIDE and RISE Research Group (2013) Long-term outcomes of ranibizumab therapy for diabetic macular edema: the 36-month results from two phase III trials: RISE and RIDE. Ophthalmology 120:2013–2022
Prünte C, Fajnkuchen F, Mahmood S, Ricci F, Hatz K, Studnička J, Bezlyak V, Parikh S, Stubbings WJ, Wenzel A, Figueira J, RETAIN Study Group (2016) Ranibizumab 0.5 mg treat-and-extend regimen for diabetic macular oedema: the RETAIN study. Br J Ophthalmol 100:787–795
Korobelnik JF, Do DV, Schmidt-Erfurth U, Boyer DS, Holz FG, Heier JS, Midena E, Kaiser PK, Terasaki H, Marcus DM, Nguyen QD, Jaffe GJ, Slakter JS, Simader C, Soo Y, Schmelter T, Yancopoulos GD, Stahl N, Vitti R, Berliner AJ, Zeitz O, Metzig C, Brown DM (2014) Intravitreal aflibercept for diabetic macular edema. Ophthalmology 121:2247–2254
Brown DM, Schmidt-Erfurth U, Do DV, Holz FG, Boyer DS, Midena E, Heier JS, Terasaki H, Kaiser PK, Marcus DM, Nguyen QD, Jaffe GJ, Slakter JS, Simader C, Soo Y, Schmelter T, Yancopoulos GD, Stahl N, Vitti R, Berliner AJ, Zeitz O, Metzig C, Korobelnik JF (2015) Intravitreal aflibercept for diabetic macular edema: 100-week results from the VISTA and VIVID Studies. Ophthalmology 122:2044–2052
Heier JS, Korobelnik JF, Brown DM, Schmidt-Erfurth U, Do DV, Midena E, Boyer DS, Terasaki H, Kaiser PK, Marcus DM, Nguyen QD, Jaffe GJ, Slakter JS, Simader C, Soo Y, Schmelter T, Vitti R, Berliner AJ, Zeitz O, Metzig C, Holz FG (2016) Intravitreal aflibercept for diabetic macular edema: 148-week results from the VISTA and VIVID studies. Ophthalmology 123:2376–2385
Baker CW, Glassman AR, Beaulieu WT, Antoszyk AN, Browning DJ, Chalam KV, Grover S, Jampol LM, Jhaveri CD, Melia M, Stockdale CR, Martin DF, Sun JK, Retina Network DRCR (2019) Effect of initial management with aflibercept vs laser photocoagulation vs observation on vision loss among patients with diabetic macular edema involving the center of the macula and good visual acuity: a randomized clinical trial. JAMA 321:1880–1894
Wells JA, Glassman AR, Ayala AR, Jampol LM, Aiello LP, Diabetic Retinopathy Clinical Research Network et al (2015) Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med 372:1193–1203
Wells JA, Glassman AR, Ayala AR, Jampol LM, Bressler NM, Bressler SB, Brucker AJ, Ferris FL, Hampton GR, Jhaveri C, Melia M, Beck RW, Diabetic retinopathy Clinical Research Network (2016) Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology 123:1351–1359
Rahimy E, Shahlaee A, Khan MA, Ying GS, Maguire JI, Ho AC, Regillo CD, Hsu J (2016) Conversion to aflibercept after prior anti-vegf therapy for persistent diabetic macular edema. Am J Ophthalmol 164:118–127.e2
Chen YY, Chang PY, Wang JK (2017) Intravitreal aflibercept for patients with diabetic macular edema refractory to bevacizumab or ranibizumab: analysis of response to aflibercept. Asia Pac J Ophthalmol (Phila) 6:250–255
Ibrahim WS, Eldaly ZH, Saleh MG, Rateb MF, Aldoghaimy AH (2019) Switching to aflibercept in diabetic macular edema after unsatisfactory response to other anti-vascular endothelial growth factor drugs. Korean J Ophthalmol 33:122–130
Bressler SB, Qin H, Beck RW, Chalam KV, Kim JE, Melia M, Wells JA 3rd, Diabetic Retinopathy Clinical Research Network (2012) Factors associated with changes in visual acuity and central subfield thickness at 1 year after treatment for diabetic macular edema with ranibizumab. Arch Ophthalmol 130:1153–1161
