Abstract
Purpose
To evaluate the effectiveness of posterior subtenon injections of triamcinolone acetonide (STTA) during treatment with intravitreal injections of bevacizumab (IVB) in eyes with diffuse diabetic macular edema (DDME).
Methods
Forty eyes of 20 patients with bilateral DDME with foveal thickness (FT) greater than 400 μm were studied. Initially, both eyes of each patient received 1.25 mg/0.05 ml of IVB. One eye then received 20 mg/0.5 ml of STTA at the onset and at 16, 32, and 48 weeks. For the control, the other eye was not treated with STTA. Patients were treated with additional IVB when DDME recurred during the study to maintain the FT at <350 μm. The FT, logMAR visual acuity (VA), and intraocular pressure (IOP) were monitored monthly for 56 weeks. The total number of IVB injections during the 1-year follow-up was also calculated.
Results
STTA-treated eyes had significantly more regression of FT and improvement of VA at several time points during the study than did the controls. The mean (SD) required number of IVB injections in the STTA-treated eyes during the study was 5.00 ± 1.75, which was significantly less than the 7.95 ± 1.57 in the control eyes.
Conclusions
Adjunctive STTA therapy to IVB for the treatment of DDME not only improved the morphological and functional regressions but also reduced the frequency of IVB treatments.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetic retinopathy is the leading cause of blindness and visual disability in the working age group in economically developed societies [1]. Diffuse diabetic macular edema (DDME) is a sight-threatening complication, and is the most prevalent cause of visual loss in diabetic patients, with its prevalence increasing to 6.81 % among those patients [2].
Recently, on the basis of scientific evidence showing that vascular endothelial growth factor (VEGF) has been implicated in the pathogenesis of DDME [3], anti-VEGF treatment for DDME has been established [4, 5] and found to be effective for reducing macular edema and improving visual function. It also has some advantages in terms of being a safe [not increasing intraocular pressure (IOP)] and rapid (usually resolving macular edema within 1 month) treatment [6, 7]. Although anti-VEGF treatment brings better anatomical and functional outcomes in DDME, recurrence of DDME after the single injection is usually observed, and thus, additional injection is often required to maintain its effectiveness. The findings of multicenter studies (the RISE and RIDE trials) have shown that monthly injection of intravitreal ranibizumab (IVR) is required [8], and even “as needed” injection of intravitreal bevacizumab (IVB) is reported to be 5.8 times per year [9]. Multiple intravitreal injections sometimes incur the adverse effects of ocular pain, ischemic retinopathy, and endophthalmitis [10] and are also associated with the financial problem of the high cost of drugs, such as ranibizumab [11]. Thus, the number of injections of intravitreal anti-VEGF antibody should be limited.
Posterior subtenon injection of triamcinolone acetonide (STTA) is also effective for reducing DDME [12–14]. Apart from intravitreal injection of triamcinolone acetonide (IVTA), the adverse effects of increased IOP or progression of cataracts were hardly observed if applied appropriately [14].
In this study, the efficacy of STTA for multiple injection of IVB in DDME was investigated to estimate the number of IVB injections for maintaining the morphological resolution of DDME and to evaluate the clinical course of the visual function and IOP.
Patients and methods
This prospective study was conducted according to the institutional guidelines of the clinical research ethics committees of both the NTT East Japan Tohoku Hospital (# 2010003) and the Tokyo Medical University Hachioji Medical Center (H-3) and was approved by the institutional review board of each institution before it was performed. The procedures conformed to the tenets of the World Medical Association’s Declaration of Helsinki. Informed consent was obtained from each of the patients after he or she had been provided sufficient information on the procedures to be used.
