Abstract
Introduction
A one-way valve lesion plays an important role in the formation of Baker’s cysts and serves as an important landmark for accessing these cysts during arthroscopic surgery. This study aimed to investigate the incidence of one-way valve lesions and their effect on clinical outcomes in patients who underwent arthroscopic cystectomy for Baker’s cysts.
Materials and methods
Patients who underwent arthroscopic cystectomy for Baker’s cysts between June 2005 and November 2017 were retrospectively reviewed. Patient demographic characteristics, radiologic/arthroscopic findings (presence of one-way valve lesions, concurrent chondral and meniscal lesions, and cyst wall thickness), and clinical outcomes (clinical recurrence rate, Lysholm score, and complications) at the 2-year follow-up were evaluated. Subgroup analysis was performed to compare clinical outcomes between patients with and without one-way valve lesions.
Results
Thirty patients (mean age, 57.4 ± 9.4 years) were included in this study. One-way valve lesions were surgically documented in 11 patients (36.7%). Ten patients (33.3%) had chondral lesions with an International Cartilage Repair Society grade ≥ 3, and 23 patients (76.7%) had concurrent chondral and meniscal lesions. At the 2-year follow-up, none of the patients had experienced clinical recurrence; the mean Lysholm score was 76.3 ± 17.5 (48–100). Three patients reported persistent pain, while two reported numbness or paresthesia. Subgroup analysis showed no significant differences in clinical recurrence rates, Lysholm scores, and complication rates between the groups.
Conclusions
The incidence of one-way valve lesions during arthroscopic cystectomy for Baker’s cysts was lower than that previously reported. Arthroscopic cystectomy showed good clinical results in patients with and without these lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Baker’s cyst is a common pathology in patients with degenerative osteoarthritis of the knee joint. Baker et al. defined it as a distension of the gastrocnemius-semimembranosus bursa due to entrapment of synovial fluid [1]. The treatment of these cysts using the conventional surgical technique of open resection is associated with a high recurrence rate of up to 50% because the intraarticular pathologies responsible for the effusion cannot be treated using open procedures [2,3,4]. With the recent advancements in arthroscopic techniques, arthroscopic cystectomy is commonly performed for treating Baker’s cysts, their orifices, and associated intra-articular pathologies [5,6,7].
Traditionally, a one-way valve lesion is defined as an opening of the Baker’s cyst behind the capsular fold located on the posteromedial side of the medial head of the gastrocnemius; this lesion permits unidirectional flow of knee effusions into the bursa through a valvular opening [3, 8]. This valvular mechanism plays an important role in the formation of Baker’s cysts and serves as an important landmark for accessing the cyst during arthroscopic surgery [7, 9, 10].
Before the development of arthroscopy, the presence of a one-way valve lesion was confirmed by checking whether the contrast in the cyst spread into the joint [11, 12]. Currently, it can be visually checked using arthroscopy [13, 14]. In previous studies, the incidence of one-way valve lesions during arthroscopic treatment for Baker’s cysts was reported to be 71–100% [13,14,15]. However, in our clinical experience, these lesions were not detected as often as previously reported. Although there have been clinical studies that evaluated the symptoms and intra-articular pathology in patients with and without one-way valve lesions [12], few studies have investigated the effect of one-way valve lesions on clinical outcomes after arthroscopic cystectomy.
Therefore, this study aimed to investigate the incidence of one-way valve lesions and their effects on clinical outcomes (clinical recurrence rate, Lysholm score, and complications) in patients who underwent arthroscopic cystectomy for Baker’s cysts. We hypothesized that the incidence of these lesions would be lower than that reported in the available literature and that arthroscopic cystectomy would show good clinical outcomes, regardless of the presence of these lesions.
