Abstract
Objective
Arthroscopy is commonly used to treat popliteal cysts, but the influence of the cyst wall on treatment outcomes remains controversial. The goal of this study was to compare clinical outcomes associated with arthroscopic cyst wall resection versus preservation in patients undergoing treatment for popliteal cysts.
Methods
We searched the PubMed, Embase, Web of Science, and Cochrane Library databases to identify all relevant articles published as of April 2020. STATA v15.1 was used for all statistical analyses. Relative risk (RR) and corresponding 95% confidence intervals (CIs) pertaining to study outcomes were calculated. Study heterogeneity was evaluated using the I2 statistic and the χ2 test, with I2 > 50% and P < 0.10 as respective significance threshold values. The risk of bias was gauged with the Cochrane Collaboration’s risk of bias tool and the Newcastle–Ottawa Scale (NOS).
Results
In total, 18 relevant studies were included in this meta-analysis, of which 16 were observational studies and 2 were randomized controlled trials (RCTs). These studies included 573 total patients, of whom 346 underwent arthroscopic cyst resection and 227 underwent arthroscopic cyst preservation. Pooled analyses revealed that clinical outcomes (RR = 0.98, 95% CI 0.94–1.00) and postoperative recurrence rates (RR = 0.90, 95% CI 0.85–0.95) were significantly better among patients that underwent cyst wall resection relative to those that underwent cyst wall preservation (RR = 0, 95% CI 0–0.02 and RR = 0.05, 95% CI 0.02–0.10, respectively). However, complications occurred more often in the cyst wall resection group relative to the cyst wall preservation group (RR = 0.05, 95% CI 0.01–0.12 vs. RR = 0.01, 95% CI 0–0.03). Sensitivity analyses confirmed the stability of these pooled results, and we detected no significant risk of publication bias.
Conclusions
Relative to cyst wall preservation, popliteal cyst wall arthroscopic resection can yield more satisfactory clinical results and decrease rates of recurrence, but can also increase the incidence of complications. Future prospective studies comparing the outcomes associated with cyst wall resection and preservation will be required to validate our results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Popliteal cysts, also referred to as Baker’s cysts, are synovial cysts that manifest in the popliteal fossa. Clinically, these lesions are common and are associated with the gastrocnemio-semimembranosus bursa (GSB) expansion in the posteromedial region of the knee [1]. These cysts were first described by Baker et al. [2] in 1877, and are associated with bursal retention of synovial fluid that is generally accompanied by internal diseases of the knee. Additional pathological analyses have found that the pathogenesis of popliteal cysts is closely associated with intra-articular pathology and with universal flow valve mechanisms in this tissue site [3,4,5].
Traditional posterior open surgery treatment of popliteal cysts is associated with high rates of recurrence, as this approach is unable to simultaneously treat primary intra-articular lesions [3, 6, 7]. An arthroscopic approach was first successfully employed to treat popliteal cysts in 199 by Sansone et al. [8], and further improved versions of this procedure have since been proposed [9,10,11]. Arthroscopy is generally favored for the treatment of popliteal cysts, as it causes minimal trauma, allows for rapid patient recovery, and can treat the cyst directly while also addressing intra-articular lesions.
Despite the promise of this approach; however, whether the inner cyst wall should be removed during surgical treatment and whether it can impact postoperative popliteal cyst recurrence remains controversial. No studies to date have directly compared recurrence rates associated with cyst wall resection relative to cyst wall preservation. Han et al. [12] conducted a systematic review and meta-analysis on this topic in 2019, but their study only included articles published through August 2016. At the same time, they acknowledged that the literature included in their study was solely derived from low-quality retrospective case series, potentially skewing their results. As many pertinent new studies [13,14,15,16,17,18,19], including randomized controlled trials [20, 21], have since been published, it is necessary to revisit and re-evaluate their conclusions. By incorporating a larger sample size and more high-quality research, the present systematic review and meta-analysis was therefore designed to compare clinical improvement, complications, and recurrence rates between arthroscopic cyst wall resection and cyst wall preservation in patients undergoing treatment for popliteal cysts.
