Abstract
Purpose
Fungus ball (FB) is the most common type of fungal rhinosinusitis and the prevalence of FB has increased over the past 10 years. The aim of this study was to compare the clinical characteristics of Korean adult patients with FB and chronic rhinosinusitis (CRS) without FB.
Methods
We retrospectively analyzed data on 1362 patients (147 FB and 1215 CRS) who underwent endoscopic sinus surgery at nine Korean medical centers in 2005, 2010, and 2016. We evaluated the prevalence of FB and compared the clinical characteristics of FB and CRS. Medical records, computed tomography (CT) findings, atopic status, concomitant diseases, tissue, and blood eosinophil count were assessed.
Results
The prevalence of FB was significantly higher in 2016 (15.9%) than in the other years (7.8% in 2005 and 7.5% in 2010). The FB patients were more likely to be female, older, have unilateral disease and less likely to have allergy compared to the CRS patients. The most common main complaint related to CRS and FB was nasal obstruction. CT determined that unilateral disease and maxillary sinus dominancy were common in patients with FB. The incidence of concomitant diseases was much higher in FB, with lower tissue and blood eosinophilia.
Conclusion
FB is commonly encountered in older women with the increased prevalence. FB had a different clinical presentation, radiological findings, and prognosis than CRS. Further studies are needed to understand the pathophysiologic mechanisms underlying the development of FB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fungus ball (FB) is the most frequent non-invasive fungal rhinosinusitis and is characterized by accumulation of fungal hyphae within the sinus cavity without microscopic evidence of tissue invasion. FB commonly affects immunocompetent and non-atopic individuals. FB is frequently diagnosed in patients with a prolonged history of recurrent sinusitis and about 3.7% of the chronic rhinosinusitis (CRS) patients in late-twentieth century [1]. The pathogenesis and risk factors for FB remain largely unknown. The frequency of FB diagnoses has tended to increase, due to the increased usage of antibiotics, global warming, Asian sand storms, and dental procedures on the maxillary teeth [2,3,4]. In Korea, the prevalence of FB continuously increased over the past 10 years [3, 5]. The incidence of FB was 13.4% in 2015 compared with 4.1% in 2005.
DeShazo proposed diagnostic criteria for FB based on clinical, radiological, morphological, and histological findings [6]. The clinical presentation of FB is non-specific and asymptomatic patients are common [7, 8]. Improvements in diagnostic imaging, such as computed tomography (CT) or magnetic resonance imaging and increased clinical suspicion, have led to more incidental or sub-clinical findings of FB [8]. CT scans reveal characteristic heterogeneous opacities associated with discrete calcified densities within the involved sinus. The maxillary sinus is the most commonly involved sinus, followed by the sphenoid sinus [9]. Many researchers have reported on the clinical characteristics of FB and focused on the clinical and radiologic characteristics of FB [7, 10,11,12]. Most of them are performed in a single medical center. They have not compared the clinicopathologic characteristics of FB with CRS. In this study, we performed a retrospective analysis of FB patients from nine centers in South Korea at three time points during the last 12 years, and in four different seasons. We analyzed the prevalence of FB in Korea and compared the clinical characteristics of FB with CRS.
Materials and methods
Study population
This retrospective study was conducted on a total of 1362 patients at nine different medical centers, who underwent endoscopic sinus surgery for CRS or FB. The medical records were assessed in 2005, 2010, and 2016, and during January, April, July, and October. We selected three different years to check the prevalence change of FB in Korea. Since Korea has clearly defined four seasons with different temperature and humidity, we collected data from patients during four different representative months. The diagnoses of CRS and FB were based on paranasal sinus CT findings, endoscopic findings, surgical findings, and pathology reports. Patients were excluded if they were younger than 18 years old, diagnosed with antrochoanal polyp, inverted papilloma, postoperative cyst, mucocele, and other benign or malignant tumors. And patients who underwent surgical procedures other than endoscopic sinus surgery were also excluded. The study design was approved by the Institutional Review Board of each medical center.