Methods
Patients
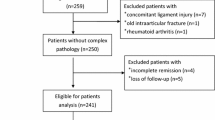
After receiving approval from the review board of our institution, the medical records and radiologic and arthroscopic data of 76 patients who underwent surgical treatment for popliteal cysts between June 2005 and November 2017 were retrospectively reviewed. The indications for arthroscopic treatment of popliteal cysts were (i) symptomatic knee joint pain with the presence of cysts and concurrent intra-articular lesions and (ii) cysts > 5 cm in diameter that did not decrease in size after repeated aspiration [10]. The inclusion criteria for this study were: (i) primary arthroscopic cystectomy, (ii) Baker’s cyst located between the semimembranosus muscle and medial head of the gastrocnemius, as documented by preoperative magnetic resonance imaging (MRI), and (iii) a minimum follow-up duration of 2 years. The exclusion criteria were: (i) popliteal cysts not located between the semimembranosus muscle and medial head of the gastrocnemius on preoperative MRI scans, (ii) revision cystectomy for recurrent Baker’s cysts, (iii) open cystectomy, (iv) insufficient medical/arthroscopic data, and (v) a follow-up period of < 2 years.
Surgical technique and rehabilitation
Arthroscopic cystectomy was performed as previously described [9]. A routine arthroscopic examination of the knee joint was performed using standard anteromedial and anterolateral portals. Any intra-articular pathologies were treated arthroscopically. Meniscal tears were treated with a partial meniscectomy, and chondral lesions were treated with chondroplasty or microfracture, depending on the International Cartilage Repair Society (ICRS) grade [16].
A standard posteromedial portal was created under needle guidance. A probe was passed through this portal to identify the presence of a one-way valve lesion, defined as an opening in the cyst behind the capsular fold located on the posteromedial side of the medial head of the gastrocnemius; this lesion can be identified by displacing the overlying capsular fold (Fig. 1A). If an opening was identified, it was enlarged using a shaver and basket forceps inserted through the posteromedial portal (Fig. 1B). If no opening was identified, the capsular fold and posteromedial capsule behind it were partially resected using basket forceps to create an open connection to the cyst in the area where the opening would normally be located; thereafter, the arthroscope was advanced into the cyst through the opening (Fig. 1C). Excisional debridement of the cystic wall was performed using basket forceps and a shaver inserted through the standard anterolateral or posteromedial portal (Fig. 1D).
Arthroscopic images from the anterolateral portal of the left knee showing the arthroscopic cystectomy procedure. A A one-way valve lesion is identified by displacing the overlying capsular fold. B The capsular fold is partially resected to enlarge the lesion. C The one-way valve lesion is located posteromedial to the medial head of the gastrocnemius. D The cystic wall is debrided by inserting a shaver through the standard posteromedial portal. PM posteromedial, GN gastrocnemius
Occasionally, in cases with a large cyst, complete cystectomy was not possible using standard portals as arthroscopic instruments could not reach the entire cyst wall. In these cases, an accessory cystic portal was created in the skin overlying the medial side of the cyst using the outside-in technique (Fig. 2). A complete arthroscopic cystectomy was then performed by inserting basket forceps and a shaver through the accessory cystic portal. Thin cystic walls were debrided using a shaver, while basket forceps were used to resect thick cystic walls.
To prevent cyst recurrence, strict postoperative rehabilitation protocols were applied for all patients. Knee joint motion and weight-bearing activities were restricted for 2 weeks after the surgery by applying a cylinder splint with a compression pad on the popliteal area. After removal of the splint, the patient was allowed to perform range-of-motion exercises and partial weight-bearing ambulation using crutches. Full weight-bearing was allowed on the affected leg 4 weeks after surgery.
Preoperative radiologic parameters and intraoperative arthroscopic evaluation
Preoperative radiologic parameters and intraoperative arthroscopic findings were evaluated by a senior resident who was blinded to the study design. Preoperative knee radiographs (anteroposterior, lateral, and axial views) were evaluated for preoperative osteoarthritis using the Kellgren–Lawrence grading scale [17, 18]. The size of the cyst was evaluated using preoperative MRI and was measured at its longest dimension in the superior-inferior length of the sagittal plane (Fig. 3).
Arthroscopic pictures, videos, and operation records were reviewed to evaluate operative time and intraoperative arthroscopic findings. Detailed arthroscopic findings, including the presence of a one-way valve lesion and concurrent chondral and meniscal lesions, and cyst wall thickness, were recorded in the operation records of all patients. During arthroscopic cystectomy, the presence of a one-way valve lesion was confirmed if the Baker’s cyst could be accessed through the capsular opening (orifice) located on the posteromedial side of the medial head of the gastrocnemius. Thin cystic walls were defined as cysts that could be debrided with a shaver, while thick cystic walls were defined as cysts that had to be resected using basket forceps.