Patient eligibility
Type II diabetic patients with bilateral center-involved DDME were recruited. DDME was defined as foveal thickness (FT) >400 μm and best-corrected logMAR visual acuity (VA) ≤0.3 in both eyes. Eyes with severe proliferative retinopathy were excluded. Patients with a history of focal or panretinal photocoagulation and/or cataract surgery in either eye within at least 6 months before entry into the study, and patients who had previous therapy for DDME, including grid laser treatment, intravitreal injection of any drugs, and/or vitreous surgery, were excluded. Patients who had systemic disorders other than hypertension and hypercholesterolemia were also excluded. During the clinical course, patients whose retinopathy progressed so as to require photocoagulation or vitreous surgery were excluded from the study.
Clinical parameters
All patients received a comprehensive ocular examination before and after the treatment. Visual acuity was measured by means of a logMAR chart (5 m) (NEITZ LVC-10; Neitz Instruments, Tokyo, Japan), and FT, by means of Cirrus OCT (Carl Zeiss Meditec, Dublin, CA, USA) during the follow-up examinations. Intraocular pressure was measured by applanation tonometry during the clinical course. The Cirrus OCT images were generated using the currently available Cirrus software. The FT was calculated by an experienced examiner (K. Y. or T. M.) by manual averaging of the FT of the horizontal and vertical images using the caliper tool built into the OCT software.
Improvement in FT was assessed by the best reduction ratio, which was calculated as \({{\left( {{\text{FT}}_{{{\text{at}}\,{\text{baseline}}}} - {\text{FT}}_{{{\text{lowest}}\,{\text{during}}\,{\text{the}}\, {\text{clinical\,course}}}} } \right)} \mathord{\left/ {\vphantom {{\left( {{\text{FT}}_{{{\text{at}}\,{\text{baseline}}}} - {\text{FT}}_{{{\text{lowest}}{\kern 1pt} {\text{during}}\, {\text{the}}\,{\text{clinical\,course}}}} } \right)} {{\text{FT}}_{{{\text{at \,baseline}}}} }}} \right. \kern-\nulldelimiterspace} {{\text{FT}}_{{{\text{at \,baseline}}}} }} \times 100 \, (\%) \). Improvement of VA was assessed by the best functional improvement, which was calculated as \( {\text{VA}}_{\text{at \,baseline}} - {\text{VA}}_{\text{best\, during\, the \,clinical \,course}} .\) Intraocular pressure elevation was assessed by the max ΔIOP, which was calculated as \( {\text{IOP}}_{\text{maximum\, during \,the \,clinical\, course}} - {\text{IOP}}_{\text{at\, baseline}} .\)
Drug injection
At the time of the drug injection, topical anesthesia was induced by applying 0.4 % oxybuprocaine eye drops (Benoxil; Santen Pharmaceutical, Osaka, Japan) at least 3 times. A topical antimicrobial drug of gatifloxacin hydrate 0.3 % ophthalmic solution (Gatiflo; Senju Pharmaceutical, Osaka, Japan) was administered 4 times/day in both eyes for at least 1 week after each drug injection. Following disinfection and draping, a 0.05-ml volume containing 1.25 mg of bevacizumab (Avastin; Genetech, South San Francisco, CA, USA) was injected into the vitreous cavity using a sharp 30-G needle at a distance of 3.5 mm from the limbus. To avoid an increase in IOP, aqueous humor was removed as appropriate. As regards the STTA, 20 mg of triamcinolone acetonide (Kenacort; Bristol-Myers Squibb, Tokyo, Japan) at a volume of 0.5 ml was gently injected into the superotemporal quadrant using a 21-gauge triport subtenon cannula (Eagle Lab, Rancho Cucamonga, CA, USA) through a conjunctival wound. The drug applications were performed in all eyes by the same retinal specialist (M. S.), and absence of a drug reflex at each injection was confirmed.
Study design and definition of effective treatment and recurrence
All eligible eyes received initial IVB. The clinical courses of FT, VA, and IOP were monitored every 4 weeks during a follow-up period of up to 56 months. IVB injection was performed monthly until an FT of less than 300 μm was obtained, and after that, additional IVB was given appropriately to maintain the FT at less than 350 μm during the clinical course. Patients who had not obtained an FT of less than 350 μm despite undergoing 6 initial consecutive IVB injections in either eye had to be excluded from the study and received other treatments. If required in both eyes, another IVB was performed within 48 h.
