Abstract
In the past 30 years, thanks in part to the advance of both endoscopic technology and imaging possibilities, the classification, diagnosis, and management of rhinosinusitis caused by fungi have been better defined. These are basically divided into invasive and non-invasive forms based on the presence or absence of microscopic evidence of fungal hyphae within the tissues. Among the non-invasive fungal sinus diseases, fungus ball has been increasingly reported and large published series have allowed better characterization of the disease and the treatment strategies. Fungus ball of the paranasal sinuses is defined as the non-invasive accumulation of dense fungal concrements in sinusal cavities, most often the maxillary sinus. To describe this entity, confusing or misleading terms such as mycetoma, aspergilloma or aspergillosis would be best avoided. Clinical presentation is non-specific and the diagnosis is usually suspected on imaging studies. Surgical treatment, usually through an endonasal endoscopic approach, is curative. In this paper, we review the clinical, radiological, and pathological presentation of the fungus ball of the paranasal sinuses as well as the surgical management with emphasis on the transnasal endoscopic approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence and prevalence of fungal rhinosinusitis, broadly defined as any kind of sinusonasal pathology related to the presence of fungi, are increasing, as is the diversity of pathogenic organisms [1].
It has been estimated that fungal rhinosinusitis is encountered in about 10% of the patients requiring surgery for the nose and the sinuses and that between 13.5 and 28.5% of all maxillary sinusitis is fungal or mixed fungal and bacterial infections [2, 3]. Furthermore recent and somewhat controversial reports suggest that fungi may play a major role in chronic sinusitis, since they can be cultured using sensitive methods in more than 95% of patients [4]. As a matter of fact the possibility of a fungal infection should always be considered in the differential diagnosis of difficult to treat diseases of the paranasal sinuses.
In the last two decades, the different clinical forms of fungal rhinosinusitis have been better defined and classified (Table 1)[1, 5–7]. In brief, the most commonly accepted classification divides fungal rhinosinusitis into invasive and non-invasive (also called extramucosal) forms, based on the presence or absence of microscopic evidence of fungal hyphae within the tissues (mucosa, blood vessels or bone), respectively.
The non-invasive form is by far the most prevalent and is classically further divided into allergic fungal sinusitis and the so-called fungus ball. However, other forms of non-invasive fungal diseases may also be included in this classification (Table 1). For example, simple contamination of nasal or sinusal cavities by fungi, called either superficial sinonasal mycosis [1] or saprophytic fungal infestation [8] has been described. This fungal colonization most often occurs in patients who had previous sinus surgery and may clinically be silent or presents with a foul smelling odour. Clinical examination shows crusts admixed with pus, the culture of which may yield bacteria as well as fungi.
In addition, the somewhat controversial eosinophilic fungal rhinosinusitis may also be included in the non-invasive form of fungal rhinosinusitis [4]. It is likely secondary to a non-allergic reaction to fungi and is characterized by the presence of fungi and cluster of eosinophils in the mucus. Finally, some authors also describe a form of non-invasive fungal sinusitis, so-called chronic erosive (non-invasive) sinusitis [9] or chronic non-invasive destructive sinusitis [10, 11]. This entity resembles the fungus ball, but is characterized by quite extensive disease and bone erosion on CT scan imaging without evidence of tissue invasion by fungi. Whether this represents a true separated entity from multiple sinus involvement by fungus ball remains unclear and it has therefore not been included in Table 1.
Correct diagnosis and classification of fungal sinusitis is paramount as management and prognosis among the various forms is greatly different. Unfortunately, retrospective study of paranasal sinus specimens obtained by functional endoscopic sinus surgery (FESS) have shown that fungal sinusitis is both often misdiagnosed or wrongly classified despite the presence of characteristic diagnostic features [12].
Fungus ball of the paranasal sinus have already been described in the end of the eighteenth century. Since then many cases have been reported and recently published large series have helped to better define the clinical spectrum, diagnosis, and therapy of the sinus fungus ball [13–16].
In this paper we review the clinical presentation, diagnosis, and treatment of the fungus ball of the paranasal sinuses based on a review of the recent literature.
Definition
In the literature, various terms such as mycetoma, aspergilloma, aspergillosis or chronic non-invasive fungal disease, have been used interchangeably to describe sinus fungus ball, that is the non-invasive accumulation of dense fungal concrements in sinus cavities [1, 17]. Unfortunately, many of these terms are inaccurate or misleading and lead to confusion.
Mycetoma is a chronic local invasive infection of the subcutaneous tissue that may extend to contiguous structure such as fascia or bone [18]. It is most often seen in the feet and hand. It can be caused by various fungi (eumycetoma) or by actinomycetes (actinomycetoma). Thus the use of the term mycetoma to describe grossly visible aggregate of fungi in paranasal sinus seems incorrect and would be better avoided.
Although in the past the term aspergillosis was used to describe both colonization and any form of sinus disease caused by Aspergillus [19], it is now used to mean either tissue invasive disease or allergic disease caused by Aspergillus and actually excludes simple saprophytic growth.