Measurement of the clinical outcomes
Patients completed a Lysholm questionnaire whenever they visited an outpatient clinic after surgery [19]. Postoperative complications, such as persistent pain, hematoma, infection, numbness, and paresthesia were also evaluated and recorded. Furthermore, an experienced surgeon evaluated each patient for clinical recurrence of Baker's cysts by checking for the presence of cysts in the popliteal area. All medical records and answers to questionnaires were collected by a senior resident, who was blinded to the study design, to evaluate the clinical outcomes of arthroscopic cystectomy, and the results were compared between patients with and without one-way valve lesions.
Data analysis and statistical methods
All statistical analyses were performed using SPSS (version 21.0; SPSS Inc., Chicago, IL, USA). Quantitative variables are presented as means and standard deviations with the respective ranges.
Demographic data, preoperative radiologic parameters, intraoperative arthroscopic findings, and clinical outcomes at the 2-year follow-up were compared between the two subgroups. Chi-square and Fisher’s exact tests were used to compare qualitative variables. Quantitative variables were compared using the independent t-test for normally distributed continuous variables and the Mann–Whitney U test for data with a non-normal distribution. Statistical significance was set at p < 0.05.
Results
Thirty patients (mean age, 57.4 ± 9.4 years) met the inclusion criteria for this study. One-way valve lesions were found during surgery in 11 patients (36.7%). Ten patients (33.3%) had chondral lesions with an ICRS grade ≥ 3, and concurrent chondral and meniscal lesions were found in 23 patients (76.7%). Eleven patients had one-way valve lesions and were classified as group A, while 19 patients who did not have the lesion were classified as group B (Fig. 4). The demographics, preoperative radiologic parameters, and intraoperative arthroscopic findings of the patients are summarized in Table 1.
At the 2-year follow-up, none of the patients had clinical recurrence of Baker’s cyst, and the mean Lysholm score was 76.3 ± 17.5 (48–100). Five patients experienced postoperative complications: three patients experienced persistent pain, and two patients experienced numbness or paresthesia in the medial aspect of the lower leg (Table 2). While the pain subsided within 3 months in all patients, complete resolution of the sensory alterations (numbness or paresthesia) was not achieved during the 2-year follow-up.
In the subgroup analysis, no significant differences were identified in the demographic data, preoperative radiologic parameters, and intraoperative arthroscopic findings between the two groups (Table 3).
There was no clinical recurrence of cysts in either group. The postoperative Lysholm scores at the 2-year follow-up were 80.0 ± 12.5 in group A and 74.2 ± 19.8 in group B; however, the scores were not significantly different between the groups (Table 4). Moreover, no significant differences were identified between the two groups with respect to complication rates (Table 4).
Discussion
The most important finding of this study was that the incidence of one-way valve lesions identified by arthroscopic examination was lower than that reported in the literature. Previous studies have reported that one-way valve lesions were identified in 71–100% of patients. Ko et al. found a posteromedial connecting hole behind the capsular fold in 10/14 cases (71%) [14]. Lie et al. reported that a valvular opening was identified in 10/11 patients (90.9%) [15], and Ji et al. reported that communication between knee joints and popliteal cysts was found in all patients undergoing arthroscopy [13]. However, in the current study, an opening in the cyst behind the posteromedial capsular fold was identified in only 11 of 30 patients (36.7%). The inconsistency in the incidence of one-way valve lesions may be due to differences in the definition of these lesions. In this study, a one-way valve lesion was defined as an opening (orifice) in the cyst behind the capsular fold that acts as a connection to allow the joint fluid to flow into the Baker’s cyst. However, several studies have reported that the one-way valve lesion of Baker’s cysts is simply an opening (orifice) in the cyst or its thin membrane [10, 13].