For each patient, 1 eye received STTA every 16 weeks (0, 16, 32, and 48 weeks), and the other eye was used as the control. To ensure equal DDME conditions, STTA-injected eyes were selected in consecutive patients by turn [15]. In brief, after the initial ocular and general examinations, the eye with thicker FT was defined as the primary eye, and the other eye as the secondary eye. For example, in the first patient, the primary eye was determined as the STTA-injected eye and the secondary eye as the control eye, and subsequently in the next patient, the primary eye was determined as the control, and the secondary eye as the STTA-injected eye. If needed, STTA and IVB injections were received on the same day, as appropriate.
The initial and total numbers of IVB injections were recorded.
Statistical analyses
The data were presented as means ± standard deviations. Statistical differences between the pre- and post-drug application clinical data were assessed using the Wilcoxon signed-rank test, and differences between the STTA-treated and control eyes were assessed using the Mann–Whitney test (SPSS, Chicago, IL, USA). Probability values of less than 0.05 were considered significant.
Results
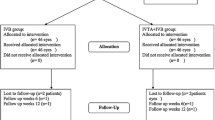
Thirty patients with bilateral DDME were recruited to this study, and during the clinical course, 7 patients (23.3 %) were excluded owing to a lack of responsiveness to the therapy after 6 continuous IVB injections in both eyes. In addition, 2 patients had vitreous surgery owing to vitreous hemorrhage in 1 eye, and 1 patient dropped out for personal reasons. Therefore, 40 eyes of 20 patients (12 men, 8 women) were studied. The age of the patients ranged from 58 to 78 years, with a mean (SD) of 68.6 ± 5.1 years. All the patients had type II diabetes, and the duration of diabetes ranged from 1 to 12 years, with a mean of 5.8 ± 2.9 years. Fourteen of the 20 patients (70 %) had a history of hypertension and were taking oral systemic antihypertensive drugs. None of the patients had a history of any other ocular disease other than refractive errors or cataracts. Twelve patients had cataract surgery with intraocular lens implantation in both eyes, and the other 8 patients had a phakic lens in both eyes, with a cataract grade of less than Emery level I, and symmetrical in both eyes. During the clinical course, none of these 8 patients showed any cataract progression. The mean (SD) HbA1c and total cholesterol (tChL) were 7.18 ± 0.49 % and 192.6 ± 17.2 mg/dl respectively, before the start of the study. During the clinical course, the HbA1c and tChL did not exceed 8.0 % or 250 mg/dl in any of the patients, and blood pressure was well controlled by the patients’ internists.
Numbers of required IVB injections
In each patient, after the comprehensive ocular examination, 1 eye received initial STTA and IVB, and the other eye received IVB. In all eyes, FT of less than 300 μm was obtained after several IVB injections in each eye. The required number of IVB injections for obtaining an FT of less than 300 μm was 3.15 ± 1.81 (range 1–5) in the STTA-treated group, which was significantly less than the 4.35 ± 1.60 (range 2–6) injections in the control group (P < 0.001) (Fig. 1a). During the clinical course, subsequent IVB injection was performed when the FT increased to more than 350 μm (see “Study design and definition of effective treatment and recurrence”), and the total number of IVB injections needed to maintain an FT of less than 350 μm was 5.00 ± 1.75 (range 1–8) in the STTA-treated group, which was significantly less than the 7.95 ± 1.57 (range 3–10) injections in the control group (P < 0.001) (Fig. 1b).
