Abstract
Chronic rhinosinusitis (CRS) is widely prevalent globally. Fungal rhinosinusitis is a subtype which requires early detection by using appropriate tests and to make an accurate decision regarding the treatment modality. This study aims at determining the clinicomycological profile of fungal rhinosinusitis (FRS). A total of 105 patients with CRS were included in the study which was prospectively done during a time period of 18 months in a tertiary care hospital. All patients were subjected to CT scans and diagnostic nasal examinations (DNE) preoperatively. The sinonasal specimens were subjected to KOH mount, fungal culture and histopathological examination following functional endoscopic sinus surgery (FESS). 53% of the patients with fungal sinusitis belonged to the age group 41–60 years. The prevalence of FRS was found to be 38% with aspergillus species accounting for about 85% cases. FRS is a disease which can have a wide spectrum of clinical presentations requiring early detection and appropriate treatment which is essential to avoid both short term and long term sequalae.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term rhinosinusitis means inflammation of the mucosa lining nose and paranasal sinuses (PNS) and it has almost completely replaced the term sinusitis due to the contiguous nature of the mucosa lining the nose and PNS. Rhinosinusitis affects almost 20% of the population globally [1].
Rhinosinusitis can be broadly classified into acute and chronic variants. Acute rhinosinusitis is usually due to an infection and depends on the host’s immune response and the type of microorganism. This can either end with self resolution of symptoms or can lead to serious morbidity and mortality [2]. Rhinosinusits is termed chronic when it lasts for atleast 12 weeks or more [3]. Chronic rhinosinusitis (CRS) disorders are heterogenous in nature due to different pathophysiologies which include the following – failure of an infection to resolve, chronic inflammatory disorder or a mix of persistent inflammation and infection [3,4,5,6,7].
Fungal rhinosinusitis can be broadly defined as a spectrum of diseases caused by fungal infections to nose and paranasal sinuses [8]. FRS can be broadly classified into invasive and non invasive types based on tissue invasion detected clinicopathologically [9,10,11]. Aspergillus is generally the most common pathogen which causes fungal infections in nose and PNS. Fungal infections can occur in all age groups but the symptomatology differs with the immune status of the individual. A clinician requires a high index of suspicion in patients presenting with non specific symptoms of CRS who are not responding to conventional antibiotic therapy to diagnose fungal rhinosinusitis [12]. There has been an increase in incidence of fungal sinusitis and this can be attributed to better diagnostic testing modalities and increase in the specimens being send for fungal staining and culture.
Most of the studies about fungal sinusitis have been published from the European and American continents in spite of the high incidence of fungal infections in India which is attributable to favorable moist and humid climatic conditions. The aim of our study was to find the prevalence and clinicomycological profile of fungal rhinosinusitis.
Materials and methods
This was a prospective study conducted in tertiary care centre during the time period November 2015 to May 2017. Approval was obtained from the institutional review board of our institute for conducting the study. A total of 105 patients who presented with chronic rhinosinusitis (CRS) in our outpatient department were included in this study.
Inclusion criteria comprised of all patients of the age group 16 to 60 years who presented with symptoms of CRS and were subjected to endoscopic sinus surgery were included in the study. Patients who had a history of previous endoscopic sinus surgeries were excluded from the study. A detailed consent was taken from the patient prior to the surgery.
A detailed history of all patients were collected which included age, sex, co morbidities, symptomatology and complications. Routine blood work up, diagnostic nasal endoscopy and CT scans were done for all the patients preoperatively. All patients underwent functional endoscopic sinus surgery. The specimen which was collected during the surgery was sent for histopathological examination, KOH staining and fungal culture separately. All the data collected was recorded in a pre formed proforma.
Data was entered into an MS Excel sheet and analysis was done using relevant statistical tools.
Results
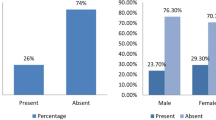
A total of 105 cases of CRS were included in the study with 67 (63.8%) males and 38 (36.2%) females. The incidence of fungal sinusitis in our study was 38%. 52% cases of fungal sinusitis were diagnosed in females and 48% in males. Highest incidence was noted in the 5th and 6th decade of life (52.5%). The mean age of patients with fungal sinusitis was 41.05 years.