Chief complaints, concomitant diseases, and allergic status were evaluated in the medical records. Preoperative CT scans were reviewed to determine the extent of the disease using the Lund–Mackay scoring system. Sinus dominancy was determined by the ratio of the ethmoid and maxillary sinus scores (E/M ratio), based on the Lund–MacKay scoring. If the E/M ratio was greater than 2, opacification of the ethmoid sinus was considered to be more severe than that of the maxillary sinus. If every sinus was involved, it was determined to be “similar”. The atopic status of each patient was determined with a skin prick test or multiple allergen simultaneous test-chemiluminescent assay against a standard panel of aeroallergens. Olfactory function was determined using the Korean version of the Sniffin’ Stick test to determine the total threshold–discrimination–identification score [13]. The number of eosinophils in the hematoxylin-and-eosin-stained tissue sections was determined by two independent physicians. The average numbers of eosinophils in the submucosal area of five high-power visual fields were counted. Blood eosinophilia was also assessed. The incidence of revision surgery cases and smoking status were also evaluated.
Statistical analysis
The results are presented as mean ± standard deviation. The normality test was performed by Kolmogorov–Smirnov test. The prevalence change at three different time points and in four different seasons was determined by one-way analysis of variance followed by the Bonferroni test. The clinicopathological differences between CRS and FB were determined using two-sample t tests and the Chi-squared test. The analyses were conducted with Statistical Package for the Social Sciences software version 21 (SPSS Inc., Chicago IL, USA). Results with p < 0.05 were regarded as statistically significant.
Results
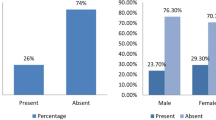
A total of 1362 patients were enrolled in this study. In 2005, 357 CRS patients (209 men, 148 women, with a mean age of 38.8 ± 17.3 years) and 30 FB patients (8 men, 22 women, mean age of 56.5 ± 12.9 years), in 2010, 419 CRS patients (276 men, 143 women, mea age of 45.0 ± 15.5 years) and 34 FB patients (14 men, 20 women, mean age of 63.0 ± 16.0 years), and in 2016, 439 CRS patients (274 men, 165 women, mean age of 49.0 ± 15.5 years) and 83 FB patients (20 men, 63 women, mean age of 61.2 ± 10.6 years) were enrolled. The incidence of FB was significantly higher in 2016 than in the other years (7.8% in 2005, 7.5% in 2010, and 15.9% in 2016; p < 0.01) and during October (8.9% in January, 8.2% in April, 11.3% in July, and 16.2% in October; p = 0.03). The mean age of FB patients (61.0 ± 11.1 years) was significantly higher than that of CRS patients (46.1 ± 15.6 years), and FB was more common in women (p < 0.01; Table 1).
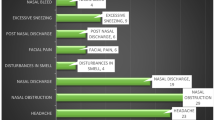
The chief complaint differed between CRS and FB. The most common chief complaint from CRS was nasal obstruction (61.1%), followed by rhinorrhea (10.8%), posterior nasal drip (5.5%), and loss of smell (5.4%). In FB, nasal obstruction (28.6%) was the most common complaint followed by facial pressure (19.1%), posterior nasal drip (18.4%), and rhinorrhea (10.9%). The mean symptom duration to visiting the rhinology department was significantly longer in the CRS group (45.9 ± 75.1 months) than in the FB (17.6 ± 42.5 months) (p < 0.01). CT determined that unilateral disease and maxillary sinus dominancy were more common in the FB group (86.4% and 78.9%) than in the CRS group (30.4% and 44.9% respectively; p < 0.01). However, the mean Lund–Mackay score was not significantly different between the two groups (p = 0.18). The prevalence of positive allergy test and anosmia were more common in the CRS group (38.2% and 26.8%) than in the FB group (16.3% and 10.2% respectively; p < 0.01). Blood and tissue eosinophil counts were significantly higher in the CRS group (p < 0.01). When comparing concomitant chronic diseases, such as asthma, diabetes, hypertension, and chronic thyroid diseases, FB patients more commonly had concomitant diseases (p < 0.01); however, the prevalence of asthma alone was not significantly different between the two groups (p = 0.27). The incidence of revision surgery cases (p = 0.03) and smoker were more common in CRS (p < 0.01; Table 2).
