Abstract
Purpose
To compare the recurrence risk of parameniscal cysts between arthroscopic meniscectomy with open cystectomy (arthroscopic excision) and entirely arthroscopic techniques with intra-articular cyst decompression (arthroscopic decompression).
Methods
A retrospective longitudinal study was conducted at a medical centre in Taiwan between 2002 and 2012. Patients with symptomatic parameniscal cysts undergoing either arthroscopic excision or arthroscopic decompression were included. Parameniscal cyst recurrence was evaluated every 3 months after surgery. The recurrence risk associated with treatment group, cyst volume, and meniscal tear circumference was investigated.
Results
This study included 241 young to middle-aged men and women. Of these, 112 underwent arthroscopic excision and 129 underwent arthroscopic decompression. During an average 26-month follow-up period, the arthroscopic decompression group had a sixfold higher recurrence risk [prevalence: 4 and 21 %, respectively; hazard ratio, HR 6.0 (95 % confidence interval, CI 2.3–15.6); p < 0.001] than the arthroscopic excision group. Furthermore, meniscal tears >12 mm in circumference and a cyst volume >2.4 cm3 conferred a fivefold higher recurrence risk than both lesions of smaller dimensions, both in the overall population and in the arthroscopic decompression group [HRs 5.3 (95 % CI 2.3–12.2) and 5.35 (95 % CI 2.2–13.3), respectively; p values <0.001 for both].
Conclusions
The suggestion of our study is that the recurrence of parameniscal cysts may be strongly related to large cystic lesions and large meniscal tears. Arthroscopic excision is preferable for treating parameniscal cysts, which are large cystic lesions with large meniscal tears, to reduce the recurrence risk.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Parameniscal cysts are an internal derangement of the knee joint that cause mass-like lesions and produce knee pain and joint swelling [1, 2]. Minimally invasive arthroscopic surgery represents the optimal treatment for symptomatic cases. Over the past two decades, two arthroscopic techniques have been widely used for the treatment of parameniscal cysts: arthroscopic meniscectomy with open cystectomy (arthroscopic excision), which aims to remove cysts entirely, and entirely arthroscopic techniques with intra-articular cyst decompression (arthroscopic decompression), which aims to disrupt the check-valve mechanism in the torn meniscus and decompress the cyst inside the knee joint. These two techniques are safe and effective in relieving the symptoms of affected patients [7, 9, 12, 14, 16, 18]. However, according to current treatment guidelines, no surgical techniques have been recommended to treat eligible patients with symptomatic parameniscal cysts to date [5, 18].
Some studies estimated that the prevalence of parameniscal cyst recurrence is 9.4–15 % in patients undergoing arthroscopic excision or arthroscopic decompression [7, 14]. To the best of our knowledge, data regarding this issue are scarce. Moreover, inadequate treatment of meniscal or cystic lesions is associated with a higher risk of disease recurrence and poor outcomes [7, 9, 18]. However, these observations are based on only a few case series. The hypothesis of our study was that meniscal and cystic lesions may not be adequately treated by arthroscopic decompression surgery because of limited access during the operation and preserves the wall of cysts, allowing intra-articular fluid to return, which may lead to a higher risk of cyst recurrence. Therefore, the recurrence of parameniscal cysts after arthroscopic excision or arthroscopic decompression was investigated, and the relative risk of cyst recurrence between the procedures in this single-centre retrospective longitudinal study was compared. As a result, a higher risk of cyst recurrence in patients undergoing arthroscopic decompression was found.