This study also evaluated differences in patient demographics, associated chondral and meniscal pathologies, and clinical outcomes with regard to the presence of a one-way valve lesion. In the subgroup analysis, no significant differences were identified in demographic data, preoperative radiologic parameters, and arthroscopic findings between the two groups; therefore, this study could not identify any factors that may be associated with the formation of one-way valve lesions. Moreover, no significant differences were found in clinical outcomes in terms of clinical recurrence, postoperative Lysholm scores, and complication rates between patients with and without one-way valve lesions. According to the results of this study, the presence of a one-way valve lesion did not appear to affect the clinical outcomes of arthroscopic cystectomy for Baker’s cysts.
Several studies have compared the clinical outcomes of different surgical methods for treating Baker’s cysts [3, 20, 21]. Yang et al. demonstrated that open cystectomy without arthroscopic treatment of the underlying joint pathology increases recurrence rates [3]. Moreover, recent meta-analyses have shown that compared with simple decompression without cystectomy, arthroscopic cystectomy can yield better clinical results and decrease rates of recurrence, but can result in more complications [22, 23]. Although we evaluated clinically symptomatic recurrence, none of the patients had clinical recurrence, and the Lysholm score was improved in this study. Five patients (16.7%) experienced persistent pain or sensory changes, but recovered completely. Therefore, arthroscopic cystectomy can be considered a safe and effective surgical technique for treating Baker’s cysts. However, attention should be paid to the major neurovascular complications, and it is recommended to perform arthroscopic cystectomy for Baker’s cysts after obtaining proficiency in arthroscopic procedures.
In this study, 23 patients (76.7%) had concurrent meniscal tears and degenerative chondral lesions with an ICRS grade ≥ 2. Previous studies also reported a high prevalence of concurrent chondral and meniscal lesions in patients who underwent arthroscopic treatment for popliteal cysts. Ko et al. reported a high incidence of degenerative cartilage damage (72%) and meniscal tears (medial meniscal tears, 79%; lateral meniscal tears, 21%) [14]. Haifeng et al. also reported that degenerative cartilage damage was the most common pathology and affected 67.6% of patients who underwent arthroscopic treatment for popliteal cysts [5]. Medial and lateral meniscal tears were identified in 32.4% and 20.6% of the cases, respectively. Stefan et al. demonstrated that the prevalence of intra-articular pathologies was significantly higher in patients with popliteal cysts than in those without such cysts [24]. The results of these studies suggest that intra-articular pathologies are associated with the development of Baker’s cysts and should be treated to prevent cyst recurrence.
There seems to be a general consensus on the surgical indications for Baker's cyst. In previous studies, surgical treatment was performed if the cyst was large and had cyst-related symptoms. Ahn et al. performed surgical treatment for (1) patients who reported symptomatic knee joint pain with cysts and a concurrent intra-articular lesion and (2) any cyst > 5 cm that failed to decrease in size after three or more aspirations [10]. Gu et al. performed surgical treatment for symptomatic cysts alone, that did not resolve after conservative treatment for at least 6 months [5]. We also applied these surgical indications to patients with Baker’s cysts in clinical practice.
Previous studies have reported the occurrence of neurovascular injuries after arthroscopic procedures [25,26,27,28]. Venkatesh et al. reported a case of popliteal artery aneurysm after arthroscopic cystectomy of a popliteal cyst [29]. They asserted that a critical review of the preoperative MRI findings is essential and that the cyst wall adjacent to the neurovascular structures should not be shaved during arthroscopic cystectomy. However, neurovascular injury can also occur during resection of the posteromedial capsular fold. If a one-way valve lesion is present, it can act as an anatomic landmark for resecting the capsular fold; however, the risk of neurovascular injury can increase in the absence of this landmark. Therefore, resection of the lateral capsule should be avoided, especially in the absence of a one-way valve lesion, as it can damage the neurovascular structures behind the capsule.