In the mid 1960s, British pathologists introduced the term aspergilloma to describe the clinically chronic and indolent form of locally invasive sinusitis most often observed in Sudan and caused mainly by Aspergillus flavus [20]. This entity is now referred to as granulomatous invasive fungal sinusitis [5, 6]. Later, aspergilloma was used to describe various entities of fungal sinusitis with Aspergillus as a pathogen. These include fungus ball, allergic fungal sinusitis, as well as, chronic (indolent) invasive fungal sinusitis.
In addition, it should be stressed that even if most fungal ball are made of Aspergillus, cultures are often negative and other species have also been implicated. Thus to describe a fungus ball both the terms aspergillosis and aspergilloma are inaccurate and should best be avoided.
Fungus ball seems therefore the more appropriate term. Recently diagnostic criteria have been proposed by de Shazo [13] and are presented in Table 2.
Of note is that although it is usually admitted that patients suffering from fungal ball of the paranasal sinus are immunocompetent, the immune status has not been included in the proposed diagnostic criteria. Fungus ball may also coexist with other forms of fungal sinusitis, most often the allergic fungal rhinosinusitis [13].
Epidemiology
Pathological reviews have shown that about 12% of patients undergoing sinus surgery and whose surgical specimen was submitted for histological analyses had some kind of fungal rhinosinusitis [12]. More precisely, fungus ball was encountered in 3.7% of the patients operated for chronic inflammatory conditions of the sinuses at the Mayo Clinic [14]. When considering only chronic maxillary sinusitis fungus ball is encountered in about 13–28.5% of the cases [2, 3].
Fungus ball of the paranasal sinuses is mostly encountered in older individuals with an average age at presentation being 64 years (range 14–90) [16, 21]. Of note is that no case has been reported in young children so far. In most series, a female predominance is noted (two female for one male). The association with pulmonary aspergillosis or pulmonary fungus ball has been only rarely described [22].
The disease is not contagious as the source of infection is endogenous and related to the growth of fungi from spores that often contaminate the upper airway of normal individuals.
Clinical presentation
Most patients present with non-specific complaints. In large studies in France 13.2–20% of patient with fungus ball were asymptomatic and the disease was incidentally discovered for example on head imaging [15, 21]. The slow and asymptomatic development of fungus ball and the non-specific symptoms often lead to late diagnosis. As a matter of fact, only 29% of patients with fungus ball are diagnosed within 1 year from the onset of symptoms [21]. When symptoms do occur, there are usually long lasting and not different from those of chronic sinusitis. The most frequent symptom is repeated (greater than two episodes per year) superimposed bacterial infection (observed in 58.5% of patients), followed by headache or facial pain (56.5%), postnasal drip (44.3%) with or without nocturnal cough, and cacosmia (20.9%). For sphenoid fungus ball, headache (typically retro-orbital, at the vertex, but also frontal or temporoparietal), post-nasal discharge, and cough are the most frequent symptoms [23, 24].
Much rarer clinical presentations include epistaxis, proptosis, neurological complaints such as seizure [13] or visual changes (blurred vision, transient loss of vision) [25–27], or even dysphonia [23]. The visual disturbance is attributed to optic neuritis. Most often symptoms are recurrent and unilateral.
Fungus ball is usually found in just one sinus, most frequently the maxillary sinus, followed by the sphenoid sinus. It should be noted that isolated opacification of sphenoid sinus is seen in less than 5% of patients with paranasal sinus disease. Of these only about 5% have fungal ball [27].
Between the superimposed bacterial infection episodes, the clinical examination is often normal. In the Klossek study, 52% of patient had a normal preoperative endoscopy [15]. Purulent nasal discharge is seen in about 38% of the cases. As in any case of chronic sinusitis a careful examination with rigid telescope or flexible endoscope is mandatory as the mucosal changes may be subtle and localized. For example, about 10% of patients have localized nasal polyps in the vicinity of the natural ostium of the involved sinus, which likely only represent an advance stage of nasal inflammation. In case of fungus ball of the sphenoid sinus however, the spheno-ethmoidal recess almost always shows some inflammatory mucosal changes with or without purulent discharge or polyps [23]. Very rarely fungus ball may be associated with large polyps protruding in the nasal cavity or vestibule [28].
When, based on the history or endoscopic findings mentioned above, a patient is suspected of having a fungal ball a computed tomography (CT) of the sinuses should be performed.
Blood examination is usually not contributory. In particular no peripheral eosinophilia can be detected.
Predisposing factors: immunology
Patients suffering from fungus ball are usually immunocompetent and only non-significant abnormalities in the serum immunoglobulin classes or IgG subclass level have been demonstrated [29]. Atopy is not more frequent than in the general population. Skin test for fungi and fungal specific IgE are usually negative [15]. Thus, these examinations should only be performed when there is suspicion of an associated allergic fungal rhinosinusitis.
Although fungus balls have been occasionally reported in combination with other pathology (diabetes mellitus, Wegener granulomatosis, asthma, lymphoproliferative diseases), these associations must be considered incidental. Only about 4% of the patients have diabetes mellitus [21].
No professional or private environmental predisposing factors have been demonstrated [21].