Discussion
Fungal rhinosinusitis used to be an uncommon disease; however, its detection is increasing with improvements in endoscopic and radiologic technologies [7]. It comprises about 4–10% of surgically treated CRS patients, and FB is the most common subtype, accounting for 53–72% of the fungal rhinosinusitis cases [7, 11]. According to a previously published study in Korea, the prevalence of FB has increased steadily over the last 10 years, and our study also showed that the incidence of FB was significantly increased in 2016 [3, 5]. Global warming, increased air pollution, and increased allergen exposure can increase the incidence of FB. The global average surface air temperature has increased by about 0.3–06 °C in the last 100 years, and recent (1981–2002) air temperature change in Korea was also higher (0.043 °C per year) than before [14, 15]. Between 1973 and 2017, the average temperature in Korea increased about 0.5–2 °C. The incidence of FB was much higher in 2016, with increasing higher average temperature (12.1 °C in 2005, 12.2 °C in 2010, and 13.6 °C in 2016 based on the data from the Korea Meteorological Administration). However the humidity was similar among 3 years (60.4% in 2005, 60.1% in 2010, and 59.2% in 2016) [16]. Although we cannot conclude with certainty that global warming is an important risk factor for the development of FB, it may play a role in its pathogenesis. Korea has a typical four-season climate. In the spring (April), the average temperature is 14.1 °C and the relative humidity (RH) is 54.8%; in the summer (July), the average temperature is 26.2 °C with an RH of 72.9%; in the fall (October), the average temperature is 16.1 °C with an RH of 62.2%; and in the winter (January), the average temperature is − 3.2 °C with an RH of 53.0%. In our study, the incidence of FB was the highest in October. Although we cannot suggest the exact condition for the aggravation of FB symptoms, adequate temperature and humidity maybe influence the conditions of patient with increased chance to visit clinic.
Fine particulate matter (aerodynamic diameter ≤ 2.5 μm; PM2.5) has been an increasing concern in Korea since the middle of the 2010s, and PM2.5 levels influence not only respiratory diseases but also systemic diseases. The Korean government measured PM2.5 levels from 2015 (26 μg/mL in 2016) and we could not compare PM2.5 levels with previous years. Therefore, we do not suggest a role for PM2.5 in the pathogenesis of FB. Particulate matter 10 (PM10) might not influence the development of FB in Korea given that PM10 levels during the studied years were decreasing (57 μg/mL in 2005, 51 μg/mL in 2010, and 47 μg/mL in 2016 based on data from the Korea Meteorological Administration). Diabetes, estrogens, previous surgical interventions, and endodontic treatment are known risk factors for the development of FB [2, 7, 12]. In this study, the incidence of concomitant diseases, such as diabetes and hypertension, was much higher in FB; however, we could not determine whether concomitant diseases were a risk factor or not. Because FB developed in elderly patients and the age factor may influence the incidence of concomitant diseases. Because FB developed in elderly patients and the age factor may influence the incidence of concomitant diseases, we could not determine whether concomitant diseases were a risk factor or not. The prevalence of allergy (16.3%) and asthma (2.1%) in the FB was similar to that in the adult population in Korea (20–30% with atopy and 3–4% with asthma); thus, the allergic status might not influence the development of FB [16].
FB is typically found in older people and more predominantly in women [10, 17]. In this study, patients with FB were older than patients with CRS and were more likely to be women (36.7% women in CRS and 71.4% in FB). The most common clinical presentation of CRS is nasal obstruction as our study. According to the previous studies, the most frequently reported symptom of FB is purulent nasal discharge (50.8–64.4%) followed by facial pain (37.0–61.5%), nasal obstruction (54.1%), and postnasal drip (14.4–44.3%) [7, 10, 12]. However, in this study, nasal obstruction (28.6%) was the most common complaint followed by facial pain and postnasal drip, and some patients were incidentally discovered without clinical symptoms. These discrepancies might be due to the previous studies checking every common symptom of FB; however, our study evaluated only the chief complaints of FB patients. When comparing the CT findings in patients with CRS and FB, most cases of FB developed unilaterally and the maxillary sinus was commonly involved as has been reported previously [7, 10, 17]. Entrapment of the fungal spores in sinuses during respiration and obliteration of sinus ostium and secondary bacterial infection induce an environment conducive to fungal growth, such as decreased oxygen saturation, low-pH, and nourishment by infected nasal secretion.