In this study, cyst recurrence was clinically assessed. We could not perform radiologic evaluation for recurrence because none of the patients complained of swelling or tenderness associated with cyst recurrence, and few patients consented to radiologic evaluation. Previously, most studies evaluated cyst recurrence using postoperative MRI or ultrasonography after open or arthroscopic cystectomy [2, 3, 5, 10, 30]. A recent systematic review showed a higher recurrence rate after open cystectomy than after arthroscopic treatment [4]. However, Ahn et al. reported that postoperative MRI performed after arthroscopic cystectomy revealed that approximately 45% of patients had persistent cysts [10]. Although there were no clinical recurrences in our study, the radiological recurrence rates using MRI or ultrasound may be higher.
This study has some limitations. First, the number of patients included in this study was too small to confirm the absence of significant differences in patient demographics, radiologic and arthroscopic findings, and clinical outcomes between patients with and without one-way valve lesions. While we included as many patients as possible to reduce the possibility of a type II error, the resulting sample size was not sufficient to obtain a statistical power > 80%. Second, as this study had a retrospective, nonrandomized design, selection bias may have influenced the results. Third, it is possible that one-way valve lesions were present in some cases but were not found during arthroscopic examination. However, careful examination to identify these lesions was performed by an experienced arthroscopic surgeon; thus, we believe that the possibility of missing a lesion was minimized. Finally, the presence of one-way valve lesions and thickness of the cyst walls were evaluated based on arthroscopic findings; this evaluation is subjective and could be influenced by the proficiency of the surgeons.
Conclusions
The incidence of one-way valve lesions found in arthroscopic cystectomy for Baker’s cysts was lower than that reported in the literature. Arthroscopic cystectomy showed good clinical results in patients with and without one-way valve lesions.
References
Baker WM (1994) On the formation of synovial cysts in the leg in connection with disease of the knee-joint. Clin Orthop Relat Res 299:2–10
Rauschning W, Lindgren PG (1979) Popliteal cysts (Baker’s cysts) in adults: I. Clinical and roentgenological results of operative excision. Acta Orthop Scand 50:583–591
Yang B, Wang F, Lou Y, Li J, Sun L, Gao L, Liu F (2017) A comparison of clinical efficacy between different surgical approaches for popliteal cyst. J Orthop Surg Res 12:1–6
Van Nest DS, Tjoumakaris FP, Smith BJ, Beatty TM, Freedman KB (2020) Popliteal cysts: a systematic review of nonoperative and operative treatment. JBJS Rev 8:e0139
Gu H, Bi Q, Chen J (2019) Arthroscopic treatment of popliteal cyst using a figure-of-four position and double posteromedial portals. Int Orthop 43:1503–1508
Yang J-H, Kwon H-H, Lee JK, Bang SY, Lee H-S (2019) Successful arthroscopic treatment of refractory and complicated popliteal cyst associated with rheumatoid arthritis in combination with osteoarthritis: case series and literature review. Rheumatol Int 39:2177–2183
Brazier BG, Sudekum SA, DeVito PM, Dodds JA (2018) Arthroscopic treatment of popliteal cysts. Arthrosc Tech 7:e1109–e1114
Kim TW, Suh JT, Son SM, Moon TY, Lee IS, Choi KU, Kim JI (2012) Baker’s cyst with intramuscular extension into vastus medialis muscle. Knee Surg Relat Res 24:249–253
Ahn JH, Yoo JC, Lee SH, Lee YS (2007) Arthroscopic cystectomy for popliteal cysts through the posteromedial cystic portal. Arthroscopy 23(559):e551-559
Ahn JH, Lee SH, Yoo JC, Chang MJ, Park YS (2010) Arthroscopic treatment of popliteal cysts: clinical and magnetic resonance imaging results. Arthroscopy 26:1340–1347
Lindgren G, Rauschning W (1979) Clinical and arthrographic studies on the valve mechanism in communicating popliteal cysts. Arch Orthop Trauma Surg 95:245–250
Rauschning W, Lindgren PG (1979) The clinical significance of the valve mechanism in communicating popliteal cysts. Arch Orthop Trauma Surg 95:251–256
