Abstract
Introduction
The Kellgren–Lawrence score helps the orthopedic surgeon to classify the severity of knee osteoarthritis (OA) before total knee arthroplasty (TKA). There might be a discrepancy between subjective complaints of the patients and radiologically visible changes of the knee joint in many cases. In this context, we performed a prospective clinical study to compare the preoperative degree of knee OA using the Kellgren–Lawrence score with the intraoperative extent of cartilage damage during primary TKA.
Materials and methods
A total of 251 primary TKA surgeries due to a primary knee OA were prospectively included. Preoperative Kellgren–Lawrence score was determined using standardized preoperative plain radiographs of three views; anteroposterior, lateral and skyline of the patella by a senior radiologist. Intraoperatively, in all cases, photographs of the medial, lateral, and patellofemoral joint compartments were taken. Using the International Cartilage Repair Society (ICRS) score, the degree of chondromalacia was assessed. Subsequently, correlation analysis was performed using the Pearson–Clopper 95% confidence interval (CI).
Results
There were higher intraoperative scores compared to the preoperative scores in 160 of all cases (63.7% of 251, 95% CI 57.5–69.7%). A mismatch of two score grade points was found in 8.4% (95% CI 5.3–12.5%). The most common mismatch was noted in patients with preoperative Kellgren–Lawrence score of 3 and an intraoperative score of 4 in 48.2% (95% CI 41.9–54.6%).
Conclusions
The preoperative radiographs using Kellgren–Lawrence underestimate the severity of knee osteoarthritis. The true extent of articular cartilage damage can be better appreciated intraoperatively. In patients undergoing primary TKA, the correlation of clinical symptoms with radiological findings is crucial in deciding when to perform the surgery. Besides, other imaging modalities may be used as an adjunct when the clinical findings and plain radiographs do not correlate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last decades, various diagnostic methods have been developed to evaluate the severity of osteoarthritis (OA). Despite the development of modern imaging techniques, conventional radiographs remain the most available tool to assess OA. Plain radiographs of the knee joint (anteroposterior, lateral, and skyline view of the patella) can be used to diagnose or monitor the progression of OA [1, 2].
The most common internationally used score was introduced in 1957 by Kellgren and Lawrence [3]. The Kellgren–Lawrence score helps to classify the severity of OA using anteroposterior view plain radiograph of the knee, which can be helpful before total knee arthroplasty (TKA) [3]. However, the discrepancy between clinical and radiographic knee OA has been already reported; therefore, the results of knee X-rays should not be used in isolation when evaluating individual patients with knee pain [4]. Despite the lack of correlation, national guidelines still recommend weight-bearing plain X-rays. Further imaging should not be necessary if clinical and X-ray findings are agreeable.
The Kellgren–Lawrence scoring system has its limitations, as it assumes a linear radiographic progression of OA and is unable to judge the joint space narrowing (JSN) without osteophyte formation [5, 6]. Furthermore, the grading system deals with the knee joint as a whole, not considering each joint compartment separately.
In this context, we performed a prospective study to compare the preoperative degree of knee OA on plain radiographs as assessed using the Kellgren–Lawrence scoring system and compared to the intraoperative findings using ICRS to determine the extent of articular cartilage damage. The results of this study might shed light on whether a TKA can be indicated in patients suffering from severe persistent symptoms, but only found to have mild to moderate OA of the knee on plain radiographs.
Materials and methods
This prospective study was performed after obtaining approval of our institutional review board and the Hamburg Medical Chamber Ethics Committee. The study was carried out in accordance with the World Medical Association Declaration of Helsinki. All subjects gave informed consent to participate in the present study.
Patient selection
A total of 251 patients, who underwent primary TKA in the author’s institution from November 2016 to March 2017 due to symptomatic OA of the knee joint after failed non-operative measures following giving consent for the study, were consecutively recruited. After taking a full history and clinical examination, the indication of TKA was made during the outpatient clinic by fully board-certified arthroplasty orthopedic surgeons. Following the presentation of the possible conservative and operative treatment options, the decision for TKA was then indicated. Patients were then scheduled for the planned surgery. To achieve optimal comparability, only patients with primary OA were included in our study protocol. Secondary OA, e.g., due to trauma, rheumatic disease, or with aseptic bone necrosis, were excluded based on clinical history.