Sophie R, Lu N, Campochiaro PA (2015) Predictors of functional and anatomic outcomes in patients with diabetic macular edema treated with ranibizumab. Ophthalmology 122:1395–1401
Dhoot DS, Baker K, Saroj N, Vitti R, Berliner AJ, Metzig C, Thompson D, Singh RP (2018) Baseline factors affecting changes in diabetic retinopathy severity scale score after intravitreal aflibercept or laser for diabetic macular edema: post hoc analyses from VISTA and VIVID. Ophthalmology 125:51–56
Murakami T, Suzuma K, Uji A, Yoshitake S, Dodo Y, Fujimoto M, Yoshitake T, Miwa Y, Yoshimura N (2018) Association between characteristics of foveal cystoid spaces and short-term responsiveness to ranibizumab for diabetic macular edema. Jpn J Ophthalmol 62:292–301
Chen YP, Wu AL, Chuang CC, Chen SN (2019) Factors influencing clinical outcomes in patients with diabetic macular edema treated with intravitreal ranibizumab: comparison between responder and non-responder cases. Sci Rep 9:10952
Avery RL, Gordon GM (2016) Systemic safety of prolonged monthly anti-vascular endothelial growth factor therapy for diabetic macular edema: a systematic review and meta-analysis. JAMA Ophthalmol 134:21–29
Virgili G, Parravano M, Evans JR, Gordon I, Lucenteforte E (2017) Anti-vascular endothelial growth factor for diabetic macular oedema: a network meta-analysis. Cochrane Database Syst Rev 22:CD007419
Papadopoulos N, Martin J, Ruan Q, Rafique A, Rosconi MP, Shi E, Pyles EA, Yancopoulos GD, Stahl N, Wiegand SJ (2012) Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF Trap, ranibizumab and bevacizumab. Angiogenesis 15:171–185
Moradi A, Sepah YJ, Sadiq MA, Nasir H, Kherani S, Sophie R, Do DV, Nguyen QD (2013) Vascular endothelial growth factor trap-eye (Aflibercept) for the management of diabetic macular edema. World J Diabetes 4:303–309
Stewart MW, Rosenfeld PJ, Penha FM, Wang F, Yehoshua Z, Bueno-Lopez E, Lopez PF (2012) Pharmacokinetic rationale for dosing every 2 weeks versus 4 weeks with intravitreal ranibizumab, bevacizumab, and aflibercept (vascular endothelial growth factor Trap-eye). Retina 32:434–457
Bressler SB, Ayala AR, Bressler NM, Melia M, Qin H, Ferris FL 3rd, Flaxel CJ, Friedman SM, Glassman AR, Jampol LM, Rauser ME, Diabetic Retinopathy Clinical Research Network (2016) Persistent macular thickening after ranibizumab treatment for diabetic macular edema with vision impairment. JAMA Ophthalmol 134:278–285
Bressler NM, Beaulieu WT, Glassman AR, Blinder KJ, Bressler SB, Jampol LM, Melia M, Wells JA 3rd, Diabetic Retinopathy Clinical Research Network (2018) Persistent macular thickening following intravitreous aflibercept, bevacizumab, or ranibizumab for central-involved diabetic macular edema with vision impairment: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol 136:257–269
Gonzalez VH, Campbell J, Holekamp NM, Kiss S, Loewenstein A, Augustin AJ, Ma J, Ho AC, Patel V, Whitcup SM, Dugel PU (2016) Early and long-term responses to anti-vascular endothelial growth factor therapy in diabetic macular edema: analysis of protocol I data. Am J Ophthalmol 172:72–79
Koyanagi Y, Yoshida S, Kobayashi Y, Kubo Y, Nakama T, Ishikawa K, Nakao S, Hisatomi T, Ikeda Y, Oshima Y, Ishibashi T, Sonoda KH (2018) Visual outcomes based on early response to anti-vascular endothelial growth factor treatment for diabetic macular edema. Ophthalmologica 239:94–102