Predisposing local factors have been advocated but not clearly demonstrated [30]. For example local anatomical anomalies such as septal deviation or paradoxal curvature of the middle turbinate are encountered in only about 15% of patients with fungus ball [22], which is not higher than the frequency in the normal population. Furthermore, there seems to exist no association between previous or existing sinus pathology and the occurrence of a fungus ball [17].
A history of previous dental care and especially of dental filling is encountered in as many as 84% of patients diagnosed with fungus ball and seems to be the only predisposing factor [21]. However, much lower figures (56%) have also been reported [15]. As a matter of fact, the occurrence of fungus ball in patients without evidence of previous dental care and the observation of isolated fungus ball of the frontal or sphenoid sinus indicated that other yet unknown factors may play a role.
Imaging
On standard radiography, unilateral partial or complete opacification of a single sinus, usually the maxillary sinus, is the most frequent finding. Focal areas of increased density and well-defined hyperdense foci are observed in about 50 and 25% of patient, respectively [30]. These latter findings strongly suggest the diagnosis of fungal ball sinusitis. However, non-mycotic sinusitis secondary to a foreign body of dental origin may present with similar radiological findings.
CT however is the imaging procedure of choice giving both information on the usual surgical landmarks for an endonasal therapeutical approach and on extent and nature of the disease. A single sinus is involved in 94% of the cases and unilateral involvement is seen in almost 99% [15, 21]. Exceptionally, distinct and bilateral involvement of multiple sinus may occur [31]. The maxillary sinus is by far the most frequently involved sinus (94%) followed by the sphenoid sinus (4–8%). The ethmoid sinus is involved in about 3% most often as a continuous involvement from the maxillary sinus. The frontal sinus alone is implicated in only about 2% [15]. Very rarely a fungus ball in a concha bullosa has been described [16].
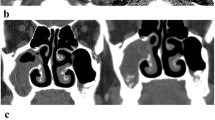
The most common CT finding, observed in about 90% of the cases is partial or often complete heterogeneous opacification of the involved sinus (Table 3; Fig. 1). In 10% of the cases, a homogenous opacification is observed. Microcalcifications or “metallic dense” spots, sometimes in combination are each seen in about one third of the cases in both homogenous and heterogeneous opacifications. The sensitivity and specificity of CT imaging, using sinus opacification and the presence of areas with hyperattenuation as diagnostic criteria for fungus ball, were calculated to be 62 and 99%, respectively [32]. In addition, the central opacification of the sinus is usually separated from the bony sinus wall by a thin zone of lower attenuation material [33]. Sclerosis of the bony wall of the involved sinus is common and observed in about 60% of the cases [14]. As a matter of fact the association of radiodense bodies or calcifications with sclerosis of the bony wall of an opacified sinus, although not pathognomonic, strongly suggests the diagnosis of a fungus ball.
In 4–17% of the cases bone erosion giving a pseudotumoral image has been reported. It has been suggested that this could represent an intermediate form between the non-invasive and invasive forms [34]. However in the Klossek study, no associate invasion of the mucosa was observed in such cases [15]. In addition, bone regeneration was observed both in postoperative imaging study or endoscopically even in case of exposed dura at the skull base. The bone erosion is thus reversible and seems to be mainly related to the inflammatory process induced by the growing of fungus and possible superimposed bacterial infection.
The nature of the metal dense spots is still debated. Stammberger proposed a fungal concrement phenomenon [30] whereas others stated they are due to overfilling of dental paste during endodontic treatment [35, 36]. It has been shown that certain calcium salts (mainly calcium phosphate and to a lesser degree calcium sulphate) were present within the fungal ball, especially in the necrotic centre of the fungus mass corresponding to the areas of high radiation density [30]. Other elements such as silver, lead, copper, cadmium, or mercury were also identified but were thought to play no significant role on the radiation density of the concrement.
In most cases of suspicious fungal ball magnetic resonance imaging (MRI) is not required. However, MRI may be indicated in case of sphenoidal as well as pansinus involvement when bone lysis is prominent and possible connection with orbital contents or brain structures must be excluded [16]. In case of homogenous involvement without microcalcifications or metallic dense spots, MRI may also be useful to differentiate a fungus ball from a mucocele (Table 3). In particular, T2-weighted images help to differentiate between fungus concretions—which display an iso- or hyposignal to brain or even signal void that may be mistaken for air—and mucosal swelling or mucous retention (hyperintense signal). The demonstrated higher concentration of iron and manganese in fungal aggregate compared to non-fungal sinusitis could explain this image [37]. In T1-weighted image fungus ball appears as a non-enhancing, often heterogeneous nodular hyposignal. However intrasinusal desiccated secretions, air or even acute clotted haemorrhage may also show hyposignal to signal void in T1 and T2 weighted [33]. After contrast, the inflamed peripheral mucosa may enhance.