Conclusion
The pathogenesis of FB is not completely understood. However, FB is commonly encountered in older women with the increased prevalence in Korea. Our findings revealed that FB had different clinical presentation, radiological findings, and prognosis from those of CRS. Appropriate surgical treatment of FB could provide excellent results with limited morbidity. Further studies are needed to better understand the pathophysiologic mechanisms underlying the development of FB.
References
Ferreiro JA, Carlson BA, Cody DT 3rd (1997) Paranasal sinus fungus balls. Head Neck 19:481–486
Park GY, Kim HY, Min JY, Dhong HJ, Chung SK (2010) Endodontic treatment: a significant risk factor for the development of maxillary fungal ball. Clin Exp Otorhinolaryngol 3:136–140
Lee JS, Shin SY, Lee KH, Kim SW, Cho JS (2013) Change of prevalence and clinical aspects of fungal ball according to temporal difference. Eur Arch Otorhinolaryngol 270:1673–1677
Shea KM, Truckner RT, Weber RW, Peden DB (2008) Climate change and allergic disease. J Allergy Clin Immunol 122:443–453 (quiz 454–455)
Lee HW, Kang SH, Jang KH, Kim DS, Shin SH, Ye MK (2017) Changes in etiologies and clinical characteristics of operated unilateral sinus diseases: comparison study between 2005 and 2015. Korean J Rhinol 24:26–30
deShazo RD, O'Brien M, Chapin K, Soto-Aquilar M, Swain R, Lyons M et al (1997) Criteria for the diagnosis of sinus mycetoma. J Allergy Clin Immunol 99:475–485
Grosjean P, Weber R (2007) Fungus balls of the paranasal sinuses: a review. Eur Arch otorhinolaryngol 264:461–470
Wani MK, Ruckenstein MJ, Parikh S (2001) Magnetic resonance imaging of the paranasal sinuses: incidental abnormalities and their relationship to patient symptoms. J Otolaryngol 30:257–262
Ferguson BJ (2000) Fungus balls of the paranasal sinuses. Otolaryngol Clin N Am 33:389–398
Nicolai P, Lombardi D, Tomenzoli D, Villaret AB, Piccioni M, Mensi M et al (2009) Fungus ball of the paranasal sinuses: experience in 160 patients treated with endoscopic surgery. Laryngoscope 119:2275–2279
Lop-Gros J, Gras-Cabrerizo JR, Bothe-Gonzalez C, Montserrat-Gili JR, Sumarroca-Trouboul A, Massegur-Solench H (2016) Fungus ball of the paranasal sinuses: analysis of our series of patients. Acta Oorrinolaringol Esp 67:220–225
Dufour X, Kauffmann-Lacroix C, Ferrie JC, Goujon JM, Rodier MH, Klossek JM (2006) Paranasal sinus fungus ball: epidemiology, clinical features and diagnosis. A retrospective analysis of 173 cases from a single medical center in France, 1989–2002. Med Mcol 44:61–67
Cho JH, Jeong YS, Lee YJ, Hong SC, Yoon JH, Kim JK (2009) The Korean version of the Sniffin' stick (KVSS) test and its validity in comparison with the cross-cultural smell identification test (CC-SIT). Auris Nasus Larynx 36:280–286
Barnes CS (2018) Impact of climate change on pollen and respiratory disease. Curr Allergy Asthma Rep 18:59
Koo MHSY, Lee JH (2006) Analyzing spatial and temporal variation of ground surface temperature in Korea. Econ Environ Geol 39:255–268
Ys C (2016) Practical guideline of asthma management—Korean guideline for asthma 2015. Korean J Med 90:298–306
Ledderose GJ, Braun T, Betz CS, Stelter K, Leunig A (2012) Functional endoscopic surgery of paranasal fungus ball: clinical outcome, patient benefit and health-related quality of life. Eur Arch Otorhinolaryngol 269:2203–2208
Author information
Authors and Affiliations
Contributions
Conceptualization: all authors. Data curation: all authors. Formal analysis: SGK. Methodology: all authors. Project administration: S-HS. Writing-original draft: DWK, YMK. Review and editing: DWK, YMK, and S-HS.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, D.W., Kim, Y.M., Min, JY. et al. Clinicopathologic characteristics of paranasal sinus fungus ball: retrospective, multicenter study in Korea. Eur Arch Otorhinolaryngol 277, 761–765 (2020). https://doi.org/10.1007/s00405-019-05738-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05738-5