Mori K, Yoshida S, Kobayashi Y, Ishikawa K, Nakao S, Hisatomi T, Haruta M, Isihibashi T, Sonoda KH (2020) Decrease in the number of microaneurysms in diabetic macular edema after anti-vascular endothelial growth factor therapy: implications for indocyanine green angiography-guided detection of refractory microaneurysms. Graefes Arch Clin Exp Ophthalmol 258:735–741
Moisseiev E, Abbassi S, Thinda S, Yoon J, Yiu G, Morse LS (2018) Subthreshold micropulse laser reduces anti-VEGF injection burden in patients with diabetic macular edema. Eur J Ophthalmol 28:68–73
Liegl R, Langer J, Seidensticker F, Reznicek L, Haritoglou C, Ulbig MW, Neubauer AS, Kampik A, Kernt M (2014) Comparative evaluation of combined navigated laser photocoagulation and intravitreal ranibizumab in the treatment of diabetic macular edema. PLoS One 9:e113981
Herold TR, Langer J, Vounotrypidis E, Kernt M, Liegl R, Priglinger SG (2018) 3-year-data of combined navigated laser photocoagulation (Navilas) and intravitreal ranibizumab compared to ranibizumab monotherapy in DME patients. PLoS One 13:e0202483
Payne JF, Wykoff CC, Clark WL, Bruce BB, Boyer DS, Brown DM, TREX-DME Study Group (2017) Randomized trial of treat and extend ranibizumab with and without navigated laser for diabetic macular edema: TREX-DME 1 year outcomes. Ophthalmology 124:74–81
Payne JF, Wykoff CC, Clark WL, Bruce BB, Boyer DS, Brown DM, TREX-DME Study Group (2019) Randomized trial of treat and extend ranibizumab with and without navigated laser versus monthly dosing for diabetic macular edema: TREX-DME 2-year outcomes. Am J Ophthalmol 202:91–99
Inagaki K, Hamada M, Ohkoshi K (2019) Minimally invasive laser treatment combined with intravitreal injection of anti-vascular endothelial growth factor for diabetic macular oedema. Sci Rep 9:7585
Takamura Y, Tomomatsu T, Matsumura T, Arimura S, Gozawa M, Takihara Y, Inatani M (2014) The effect of photocoagulation in ischemic areas to prevent recurrence of diabetic macular edema after intravitreal bevacizumab injection. Invest Ophthalmol Vis Sci 55:4741–4746
Browrn DM, Ou WC, Wong TP, Kim RY, Croft DE, Wykoff CC, DAVE Study Group (2018) Targeted retinal photocoagulation for diabetic macular edema with peripheral retinal nonperfusion: three-year randomized DAVE trial. Ophthalmology 125:683–690
Kozak I, Oster SF, Cortes MA, Dowell D, Hartmann K, Kim JS, Freeman WR (2011) Clinical evaluation and treatment accuracy in diabetic macular edema using navigated laser photocoagulator NAVILAS. Ophthalmology 118:1119–1124
Kernt M, Cheuteu RE, Cserhati S, Seidensticker F, Liegl RG, Lang J, Haritoglou C, Kampik A, Ulbig MW, Neubauer AS (2012) Pain and accuracy of focal laser treatment for diabetic macular edema using a retinal navigated laser (Navilas). Clin Ophthalmol 6:289–296
Kernt M, Cheuteu R, Vounotrypidis E, Haritoglou C, Kampik A, Ulbig MW, Neubauer AS (2011) Focal and panretinal photocoagulation with a navigated laser (NAVILAS®). Acta Ophthalmol 89:e662–e664
Neubauer AS, Langer J, Liegl R, Haritoglou C, Wolf A, Kozak I, Seidensticker F, Ulbig M, Freeman WR, Kampik A, Kernt M (2013) Navigated macular laser decreases retreatment rate for diabetic macular edema: a comparison with conventional macular laser. Clin Ophthalmol 7:121–128
Jung JJ, Gallego-Pinazol R, Lleó-Pérez A, Huz JI, Barbazetto IA (2013) NAVILAS laser system focal laser treatment for diabetic macular edema - one year results of a case series. Open Ophthalmol J 7:48–53