Methods
As this was a study of previously published studies, no ethical oversight or patient consent was required.
Study design and search strategy
This meta-analysis was conducted in a manner consistent with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. We systematically searched the PubMed, Embase, Cochrane Library, and Web of Science databases for all relevant studies published as of April 2020 using the following search terms: “popliteal cyst” and “arthroscopy”. The search strategy consisted of combining these terms with “AND” or “OR”. No language restrictions were imposed during the search process. References of eligible studies and pertinent reviews were also assessed in order to identify other studies potentially eligible for inclusion in this analysis.
Study selection
Studies identified via the above search strategy were eligible for inclusion in this analysis if they: (1) were studies of the arthroscopic treatment of popliteal cysts; (2) did not study patients with other diseases likely to impact arthroscopic efficacy; and (3) reported postoperative Rauschning and Lindgren grades, recurrence rates, and incidence of complications at a minimum. Studies were excluded from this meta-analysis if they: (1) were duplicate articles; (2) were reviews, meta-analyses, or case reports; or (3) did not provide data corresponding to the appropriate outcome indicators in a form that could be extracted.
Data extraction
Two investigators independently extracted all relevant data from included studies and compiled this data in a pre-constructed Excel spreadsheet. Collected data included first author, publication year, country, sex, sample size, mean patient age, mean patient follow-up period, pre- and post-operative Rauschning and Lindgren grades (≥ grade 2 was considered to indicate unsuccessful clinical remission), recurrence rate, and complication incidence. Any inconsistencies were resolved through consensus and discussion with a third author. When the data were not available, efforts were made to contact corresponding authors of the appropriate studies to obtain these missing items.
Study quality assessment
For the two RCTs included in this study, the two authors independently assessed methodological quality using the Cochrane Collaboration’s “Risk of Bias” tool, which assesses studies based on criteria including blinding of participants, personnel, and outcome assessors, randomization (allocation concealment and sequence generation), selection of outcomes reported, and data completeness. Based on the tense scores, the risk of bias was determined to be low, high, or unclear [22]. For observational studies, the 9-point Newcastle–Ottawa Scale (NOS) was used to assess study quality, with higher scores corresponding to a lower risk of bias [23, 24]. NOS scores of ≤ 5 correspond to a high bias risk.
Statistical analysis
STATA v15.1 (Statacorp LLC, College Station, TX, USA) was used for all statistical analyses. Pooled analyses of dichotomous variables were conducted by calculating the relative risk (RR) and 95% confidence interval (CIs). Cochran's Q statistics and the I2 statistic were used to gauge heterogeneity among included studies, with respective thresholds of I2 ≤ 25%, 25–75%, and ≥ 75% corresponding to low, medium, and high heterogeneity [25]. For sensitivity analyses, individual studies were sequentially omitted from pooled analyses in order to assess the impact on the overall results. Funnel plots, Egger’s test, and Begg’s test were employed to assess the risk of publication bias [26,27,28]. P < 0.05 was the significance threshold for this study. Forest plots were used to express study outcomes.
Results
Study identification and inclusion
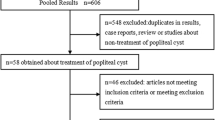
We began by searching the PubMed, Embase, Web of Science, and Cochrane Library databases, leading us to identify 181 potentially relevant articles. Following the removal of duplicate articles, 118 articles remained, of which 71, 12, and 5 were excluded following abstract review as they were irrelevant, case reports, and reviews, respectively. We then subjected the remaining 30 articles to full-text review. Of these, 10 were excluded due to the lack of consistent data and two were excluded due to the lack of available data. The remaining 18 studies were included in the present meta-analysis, including 16 observational studies and 2 RCTs. The study selection process for this meta-analysis is outlined in Fig. 1.