Comparison of the number of intravitreous bevacizumab (IVB) injections with and without subtenon injection of triamcinolone acetonide (STTA) every 4 months. a Average number of IVB injections needed to obtain an initial foveal thickness (FT) of less than 300 μm in eyes with diabetic macular edema. b Average number of IVB injections needed to maintain an FT of less than 350 μm in eyes with diabetic macular edema. Number of eyes in which IVB was injected at each time point. The arrows indicate treatment with STTA; the black bars indicate eyes treated with STTA; the white bars indicate the control eyes. Each vertical bar indicates the standard deviation. Asterisks indicate significant differences between them (P < 0.05)
Alteration of FT
Before the administration of the drugs, the FT was 599.2 ± 91.7 μm in the STTA-treated eyes, and 594.6 ± 97.2 μm in the control eyes, with no significant difference between them (P = 0.429). After the initial IVB, the FT in both groups decreased significantly and remained at a level of less than 350 μm throughout the clinical course. At each time point, the difference was significant between the STTA-treated and the control eyes at several time points other than at 28 (P = 0.410), 32 (P = 0.186), 44 (P = 0.466), and 48 (P = 0.245) weeks (Fig. 2a). The best reduction ratio in the STTA-treated eyes was 54.1 ± 6.7 %, which did not differ significantly from that in the control eyes (52.3 ± 7.6 %; P = 0.224) (Fig. 2b).
a Clinical course of foveal thickness (FT) with multiple injections of intravitreous bevacizumab (IVB) in patients with DDME. The open circles indicate eyes with an additional subtenon injection of triamcinolone acetonide (STTA), and the filled circles, the contralateral eyes without STTA. Each vertical bar indicates the standard deviation. The arrows indicate the application time points of STTA. Asterisks indicate significant differences between the STTA-treated eyes and the control eyes at each time point (P < 0.05). b Reduction ratio (refer to the text) in eyes with (black bar) and without (white bar) STTA. No significant difference was found between the 2 groups
Alteration of logMAR VA
Before the administration of the drugs, the logMAR VA was 0.56 ± 0.19 in the STTA-treated eyes and 0.59 ± 0.20 in the control eyes, which was not significantly different (P = 0.178). After the initial IVB injection, the logMAR VA in both groups improved significantly up to 12 weeks and then became stable after 20 weeks throughout the clinical course. Although the STTA-treated and control eyes differ significantly at 4 (P = 0.027), 8 (P = 0.038), 24 (P = 0.041), 36 (P = 0.011), 40 (P = 0.023), 52(P = 0.023), and 56 (P = 0.050) weeks (Fig. 3a), the best functional improvement in the STTA-treated eyes during the clinical course was 0.25 ± 0.11, which was not significantly different from that in the control eyes (0.23 ± 0.06; P = 0.253) (Fig. 3b).
a Clinical course of best-corrected visual acuity with logMAR chart (VA) with multiple intravitreous bevacizumab (IVB) treatments in patients with DDME. The open circles indicate eyes with additional STTA, and the filled circles, contralateral eyes without STTA. Each vertical bar indicates the standard deviation. The arrows indicate the application time points of STTA. The asterisks indicate significant differences between the STTA-treated eyes and the control eyes at each time point (P < 0.05). b Functional improvement (refer to the text) in eyes with (black bar) and without (white bar) STTA. No significant difference was found between the 2 groups
Alteration of IOP
Before the administration of the drugs, the IOP was 15.6 ± 2.3 (range 11–20) mmHg in the STTA-treated eyes and 15.7 ± 2.8 (range 11–20) mmHg in the control eyes, and there was no significant difference between them (P = 0.927). After the initial IVB injection, the IOP in the STTA-treated eyes increased steeply and, after 24 weeks, significantly increased, while the IOP in the control eyes did not change significantly during the clinical course. The STTA-treated and control eyes showed a significant difference at 32 (P = 0.046), 44 (P = 0.021), and 52 (P = 0.007) weeks (Fig. 4a). The max ΔIOP in the STTA-treated eyes was 2.70 ± 0.92 mmHg, which was significantly higher than that in the control eyes (2.05 ± 1.19 mmHg; P = 0.008) (Fig. 4b). However, the IOP in all eyes did not exceed 21 mmHg without antiglaucoma drugs throughout the clinical course.