Kato F, Nozaki M, Kato A, Hasegawa N, Morita H, Yoshida M, Ogura Y (2018) Evaluation of navigated laser photocoagulation (Navilas 577+) for the treatment of refractory diabetic macular edema. J Ophthalmol 2018:3978514
Nozaki M, Kato A, Yasukawa T, Suzuki K, Yoshida M, Ogura Y (2019) Indocyanine green angiography-guided focal navigated laser photocoagulation for diabetic macular edema. Jpn J Ophthalmol 63:243–254
Su D, Hubschman JP (2017) A review of subthreshold micropulse laser and recent advances in retinal laser technology. Ophthalmol Therapy 6:1–6
Gawęcki M (2019) Micropulse laser treatment of retinal diseases. J Clin Med 8:242
Moore SM, Chao DL (2018) Application of subthreshold laser therapy in retinal diseases: a review. Expert Rev Ophthalmol 13:311–320
Figueira J, Khan J, Nunes S, Sivaprasad S, Rosa A, de Abreu JF, Cunha-Vaz JG, Chong NV (2009) Prospective randomised controlled trial comparing sub-threshold micropulse diode laser photocoagulation and conventional green laser for clinically significant diabetic macular oedema. Br J Ophthalmol 93:1341–1344
Lavinsky D, Cardillo JA, Melo LA Jr, Dare A, Farah ME, Belfort R Jr (2011) Randomized clinical trial evaluating mETDRS versus normal or high-density micropulse photocoagulation for diabetic macular edema. Invest Ophthalmol Vis Sci 52:4314–4323
Luttrull JK, Musch DC, Mainster MA (2005) Subthreshold diode micro-pulse photocoagulation for the treatment of clinically significant diabetic macular oedema. Br J Ophthalmol 89:74–80
Luttrull JK, Spink CJ (2006) Serial optical coherence tomography of subthreshold diode laser micropulse photocoagulation for diabetic macular edema. Ophthalmic Surg Lasers Imaging 37:370–377
Othman IS, Eissa SA, Kotb MS, Sadek SH (2014) Subthreshold diode-laser micropulse photocoagulation as a primary and secondary line of treatment in management of diabetic macular edema. Clin Ophthalmol 8:653–659
Vujosevic S, Gatti V, Muraca A, Brambilla M, Villani E, Nucci P, Rossetti L, De Cillaʼ S (2020) Optical coherence tomography angiography changes after subthreshold micropulse yellow laser in diabetic macular edema. Retina 40:312–320
Vujosevic S, Frizziero L, Martini F, Bini S, Convento E, Cavarzeran F, Midena E (2018) Single retinal layer changes after subthreshold micropulse yellow laser in diabetic macular edema. Ophthalmic Surg Lasers Imaging Retina 49:e218–e225
The diabetic retinopathy study research group (1981) Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of diabetic retinopathy study (DRS) findings, DRS report number 8. Ophthalmology 88:583–600
Japanese Society of Ophthalmic Diabetology, Subcommittee on the Study of Diabetic Retinopathy Treatment, Sato Y, Kojimahara N, Kitano S, Kato S, Ando N, Yamaguchi N, Hori S (2012) Multicenter randomized clinical trial of retinal photocoagulation for preproliferative diabetic retinopathy. Jpn J Ophthalmol 56:52–59
Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, Pasquale LR, Thieme H, Iwamoto MA, Park JE, Nguyen HV, Aiello LM, Ferrara N, King GL (1994) Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 331:1480–1487
Writing Committee for the Diabetic Retinopathy Clinical Research Network, Gross JG, Glassman AR, Jampol LM, Inusah S, Aiello LP, Antoszyk AN, Baker CW, Berger BB, Bressler NM, Browning D, Elman MJ, Ferris FL 3rd, Friedman SM, Marcus DM, Melia M, Stockdale CR, Sun JK, Beck RW (2015) Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA 314:2137–2146