Microbiology: fungal culture
Cultures are frequently negative and in only 23–50% of cultures can a fungus be grown [17]. This is probably related to the poor viability of fungal elements in the fungus ball. The most often cultured species is Aspergillus. In the Klossek study, 93% of the positive culture showed Aspergillus fumigatus [15]. Aspergillus fumigatus is an ubiquitous organism whose natural ecological niche is the soil where it grows on decomposing vegetable material. It sporulates abundantly producing conidia which are released in the atmosphere and which are small enough to reach not only the nose and sinuses but also the lung alveoli. Every human will inhale hundreds of A. fumigatus conidia per day, which in immunocompetent patients are normally easily eliminated by innate immunological defence [38]. Other fungus occasionally cultured are Scedosporium apiospermum (Pseudoallescheria boydii) [15], Aspergillus flavus, niger or terrus [14, 39], and Pleurophomopsis lignicola [40].
Case reports have been published in which the fungus ball was thought to be secondary to mucor [32, 41, 42]. However the identification of mucor was based only on the morphology on histological slides and this fungus has never been cultured in case of fungus ball. Thus, in such cases, the true identity of the involved fungus could be questioned.
Despite the relative poor yield of fungal culture, this should always be performed, as it is complementary to special staining techniques in correctly identifying the causative fungal species. In case of tissue invasion, which can only be ascertained or excluded by definitive microscopic examination, the accurate identification of the responsible fungus by culture may be crucial to direct the necessary antimycotic treatment.
Histopathology
Macroscopically, the fungus ball is characterized by grumous friable cheesy material, which can be green, yellow, brown or black and that is easily peeled off the mucosa (Fig. 2). The sensitivity and specificity of these positive gross findings observed during the operation were calculated to be 100 and 99%, respectively [32]. The fungus ball may partially or totally fill the cavity. Occasionally, fungus ball as small as 5 mm in diameter may cause symptoms [43]. Grossly, the mucosa of the involved sinus appears normal or may show oedema or hypertrophy.
Rarely, the fungus ball may accumulate so much calcium salts that it becomes bony hard and form an antrolith, so-called in analogy to the calcified foreign body called rhinolith in the nasal cavity [28]. Histological examination of antrolith may confirm the presence of a fungal nidus.
Microscopically, fungus ball is represented by an aggregate of tightly packed hyphae and often exhibits alternating zone of dense and less dense growth of the fungus giving a concentric onion skin-like appearance in low power microscopic examination. The fungus ball may be surrounded by a dense inflammatory exudate with abundant neutrophils. As fungus ball is an extramucosal fungal infection, neither fungal invasion nor granulomatous tissue reaction can be detected in the sinus mucosa samples. The mucosa however shows a non-specific inflammation in which plasma cells and lymphocytes predominate. Neutrophils and eosinophils are however also observed. Although fungus such as Aspergillus sp. can often be seen on haematoxylin–eosin (H&E) slides, periodic-acid-schiff (PAS) or silver impregnation stains are very helpful and should be done not only on the mucosal samples but also on the cheesy material removed. Gomory or Grocott methenamine silver stain in particular, employing deposition of silver onto the fungus wall, are the most sensitive to identify fungi [12]. As a matter of fact no histological specimen should be considered to be negative for fungus unless a silver stain has been performed. PAS works well in many cases but is less sensitive than silver stains because senescent fungal cells may not be stained. Its advantage is that it usually permits a better study of the fungus morphology, especially septations, than silver stain. These morphological characteristics of the fungus are however rarely sufficient to definitely identify the species. For example, Aspergillus species is recognized by its septae and 45° angle dichotomous branching hyphae. But other fungal hyphae such as Scedosporium, Fusarium and many other rarer fungi may mimic this [19]. Thus only culture can identify the fungal species with certainty. One exception is the rare visualisation of the sporulating head (conidiophores) and spores, which may help to further characterize the fungus [44].
Of note is that, unless in rare cases where association with allergic fungal rhinosinusitis was observed, allergic mucin is absent in fungus ball [12].
Pathogenesis
The pathogenesis of fungus ball remains unclear. Two ways of entry of the fungus have been suggested:
-
1.
the so-called “aerogenic” pathway in which high quantities of the airborne fungus spores enter the sinus through the natural ostium, and
-
2.
the odontogenic “iatrogenic” pathway in which colonization of the maxillary sinus by fungi occurs through a iatrogenic oro-antral communication secondary to dental extraction, periodontal destruction or most often endodontic treatment with over filling of the dental canal [39].
A combination of the two mechanisms is also possible. Then, heavy metals and especially zinc oxide contained in root canal sealants may affect the mucociliary clearance ability of the sinus mucosa, thus preventing the fungal spores to be eliminated. Furthermore, zinc is indispensable to activate the metabolism of the Aspergillus sp, thus favoring germination of fungal spores and fungal growth [35, 39].
This theory is supported by experimental work evaluating the known inhibiting properties of commonly used endodontic sealers on the growth of fungi, and especially Aspergillus, over time [39]. Theses sealers have two components: a powder containing zinc oxide and a liquid containing eugenol. Whereas the powder used alone permitted the growth of fungi, both the eugenol solution and the reconstituted sealers (mixture of powder and eugenol) inhibit Aspergillus growth. However, over time, the inhibiting effect of eugenol gradually fades away. It is therefore hypothesized that the endodontics sealers may promote fungal growth by the progressive loss of the inhibiting effect of eugenol on fungal growth over time and that the progressive diffusion of zinc in the sinus may in fact promote fungal development. This could explain the development of fungal ball many years after endodontic treatment.