Materials and methods
This study was approved by the institutional review board of and performed at the Tri-Service General Hospital, a 1600-bed tertiary teaching hospital in Taiwan. We reviewed our hospital database for patients with parameniscal cysts diagnosed between 2002 and 2012 and recorded their baseline characteristics, imaging findings, operative findings, and follow-up recurrence events as evaluated by physical examinations and confirmed by magnetic resonance imaging (MRI). All patients provided written informed consent to participate in the study retrospectively. Patients with symptomatic parameniscal cysts (pain, a palpable mass, or mechanical locking unresponsive to medical treatment for a minimum of 6 months) confirmed by preoperative MRI (Vista Nuclear MRI System; Picker International, Inc., Cleveland, OH, USA, and Sigma IMR; General Electric Medical System, Milwaukee, WI, USA) were included. We excluded patients who received medical treatment only, leaving a population comprising those who underwent surgical intervention. At the Tri-Service General Hospital, traditional open meniscectomy and cystectomy have not been used in the past 15 years; instead, arthroscopic excision and arthroscopic decompression are the two major surgical options for patients with symptomatic parameniscal cysts. All affected patients willing to receive the surgery were randomly assigned to either a surgeon major in arthroscopic decompression or a surgeon major in arthroscopic excision, in the orthopaedic section. MRI images were interpreted by two experienced musculoskeletal radiologists, and any discrepancies were resolved by a third musculoskeletal radiologist. A parameniscal cyst was defined as focal parameniscal fluid collection, presenting as a palpable mass with the signal intensity of fluid on both T1- and T2-weighted imaging. Patients who met one of the following conditions were excluded from the analysis:
-
1.
those with an incomplete remission of parameniscal cysts (a residual mass and/or no improvement in pain or knee function scores) within 6 months of primary surgery (regarded as a failed surgical outcome);
-
2.
those with concomitant severe knee derangement {an anterior/posterior cruciate ligament tear, a medial/lateral collateral ligament tear, and/or severe arthrosis [French Society of Arthroscopy (SFA) Grade IV]};
-
3.
those with inflammatory arthritis, such as rheumatoid or gouty arthritis;
-
4.
those with old intra-articular fractures of the tibial plateau or distal femur; and
-
5.
those who failed to attend an outpatient follow-up examination every 3 months.
Parameniscal cyst recurrence was defined as a relapsed mass, with joint-line pain or mechanical symptoms, at the original operative site after the complete remission of previous symptoms. All recurrences were confirmed by MRI imaging. We compared potential risk factors related to recurrence, including age, sex, body mass index, pattern of meniscal tearing, associated intra-articular derangement, cyst volume, and meniscal tear circumference at baseline between the arthroscopic excision and arthroscopic decompression groups. Cyst volume and meniscal tear circumference were measured from preoperative MRI images in each patient. Cyst volume was defined as the sum of a cyst’s surface area in each axial slice multiplied by the slice thickness (4 mm) from its superior to inferior edges (Supplemental Figure S1). Meniscal tear circumference was defined as the longest dimension from the anterior to posterior aspects of the meniscal tear in coronal MRI images (Supplemental Figure S2). The test–retest reliability coefficients for the cyst volume and meniscal tear circumference were 0.92 and 0.89, respectively. Other factors, including the pattern of meniscal tearing and associated internal derangement, were acquired from intra-operative documentation.
Surgical technique
In both groups, all patients underwent routine arthroscopic examination with anterolateral and anteromedial portals. The torn meniscus was carefully probed, and an underlying connecting tract to the peripheral cyst was found in all cases. The torn meniscus was carefully resected back to a stable rim using the standard technique. In some patients with a repairable meniscal tear, such as a peripheral vertical tear or bucket-handle tear, menisci were repaired using an arthroscopic inside-out technique with nonabsorbable sutures.
In the arthroscopic excision group, open cystectomy with a visible margin of normal soft tissue was performed. After inserting a small curette from the meniscal tear to the localized meniscocapsular opening, the opening was repaired with nonabsorbable sutures. To treat cystic lesions in the arthroscopic decompression group, a motorized shaver or small curette was introduced into the cyst through the intra-substance tract in the torn meniscus to debride the connecting tract, open the meniscocapsular junction, and disrupt the septa of lobulated cysts. The cystic wall was not removed or was only partially removed. Finger-tip compression from the outer aspect of the knee joint directly down to the shaver tip helped complete intra-articular decompression (Supplemental Figure S3).