Gross JG, Glassman AR, Liu D, Sun JK, Antoszyk AN, Baker CW, Bressler NM, Elman MJ, Ferris FL 3rd, Gardner TW, Jampol LM, Martin DF, Melia M, Stockdale CR, Beck RW, Diabetic Retinopathy Clinical Research Network (2018) Five-year outcomes of panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol 136:1138–1148
Sivaprasad S, Prevost AT, Vasconcelos JC, Riddell A, Murphy C, Kelly J, Bainbridge J, Tudor-Edwards R, Hopkins D, Hykin P, CLARITY Study Group (2017) Clinical efficacy of intravitreal aflibercept versus panretinal photocoagulation for best corrected visual acuity in patients with proliferative diabetic retinopathy at 52 weeks (CLARITY): a multicentre, single-blinded, randomised, controlled, phase 2b, non-inferiority trial. Lancet 389:2193–2203
EVICR.net Study Group (2018) Ranibizumab plus panretinal photocoagulation versus panretinal photocoagulation alone for high-risk proliferative diabetic retinopathy (PROTEUS Study). Ophthalmology 125:691–700
Obeid A, Gao X, Ali FS, Talcott KE, Aderman CM, Hyman L, Ho AC, Hsu J (2018) Loss to follow-up in patients with proliferative diabetic retinopathy after panretinal photocoagulation or intravitreal anti-VEGF injections. Ophthalmology 125:1386–1392
Obeid A, Su D, Patel SN, Uhr JH, Borkar D, Gao X, Fineman MS, Regillo CD, Maguire JI, Garg SJ, Hsu J (2019) Outcomes of eyes lost to follow-up with proliferative diabetic retinopathy that received panretinal photocoagulation versus intravitreal anti-vascular endothelial growth factor. Ophthalmology 126:407–413
Hirano T, Toriyama Y, Iesato Y, Imai A, Hirabayashi K, Nagaoka T, Takamura Y, Sugimoto M, Murata T (2017) Effect of leaking perifoveal microaneurysms on resolution of diabetic macular edema treated by combination therapy using anti-vascular endothelial growth factor and short pulse focal/grid laser photocoagulation. Jpn J Ophthalmol 61:51–60
Mansouri A, Sampat KM, Malik KJ, Steiner JN, Glaser BM, Medscape (2014) Efficacy of subthreshold micropulse laser in the treatment of diabetic macular edema is influenced by pre-treatment central foveal thickness. Eye (Lond) 28:1418–1424
Jonas JB, Söfker A (2001) Intraocular injection of crystalline cortisone as adjunctive treatment of diabetic macular edema. Am J Ophthalmol 132:425–427
Tao Y, Jonas JB (2011) Intravitreal triamcinolone. Ophthalmologica 225:1–20
Mehta H, Hennings C, Gillies MC, Nguyen V, Campain A, Fraser-Bell S (2018) Anti-vascular endothelial growth factor combined with intravitreal steroids for diabetic macular oedema. Cochrane Database Syst Rev 4:CD011599
Bakri SJ, Kaiser PK (2005) Posterior subtenon triamcinolone acetonide for refractory diabetic macular edema. Am J Ophthalmol 139:290–294
Shimura M, Nakazawa T, Yasuda K, Shiono T, Nishida K (2007) Pretreatment of posterior subtenon injection of triamcinolone acetonide has beneficial effects for grid pattern photocoagulation against diffuse diabetic macular oedema. Br J Ophthalmol 91:449–454
Shimura M, Yasuda K, Nakazawa T, Shiono T, Sakamoto T, Nishida K (2009) Drug reflux during posterior subtenon infusion of triamcinolone acetonide in diffuse diabetic macular edema not only brings insufficient reduction but also causes elevation of intraocular pressure. Graefes Arch Clin Exp Ophthalmol 247:907–912