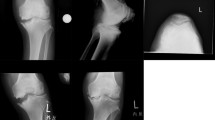
Preoperative evaluation
All patients were admitted one day prior to the planned TKA to the author’s institution. After clinical examination, standard conventional radiographs of all affected knee joints in a standing position (anteroposterior and lateral) were performed. Furthermore, standard skyline views of the patella were taken in all patients. Prior to TKA, the author’s clinic performed in all patients standing long leg radiographs to determine the leg alignment.
Determination of the Kellgren–Lawrence Score
In all patients, the senior radiologists determined the severity of OA. The JSN, as well as sclerosis in each joint compartment was subdivided according to Kellgren and Lawrence into four subgroups; “none”, “minimal”, “moderate”, and “severe”. The extent of osteophyte formations was classified into “none”, “beginning”, and “extensive”. Presence of subchondral cysts and any subluxation were documented. A subsequent classification according to Kellgren–Lawrence was then made (Table 1).
Intraoperative assessment
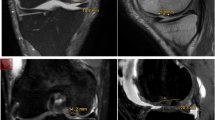
All TKA procedures followed the same surgical protocol. A cemented bicondylar surface total knee endoprosthesis was implanted (NexGen, Zimmer, Warsaw, USA), through the midvastus or medial parapatellar approach of the knee joint. Photographic documentation of all joint compartments in a bloodless field was taken using a Canon EOS 600D SLR camera. The medial and lateral parts of the femur and tibia were documented using the camera in 90° knee flexion (Fig. 1a). The photographic documentation of the patella was done after eversion of the patella in full extension of the leg (Fig. 1b). Additional photographs of the tibia were taken after tibial resection on the operating table (Fig. 2). The images under suitable image modes and digitization were standardized under the expert guidance of the trained photographer.
The extent of articular cartilage damage for each joint compartment was assessed using the modified Outerbridge scoring system as per ICRS by the senior surgeon (Table 2). The final grading of the OA for the whole joint was determined according to the compartment with the most severe arthritic changes. Postoperatively, we verified the intraoperative taken high-quality photographs again to ensure uniform classification results.
Statistical analysis
Descriptive statistics are presented in the form of the number of occurrences and percentage or mean and standard deviation (SD). The primary outcome measure was the comparison of the preoperative Kellgren–Lawrence grading system with the intraoperative International Cartilage Repair Society (ICRS) scoring system, using the exact Pearson–Clopper 95% confidence interval (CI).
Results
A total of 251 patients with a mean age of 66.8 years (range from 41 to 88 years; SD 9.2) were recruited for the final analysis. There were 163 females (64.9%) and 88 males (35.1%) of whom 135 patients (53.8%) were operated on the left knee and 116 patients (46.2%) on the right knee.
The medial joint compartment was the most commonly affected compartment in 197 patients (78.5%) followed by the patellofemoral compartment in 145 patients (57.8%) and lastly the lateral compartment in 81 patients (32.3%). In the vast majority of cases, there was a mismatch between the preoperative Kellgren–Lawrence score and the intraoperative finding.
In 160 cases (63.7%), intraoperatively determined scores were higher than the preoperative findings (95% CI 57.5–69.7%) (Fig. 3). A mismatch of two score grade points was found in 8.4% (95% CI 5.3–12.5%) (Fig. 4). The most common mismatch was noted in patients with preoperative Kellgren–Lawrence score of 3 and an intraoperative score of 4 in 48.2% (95% CI 41.9–54.6%). In only 85 patients (33.9%), the preoperative and intraoperative scores were concordant (Fig. 3). In just six patients (2.4%), the preoperatively determined score was higher than the intraoperative finding. The differences regarding each joint compartment individually were also determined and are presented in Table 3.