22% of cases of fungal sinusitis were found in patients with agriculture as their occupation and 60% of cases were diagnosed during the monsoon season. There was no significant relationship between smoking and alcohol consumption in the incidence of fungal sinusitis. (p-0.4 and p-0.7 respectively)
In our study, 1 patient was HIV positive and 3 were HbsAg positive and all of them were diagnosed with fungal sinsusitis. 68% of diabetic patients were diagnosed with fungal sinusitis. 42.5% cases of fungal sinusitis cases were found to be diabetic. 23.1% patients with allergy had fungal sinusitis. Diabetes mellitus (p < 0.0001) and immune status (HbsAg, p-0.02) shows a statistically significant correlation to the incidence of fungal sinusitis. The mean RBS value was determined to be 153.68 and mean Hba1c value for fungal sinusitis cases were found to be 9.4 based on this study, hence proving that poor diabetic control is an important factor predisposing to fungal sinusitis.
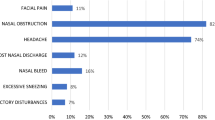
The most common clinical symptoms observed in our study were nasal obstruction (72.5%) and headache (57.5%). The other symptoms included nasal discharge, excessive sneezing, nasal bleed, post nasal discharge, facial pain and olfactory disturbances. (Fig. 1)
On clinical examination the following were observed in the patients with fungal sinusistis – anterior rhinoscopy showed that 6 had congested mucosa, 7 had pale mucosa and the rest normal (n = 40), blackish debris in 4/40 patients and mucopurulent discharge in 10/40, On examining sinus tenderness, majority of patients had frontal sinus tenderness (15%) followed by maxillary and ethmoid tenderness. Other signs which were recorded included the following – palatal erosion 1/40, proptosis 5/40, chemosis of eye 3/40, periorbital swelling 3/40, decreased vision 2/40, ptosis 3/40 and swelling over medial canthus 1/40.
All patients were subjected to diagnostic nasal endoscopy (DNE) and CT of paranasal sinuses prior to surgery. Based on the CT scan findings, most commonly involved sinuses were maxillary sinus (34/40) and ethmoidal sinus (32/40) (Fig. 2). 40% fungal sinusitis cases showed bilateral involvement of sinuses. 92.3% cases of fungal sinusitis showed metal dense deposits and 63.6% cases showed bone erosion on CT scan. (Fig. 3). 10 cases of fungal sinusitis showed polypoidal changes, 8 cases showed blackish debris and 9 cases showed mucopurulent discharge on DNE.
All patients underwent functional endoscopic sinus surgery. None of the patients had to undergo any facial skeleton resection as part of disease removal. There were no significant post-operative complications like intractable haemorrhage or orbital complications.
38% (40) of the CRS cases were of fungal sinusitis which had a positive fungal culture. However only 29.5% cases of CRS were positive for fungal staining with KOH whereas histopathological examination showed features of fungal sinusitis in 18% of the cases. 80% of the fungal sinusitis cases detected were non invasive in nature.
The most common fungal organism cultured was Aspergillus flavus accounting for 62.5% (25) of fungal sinusitis cases. The other fungi cultured included aspergillus fumigatus, aspergillus niger, mucormycosis, Rhizopus and scopularis. (Fig. 4)
8 cases (20%) of fungal sinusitis cases presented with complications which included 2 cases of orbital apex syndrome and 1 case each of superior orbital fissure syndrome, meningoencephalitis, orbital cellulitis, cavernous sinus thrombosis, Ophthalmoplegia and proptosis.