Shimura M, Yasuda K, Minezaki T, Noma H (2016) Reduction in the frequency of intravitreal bevacizumab administrations achieved by posterior subtenon injection of triamcinolone acetonide in patients with diffuse diabetic macular edema. Jpn J Ophthalmol 60:401–407
Shimura M, Yasuda K, Shiono T (2006) Posterior sub-Tenon’s capsule injection of triamcinolone acetonide prevents panretinal photocoagulation-induced visual dysfunction in patients with severe diabetic retinopathy and good vision. Ophthalmology 113:381–387
Maturi RK, Glassman AR, Liu D, Beck RW, Bhavsar AR, Bressler NM, Jampol LM, Melia M, Punjabi OS, Salehi-Had H, Sun JK, Diabetic Retinopathy Clinical Research Network (2018) Effect of adding dexamethasone to continued ranibizumab treatment in patients with persistent diabetic macular edema: a DRCR Network phase 2 randomized clinical trial. JAMA Ophthalmol 136:29–38
Sun JK, Jampol LM (2019) The diabetic retinopathy clinical research network (DRCR.net) and its contributions to the treatment of diabetic retinopathy. Ophthalmic Res 62:225–230
Lewis H, Abrams GW, Blumenkranz MS, Campo RV (1992) Vitrectomy for diabetic macular traction and edema associated with posterior hyaloidal traction. Ophthalmology 99:753–759
Tachi N, Ogino N (1996) Vitrectomy for diffuse macular edema in cases of diabetic retinopathy. Am J Ophthalmol 122:258–260
Terasaki H, Kojima T, Niwa H, Piao CH, Ueno S, Kondo M, Ito Y, Miyake Y (2003) Changes in focal macular electroretinograms and foveal thickness after vitrectomy for diabetic macular edema. Invest Ophthalmol Vis Sci 44:4465–4472
Kojima T, Terasaki H, Nomura H, Suzuki T, Mori M, Ito Y, Miyake Y (2003) Vitrectomy for diabetic macular edema: effect of glycemic control (HbA(1c)), renal function (creatinine) and other local factors. Ophthalmic Res 35:192–198
Yamamoto T, Hitani K, Sato Y, Yamashita H, Takeuchi S (2005) Vitrectomy for diabetic macular edema with and without internal limiting membrane removal. Ophthalmologica 219:206–213
Patel JI, Hykin PG, Schadt M, Luong V, Fitzke F, Gregor ZJ (2006) Pars plana vitrectomy with and without peeling of the inner limiting membrane for diabetic macular edema. Retina 26:5–13
Yanyali A, Horozoglu F, Celik E, Nohutcu AF (2007) Long-term outcomes of pars plana vitrectomy with internal limiting membrane removal in diabetic macular edema. Retina 27:557–566
Hatano N, Mizota A, Tanaka M (2007) Vitreous surgery for diabetic macular edema--its prognosis and correlation between preoperative systemic and ocular conditions and visual outcome. Ann Ophthalmol (Skokie) 39:222–227
Hartley KL, Smiddy WE, Flynn HW Jr, Murray TG (2008) Pars plana vitrectomy with internal limiting membrane peeling for diabetic macular edema. Retina 28:410–419
Kumagai K, Furukawa M, Ogino N, Larson E, Iwaki M, Tachi N (2009) Long-term follow-up of vitrectomy for diffuse nontractional diabetic macular edema. Retina 29:464–472
Diabetic Retinopathy Clinical Research Network Writing Committee1, Haller JA, Qin H, Apte RS, Beck RR, Bressler NM, Browning DJ, Danis RP, Glassman AR, Googe JM, Kollman C, Lauer AK, Peters MA, Stockman ME (2010) Vitrectomy outcomes in eyes with diabetic macular edema and vitreomacular traction. Ophthalmology 117:1087–1093
Simunovic MP, Hunyor AP, Ho IV (2014) Vitrectomy for diabetic macular edema: a systematic review and meta-analysis. Can J Ophthalmol 49:188–195