However this theory cannot account for the fungus ball arising in remote sinus cavities such as the sphenoid or frontal sinus.
Furthermore, a history of dental care can only be elicited in about 84% of the cases [21]. Thus other factors must play a role. Closure of the ostium, leading to anaerobic and low pH environment, has been thought to favour fungus growth and to transform a saprophytic fungal colonisation into a pathological form [45, 46]. According to Stammberger, most fungal maxillary sinusitis are secondary to a chronic recurring sinusitis, the focus of which usually lies in the anterior ethmoid [45]. However this hypothesis has recently been challenged in a study showing that ostiomeatal complex obstruction is most often not observed in case of fungus ball of the maxillary sinus [47].
Diagnosis
The diagnosis of fungus ball should be considered in any case of recurrent or refractory sinusitis, especially when unilateral. The presence on the CT imaging of an opacified sinus with central metal dense spots, in the absence of previous history of foreign body, strongly suggests the diagnosis. Definitive diagnosis, however, is based chiefly on the characteristic macroscopic image and histopathology, as cultures are frequently negative [17]. In the Klossek study [15], when a fungus ball was macroscopically visualized, hyphae were detected microscopically in 94% of the cases using Grocott’s methenamine silver stain and in 72% of the direct smears were positive. Culture for fungus was positive in only 30% of the cases.
Positive culture results alone can be difficult to interpret if microscopy is negative. This is especially true if the cultured fungus is an unusual cause of rhinosinusitis. In these cases, a contamination must be considered. Also, histopathology is key to determine if the fungus has invaded host tissues, since invasive forms require systemic antifungal therapy.
According to Klossek, the intraoperative visualization of a fungal ball, the identification of fungus at histology, on smears or culture, the absence of mucosal invasion and negative serological results are necessary to make the diagnosis of fungus ball [15]. For others the exclusion of allergic mucin seems sufficient to exclude allergic fungal rhinosinusitis [13].
Treatment
There have been no published controlled series on the treatment of fungus ball. When a patient presents with symptoms and an opacified sinus on imaging studies, the indication for surgical treatment is clear.
Somehow more controversial may be the management of an asymptomatic patient with a homogenous opacified sinus and without any signs of bony erosion. However most authors recommend surgical treatment, if the sinus does not clear after medical therapy, as this usually indicates an uncommon histological finding such as tumour [48] or fungal sinusitis [49, 50]. Furthermore fungal sinusal disease may occasionally coexist with a malignant tumour [51].
Historically the Caldwell-Luc procedure has been the traditional approach [52]. Later a combination of canine fossa approach and FESS has been proposed [45]. Performing endonasal endoscopic sinus surgery with modern technology these external approaches seem to be obsolete in treating fungus balls. FESS combines both high success rate and low morbidity [15, 26].
The extent of the surgical procedure is tailored to the preoperative imaging study and the intraoperative findings. Basically, it requires a wide opening of the involved sinus or sinuses and complete removal of all the fungus concrements with the use of curved suctions and forceps. Whenever dental filling is present within the sinus, it should be thoroughly evacuated to avoid it serving as a nidus for regrowth of the fungus ball. Although the mucosa should be preserved, it must be biopsied to exclude any microscopic invasion by fungus. Some authors advocated rinsing the cavity with normal saline or with an iodine solution [53].
For fungus ball of the maxillary sinus, an uncinectomy and a wide middle meatus antrostomy is performed. There are some different opinions on which size the antrostomy should be. Some early reports have advocated a very large opening including removal of part or totality of the inferior turbinate [54]. With regard to the suspected pathogenesis, this seems not to be necessary in most cases as the goal of the opening is to allow sufficient access to the maxillary sinus cavity to remove all the fungus concrements, which is the key to successful treatment. In the Klossek study, the middle meatus antrostomy had to be associated with an inferior antrostomy in about 65% of the cases in order to facilitate access and removal of the fungal ball [15]. This seems to be especially necessary in case of a large and well-pneumatized maxillary sinus completely filled with fungal concretions. To verify complete removal of the fungal ball, the use of 30°, 45°, 70° or even 120° telescope may be required.
Sphenoid and ethmoid localizations can be successfully managed by endonasal sphenoidotomy and partial or complete ethmoidectomy, respectively [23].
The rare cases of frontal sinus fungus ball may be more difficult to manage. In the Dufour study, [16] although an endonasal access to the frontal sinus was possible in all four patients, insufficient visualization of the frontal cavity prevented complete removal of the fungus ball in two of them, despite the use of irrigation, which seems to have been done from a minimal external osteoplastic approach. Residual disease was later successfully treated through a combined endonasal and external osteoplastic approach. Theoretically, an enlarged frontal drainage (Draf Type III procedure) [55, 56] could help to overcome these shortcomings. However, treatment of frontal fungus ball using this technique has not yet been reported.
In the rare pan-sinus involvement, a combination of the above-mentioned procedures according to the extent of disease is used.