Rehabilitation programme following surgery
In both groups, patients without meniscal repair were restricted to partial weight-bearing movement with crutches in the first 4 weeks postsurgery. In patients who underwent meniscal repair, protective partial weight-bearing movement with crutches for the first 8 weeks postsurgery and knee range of motion with permission to attempt 60° flexion in first 2 weeks, 120° at 4 weeks, and full flexion at 8 weeks, were suggested. The proportion of patients that adhered to the rehabilitation programme was approximately 95 % in each group, according to their self-reported statements.
Surgical outcomes and longitudinal assessment of recurrence events
The knee condition of all patients was followed up in the outpatient department every 3 months for 3 years. The outcome of interest was cyst recurrence, which was defined as a clinically palpable mass in the treated area that was visible on MRI after 6 months postsurgery. At 6-month intervals, we also evaluated changes in postoperative visual analogue scale (VAS) pain and Lysholm Knee Scoring Scale scores. All patients who experienced recurrence were treated by arthroscopic excision. After revision surgery, no further recurrence events have occurred to date. This study was approved by the institutional review board of Tri-Service General Hospital National Defense Medical Center (ID number: 2-101-05-131).
Statistical analysis
The study was designed to have a power of 80 % to detect a 10 % increase in the recurrence for patients in the arthroscopic decompression group as compared with the arthroscopic excision group, assuming a two-sided alpha level of 0.05 and a recurrence rate of 5 % in the arthroscopic excision group. The baseline characteristics of patients were presented as numbers and percentages for categorical data and means ± standard deviation (SD) for normal data. The Student’s t test for continuous data and Chi-squared test for categorical data were used to compare the two groups. The follow-up time for each subject, defined as person-months at risk, began with the date of the operation and ended with parameniscal cyst recurrence as the time the patient had recurrent symptoms or the end of the study period (maximum duration of 3 years). Kaplan–Meier survival curves were plotted to depict the cumulative probabilities of recurrence for the study subjects over time. Curves were compared using the log-rank test. Cox proportional hazards regression models were used to determine the adjusted hazard ratios (HRs) for parameniscal cyst recurrence associated with treatment group, cyst volume, and meniscal tear circumference, both for the whole study cohort and for the arthroscopic decompression group. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). All p values <0.05 were considered statistically significant.
Results
Figure 1 shows the selection of eligible patients for analysis. After excluding those with medical treatment only, concomitant cruciate ligament or collateral ligament injuries, old intra-articular fracture of the tibial plateau, rheumatoid arthritis, lost to follow-up, or incomplete remission within 6 months of surgery, there were 241 patients (88 %) eligible for inclusion in the analysis (112 received arthroscopic excision, and 129 received arthroscopic decompression).
Table 1 shows the baseline characteristics of patients who underwent arthroscopic excision and of those who underwent arthroscopic decompression. The patients were young to middle aged and predominantly male. MRI imaging determined that the median of cyst volume was 2.4 cm3, and the average meniscal tear circumference was 13.2 mm. Meniscal repair was performed in six patients (5 %) with arthroscopic excision and in eight patients (6 %) with arthroscopic decompression. Notably, there were no significant differences in baseline demographic, MRI, and surgical findings between groups. However, a significantly larger proportion of patients had a cyst volume greater than the median in the arthroscopic excision group (p = 0.038).
Table 2 shows the changes in VAS pain and Lysholm Knee Scoring Scale scores in each group. There was no significant difference in the change in VAS pain scores between the two groups. Compared with arthroscopic excision, arthroscopic decompression yielded a relatively greater improvement in Lysholm Knee Scoring Scale scores (p = 0.014).