Discussion
Knee OA is the most common form of arthritis and a leading cause of chronic pain and disability [7,8,9]. Usually, OA involves pathological changes in most joint tissues, including cartilage, synovium, ligaments, and bone resulting in the development of osteophytes, subchondral bone cysts, and sclerosis. These degenerative changes lead to failure of the joint, which can cause immobility, and thus significant morbidity [10,11,12].
Despite the development of new imaging methods, the discordance between clinical and radiographic knee OA remains unclear. In the current study, we demonstrated an overall mismatch of 66.1% between the preoperative radiological determination and the true intraoperative finding. Nearly, half of the sample size (48.2%) showed an extensive intraoperative finding with grade four, compared to class three, according to Kellgren–Lawrence scores preoperatively. This could be explained by the fact that both position and degeneration of the meniscus account for a considerable proportion of JSN so that an accurate thickness estimation of the preserved articular cartilage layer of the knee joint with plain radiographs is not possible [13].
Kijowski et al. reported already that the Kellgren–Lawrence score had only a moderately strong correlation with the actual degree of articular cartilage degeneration within the tibiofemoral joint [14]. A more recent study published by the MARS group presented that the commonly used radiographic classification systems have a medium correlation with arthroscopic findings [2].
The original Kellgren–Lawrence score does not provide a precise definition of the joint space narrowing. Therefore, individual assessment is prone to different variations. This inaccuracy can lead to varying results of classification [15]. The association between a biological cutoff for the JSN and a significant increase in knee pain could not be identified [16].
The articular cartilage, which is very important for monitoring the course of arthritis, can only be evaluated indirectly via JSN that is not clearly defined in the description of the Kellgren–Lawrence scoring system. However, different measures of joint space width (JSW) have been introduced, including minimum JSW, mean JSW, joint space area, and location-specific JSW [17,18,19].
In cases of functional limitation due to severe symptoms but with moderate signs of OA, the experience of the surgeon plays a great role, whether the indication for total joint replacement is given. However, high demands on joint replacement surgeries as well as postoperative patient satisfaction make an exact diagnosis essential, to identify those patients who benefit from such procedures. In this context, especially in association with diverse clinical manifestations, a standardized algorithm, and an accurate classification system concerning diagnosis and therapy of knee OA are mandatory.
Concerning the intraoperative evaluation of the arthritic changes in the knee joint, the degree of chondromalacia, sclerosis as well as osteophyte formation can be estimated well as one would expect. However, we believe that an accurate intraoperative assessment of JSN is indeed not possible.
Not using the Rosenberg view of the knee joint in our center could be one of the limitations of the study. A multicenter study using six radiographic classification systems, including the Kellgren–Lawrence scoring system, demonstrated the higher interobserver reliability of the 45° posteroanterior flexion weight-bearing radiographs according to Rosenberg compared to the anteroposterior radiographs during correlation analysis with the arthroscopic findings of chondral disease [2]. Another limitation of our study is the fact that we did not include validated patient-reported outcomes, e.g., Oxford Knee Scores pre- and postoperatively, particularly that different observations regarding the correlation between preoperative radiographic disease severity of knee OA and postoperative functional outcome following TKA have been reported [20, 21]. However, the main purpose of our prospective study was to analyze the preoperative radiological results utilizing the commonly used Kellgren–Lawrence scoring system, comparing these with the actual degree of intraoperative cartilage and bone damage, utilizing high-quality photographs of the joint compartments in all included patients. Furthermore, determining the size and exact location of the cartilage lesion intraoperatively; and the degree of varus or valgus deformity preoperatively would be interesting, which have not been addressed in our study.
Summarizing our study results, we showed an apparent discrepancy between the radiologically determined JSN according to Kellgren–Lawrence and the actual grade of cartilage damage with a higher degree of intraoperative findings in the vast majority of the cases.
In conclusion, the Kellgren–Lawrence scoring system was associated with an underestimation of the real degree of knee OA. It means, the Kellgren–Lawrence scoring system is a tried and tested method for diagnosing and confirming the diagnosis of advanced cases of knee OA, as established in our study. Overestimating the severity of cartilage damage is relatively rare. On the other hand, it is not appropriate to exclude OA by X-rays, especially in mild cases as a significant underestimation could be observed. Furthermore, total knee arthroplasty is a successful procedure, but a careful selection of the suitable patients after failed conservative therapy is imperative to achieve excellent results, even in mild to moderate cases according to X-ray evaluation.