True sinus fungus ball requires no adjuvant local or systemic antimycotic treatment even if bone destruction is observed [15]. Broad spectrum systemic antibiotics are only given in cases of superimposed intra- or postoperative bacterial infection. Other postoperative care is similar to that used after FESS for chronic sinusitis and involves the short-term use of topical steroids and nasal irrigation with saline solution for a few weeks [16].
For the rare cases of sinus fungus ball occurring in immunocompromised patients some authors recommend adjunctive systemic antifungal treatment such as itraconazole, especially if bony erosion of the involved sinus is present [17]. The rationale for this is that post-operative progression to invasive fungal sinusitis was observed in an immunocompromised patient operated for a sphenoid fungus ball. Other authors prefer close clinical observation of the patient in such situations [57].
Prognosis
Surgical treatment most often results in definitive cure. Only very rare recurrences have been described after Caldwell procedure. Using a limited endoscopic canine fossa approach only, no recurrence was observed in 12 patients although the follow-up was short [53]. Also, only a minority of patients treated by FESS alone (4–7%) showed a recurrence or persistent disease after the first procedure [14, 16]. Persistent disease is most likely to occur in cases of major inflammatory reaction surrounding the fungus ball thus preventing adequate removal of fungal concrements. Recurrent or persistent disease is most often detected during investigations for persistent or recurrent symptoms such as postnasal discharge [15] and is most often diagnosed in the first 2 or 4 years after surgery. In 50% of these cases a closure of the sinusotomy is observed. Resolution can usually be achieved with a minimally invasive surgical procedure (reopening of the sinusotomy, suctionning and washing of the fungal concrements) [15]. Other authors propose a Caldwell Luc approach for recurrence of a maxillary fungus ball [14].
Follow up should be both clinically and endoscopically as most patients with persistent or recurrent disease have symptoms or abnormal findings on nasal endoscopy. The patency of the middle antrostomy as well as the maxillary sinus cavity and mucosal lining can be visualized using rigid angulated telescopes or the flexible fiber optic endoscope. In more than 86% of the patients treated the mucosa of the involved sinus returned to normal and in a minority endoscopic signs of inflammation or edema remained. Imaging studies should not routinely be performed during follow up as it provide less information than nasal endoscopy.
Complications
Untreated fungus ball of the paranasal sinuses may occasionally lead to complications. The most frequent is recurrent bacterial sinusitis, which may be explained by the fungal concrement acting as a foreign body. Mucoceles and pyoceles have also been reported [58]. Neurological complications have also been rarely described and include optic neuritis [25, 26], ophthalmoplegia and seizures [13]. If immunodeficiency develops however this non-invasive fungal colonization may become an invasive fungal infection [59]. The possibility for a fungus ball to progress to invasive fungal disease in immunocompetent patients has also been suggested but is not well documented [60, 61].
In most studies, complications of the surgical treatment are the same as those described in FESS for other diseases. However, one study surprisingly reports three patients with sphenoid fungus ball who died of intracerebral bleeding or infarct within one month after surgery [14]. In case of maxillary fungus ball, minor transitory tooth ache and post-nasal drip may be observed but complete recovery is the rule although it may take as long as 1 year.
Conclusion
Fungus ball should be suspected in any case of difficult to treat or recurrent unilateral sinusitis. In such situations, CT scan is the imaging procedure of choice. Typical although not pathognomonical findings include heterogeneous opacification of one sinus, usually the maxillary sinus associated with hyperdense foci and less frequently sclerosis of the sinus bony frame. FESS is nowadays the treatment of choice allowing excellent results with limited morbidity. Surgery is most often curative and no local or systemic antifungal therapy is required. Close follow-up is mandatory in immunodepressed patients.