Ji J-H, Kim W-Y, Park S-E, Shin E-S, Moon C-Y (2009) Arthroscopic treatment of popliteal cysts using the trans-septal approach. Knee Surg Relat Res 21:158–164
Ko S, Ahn J (2004) Popliteal cystoscopic excisional debridement and removal of capsular fold of valvular mechanism of large recurrent popliteal cyst. Arthroscopy 20:37–44
Lie CW, Ng TP (2011) Arthroscopic treatment of popliteal cyst. Hong Kong Med J 17:180–183
Dwyer T, Martin CR, Kendra R, Sermer C, Chahal J, Ogilvie-Harris D, Whelan D, Murnaghan L, Nauth A, Theodoropoulos J (2017) Reliability and validity of the arthroscopic International Cartilage Repair Society classification system: correlation with histological assessment of depth. Arthroscopy 33:1219–1224
Kohn MD, Sassoon AA, Fernando ND (2016) Classifications in brief: Kellgren–Lawrence classification of osteoarthritis. Clin Orthop Relat Res 474:1886–1893
Abdelaziz H, Balde OM, Citak M, Gehrke T, Magan A, Haasper C (2019) Kellgren–Lawrence scoring system underestimates cartilage damage when indicating TKA: preoperative radiograph versus intraoperative photograph. Arch Orthop Trauma Surg 139:1287–1292
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Ame J Sports Med 10:150–154
Jiang J, Ni L (2017) Arthroscopic internal drainage and cystectomy of popliteal cyst in knee osteoarthritis. J Orthop Surg Res 12:182
Su C, Kuang SD, Zhao X, Li YS, Xiong YL, Gao SG (2020) Clinical outcome of arthroscopic internal drainage of popliteal cysts with or without cyst wall resection. BMC Musculoskelet Disord 21:440
Li H, Zhang M, Li Y, Wang H (2021) Comparison of clinical outcomes associated with arthroscopic cyst wall preservation or resection in the treatment of popliteal cyst: a systematic review and meta-analysis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03812-4
Han JH, Bae JH, Nha KW, Shin YS, Lee DH, Sung HJ, Kim JG (2019) Arthroscopic treatment of popliteal cysts with and without cystectomy: a systematic review and meta-analysis. Knee Surg Relat Res 31:103–112
Rupp S, Seil R, Jochum P, Kohn D (2002) Popliteal cysts in adults: prevalence, associated intraarticular lesions, and results after arthroscopic treatment. Ame J Sports Med 30:112–115
Alserr AH, Antonopoulos CN, Papapetrou A, Kakisis JD, Brountzos E, Liapis CD (2014) Endovascular repair of popliteal artery pseudoaneurysm with arteriovenous fistula after knee arthroscopy: case report and literature review. Vasc Endovasc Surg 48:166–170
Lee GC, Kim DH, Park S-H (2014) Popliteal artery pseudoaneurysm after anterior cruciate ligament re-revision using a rigidfix cross pin. Knee Surg Relat Res 26:121–124
Lee KB, Song SY, Kwon DJ, Shin J, Paik SH (2009) Pseudoaneurysm of the medial superior genicular artery after arthroscopic partial meniscectomy. Clin Orthop Surg 1:173–175
Tsubosaka M, Matsushita T, Kuroda R, Matsumoto T, Kurosaka M (2017) Pseudoaneurysm of the articular branch of the descending genicular artery following double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 25:2721–2724
Kp V, Yoon J-R, Nha KW, Yang J-H, Lee J-H, Jegal H (2009) Popliteal artery pseudoaneurysm after arthroscopic cystectomy of a popliteal cyst. Arthroscopy 25:1054–1057
Chen Y, Lee P-Y, Ku M-C, Wu N-Y, Lo C-S (2019) Extra-articular endoscopic excision of symptomatic popliteal cyst with failed initial conservative treatment: a novel technique. Orthop Traumatol Surg Res 105:125–128
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Institutional review board approval was obtained by the ethics committee of Inje University Ilsan Paik Hospital (IRB number: 2019-08-014).
Informed consent
Acquisition of informed consent was not applicable in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nha, K.W., Kim, S.J., Park, J.H. et al. Arthroscopic cystectomy for Baker’s cysts with and without one-way valve lesions: incidence of one-way valve lesion, associated pathologies, and clinical outcomes. Arch Orthop Trauma Surg 143, 287–294 (2023). https://doi.org/10.1007/s00402-021-04076-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04076-8