Study characteristics
In total, we evaluated 18 studies for the present meta-analysis, [8, 10, 11, 29,30,31,32,33,34] including 2 RCTs and 16 retrospective studies. These studies were conducted between 1999 and 2020 in six countries (Japan, Korea, China, India, Italy, and Poland), and involved 573 patients (346 that underwent arthroscopic cyst resection, and 227 that underwent arthroscopic cyst preservation). Patients were 42.6–62.6 years old, and average follow-up durations were between 12.5 and 36.1 months. Study clinical outcomes were primarily assessed based on Rauschning and Lindgren grades, recurrence rates, and complication rates. For full details regarding the included studies, see Table 1.
Assessment of study quality
The results of methodological quality assessments for the included studies are compiled in Fig. 2 and Table 2. Of the included RCTs, the study conducted by Yang et al. clearly described the random sequence generation by complete block design, but failed to discuss blinding and allocation concealment. For the study conducted by Shi et al., groups were randomly assigned, but the investigators failed to follow double-blind group assignments, and group allocation was not mentioned. The Newcastle–Ottawa Scale was used to assess observational studies according to participant selection criteria, comparability, exposure, and outcomes in order to gauge the risk of bias. All 16 studies scored between 6 and 8 points, consistent with a low risk of bias.
Risk of bias summary. A risk of bias tool incorporated the assessment of factors including randomization (sequence generation and allocation concealment), blinding (participants and outcome assessors), incomplete outcome data, selective outcome reporting, and other risk of bias. For each of these items, studies were considered to be of low, unclear, or high risk (green, yellow, and red, respectively)
Clinical outcomes
Postoperative Rauschning and Lindgren grades were reported in all studies, with grades of 0 and I being considered to indicate successfully improved clinical outcomes, and grades II and II being indicative of unsuccessful clinical outcomes. Summary results (Fig. 3) revealed an improved success rate in both the cyst wall resection group (RR = 0.98, 95% CI 0.94–1.00, P < 0.05; I2 = 59.57%, P = 0.01) and the cyst wall preservation group (RR = 0.90, 95 CI 0.85–0.95, P < 0.05; I2 = 26.58% P = 0.22). For all included studies (cyst wall resection and preservation group together) results, I2 = 64.24%, z = 33.29, P < 0.05. Sensitivity analyses did not indicate that any individual studies had an impact on the overall findings. In addition, no evidence of publication bias was detected as evidenced by a symmetrical funnel plot (Fig. 4), a Begg’s test P = 0.674, and an Egger’s test P = 0.322.
Cyst recurrence rate
Postoperative cyst recurrence rates were described in all studies. Overall, the postoperative cyst recurrence rate was 1.2% (4 out of 346) in the cyst wall resection group and 7.5% (17 out of 227) in the cyst wall preservation group. Summary results (Fig. 5) were prepared for the cyst wall resection group (RR = 0, 95% CI 0–0.02, P = 0.72; I2 = 29.39%, P = 0.17) and the cyst wall preservation group (RR = 0.05, 95% CI 0.02–0.10, P < 0.05; I2 = 37.83%, P = 0.13). For all included studies (cyst wall resection and preservation group together), I2 = 55.94%, Z = 2.58, P < 0.05. Sensitivity analyses did not indicate that any individual studies had an impact on the overall findings. In addition, no evidence of publication bias was detected as evidenced by a symmetrical funnel plot (Fig. 6), a Begg’s test P = 0.059, and an Egger’s test P = 0.31.
Complication rate
In total, 16 of the included studies reported on the incidence of postoperative complications. Overall, 6.9% (22 out of 318) of the cyst wall resection group and 1.1% (2 out of 183) of the cyst wall preservation group experienced postoperative complications. Summary results (Fig. 7) were generated for the cyst wall resection group (RR = 0.05, 95% CI 0.01–0.12, P = 0.72; I2 = 69.23%, P = 0.00) and the cyst wall preservation group (RR = 0.01, 95% CI 0–0.03, P = 0.85; I2 = 0%, P = 0.85). For all included studies (cyst wall resection and preservation group together), I2 = 59.63%, Z = 2.96, and P < 0.05. Sensitivity analyses did not indicate that any individual studies had an impact on the overall findings. In addition, no evidence of publication bias was detected as evidenced by a symmetrical funnel plot (Fig. 8), a Begg’s test P = 0.095, and an Egger’s test P = 0.359.