a Clinical course of intraocular pressure (IOP) with multiple IVB treatments in patients with DDME. The open circles indicate eyes with additional STTA, and the filled circles, contralateral eyes without STTA. Each vertical bar indicates the standard deviation. The arrows indicate the application time points of STTA. Asterisks indicate a significant difference between the STTA-treated eyes and the control eyes at each time point (P < 0.05). b Maximum ΔIOP (refer to the text) in eyes with (black bar) and without (white bar) STTA. A significant difference was found between the 2 groups (P = 0.008)
Discussion
A growing body of scientific evidence has implicated VEGF in the pathophysiologic features of DDME, and recent studies have shown the effectiveness of IVB in reducing DDME. Therefore, IVB has become the representative treatment for DME [16]; however, frequent injections of IVB are required to achieve the visual outcome. Yet, the findings of this study showed that 7 of 30 patients did not respond to IVB therapy even after 6 continuous injections.
In this prospective case–control study, among the IVB-responsive patients, adjunctive therapy of STTA to IVB not only yielded better functional and morphological results than did IVB monotherapy but also required fewer numbers of IVB injections to maintain these results for at least a 1-year follow-up period. Moreover, fewer IVB injections were required to achieve an FT of less than 350 μm.
Before our study, several studies were published on combined focal administration of triamcinolone acetonide and bevacizumab. Most of those studies were performed with IVTA and bevacizumab, and the authors concluded that IVTA/IVB induced earlier functional and morphological regression than did IVB, although the prognoses did not differ significantly between IVTA/IVB and IVB [17, 18]. Although the efficacy of combined IVTA/IVB for DME was reported [19], the beneficial inferiority of IVTA/IVB to IVB owing to treatment complications was also pointed out [20, 21].
Unlike in previous studies, in our study, combined triamcinolone acetonide and bevacizumab for DDME was superior in terms of morphological and functional efficacy and required less frequent IVBs for maintaining the effects.
As for the medical treatment for DDME, anti-VEGF drugs and anti-inflammatory corticosteroids were usually used. Usually, anti-VEGF drugs have to be administered by vitreous injection, whereas corticosteroids can be administered via 2 routes: vitreous injection and subtenon injection. In past studies of combination therapy of bevacizumab and triamcinolone acetonide, both drugs were administered by vitreous injection, which requires a bigger liquid volume (twice as much as that for single-drug therapy) and induces IOP elevation. In contrast, in our study, triamcinolone acetonide was administered through the subtenon space, which prevents cataract formation and IOP elevation if injected appropriately [14, 22]. Thus, STTA/IVB combination therapy, which is different from IVTA/IVB therapy, might show better, safer, and longer-lasting results than IVB monotherapy for suppression of DME.
In this study, progression of VA in both treated eyes showed logMAR values of 0.23 and 0.25, which was better than that shown in a previous report of IVB monotherapy (logMAR value of 0.14) [9]. The possible explanation for the better visual prognosis in our study is that the eligible patients were limited to those who were morphologically responsive to IVB. Thus, in the clinical field, it may be important to select drug-responsive patients before starting the treatment.
Unlike prior studies, and despite its small sample size, we used the paired eyes of each patient to avoid possible bias against systemic factors of glycemic control, blood pressure, and nephropathy. The difference in the morphological and functional efficacy of STTA/IVB and IVB seems small, but showed statistical significance according to our rigorous case–control study.
