Abstract
Fungal ball in paranasal sinus was reported to be rare, but these days we have encountered numerous cases. We retrospectively analyzed the data of 4,485 patients with chronic rhinosinusitis (CRS) who underwent sinus surgery from 1999 to 2010. Patients were categorized into group A (patients from 1999 to 2004) and group B (patients from 2005 to 2010). We compared the prevalence and clinical aspects of fungal ball between the two groups by analyzing the medical records, PNS CT findings, surgical findings, and pathologic reports. One hundred and twelve patients were diagnosed with fungal ball during the study periods. The prevalence of fungal ball was 0.9 % (23/2,333) in group A and 4.1 % (89/2,152) in group B, showing that it increased 4.6 times over 6 years. The prevalence of underlying diseases was 21.7 % (5/23) for hypertension and 8.7 % (2/23) for diabetes in group A, and 23.6 % (21/89) for hypertension and 14.6 % (13/89) for diabetes in group B. On PNS CT examination, calcification was identified in 78.2 % (18/23) of cases in group A and 44.9 % (40/89) in group B. The most involved paranasal sinus in group A was the co-involved maxillary and ethmoid sinuses at 26.1 % (6/23), whereas, the most prevalent involved sinus in group B was the maxillary sinus at 33.7 % (30/89). We found that the prevalence of fungal ball has increased steadily each year since 2005, accompanied by changes in the clinical aspects. These facts should be kept in mind when diagnosing and treating patients with medically intractable CRS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fungal rhinosinusitis in the nasal cavity and paranasal sinuses were considered uncommon in the past, but the diagnosis rate has noticeably increased due to improvements in endoscopic and radiologic technologies over the past 30 years [1]. The frequency of fungal rhinosinusitis tends to be higher in patients with immune deficiencies such as AIDS, leukemia, organ transplants, chemotherapy-induced immunodepression, diabetes, or steroid and antibiotic treatments [2]. And, we hypothesized that climate change, including global warming and Asian dust storms, is another influencing factor. Global warming has increased sensitization to air-borne allergens, especially pollen and mold [3]. Asian dust is known to contain bacteria, virus, and fungus that cause damage to the upper and lower respiratory tracts. South Korea is facing two climate-related problems these days.
Fungal ball is the most common subtype of fungal rhinosinusitis. A clinico-pathological report from the Mayo Clinic stated that fungal balls are found in 3.7 % of chronic rhinosinusitis (CRS) patients [4]. The most common species of fungus found in fungal ball patients is Aspergillus spp., which are reported to be found in 93 % of fungal ball patients [5]. The preferred treatment of fungal ball is complete removal through functional endoscopic sinus surgery, and this is associated with a low recurrence rate.
Clinically, we have observed many more cases of fungal ball within the past few years than in the past. The aim of this study was to identify the changes in prevalence and clinical aspects of patients with fungal ball infections over the past 12 years and to investigate the potential factors that influence the prevalence of fungal ball.
Materials and methods
Subjects
A total of 4,485 patients who were diagnosed with CRS and underwent sinus surgery at Kyung Hee Medical Center during the past 12 years were enrolled in this study, and the prevalence of fungal balls was inspected using medical records, surgical findings, PNS CT findings, and pathologic reports. The patients were categorized into group A, that included patients from 1999 to 2004, and group B, that included patients from 2005 to 2010, to analyze and compare fungal ball prevalence, age, underlying diseases, PNS CT results, and surgical findings between the two groups. Because the year 2005 was the median time for our investigation, and was the year noted for the acceleration of climate changes according to the Korean Meteorological Administration, we categorized the patients into group A and group B by the year 2005. Only fungal ball diagnoses that were in accordance with the clinico-pathological diagnosis criteria suggested by deShazo [6] were considered (Table 1). Climate data from 1999 to 2010 were obtained from the Korean Meteorological Administration. The study design was approved by the Institutional Review Board of Kyung Hee University Medical Center.
Statistical analysis
For statistical analysis, SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used to perform the Mann–Whitney U test to detect differences between items in each group. Pearson correlations were performed to identify correlations between the prevalence of fungal ball in CRS patients and alterations in Korean climate such as change in mean annual temperature and increases in the occurrence of Asian yellow dust storms.
Results
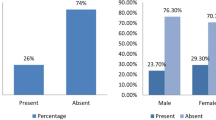
Among the 4,485 patients who underwent CRS surgery, including endoscopic sinus surgery and the Caldwell-Luc approach, from 1999 to 2010, 112 had a fungal ball for a prevalence of 2.5 %. The number of male patients was 32 and those of females was 80. Mean (±SD) age was 41 (±14) and age distribution was from 41 to 78 years. Female patients over 50 showed higher prevalence (32.7 %) than other patients and the number of fungal ball patients. There were no patients who had malignancy or immunocompromised state. The prevalence of fungal ball in group A was 0.9 % (23/2,333) while that of group B was 4.1 % (89/2,152), showing a significant increase of 4.6-fold over 6 years, and the prevalence of fungal ball increased rapidly from 2004 onward (Fig. 1).