Discussion
Several treatment approaches for popliteal cysts have been described to date. Although the pathogenesis of these cysts remains incompletely understood, anatomical and pathological evidence suggest that they should not be treated as local tumors. Popliteal cysts are frequently accompanied by intra-articular lesions that can manifest as degenerative surface cartilage changes and tearing of the medial meniscus [4, 35,36,37]. These lesions can serve as a primary source of synovial fluid; thus, supporting the development and persistence of popliteal cysts. The formation of these cysts is also facilitated by valve mechanisms governing unidirectional synovial fluid flow [38]. These mechanical factors together with intra-articular disorder; thus, drive popliteal cyst development.
Traditional posterior resection of popliteal cysts does not allow for the simultaneous treatment of primary intra-articular lesions, resulting in high rates of postoperative cyst recurrence [39]. In contrast, arthroscopy allows for the correction of these intra-articular lesions while also allowing for enlargement of the valve communication port so as to restore two-way communication between the bursa and the joint cavity via a minimally invasive approach, thereby eliminating the drivers of popliteal cysts. As arthroscopic technology has advanced, however, whether the cyst wall should be removed or preserved has been a matter of significant scholarly debate. Kongmalai et al. [40] determined that the wall of a popliteal cyst is composed of thickened hyaloid tissue and lacks synovial fluid-producing synovial cells, leading them to speculate that this wall primarily functions as a barrier that permits cyst fluid storage, and thus does not require resection. This view has been reported by multiple other studies. For example, Billières et al. [41] determined that the inner cyst wall is not the source of synovial fluid, while Sansone and De Ponti [8] solely corrected the valve mechanism and intraarticular pathology via an arthroscopic approach without excising the capsule wall and achieved a success rate of 95%. Ohishi et al. [32] also reported a 93.1% clinical improvement rate when patients underwent arthroscopic expansion of unidirectional valvular slits via two posterior portals. Ahn et al. [11], in contrast, conducted cyst wall resection via adding an additional cystic portal in 24 patients with a fibrous structure in treated cysts, and found that all cysts shrank or disappeared over a 36.1-month follow-up period. Recently, Gu et al. [17] employed a dual-posteromedial port approach in combination with four-figure posture to completely dissect the capsule wall, achieving satisfactory outcomes in all 31 treated patients. Herein, we attempted to provide a rigorous overview of the relative advantages of these two surgical treatment strategies. However, we were unable to identify any strictly controlled studies comparing these two approaches in the course of our literature review. As such, we instead conducted a systematic evaluation and used corresponding statistical methods to better understand the outcomes associated with these two surgical strategies.
Our study serves as a valuable update of previous studies, incorporating many recent high-quality studies and thereby improving our overall statistical power to resolve meaningful differences between these two surgical approaches. Our key finding was that removal of the popliteal cyst wall is associated with better clinical efficacy and lower rates of recurrence (1.2% in the cyst wall resection vs 7.5% in the cyst wall preservation). This effect may be due to the role of the cyst wall in the incidence of symptoms and cyst recurrence, but the exact mechanistic basis for this finding remains unknown. These results are not completely consistent with the previous meta-analysis results generated by Han et al., although in their study they concluded that arthroscopic cystotomy after management of intra-articular pathological changes was associated with a low-risk rate, they did not observe any clear advantages in the cystostomy group relative to the non-cystotomy groups. In addition, we also found that cyst wall removal was associated with higher rates of complications (6.9%) than cyst wall preservation (1.1%). We thus recommend that arthroscopic operations be conducted carefully when shaving away the inner wall of the cyst. The neurovascular bundle of the popliteal fossa, which is located in the septum or slightly lateral portion of the popliteal fossa, is the main neurovascular structure at risk during this operation. For larger cysts extending to the posterolateral side of the knee joint, rates of associated vascular and nerve injury are elevated. Cho [29] found that arthroscopic cyst resection is associated with a 4.5% complication rate, with hematoma being the most common such complication. In a study published in 2009, Kp et al. [42] found that at two months post-arthroscopic cyst wall resection, one patient developed a pseudoaneurysm of the popliteal artery. As such, these authors recommended against the planning of the lateral wall of the cyst to avoid injuring the popliteal artery.