The patient with superior orbital fissure syndrome was a diabetic and was diagnosed with rhizopus and mucor in the fungal culture. Post surgery, a thorough wash was given to the sinuses followed by treatment with Amphotericin B and strict diabetic control. He was on regular follow up for a duration of 6 months and underwent diagnostic nasal endoscopies on follow up visits during which there was no evidence of recurrence, but his vision continued to be diminished. After 6 months the patient was lost to follow up. Both patients with orbital apex syndrome were uncontrolled diabetics and were diagnosed with aspergillus niger and mucormycosis respectively. The patient with mucormycosis was put on amphotericin B. Both patients have been on regular follow up with no evidence of disease in endoscopy or imaging for the past 1 year. The patient with meningoencaphilitis was diagnosed with aspergillus flavus. After surgery he was put on third generation cephalosporins. Patient recovered fully and was discharged in a stable condition after 14 days and have been on regular follow up with no signs of residual or recurrent disease. The patient who presented with orbital cellulitis had mucor present in fungal culture and was also an uncontrolled diabetic. Prior to FESS he was started on trimethoprim-sulfamethoxazole as treatment of orbital cellulitis. Following FESS he was aggressively treated with amphotericin B. He was on regular follow up with us for 6 months post-surgery. The patient with cavernous sinus thrombosis was diabetic as well as Hepatitis B positive. Mucor was present in the fungal culture. After FESS he was started on systemic amphotericin B. A brief course of anti coagulation was also given to this patient. He was on follow up for a period of 1 year with us. He had no sequalae following this complication and had a good recovery. The patient who presented with Ophthalmoplegia was also an uncontrolled diabetic. He had 3 types of fungi cultured which included rhizopus, mucor and aspergillus fumigatus. After FESS, he was started on systemic amphotericin B and was on follow up for 3 months during which no recurrence of disease was noted although there was only partial recovery of eye movements. Aspergillus flavus was cultured from the patient who presented with proptosis. Following surgery he was on follow up for a duration of 6 months with no signs of residual or recurrence.
The average duration of follow up for patents was 11.1 months (range 3–18 months ) None of the patients had any clinical or endoscopic signs of recurrence or residual disease during the follow up period. There were no significant post-operative complications noted in the immediate or delayed period. 2 patients were identified with intraoperative CSF leak which was repaired and they had an uneventful recovery. All patients were considered to have a good prognosis following the surgery and antifungal treatment, as none of them presented with any residual or recurrent disease nor did they present with any further complications secondary to fungal sinusitis. Although the patients with cavernous sinus thrombosis and Ophthalmoplegia had residual weakness in eye movements.
Discussion
Fungal sinusitis is now an important part of the spectrum of sinonasal diseases with its rising incidence and varied clinical presentation. There has been a spike in the number of fungal sinusitis cases world wide possibly due to weakened immune systems. Increase in the incidence of life style diseases like diabetes and cancer along with treatment with chemoradiotherapy, all are add on risk factors for the development of fungal sinusitis.
The mean age of patients with fungal sinusitis was 41.05 years as per our study which is comparable to several other studies [13, 14]. 52.5% cases belonged to the 5th and 6th decade of life which is similar to the study by Satish et al. [15], however study conducted in 2016 showed a peak incidence of fungal sinusitis cases in 3rd and 4th decade [12]. There was a male preponderance for fungal sinusitis (52%) which is in line with several other studies conducted previously [12, 16, 17].
Our study showed that 60% of the cases of fungal sinusitis were diagnosed in monsoon season in contrast to other studies which demonstrated an increase in the incidence of fungal sinusitis during winters [16]. We can infer from our findings that that humidity may have an important role in the development of fungal sinusitis.
42.5% of fungal sinusitis cases were diabetic in our study which was the most common co morbidity in this group of patients as previously mentioned in other studies [15]. In our fungal sinusitis patients, 1 patient was HIV positive and 3 were Hepatitis B positive (HbsAg+). The HIV patient had oculocerebral mucormycosis. All cases of invasive fungal sinusitis had either uncontrolled diabetes or an immunocompromised status which is comparable to the 63% as observed in the study conducted by Rajiv et al.(13).Both diabetes mellitus and immunocompromised status was found to be significantly associated with fungal sinusitis. The rising trend of fungal sinusitis can be indirectly attributed to the change in lifestyle and food habits of the people thereby predisposing them to development of chronic disease conditions like diabetes mellitus which is closely associated with incidence of fungal sinusitis. The mean RBS value in patients with fungal sinusitis as per our study was 153.68 which is elevated. Elevated RBS values was found to have a strong correlation with fungal sinusitis. The mean Hba1c value in fungal sinusitis case was found to be 9.4 which proves that poor diabetic control is an important predisposing factor for fungal sinusitis.
18 (45%) out of 40 patients with fungal sinusitis were chronic smokers in our study where as in the study conducted by Sathish et al. 24 (54.5%) out of 44 patients with fungal sinusitis were chronic smokers.[98] The higher incidence of fungal sinusitis among smokers can be attributed to impaired mucociliary clearance. However no correlation was found between consumption of alcohol and the incidence of fungal sinusitis.