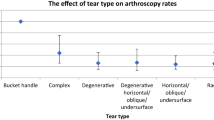
Table 3 shows the risk of parameniscal cyst recurrence associated with cyst volume, meniscal tear circumference, and the surgical technique used. Arthroscopic decompression was associated with a higher recurrence risk than arthroscopic excision [recurrence: 27 and 5 cases, respectively; HR 6.0, p < 0.001] during an average 26-month follow-up period (range 7–36 months).The average recurrent cyst sizes in patients undergoing arthroscopic excision and in those undergoing arthroscopic decompression were 1.9 cm3 (range 1.2–2.2 cm3) and 2.1 cm3 (range 1.2–4.2 cm3), respectively (data not shown). Furthermore, preoperative cyst volume and meniscal tear circumference were both associated with recurrence (p value for trend: <0.05). Compared with a cyst volume ≤2.4 cm3 and a tear circumference ≤12 mm, a reference was found to be associated with the development of parameniscal cysts in a previous study [28]; a cyst volume >2.4 cm3 and a tear circumference >12 mm were associated with the highest recurrence risk, both in the overall cohort and in the arthroscopic decompression group [HRs 5.3 and 5.4, respectively; p values <0.001 for both]. Figure 2 shows the Kaplan–Meier curves of parameniscal cyst recurrence in both groups. Cyst recurrence occurred an average of 12.3 months (range 7–26 months) after arthroscopic surgery. Recurrence was significantly higher after arthroscopic decompression than after arthroscopic excision (log-rank p value <0.001). Figure 3 shows the Kaplan–Meier curves of cyst recurrence across four subgroups categorized by a cyst volume of 2.4 cm3 and a meniscal tear circumference of 12 mm in the arthroscopic decompression group. Recurrence was significantly higher in the group in which both lesions were greater in size than in the other three groups.
Paramensical cysts recurrence rate in the arthroscopic excision and arthroscopic decompression groups. The Kaplan–Meier curves show the cysts recurrence occurring on an average of 12.3 months (range 7–26 months) after the primary surgery. There was a higher recurrence rate in the arthroscopic decompression group than the arthroscopic excision group (log-rank p value <0.001)
Paramensical cysts recurrence rate categorized into four subgroups by cyst volume and meniscal tear circumference in the arthroscopic decompression group. The Kaplan–Meier curves show the recurrence rate of the cystic volume >2.4 cm3 and meniscal tear circumference >12 mm group significantly higher than the other three cyst volume/meniscal tear circumference groups (log-rank p value <0.001). The cutoff point of cyst volume was selected by the median of 2.4 cm3
Discussion
The finding of our study was that a sixfold increased risk of cyst recurrence associated with arthroscopic decompression compared with arthroscopic excision for patients with symptomatic parameniscal cysts during an average 26-month follow-up period. Furthermore, cyst volume and meniscal tear circumference are associated with disease recurrence. Notably, patients with both a greater cyst volume and bigger meniscal tear circumference were at a fivefold increased risk of disease recurrence than those in whom both lesions were smaller.
Parameniscal cysts are common in about 4–8 % of patients with a torn meniscus. Most cysts exhibit horizontal cleavage or are combined with horizontal cleavage components [1, 2, 6, 18, 23]. Their pathogenesis is mostly related to the myxoid degeneration of collagen, which can result in the delamination of meniscal substance [9, 23, 28]. Consequently, parameniscal cysts are formed as a result of the forceful extravasation of joint fluid through the torn meniscus [2, 3, 6, 16, 23, 27]. Wu et al. [28] reported that a large meniscal tear circumference, with a cutoff value of ≥12 mm, confers the strongest risk of parameniscal cyst development. Their finding suggests that meniscal tear size is one of the main factors underlying the pathogenesis of parameniscal cysts.
Regarding parameniscal cyst recurrence, several studies [14, 18, 21, 22, 24] have identified risk factors, such as failure to disrupt the check-valve mechanism or to open the meniscocapsular junction in meniscal cysts. A larger meniscal tear size may prevent surgeons from completely opening the check-valve mechanism and debriding the meniscal substance and its connecting tract. As a result, the check valve persists, and joint fluid continues to extravasate in an inside-out direction and accumulate in the parameniscal space. When treating meniscal pathology, we recommend that in addition to resection of the torn meniscus back to a stable rim, debridement of the connecting tract and opening of the meniscocapsular junction are necessary to disrupt the check valve and balance the pressure between the bilateral ends.