There are multiple limitations to this meta-analysis. For one, while we have sought to incorporate all relevant studies in our systematic review, the majority of the included studies are from China. This may be a consequence of regional differences in morbidity, but also has the potential to influence our findings as a consequence of such regional and ethnic variability. We attempted to overcome such variation through subgroup analyses, but our sample sizes were too limited to facilitate such an approach. In addition, some of the included studies failed to report certain relevant results. Although we attempted to contact the corresponding authors of these studies to obtain the missing data, we did not receive any responses. As such, these omitted data may inadvertently bias our findings. Furthermore, most included studies were retrospective analyses rather than RCTs, introducing a high risk of selection bias. Future large-scale multi-center RCTs of high quality will thus be essential to validate and expand upon our present findings.
Conclusion
In summary, relative to cyst wall preservation, arthroscopic cyst wall resection can yield more satisfactory clinical outcomes and lower recurrence rates, but is associated with higher rates of complications.
References
Adams R (1840) Chronic rheumatic arthritis of the knee joint. Dublin J Med Sci 17:520–522
Baker WM (1994) On the formation of synovial cysts in the leg in connection with disease of the knee-joint. 1877. Clin Orthop Relat Res 299:2–10
Childress HM (1970) Popliteal cysts associated with undiagnosed posterior lesions of the medial meniscus. The significance of age in diagnosis and treatment. J Bone Jt Surg Am 52(7):1487–1492
Rupp S, Seil R, Jochum P, Kohn D (2002) Popliteal cysts in adults. Prevalence, associated intraarticular lesions, and results after arthroscopic treatment. Am J Sports Med 30(1):112–115. https://doi.org/10.1177/03635465020300010401
Lindgren PG, Willén R (1977) Gastrocnemio-semimembranosus bursa and its relation to the knee joint. I. Anatomy and histology. Acta Radiol Diagn (Stockh) 18(5):497–512. https://doi.org/10.1177/028418517701800501
Dinham JM (1975) Popliteal cysts in children. The case against surgery. J Bone Jt Surg Br 57(1):69–71
Rauschning W, Lindgren PG (1979) The clinical significance of the valve mechanism in communicating popliteal cysts. Arch Orthop Trauma Surg 95(4):251–256. https://doi.org/10.1007/BF00389694
Sansone V, De Ponti A (1999) Arthroscopic treatment of popliteal cyst and associated intra-articular knee disorders in adults. Arthroscopy 15(4):368–372. https://doi.org/10.1016/s0749-8063(99)70053-8
Jiang J, Ni L (2017) Arthroscopic internal drainage and cystectomy of popliteal cyst in knee osteoarthritis. J Orthop Surg Res 12(1):182. https://doi.org/10.1186/s13018-017-0670-4
Calvisi V, Lupparelli S, Giuliani P (2007) Arthroscopic all-inside suture of symptomatic Baker’s cysts: a technical option for surgical treatment in adults. Knee Surg Sports Traumatol Arthrosc 15(12):1452–1460. https://doi.org/10.1007/s00167-007-0383-z
Ahn JH, Lee SH, Yoo JC, Chang MJ, Park YS (2010) Arthroscopic treatment of popliteal cysts: clinical and magnetic resonance imaging results. Arthroscopy 26(10):1340–1347. https://doi.org/10.1016/j.arthro.2010.02.012
Han JH, Bae JH, Nha KW et al (2019) Arthroscopic treatment of popliteal cysts with and without cystectomy: a systematic review and meta-analysis. Knee Surg Relat Res 31(2):103–112. https://doi.org/10.5792/ksrr.18.068