Fungal sinusitis is a wide spectrum with varied clinical presentation. The most common symptoms in fungal sinusitis as observed in our study included nasal obstruction (72.5%) and headache (57.5%). Other symptoms included nasal discharge, excessive sneezing, nasal bleed, olfactory disturbances, post nasal discharge and facial pain. In the studies conducted by Celso et and Satish et al. the most common symptoms included nasal obstruction, nasal discharge and chronic headache [14, 15].
All patients underwent DNE and CT PNS prior to surgery. Diagnostic nasal endoscopy showed polypoidal changes in 10 patients (25%), blackish debris in 8 patients (20%) and mucopurulent discharge in middle meatus in 9 cases (22.5%) out of the 40 cases of fungal sinusitis. Polypoidal changes were seen in majority of patients with fungal sinusitis in the study conducted by Sandeep et al. and Karthikeyan et al. [12, 18]. However eschar was seen in less than 15% cases in similar studies [12, 18]. 60% cases had unilateral sinus involvement on CT scan which was comparable to 83.3% cases in a similar study [12]. The most commonly involved sinuses were maxillary (85%) and ethmoid (80%), similar findings were observed in a study conducted by Sandeep et al. [12]. Maxillary sinus was most commonly involved in fungal rhinosinusitis probably because the sinus ostium is located lowest in the middle meatus compared with other sinus ostia, which provides easy access to microorganisms. As per our study 30% of fungal rhinosinusitis cases showed metal dense deposits and 17.5% cases showed features of bony erosion whereas there have been studies which have recorded the presence of metal dense deposits in as high as 50% cases [12].
All patients were subjected to FESS and the specimen collected during surgery were subjected to KOH, fungal culture and HPE. Only 30% cases were positive on KOH mount (38% positive on fungal culture) and this can be attributed probably due to drying of the sample and delay in processing. However there were no cases which were positive on KOH but negative on fungal culture. But it is very important that we use a combination of methods to arrive at the final result and not rely on just one method.
The incidence of fungal sinusitis as per our study was 38% which is similar to the findings seen in the study conducted by Granville et al. in 2004 and Das et al. in 2009 which demonstrated an incidence between 12 to 47% [9, 11]. More recent studies show an incidence as high as 48.6% [16]. However there are other studies which have recorded incidence of fungal sinusitis as less than 10% [14, 15].
85% cases in our study had aspergillus as the causative organism with aspergillus flavus being the most common, this was comparable to other studies conducted in the Indian subcontinent on fungal sinusitis [13, 16]. Aspergillus Fumigatus was found to be more common in USA and Aspergillus Flavus was found to be more common in India, this can probably be attributed to the difference in climate and geographic conditions [16].
On HPE, only 18% of the total cases of chronic rhinosinusitis showed features of fungal sinusitis whereas the most common finding was chronic inflammation (52%). Similar studies conducted have shown 6 to 24% presence of fungal invasion on HPE [9, 14]. Therefore histopathological confirmation was obtained in in 47.5% cases of fungal sinusitis in our study. This can be due to multiple factors like insufficient sample, sample collected from areas where the hyphae had not reached the tissues or due to improper fixation of the sample in formalin.
8 cases (20%) of fungal sinusitis were diagnosed to have complications which included 2 cases of orbital apex syndrome and 1 case each of superior orbital fissure syndrome, meningoencephalitis, orbital cellulitis, cavernous sinus thrombosis, Ophthalmoplegia and proptosis.
All cases were treated appropriately with surgical debridement by functional endoscopic sinus surgery followed by oral itraconazole for a duration of 15 days. Mucormycosis cases were started on injection amphotericin B with regular monitoring of electrolytes and liver function tests and nasal douching with amphotericin.
This study has helped us to conclude that contrary to the previous belief that fungal sinusitis is a rare entity, all cases of chronic rhinosinusitis should be evaluated clinically and investigated appropriately with KOH mount, fungal culture and histopathological examination for fungal sinusitis also, not only in immunocompromised individuals but also in immunocompetent persons and treated appropriately with surgical debridement and antifungal therapy. Culture and microscopic examination is the gold standard for diagnosis. Imaging with CT paranasal sinuses help more in planning surgery rather than in giving a diagnosis.