Group B had a higher prevalence of the underlying diseases of hypertension and diabetes, with hypertension occurring in 21.7 % (5/23) patients and diabetes occurring in 8.7 % (2/23) patients of group A, and hypertension in 23.6 % (21/89) and diabetes in 14.6 % (13/89) in group B. These differences were only significant in diabetes between the two groups (Table 2).
In PNS CT, 78.2 % (18/23) in group A and 44.9 % (40/89) in group B showed calcification intensities. The most commonly involved regions of the sinus differed between the two groups, with both the maxillary and ethmoid sinuses being co-involved in 26.1 % (6/23) of group A and the maxillary sinus alone being involved in 33.7 % (30/89) of group B. It was also noted in two cases that fungal ball involved only the sphenoid sinus in group B (Table 2).
There were positive correlations between the prevalence of fungal ball and changes in climate including the frequency of Asian yellow dust storms and the average temperature in Korea over the past 12 years (Fig 1; Table 3).
Discussion
As a genus of the ascomycetes group, Aspergillus is pervasive throughout the world and is the strain most commonly involved in the formation of fungal ball. A number of fungi are found in food, fruit, grains, and flowers. A specific type of Aspergillus spore mingles with dirt that enters human hosts through the respiratory organs under favorable climatic conditions. In such cases, the respiratory organs then function as reservoirs of infection. In particular, when the respiratory organs are exposed to fine dust and Aspergillus spores for long periods of time, fungus is able to invade the damaged human paranasal sinus mucosa, resulting in infection. In addition, the overuse of antibiotics, anti-histamines, and steroids causes overgrowth of fungus by changing the immune defense system of the microbial flora within the paranasal sinus mucosa, resulting in increased sensitivity of the host to fungal infection [6–8].
Aspergillosis in sinus was first reported by Schubert [9]. Stammberger [10] reported that 10 % of patients who had sinus surgery were infected by fungus, and Park [11] and Lee [12] reported fungal infection rates of 1 and 4 %, respectively. In this study, we found that the overall prevalence of fungal ball in CRS during the past 12 years was 2.5 %. However, the prevalence before and after year 2005 were not equal. From 1999 to 2004, the prevalence was 0.9 %, while from 2005 to 2010 it was 4.1 %, meaning that the prevalence increased by 4.6 times in 6 years. The intermittent increase in the prevalence of fungal ball infection that started in the early 2000s changed to a rapid increase from the year 2005. The authors assumed that the reason for the increase might be climate change. Other reasons might be the above-mentioned improvements in diagnostic technology, an increase in the number of immunosuppressive patients, and the overuse of antibiotics or steroids. Fungus within the fungal ball itself proliferates when exposed to high temperatures [13], and subtropicalization brings increases in average annual temperatures and rainfall. The climate change for this period in Korea showed a 0.05 °C increase in temperature which is a similar rate of change as the change in prevalence of fungal ball in the past 10 years. Frequent exposure to fine dust or dusty wind containing microorganisms, viruses, and fungi could affect the morbidity rate of fungal ball. Considering past examples in areas such as Great Britain where atmospheric phenomena similar to that of Asian dust caused increases in Aspergillus infections, it could be inferred that the introduction of microorganisms carried by dusty wind not only aggravates the prevalence of asthma and other basal lung diseases, but also influences the prevalence of fungal ball due to infection by the microorganism itself [14]. As the frequency of Asian yellow dust storms has been increasing in Korea since the early 2000s and the phenomenon is considered to be a manifestation of major climate change in the Korean peninsula, it is conceivable that the increased frequency of exposure to Asian yellow dust storms influences the pathophysiology of the fungal ball to some extent (Fig. 2; Table 3).
While CRS caused by microorganisms is found in subjects of all ages, the age distribution of fungal ball infection is more frequent in subjects over 30 years, and its highest frequency is reported in middle-aged females [12, 15, 16]. In this study, the prevalence of fungal ball was the highest both in male and female patients between the ages of 50 and 59 years, which was in concordance with preceding reports.
Unlike patients with fulminant or invasive subtypes of fungal sinusitis, many fungal ball patients have normal immune systems, and the relationship between fungal ball sinusitis and chronic disease has not been confirmed [1]. In this study, we also could not detect a significant correlation between fungal ball and underlying diseases. However, the prevalence of diabetes in fungal ball patients of group B was 14.6 %, which is higher than the 8.7 % prevalence of group A. This observation suggests that there may be a relationship between chronic wasting diseases such as diabetes and the occurrence of fungal ball. And, it is thought that various factors in diabetes were influenced to the patients as like altered microvasculation of nasal mucosa, decrease of mucociliary clearance and increase of sensitivity to fungus, etc. [17].