Another risk factor for parameniscal cyst recurrence is large cyst volume. Today several high-quality randomized studies have reported that resection of the meniscal lesion alone, or even watchful waiting, can relieve the symptoms of patients with degenerative meniscal tears [13, 15, 25]. Also, the treatment of popliteal cysts is today less dependent on surgery than some years ago [8]. In contrast, Reagan et al. [21] advocated that both the torn meniscus and the cyst should be addressed simultaneously. Cases in which the cysts were treated simultaneously to the torn meniscus had 80 % good or excellent results, whereas cases in which the cysts were not addressed had only 50 % good or excellent results. In this study, only 16 symptomatic patients receiving medical treatment were too few to have enough power as compared with those undergoing arthroscopic surgery; whether there was a benefit of combined meniscal tear and parameniscal cyst treatment in symptomatic patients undergoing surgical treatment requires further investigation.
To preserve more meniscal substance, several arthroscopic techniques and outside-in methods of decompressing cysts while avoiding the torn meniscus have been reported. Howe et al. [12] described the arthroscopic internal marsupialization of meniscal cysts, which creates a 5-mm channel through the knee capsule adjacent to the cyst to equalize the pressure between the cyst and intra-articular compartment. Ugur et al. [11] created an intra-articular portal on the anterior synovial wall of cysts and inserted a shaver to decompress the cyst. In a study by Tudisco, a cyst was decompressed from an outside-in direction by percutaneously inserting a shaver after arthroscopically debriding the meniscal lesion [26]. The clinical outcomes of these studies were good to excellent, and there were no cases of recurrence. However, these studies involved small numbers of patients and did not compare characteristics of meniscal cysts, such as cyst volume or meniscal tear circumference.
Since parameniscal cysts possess a multilobulated structure and an irregular shape, not every case is suitable for intra-articular decompression [10, 19, 20]. Complete destruction of the intra-cystic septa through the connecting tract to balance the pressure between the bilateral ends is difficult, particularly in large cysts that occupy a more extensive area [4, 16, 17]. It is known that an inadequate surgical treatment of parameniscal cysts is associated with poor outcomes, including a high risk of disease recurrence; our findings in patients undergoing arthroscopic decompression were consistent with this and with our hypothesis.
The strengths of our study are that the baseline characteristics of patients were very similar between two groups, allowing us to avoid a moderator effect even when controlled by adjustments for multiple covariates. In addition, the overall recurrence was 13.3 %, which was similar to the results of previous studies that ranged from 9.4 to 15 %. The limitations of our study included its retrospective and nonrandomized design, which may have led to bias. Furthermore, postoperative MRI images were not routinely evaluated in asymptomatic patients; thus, an objective estimate of postoperative cyst size was lacked in our study.
Conclusion
Our suggestion was that parameniscal cyst recurrence may be strongly related to large cystic lesions and large meniscal tears. Thus, arthroscopic excision is recommended for the treatment of parameniscal cysts, which have both large cystic lesions and large meniscal tears, to reduce the recurrence risk.