Xinxian X, Yuezheng H, Jian L, Huachen Y (2018) Clinical outcome of arthroscopic management of popliteal cysts with or without additional posterior open cystectomy. Klinisches Outcome der arthroskopischen Behandlung poplitealer Zysten mit und ohne zusätzlicher posteriorer offener Zystektomie. Orthopade 47(6):530–535. https://doi.org/10.1007/s00132-018-3573-0
Malinowski K, Synder M, Sibiński M (2011) Selected cases of arthroscopic treatment of popliteal cyst with associated intra-articular knee disorders primary report. Ortop Traumatol Rehabil 13(6):573–582. https://doi.org/10.5604/15093492.971042
Guo D, Cheng L, Chen G, Yu X, Zhang H, She Y (2020) A comparison of the clinical effects of arthroscopic treatment for popliteal cyst between techniques using one posteromedial portal and two posteromedial portals. Medicine (Baltimore) 99(20):e20020. https://doi.org/10.1097/MD.0000000000020020
Chen Y, Lee PY, Ku MC, Wu NY, Lo CS (2019) Extra-articular endoscopic excision of symptomatic popliteal cyst with failed initial conservative treatment: a novel technique. Orthop Traumatol Surg Res 105(1):125–128. https://doi.org/10.1016/j.otsr.2018.09.022
Gu H, Bi Q, Chen J (2019) Arthroscopic treatment of popliteal cyst using a figure-of-four position and double posteromedial portals. Int Orthop 43(6):1503–1508. https://doi.org/10.1007/s00264-018-4087-4
Wu LC, Zhou HB, Zhang C et al (2017) Therapeutic effects of internal drainage by expanding arthroscopic gastrocnemius-semimembranosus bursa and cyst wall resection for the treatment of 41 patients with popliteal cysts. Zhongguo Gu Shang 30(4):304–308. https://doi.org/10.3969/j.issn.1003-0034.2017.04.004
Pankaj A, Chahar D, Pathrot D (2016) Arthroscopic management of popliteal cysts. Indian J Orthop 50(2):154–158. https://doi.org/10.4103/0019-5413.177568
Shi Z, Ni J, Fan L et al (2018) Clinical prospective comparative study on short-term effectiveness of arthroscopic treatment of popliteal cyst between cyctectomy and internal drainage combined with cyctectomy. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 32(10):1326–1331. https://doi.org/10.7507/1002-1892.201804113
Yang B, Wang F, Lou Y et al (2017) A comparison of clinical efficacy between different surgical approaches for popliteal cyst. J Orthop Surg Res 12(1):158. https://doi.org/10.1186/s13018-017-0659-z
Kim SH, Ha CW, Park YB et al (2019) Intra-articular injection of mesenchymal stem cells for clinical outcomes and cartilage repair in osteoarthritis of the knee: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 139(7):971–980. https://doi.org/10.1007/s00402-019-03140-8
Wells G, Shea B, O’Connell D et al (2015) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in metaanalyses. Ottawa Hospital Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 9 Mar 2015
Wu L, Li M, Zeng Y et al (2020) Prevalence and risk factors for prolonged opioid use after total joint arthroplasty: a systematic review, meta-analysis, and meta-regression. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03486-4
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Gatz M, Driessen A, Eschweiler J et al (2020) Open versus minimally-invasive surgery for Achilles tendon rupture: a meta-analysis study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03437-z
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
Cho JH (2012) Clinical results of direct arthroscopic excision of popliteal cyst using a posteromedial portal. Knee Surg Relat Res 24(4):235–240. https://doi.org/10.5792/ksrr.2012.24.4.235