References
Dhong HJ, Lanza DC (2001) Fungal rhinosinusitis. In: Kennedy DW, Bolger WE, Zinreich SJ (eds) Diseases of the sinuses: diagnosis and management. BC Decker Inc., Hamilton, pp 179–195
Bambule G, Grigoriu D, Savary M, Delacretaz J (1982) Les rhinosinusites mycosiques et leur traitement. Ann Otolaryngol Chir Cervicofac 99:531–535
Laskownick A, Kurdzielewica J, Macura A, Odrasinska-Cholewa B (1978) Mycotic sinusitis in children. Mykosen 21:407–411
Ponikau JU, Sherris DA, Kern EB, Homburger HA, Frigas E, Gaffey TA, Roberts GD (1999) The diagnosis and incidence of allergic fungal sinusitis. Mayo Clin Proc 74:877–884
Schubert MS (2001) Fungal rhinosinusitis: diagnosis and therapy. Curr Allergy Asthma Rep 1:268–276
deShazo RD, O’Brien M, Chapin K, Soto-Aguilar M, Gardner L, Swain R (1997) A new classification and diagnostic criteria for invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg 123:1181–1188
Stammberger H (2004) Classification of fungal disease. International Conference about Controversies in Paranasal Sinus Surgery, Zürich, 1 October 2004
Ferguson BJ (2000) Definitions of fungal rhinosinusitis. Otolaryngol Clin North Am 33:227–235
Uri N, Cohen-Kerem R, Elmalah I, Doweck I, Greenberg E (2003) Classification of fungal sinusitis in immunocompetent patients. Otolaryngol Head Neck Surg 129:372–378
Jones JMR, Moore-Gillon V (1994) Destructive non-invasive paranasal sinus aspergillosis: component of spectrum of disease. J Otolaryngol 23:92–96
Panda NK, Balaji P, Chakrabarti A, Sharma SC, Reddy CE (2004) Paranasal sinus aspergillosis: its categorization to develop a treatment protocol. Mycoses 47:277–283
Granville L, Chirala M, Cernoch P, Ostrowski M, Truong LD (2004) Fungal sinusitis: histologic spectrum and correlation with culture. Hum Pathol 35:474–481
deShazo RD, O’Brien M, Chapin K, Soto-Aguilar M, Swain R, Lyons M, Bryars WC, Alsip S (1997) Criteria for the diagnosis of sinus mycetoma. J Allergy Clin Immunol 99:475–485
Ferreiro JA, Carlson BA, Thane Cody III D (1997) Paranasal sinus fungus ball. Head Neck 19:481–486
Klossek JM, Serrano E, Péloquin L, Percodani J, Fontanel JP, Pessey JJ (1997) Functional endoscopic sinus surgery and 109 mycetomas of the paranasal sinuses. Laryngoscope 107:112–117
Dufour X, Kauffmann-Lacroix C, Ferrie JC, Goujon JM, Rodier MH, Karkas A, Klossek JM (2005) Paranasal sinus fungus ball and surgery: a review of 175 cases. Rhinology 43:34–39
Ferguson BJ (2000) Fungus balls of the paranasal sinuses. Otolaryngol Clin North Am 33:389–398
Mahgoub ES (2000) Agents of mycetoma. In: Mandell GL, Bennett JE, Dolin R (eds) Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, 5th edn. Churchill Livingstone, Philadelphia, pp 2702–2706
Denning DW (2000) Aspergillus species. In: Mandell GL, Bennett JE, Dolin R (eds) Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, 5th edn. Churchill Livingstone, Philadelphia, pp 2674–2684
Milosev B, el-Mahgoub S, Aal OA, el-Hassan AM (1969) Primary aspergilloma of paranasal sinuses in the Sudan. A review of seventeen cases. Br J Surg 56:132–137
Barry B, Topeza M, Gehanno P (2002) Aspergillosis of the paranasal sinus and environmental factors. Ann Otolaryngol Chir Cervicofac 119:170–173
Serrano E, Percodani J, Flores P, Dilem S, Pessey JJ (1996) Les aspergillomes sinusiens. A propos de 45 cas. Ann Otolaryngol Chir Cervicofac 113:86–91
Klossek JM, Peloquin L, Fourcroy PJ, Ferrie JC, Fontanel JP (1996) Aspergillomas of the sphenoid sinus: a series of 10 cases treated by endoscopic sinus surgery. Rhinology 34:179–183
Yiotakis I, Psarommatis I, Seggas I, Manolopoulos L, Ferekidis E, Adamopoulos G (1997) Isolated sphenoid sinus aspergillomas. Rhinology 35:136–139
Müller T, Wolf SR, Velten I (2001) Beidseitiger, progredienter Visusverlust. HNO 49:406–407
Simmen D, Briner HR, Schär G, Schuhknecht B (1998) Chronische Mykosen der Nasennebenhöhlen—Stellenwert der endonasalen Nasennebenhöhlenchirurgie. Laryngorhinootologie 77:445–453
Sethi DS (1999) Isolated sphenoid lesions: diagnosis and management. Otolaryngol Head Neck Surg 120:730–736
Wu CW, Tai CF, Wang LF, Tsai KB, Kuo WR (2005) Aspergillosis: a nidus of maxillary antrolith. Am J Otolaryngol Head Neck Med Surg 26:426–429
Jiang RS, Hsu CY (2004) Serum immunoglobulins and IgG subclass levels in sinus mycetoma. Otolaryngol Head Neck Surg 130:563–566
Stammberger H, Jakse R, Beaufort F (1984) Aspergillosis of the paranasal sinuses. X-ray diagnosis, histopathology, and clinical aspects. Ann Otol Rhinol Laryngol 93:251–256
Ting-Kuang Chao (2004) Triple discrete fungus balls of the paranasal sinuses. Otolaryngol Head Neck Surg 131:1014–1015
Dhong HJ, Jung JY, Park JH (2000) Diagnostic accuracy in sinus fungus balls: CT scan and operative findings. Am J Rhinol 14:227–231