CT of the sinus is performed to detect fungal balls and to recognize sinus invasion, and calcified partial hyperintensity is usually inspected by this method. From the 12 years of patient records with image data, we observed calcified intensity in 58 (51.7 %) of 112 cases. Maxillary invasion was seen in 35 cases (31.3 %) and invasion of both the maxillary and ethmoid sinuses was found in 31 cases (27.7 %); these results were similar to those of previous studies [18]. The location of sinus invasion was not significantly different between group A and group B. Mucociliary propagation and drainage of the maxillary and ethmoid sinuses are expected to play crucial roles in determining the location of invasion [2]. However, the reason why the more recent cases (group B) were more likely to have invasion limited to the maxillary sinus compared to the more extensive invasion seen in the earlier cases (group A) is thought to be due to improvements in care resulting in earlier diagnoses before spread to the ethmoid sinus. Earlier diagnosis is thought to underlie the recent increase in the rate of early diagnosis for CRS. In addition, the decreased rate of calcification determined by PNS CT in the last 6 years is also thought to be related to earlier diagnosis prior to the formation of calcification in the maxillary or ethmoid sinus. Based on these findings, earlier endoscopic sinus surgery is recommended for patients with medically intractable CRS that may be due to fungal ball.
Conclusions
The affiliation’s prevalence of fungal ball has increased steadily each year since 2005, accompanied by changes in clinical aspects. We have to keep in mind these facts when diagnosing and treating patients with medically intractable CRS. Additional studies related to environmental factors influencing fungal ball need to be done in the future.
References
Pierre G, Rainer W (2007) Fungal balls of the paranasal sinuses: a review. Eur Arch Otorhinolaryngol 264:461–470
Kim SW, Park YJ, Kim SW, Kang MG, Joo YH, Cho JH (2005) A clinical analysis of fungal sinusitis. Korean J Otolaryngol 48:332–337
Shea KM, Truckner RT, Weber RW, Peden DB (2008) Climate change and allergic disease. J Allergy Clin Immunol 122(3):443–453
Ferreiro JA, Carlson BA, Thane Cody D 3rd (1997) Paranasal sinus fungus ball. Head Neck 19:481–486
Klossek JM, Serrano E, Péloquin L, Percodani J, Fontanel JP, Pessey JJ (1997) Functional endoscopic sinus surgery and 109 mycetomas of paranasal sinuses. Laryngoscope 107(1):112–117
deShazo RD, O’Brien M, Chapin K, Soto-Aguilar M, Swain R, Lyons M, Bryars WC Jr, Alsip S (1997) Criteria for the diagnosis of sinus mycetoma. J Allergy Clin Immunol 99:475–485
McGuirt WF, Harrill JA (1979) Paranasal sinus aspergillosis. Laryngoscope 89:1563–1568
Latge JP (1999) Aspergillus fumigatus and aspergillosis. Clin Microbiol Rev 12:311–350
Schubert J (1885) um Kasuistick des Aspergillusmykosen. Ditch Arch Klin Med 36:162
Stammberger H (1985) Endoscopic surgery for mycotic and chronic recurring sinusitis. Ann Otol Rhinol Laryngol Suppl 119:1–11
Park JH, Lee KC, Lee JH, Lee SD, Lee YB (1994) Clinical evaluation of fungal sinusitis. Korean J Otolaryngol 37:511–516
Lee BJ, Kim H, Kim JH, Kim YJ (1998) Fungal sinusitis: clinical features and treatment outcomes with emphasis on endoscopic sinus surgery. Korean J Otolaryngol 41:318–322
Peter JC, Ramon JG (2007) Influences of climate on aflatoxin producing fungi and aflatoxin contamination. Int J Food Microbiol 119:109–115
Park JW, Lim YH, Kyung SY, An CH, Lee SP, Jeong SH (2005) Detection of pathogenic viruses in the atmosphere during Asian dust events in Incheon City. Tuberc Respir Dis 59(3):266–271
Min YG, Kang MK, Lee JW, Choo MJ, Lee KS (1993) A clinical study of mycotic sinusitis. Korean J Otolaryngol 36:292–301
Kim YD, Bai CH, Kwon OC, Choi CG, Suh JS, Song KW (1997) Endoscopic sinus surgery of Aspergillus sinusitis. Korean J Otolaryngol 40:1531–1536
Müller M, Betlejewski S (2003) Nasal mucosa in patients with diabetes mellitus. Otolaryngol Pol 57(3):361–364
Kim BK, Kwon SH, Kim CH (2003) A clinical analysis of 60 cases of mycetoma. J Clin Otolaryngol 14:70–75
Acknowledgments
This research was supported by the Kyung Hee University Research Fund in 2010(KHU-2010-0690).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, J.S., Shin, S.Y., Lee, K.H. et al. Change of prevalence and clinical aspects of fungal ball according to temporal difference. Eur Arch Otorhinolaryngol 270, 1673–1677 (2013). https://doi.org/10.1007/s00405-012-2234-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-012-2234-x