Patients with chronic rhinosinusitis should be diagnosed with a thorough work up and fungal sinusitis should be considered as an important differential while treating a patient. Treating physicians should be very careful while diagnosing such cases and should not blindly treat patients with the usual combo of steroid sprays, antibiotics or antihitaminics especially in immunocompromised patients and in those with other predisposing factors. Such mismanagement of cases can do more harm to the patient than leaving the patient untreated. Therapeutic dilemmas in fungal sinusitis is maily due to delay in diagnosis, rapid disease progression and high cost of anti fungal drugs.
As otorhinolaryngologists, we should be well versed in the diagnostic and treatment modalities of fungal sinusitis and its complications, because, as this case series has clearly shown us, it is not as rare as it seems.
References
International Rhinosinusitis Advisory Board (1997) Infectious rhinosinusitis in adults: classification, etiology and management. Ear Nose Throat J 76:5–22
Mark S, Schubert (2009) ; 47 (Supplement 1) : 324 – 30
Benninger M, Ferguson B, Hadley J et al (2003) Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg 129(Suppl):1–32
Meltzer EO, Hamilos DL, Hadley JA et al (2004) Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol 114(Suppl):155–212
Hamilos DL (2000) Chronic sinusitis. J Allergy Clin Immunol 106:213–227
Hamilos DL (2001) Noninfectious sinusitis. ACI Int 13:27–32
Schubert MS (2006) Allergic fungal sinusitis. Clin Rev Allergy Immunol 30:205–216
Pannathat Soontrapa N, Larbcharoensub T, Luxameechanporn et al (2010) Fungal rhinosinusitis: a retrospective analysis of clinicopathologic features and treatment outcomes at ramathibodi hospital. Southeast asian J trop med public health 42:442–449
Das A, Bal A, Chakrabarti A et al (2009) Spectrum of fungal rhinosinusitis; histopathologist’s perspective. Histopathology 54:854–859
De Shazo RD, Chapin K, Swain R (1997a) Fungal sinusitis. N Engl J Med 337:254–259
Granville L, Chirala M, Cernoch P et al (2004) Fungal sinusitis: histologic spectrum and correlation with culture. Hum Pathol 35:474–481
Sandeep Suresh D, Arumugam G, Zacharias et al (2016) Prevalence and clinical profile of fungal rhinosinusitis. Allergy Rhinol 7:115–120
Rajiv C, Michael, Joy S, Michael1, Ruth H, Ashbee1 et al (2008) Mycological profile of fungal sinusitis: an audit of specimens over a 7-year period in a tertiary care hospital in Tamil Nadu. Indian J Pathol Microbiol 51(4):493–496
Dall’Igna C, Palombini BC, Anselmi F et al (2005) Fungal rhinosinusitis in patients with chronic sinusal disease. Braz J Otorhinolaryngol 71(6):712–720
Dr HS, Satish Dr. Jolene Alokkan, ‘Clinical study of Fungal Rhinosinusitis’,IOSR Journal of Dental and Medical Sciences. ; 5(4) :37–40
Singh AK, Gupta P (2017) Fungal rhinosinusitis: microbiological and histopathological perspective. J Clin Diagn Res 11(7):10–12
Navya N, Vivek T, Sudhir et al (2015) Role of histopathology in the diagnosis of Paranasal Fungal Sinusitis. IOSR J Dent Med Sci 14(1):97–101
Karthikeyan P, Nirmal Coumare V (2010) Incidence and presentation of fungal sinusitis in patient diagnosed with chronic Rhinosinusitis. Indian J Otolaryngol Head Neck Surg 62(4):381–385
Funding
No source of funding for the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study is conducted abiding the ethical standards of the institution.
Conflict of Interest
There is no conflict of interest amongst the authors of the study.
Informed consent
A written and informed consent was taken for the procedure from all the participants of the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Menon, N.N., B, B.M. & S, S. Clinicomycological Profile of Fungal Rhinosinusitis in South India. Indian J Otolaryngol Head Neck Surg 75, 2142–2148 (2023). https://doi.org/10.1007/s12070-023-03826-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-03826-x