References
Braun HJ, Gold GE (2012) Diagnosis of osteoarthritis: imaging. Bone 51:278–288
Wright RW, Group M (2014) Osteoarthritis classification scales: interobserver reliability and arthroscopic correlation. J Bone Jt Surg Am 96:1145–1151
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Bedson J, Croft PR (2008) The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord 9:116
Altman RD, Hochberg M, Murphy WA Jr, Wolfe F, Lequesne M (1995) Atlas of individual radiographic features in osteoarthritis. Osteoarthr Cartil 3(Suppl A):3–70
Roemer FW, Crema MD, Trattnig S, Guermazi A (2011) Advances in imaging of osteoarthritis and cartilage. Radiology 260:332–354
Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW et al (1994) The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health 84:351–358
Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D et al (2013) The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA 310:591–608
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M et al (2012) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2163–2196
Goldring MB (2006) Update on the biology of the chondrocyte and new approaches to treating cartilage diseases. Best Pract Res Clin Rheumatol 20:1003–1025
Loeser RF (2011) Aging and osteoarthritis. Curr Opin Rheumatol 23:492–496
Lotz M, Loeser RF (2012) Effects of aging on articular cartilage homeostasis. Bone 51:241–248
Hunter DJ, Zhang YQ, Tu X, Lavalley M, Niu JB, Amin S et al (2006) Change in joint space width: hyaline articular cartilage loss or alteration in meniscus? Arthritis Rheum 54:2488–2495
Kijowski R, Blankenbaker D, Stanton P, Fine J, De Smet A (2006) Arthroscopic validation of radiographic grading scales of osteoarthritis of the tibiofemoral joint. AJR Am J Roentgenol 187:794–799
Schiphof D, de Klerk BM, Kerkhof HJ, Hofman A, Koes BW, Boers M et al (2011) Impact of different descriptions of the Kellgren and Lawrence classification criteria on the diagnosis of knee osteoarthritis. Ann Rheum Dis 70:1422–1427
Lanyon P, O'Reilly S, Jones A, Doherty M (1998) Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Ann Rheum Dis 57:595–601
Cootes TF, Taylor CJ (2004) Anatomical statistical models and their role in feature extraction. Br J Radiol 77(Spec No 2):S133–139
Ravaud P, Chastang C, Auleley GR, Giraudeau B, Royant V, Amor B et al (1996) Assessment of joint space width in patients with osteoarthritis of the knee: a comparison of 4 measuring instruments. J Rheumatol 23:1749–1755
Seise M, McKenna SJ, Ricketts IW, Wigderowitz CA (2007) Learning active shape models for bifurcating contours. IEEE Trans Med Imaging 26:666–677
Chang CB, Yoo JH, Koh IJ, Kang YG, Seong SC, Kim TK (2010) Key factors in determining surgical timing of total knee arthroplasty in osteoarthritic patients: age, radiographic severity, and symptomatic severity. J Orthop Traumatol 11:21–27
Haynes J, Sassoon A, Nam D, Schultz L, Keeney J (2017) Younger patients have less severe radiographic disease and lower reported outcome scores than older patients undergoing total knee arthroplasty. Knee 24:663–669
Acknowledgements
We acknowledge the professional support from Mr. Sven Brügmann regarding the intraoperative high-quality photographs.
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest regarding this manuscript. Outside the manuscript, one or more of the authors of this paper have disclosed the following disclosures: Waldemar Link, Hamburg, Germany, Zimmer Biomet, USA, Ceramtec, Heraeus.
Ethical approval
This study was performed after obtaining approval from the institutional review board. The PV number is “5367”.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdelaziz, H., Balde, O.M., Citak, M. et al. Kellgren–Lawrence scoring system underestimates cartilage damage when indicating TKA: preoperative radiograph versus intraoperative photograph. Arch Orthop Trauma Surg 139, 1287–1292 (2019). https://doi.org/10.1007/s00402-019-03223-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03223-6