References
Anderson JJ, Connor GF, Helms CA (2010) New observations on meniscal cysts. Skeletal Radiol 39:1187–1191
Barrie HJ (1979) The pathogenesis and significance of meniscal cysts. J Bone Joint Surg 61B:184–189
Burgan DW (1971) Arthrographic findings in meniscal cysts. Radiology 101:579–581
Chang A (2009) Imaging-guided treatment of meniscal cysts. HSS J 5:58–60
Cowden CH 3rd, Barber FA (2014) Meniscal cysts: treatment options and algorithm. J Knee Surg 27:105–111
De Smet AA, Graf BK, del Rio AM (2011) Association of parameniscal cysts with underlying meniscal tears as identified on MRI and arthroscopy. AJR Am J Roentgenol 196:180–186
El-Assal M, Mostafa M, Abdel-Aal A, El-Shafee M (2003) Arthroscopy alone or in association with open cystectomy: in treatment of lateral meniscal cysts. Knee Surg Sports Traumatol Arthrosc 11:30–32
Frush TJ, Noyes FR (2015) Baker’s cyst: diagnostic and surgical considerations. Sports Health 7:359–365
Glasgow MM, Allen PW, Blakeway C (1993) Arthroscopic treatment of cysts of the lateral meniscus. J Bone Joint Surg Br 75:299–302
Guermazi A, Hayashi D, Roemer FW et al (2010) Cyst-like lesions of the knee joint and their relation to incident knee pain and development of radiographic osteoarthritis: the MOST study. Osteoarthr Cartil 18:1386–1392
Haklar U, Ayhan E, Ustundag S, Canbora K (2014) A new arthroscopic technique for lateral parameniscal cyst decompression. Knee 21:126–128
Howe TS, Koh JS (2007) Arthroscopic internal marsupialization of meniscal cysts. Knee 14:408–410
Howell R, Kumar NS, Patel N, Tom J (2014) Degenerative meniscus: pathogenesis, diagnosis, and treatment options. World J Orthop 5:597–602
Hulet C, Souquet D, Alexandre P, Locker B, Beguin J, Vielpeau C (2004) Arthroscopic treatment of 105 lateral meniscal cysts with 5-year average follow-up. Arthroscopy 20:831–836
Järvinen TL, Sihvonen R, Malmivaara A (2014) Arthroscopic partial meniscectomy for degenerative meniscal tear. N Engl J Med 370:1260–1261
Lu KH (2006) Arthroscopic meniscal repair and needle aspiration for meniscal tear with meniscal cyst. Arthroscopy 22:1367
Macmahon PJ, Brennan DD, Duke D, Forde S (2007) Ultrasound-guided percutaneous drainage of meniscal cysts: preliminary clinical experience. Clin Radiol 62:683–687
Pedowitz RA, Feagin JA, Rajagopalan S (1996) A surgical algorithm for treatment of cystic degeneration of the meniscus. Arthroscopy 12:209–212
Pinar H, Boya H, Satoglu IS, Oztekin HH (2009) A contribution to Pisani’s sign for diagnosing lateral meniscal cysts: a technical report. Knee Surg Sports Traumatol Arthrosc 17:402–404
Pisani AJ (1947) Pathognomonic sign for cyst of knee cartilage. Arch Surg 54:188–190
Reagan WD, McConkey JP, Loomer RL, Davidson RG (1989) Cysts of the lateral meniscus: arthroscopy versus arthroscopy plus open cystectomy. Arthroscopy 5:274–281
Ryu RK, Aj Ting (1993) Arthroscopic treatment of meniscal cysts. Arthroscopy 9:591–595
Sarimo J, Rainio P, Rantanen J, Orava S (2002) Comparison of two procedures for meniscal cysts. A report of 35 patients with a mean follow-up of 33 months. Am J Sports Med 30:704–707
Seger BM, Woods GW (1986) Arthroscopic management of lateral meniscal cysts. Am J Sports Med 14:105–108
Stensrud S, Risberg MA, Roos EM (2014) Knee function and knee muscle strength in middle-aged patients with degenerative meniscal tears eligible for arthroscopic partial meniscectomy. Br J Sports Med 48:784–788
Tudisco C, Meo A, Blasucci C, Ippolito E (2000) Arthroscopic treatment of lateral meniscal cysts using an outside-in technique. Am J Sports Med 28:683–686
Wroblewski BM (1973) Trauma and the cystic meniscus: review of 500 cases. Injury 4:319–321
Wu CC, Hsu YC, Chiu YC et al (2013) Parameniscal cyst formation in the knee is associated with meniscal tear size: an MRI study. Knee 20:556–561
Acknowledgments
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chang, JJ., Li, YH., Lin, GM. et al. Comparison of the recurrence risk of parameniscal cysts between patients treated with arthroscopic excision and arthroscopic decompression techniques. Knee Surg Sports Traumatol Arthrosc 24, 1547–1554 (2016). https://doi.org/10.1007/s00167-016-3998-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-3998-0