Lie CW, Ng TP (2011) Arthroscopic treatment of popliteal cyst. Hong Kong Med J 17(3):180–183
Ko S, Ahn J (2004) Popliteal cystoscopic excisional debridement and removal of capsular fold of valvular mechanism of large recurrent popliteal cyst. Arthroscopy 20(1):37–44. https://doi.org/10.1016/j.arthro.2003.10.017
Ohishi T, Takahashi M, Suzuki D et al (2015) Treatment of popliteal cysts via arthroscopic enlargement of unidirectional valvular slits. Mod Rheumatol 25(5):772–778. https://doi.org/10.3109/14397595.2015.1008779
Wang L, Xia BJ, Ruan WM et al (2014) Extracapsular arthroscopic excision of popliteal cysts through anterior combined with posterior approach. Zhongguo Gu Shang 27(8):635–637
Ji JH, Kim WY, Park SE, Shin ES, Moon CY (2009) Arthroscopic treatment of popliteal cysts using the trans-septal approach. J Korean Knee Soc 21:158–164
Stone KR, Stoller D, De Carli A, Day R, Richnak J (1996) The frequency of Baker’s cysts associated with meniscal tears. Am J Sports Med 24(5):670–671. https://doi.org/10.1177/036354659602400518
Johnson LL, van Dyk GE, Johnson CA, Bays BM, Gully SM (1997) The popliteal bursa (Baker’s cyst): an arthroscopic perspective and the epidemiology. Arthroscopy 13(1):66–72. https://doi.org/10.1016/s0749-8063(97)90211-5
Artul S, Jabaly-Habib H, Artoul F, Habib G (2015) The association between Baker’s cyst and medial meniscal tear in patients with symptomatic knee using ultrasonography. Clin Imaging 39(4):659–661. https://doi.org/10.1016/j.clinimag.2015.03.003
Calvisi V, Zoccali C (2016) Arthroscopic patterns of the poster-medial aspect of the knee joint: classification of the gastrocnemius-semimembranosus gateway and its relationship with Baker’s cyst. Muscles Ligaments Tendons J 6(4):492–498. https://doi.org/10.11138/mltj/2016.6.4.492
Ravlić-Gulan J, Gulan G, Novak S, Sestan B (2009) Rapid recurrence of a giant popliteal cyst in a patient with rheumatoid arthritis. J Clin Rheumatol 15(6):300–302. https://doi.org/10.1097/RHU.0b013e3181b5c653
Kongmalai P, Chernchujit B (2015) Arthroscopic treatment of popliteal cyst: a direct posterior portal by inside-out technique for intracystic debridement. Arthrosc Tech 4(2):e143–e148. https://doi.org/10.1016/j.eats.2014.12.002
Billières J, Lascombes P, Peter R (2014) Popliteal cysts: etiologic and therapeutic approach. Rev Med Suisse 10(432):1211–1215
Kp V, Yoon JR, Nha KW, Yang JH, Lee JH, Jegal H (2009) Popliteal artery pseudoaneurysm after arthroscopic cystectomy of a popliteal cyst. Arthroscopy 25(9):1054–1057. https://doi.org/10.1016/j.arthro.2009.05.005
Acknowledgements
The authors would like to thank all the reviewers who participated in the review and MJEditor (http://www.mjeditor.com) for its linguistic assistance during the preparation of this manuscript.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
HL and YKL have made substantial contributions to conception and design of the study, written the manuscript; HL and HHW earched literature, extracted data from the collected literature and analyzed the data; MZ revised the manuscript; All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, H., Zhang, M., Li, Y. et al. Comparison of clinical outcomes associated with arthroscopic cyst wall preservation or resection in the treatment of popliteal cyst: a systematic review and meta-analysis. Arch Orthop Trauma Surg 141, 1741–1752 (2021). https://doi.org/10.1007/s00402-021-03812-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03812-4