Som PM, Dillon WP, Curtin HD, Fullerton GD, Lidov M (1990) Hypointense paranasal sinus foci: differential diagnosis with MR imaging and relation to CT findings. Radiology 176:777–781
Rowe-Jones JM, Moore-Gillon V (1994) Destructive non-invasive paranasal sinus aspergillosis: component of a spectrum of disease. J Otolaryngol 23:92–96
Beck-Mannagetta J, Necek K, Grasserbauer M (1983) Solitary aspergillosis of maxillary sinus: a complication of dental treatment. Lancet 2:1260
Legent F, Billet J, Beauvillain C, Bonnet J, Miegeville M (1989) The role of dental canal fillings in the development of Aspergillus sinusitis. a report of 85 cases. Arch Otorhinolaryngol 246:318–320
Zinreich SJ, Kennedy DW, Malat J, Curtin HD, Epstein JI, Huff LC, Kumar AJ, Johns ME, Rosenbaum AE (1988) Fungal sinusitis: diagnosis with CT and MR imaging. Radiology 169:439–444
Latge JP (1999) Aspergillus fumigatus and aspergillosis. Clin Microbiol Rev 12:311–350
Mensi M, Salgarello S, Pinsi G, Piccioni M (2004) Mycetoma of the maxillary sinus: endodontic and microbiological correlations. Oral Surg Oral Med Oral Path Oral Radiol Endod 98:119–123
Padhye AA, Gutekunst RW, Smith DJ, Punithalingam E (1997) Maxillary sinusitis caused by Pleurophomopsis lignicola. J Clin Microbiol 35:2136–2141
Henderson LT, Robbins T, Weitzner S, Dyer TC, Jahrsdoerfer RA (1988) Benign Mucor colonization (fungus ball) associated with chronic sinusitis. South Med J 81:846–850
Goodnight J, Dulguerov P, Abemayor E (1993) Calcified mucor fungus ball of the maxillary sinus. Am J Otolaryngol 14:209–210
Matjaz R, Jernej P, Mirela KR (2004) Sinus maxillary mycetoma of odontogenic origin: case report. Braz Dent J 15:248–250
Schell WA (2000) Histopathology of fungal rhinosinusitis. Otolaryngol Clin North Am 33:251–276
Stammberger H (1985) Endoscopic surgery for mycotic and chronic recurring sinusitis. Ann Otol Rhinol Laryngol 94(Suppl119):1–11
Eloy P, Bertrand B, Rombeaux P (1997) Mycotic sinusitis. Acta Otorhinolaryngol Belg 51:339–252
Tsai TL, Guo YC, Ho CY, Lin CZ (2006) The role of ostiomeatal complex obstruction in maxillary fungus ball. Otolaryngol Head Neck Surg 134:494–498
Shaw CL, McLeave M, Wormald PJ (2000) Unusual presentations of isolated sphenoid fungal sinusitis. J Laryngol Otol 114:385–388
Eichel BS (1997) The medical and surgical approach in management of the unilateral opacified antrum. Laryngoscope 87:737–750
Kaplan BA, Kountakis SE (2004) Diagnosis and pathology of unilateral maxillary sinus opacification with or without evidence of controlateral disease. Laryngoscope 114:981–985
Tanaka T, Nishioka K, Naito M, Masuda Y, Ogura Y (1985) Coexistence of aspergillosis and squamous cell carcinoma in the maxillary sinus proven by preoperative cytology. Acta Cytol 29:73–78
De Freitas J, Lucente FE (1988) The Caldwell Luc procedure. Institutional review of 670 cases, 1975–1985. Laryngoscope 98:1297–1300
Chobillon MAJ, Jankowski R (2004) What are the advantages of the endoscopic canine fossa approach in treating maxillary sinus aspergillomas? Rhinology 43:230–235
Gilain L, Planquart X, Coste A, Lelievre G, Peynegre R (1992) Résultats du traitement des aspergilloses du sinus maxillaire par voie de méatotomie moyenne exclusive. Ann Oto-Laryngol (Paris) 109:289–293
Draf W (1991) Endonasal micro-endoscopic frontal sinus surgery. The fulda concept. Op Tech Otolaryngol Head Neck Surg 2:234–240
Weber R, Draf W, Kratzsch B, Hosemann W, Schaefer SD (2001) Modern concepts of frontal sinus surgery. Laryngoscope 111:137–146
Adelson RT, Marple BF (2005) Fungal rhinosinusitis: state-of-the-art diagnosis and treatment. J Otolaryngol 34(Suppl1):S18–S22
Swoboda H, Ullrich R (1992) Aspergilloma in the frontal sinus expanding into the orbit. J Clin Pathol 45:629–630
Gungor A, Adusumilli V, Corey JP (1998) Fungal sinusitis: progression of disease in immunosuppression. A case report. Ear Nose Throat J 77:207–215
Thiagalingam S, Fernando GT, Tan K, O’Donnell BA, Weeks K, Branley M (2004) Orbital apex syndrome secondary to Pseudallescheria boydii fungal sinusitis in an immunocompetent patient. Clin Exp Ophtalmol 32:545–547
Senocak D, Kaur A (2004) What’s in a fungus ball? Report of a case with submucosal invasion and tissue eosinophilia. Ear Nose Throat J 83:696–698
Acknowledgments
P. Grosjean benefits from a grant from SICPA SA, Lausanne, Switzerland, Fondation G. Dreyfus, Lausanne, Switzerland, Fonds Decker and Fonds de Perfectionnement du CHUV, Lausanne, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grosjean, P., Weber, R. Fungus balls of the paranasal sinuses: a review. Eur Arch Otorhinolaryngol 264, 461–470 (2007). https://doi.org/10.1007/s00405-007-0281-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-007-0281-5