Adelman R, Parnes A, Michalewska Z, Parolini B, Boscher C, Ducournau D (2015) Strategy for the management of diabetic macular edema: the European vitreo-retinal society macular edema study. Biomed Res Int 2015:352487
Terasaki H, Ogura Y, Kitano S, Sakamoto T, Murata T, Hirakata A, Ishibashi T (2018) Management of diabetic macular edema in Japan: a review and expert opinion. Jpn J Ophthalmol 62:1–23
Chhablani JK, Kim JS, Cheng L, Kozak I, Freeman W (2012) External limiting membrane as a predictor of visual improvement in diabetic macular edema after pars plana vitrectomy. Graefes Arch Clin Exp Ophthalmol 250:1415–1420
Yamada Y, Suzuma K, Ryu M, Tsuiki E, Fujikawa A, Kitaoka T (2013) Systemic factors influence the prognosis of diabetic macular edema after pars plana vitrectomy with internal limiting membrane peeling. Curr Eye Res 38:1261–1265
Koyanagi Y, Yoshida S, Kobayashi Y, Kubo Y, Yamaguchi M, Nakama T, Nakao S, Ikeda Y, Ohshima Y, Ishibashi T, Sonoda KH (2016) Comparison of the effectiveness of intravitreal ranibizumab for diabetic macular edema in vitrectomized and nonvitrectomized eyes. Ophthalmologica 236:67–73
Bressler SB, Melia M, Glassman AR, Almukhtar T, Jampol LM, Shami M, Berger BB, Bressler NM, Diabetic Retinopathy Clinical Research Network (2015) Ranibizumab plus prompt or deferred laser for diabetic macular edema in eyes with vitrectomy prior to anti-vascular endothelial growth factor therapy. Retina 35:2516–2528
Yamakiri K, Sakamoto T, Noda Y, Nakahara M, Ogino N, Kubota T, Yokoyama M, Furukawa M, Sonoda Y, Yamada T, Doi N, Enaida H, Hata Y, Ishibashi T (2007) Reduced incidence of intraoperative complications in a multicenter controlled clinical trial of triamcinolone in vitrectomy. Ophthalmology 114:289–296
Reeser F, Fleischman J, Williams GA, Goldman A (1981) Efficacy of argon laser photocoagulation in the treatment of circinate diabetic retinopathy. Am J Ophthalmol 92:762–767
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shigeo Yoshida has received a speaker honorarium from Bayer Yakuhin, Ltd., Novartis Pharma K.K., and Santen Pharmaceutical Co., Ltd. and has received subsidy and donation from Bayer Yakuhin, Ltd., and Santen Pharmaceutical Co. Tomoaki Murakami has received a speaker honorarium from Bayer Yakuhin, Ltd., and Novartis Pharma K.K. and has received research funds from Novartis Pharma K.K. Miho Nozaki has received a speaker honorarium from Novartis Pharma K.K. Takao Hirano has received a speaker honorarium from Novartis Pharma K.K. Masahiko Sugimoto has received a research funds from Alcon Japan Ltd., and Bayer Yakuhin, Ltd. and has received speaker honorarium and consulting fees from Alcon Japan Ltd., Kowa Company, Ltd., Senju Pharmaceutical Co., Ltd., Daiichi Yakuhin Sangyo Co., Ltd., Bayer Yakuhin, Ltd., and Wakamoto Pharmaceutical Co., Ltd.
Interscience Co., Ltd. assisted in the writing and editing of this paper with funding from Bayer Yakuhin, Ltd. All authors wrote this review considering the view of expert doctors with the assistance of Interscience Co., Ltd.; however, Bayer Yakuhin, Ltd. has not been involved in the preparation of this article in any way.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yoshida, S., Murakami, T., Nozaki, M. et al. Review of clinical studies and recommendation for a therapeutic flow chart for diabetic macular edema. Graefes Arch Clin Exp Ophthalmol 259, 815–836 (2021). https://doi.org/10.1007/s00417-020-04936-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04936-w