The result showing that STTA augmented IVB for reduction of DDME is not surprising. DDME is related not only to VEGF but also to IL-6 and ICAM-1 [23, 24]; therefore, the pathogenesis of DDME is related not only to VEGF dependency but also to other mechanisms suppressed by corticosteroids [25]. Corticosteroids affect a number of different cytokines including VEGF [26]; thus, it may be necessary to reduce more than 1 cytokine to achieve an effective reduction in DDME. In fact, recent studies revealed that IVTA is more effective than IVB for improving visual function in DDME [15, 27]. However, IVTA has a major and serious side effect of prominent elevation of IOP. As in our study, STTA elevated IOP but within the normal range. From this study’s findings, our conclusion is that adjunctive STTA augmented IVB for regression of DDME without marked IOP elevation.
Another important finding of this study is that adjunctive STTA reduced the frequency of IVB for obtaining and maintaining regression of DDME. According to a recent interesting study, the cost-effectiveness of managing DDME with an anti-VEGF drug was estimated to be between US $10,000 and $100,000 per year [28]; therefore, reduction in the required numbers of anti-VEGF drugs is important not only for patients but also for medical expenses. Thus, adjunctive STTA also has an advantage in terms of cost savings for the social health care system.
Although this nonrandomized case–control pilot study was not large enough to permit us to reach definitive conclusions, its results present a possibility of STTA with the augmentative effect of IVB in reducing DDME with less frequent injections. However, we also recognize that a further prospective randomized study with a larger number of cases and a longer observation period is necessary to confirm our hypothesis.
References
Klein BE. Overview of epidemiologic studies of diabetic retinopathy. Ophthalmic Epidemiol. 2007;14:179–83.
Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64.
Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994;331:1480–7.
Bandello F, Cunha-Vaz J, Chong NV, Lang GE, Massin P, Mitchell P, et al. New approaches for the treatment of diabetic macular oedema: recommendations by an expert panel. Eye (Lond). 2012;26:485–93.
Lang GE. Diabetic macular edema. Ophthalmologica. 2012;227(Suppl 1):21–9.
Arevalo JF, Fromow-Guerra J, Quiroz-Mercado H, Sanchez JG, Wu L, Maia M, et al. Primary intravitreal bevacizumab (Avastin) for diabetic macular edema. Ophthalmology. 2007;114:743–50.
Haritoglou C, Kook D, Neubauer A, Wolf A, Priglinger S, Strauss R, et al. Intravitreal bevacizumab (Avastin) therapy for persistent diffuse diabetic macular edema. Retina. 2006;26:999–1005.
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119:789–801.
Arevalo JF, Sanchez JG, Lasave AF, Wu L, Maia M, Bonafonte S, et al. Intravitreal bevacizumab (Avastin) for diabetic retinopathy: the 2010 GLADAOF lecture. J Ophthalmol. 2011;2011:584238.
Gunther JB, Altaweel MM. Bevacizumab (Avastin) for the treatment of ocular disease. Surv Ophthalmol. 2009;54:372–400.
Smiddy WE. Clinical applications of cost analysis of diabetic macular edema treatments. Ophthalmology. 2012;119:2558–62.
Bakri SJ, Kaiser PK. Posterior subtenon triamcinolone acetonide for refractory diabetic macular edema. Am J Ophthalmol. 2005;139:290–4.
Shimura M, Nakazawa T, Yasuda K, Shiono T, Nishida K. Pretreatment of posterior subtenon injection of triamcinolone acetonide has beneficial effects for grid pattern photocoagulation against diffuse diabetic macular edema. Br J Ophthalmol. 2007;91:449–54.
Shimura M, Yasuda K, Nakazawa T, Shiono T, Sakamoto T, Nishida K. Drug reflux during posterior subtenon infusion of triamcinolone acetonide in diffuse diabetic macular edema not only brings insufficient reduction but also causes elevation of intraocular pressure. Graefes Arch Clin Exp Ophthalmol. 2009;247:907–12.
Shimura M, Nakazawa T, Yasuda K, Shiono T, Iida T, Sakamoto T, et al. Comparative therapy evaluation of intravitreal bevacizumab and triamcinolone acetonide on persistent diffuse diabetic macular edema. Am J Ophthalmol. 2008;145:854–61.
Thomas BJ, Shienbaum G, Boyer DS, Flynn HW Jr. Evolving strategies in the management of diabetic macular edema: clinical trials and current management. Can J Ophthalmol. 2013;48:22–30.
Ahmadieh H, Ramezani A, Shoeibi N, Bijanzadeh B, Tabatabaei A, Azarmina M, et al. Intravitreal bevacizumab with or without triamcinolone for refractory diabetic macular edema; a placebo-controlled, randomized clinical trial. Graefes Arch Clin Exp Ophthalmol. 2008;246:483–9.
Faghihi H, Roohipoor R, Mohammadi SF, Hojat-Jalali K, Mirshahi A, Lashay A, et al. Intravitreal bevacizumab versus combined bevacizumab-triamcinolone versus macular laser photocoagulation in diabetic macular edema. Eur J Ophthalmol. 2008;18:941–8.
Tsilimbaris MK, Pandeleondidis V, Panagiototglou T, Arvanitaki V, Fragiskou S, Eleftheriadou M, et al. Intravitreal combination of triamcinolone acetonide and bevacizumab (Kenacort–Avastin) in diffuse diabetic macular edema. Semin Ophthalmol. 2009;24:225–30.
Soheilian M, Garfami KH, Ramezani A, Yaseri M, Peyman GA. Two-year results of a randomized trial of intravitreal bevacizumab alone or combined with triamcinolone versus laser in diabetic macular edema. Retina. 2012;32:314–21.
Soheilian M, Ramezani A, Obudi A, Bijanzadeh B, Salehipour M, Yaseri M, et al. Randomized trial of intravitreal bevacizumab alone or combined with triamicinolone versus macular photocoagulation in diabetic macular edema. Ophthalmology. 2009;116:1142–50.
Inatani M, Iwao K, Kawaji T, Hirano Y, Ogura Y, Hirooka K, et al. Intraocular pressure elevation after injection of triamcinolone acetonide: a multicenter retrospective case-control study. Am J Ophthalmol. 2008;145:676–81.
Funatsu H, Yamashita H, Ikeda T, Mimura T, Eguchi S, Hori S. Vitreous levels of interleukin-6 and vascular endothelial growth factor are related to diabetic macular edema. Ophthalmology. 2003;110:1690–6.
Funatsu H, Yamashita H, Sakata K, Noma H, Mimura T, Suzuki M, et al. Vitreous levels of vascular endothelial growth factor and intracellular adhesion molecule 1 are related to diabetic macular edema. Ophthalmology. 2005;112:806–16.
Sohn HJ, Han DH, Kim IT, Oh IK, Kim KH, Lee DY, et al. Changes in aqueous concentrations of various cytokines after intravitreal triamcinolone versus bevacizumab for diabetic macular edema. Am J Ophthalmol. 2011;152:686–94.
Barnes PJ. Corticosteroid effects on cell signalling. Eur Respir J. 2006;27:413–26.
Zhang Y, Ma J, Meng N, Li H, Qu Y. Comparison of intravitreal triamcinolone acetonide with intravitreal bevacizumab for treatment of diabetic macular edema: a meta-analysis. Curr Eye Res. 2013;38:578–87.
Stein JD, Newman-Casey PA, Kim DD, Nwanyanwu KH, Johnson MW, Hutton DW. Cost-effectiveness of various interventions for newly diagnosed diabetic macular edema. Ophthalmology. 2013;120:1835–42.
Conflicts of interest
M. Shimura, Grant (NTT East Japan Tohoku Hospital); K. Yasuda, None; T. Minezaki, None; H. Noma, None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Shimura, M., Yasuda, K., Minezaki, T. et al. Reduction in the frequency of intravitreal bevacizumab administrations achieved by posterior subtenon injection of triamcinolone acetonide in patients with diffuse diabetic macular edema. Jpn J Ophthalmol 60, 401–407 (2016). https://doi.org/10.1007/s10384-016-0458-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-016-0458-9