Abstract
Background
The use of noninvasive diagnostics in coronary artery disease remains underdeveloped. To date, there is no simple and inexpensive method that can lead to a reliable diagnosis. Aside from costly and elaborate imaging techniques, exercise ECG, with its rather moderate sensitivity and specificity, is the main diagnostic method available.
Methods
In this prospective study of 109 patients, the diagnostic value of cardiogoniometry (CGM), a three-dimensional, computer-analyzed vector cardiogram, was determined before and after physical stress, and the results were compared with those obtained from a stress test. We also investigated whether the sensitivity and specificity of the classical bicycle stress test could be increased with the addition of measurements obtained by CGM. Coronary angiography was used as a reference method.
Results
CGM had a sensitivity of 39% at rest and 42% after physical stress and a specificity of 63% at rest and 57% after stress. This method was found to be markedly inferior to pre-test probability (sensitivity 53%, specificity 81%), stress ECG (sensitivity 52%, specificity 81%), and resting ECG (sensitivity 50%, specificity 64%). The efficiency of exercise ECG testing was not improved by use of CGM results.
Conclusion
If CGM is to be established as a viable diagnostic method in daily clinical practice, it must undergo further development.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Although chronic ischemic heart disease is the most common cause of death in Germany [1], the steady decline in mortality due to coronary artery disease (CAD) during recent years [2] demonstrates the success of therapeutic options as well as the importance of timely therapy. Thus, early diagnosis is critical, especially in view of the enormous prevalence of this disease.
If CAD is suspected, diagnostic tests based on established guidelines are initiated (patient history, physical examination, and laboratory tests) [1, 3]. Pre-test probability assessment takes into account a number of factors, including age, gender, and symptoms, and accordingly attaches a risk factor to the various combinations [4]. Repolarization disturbances, left ventricular hypertrophy, conduction disturbances, or signs of a prior myocardial infarction can be indications of CAD. Stress testing has a sensitivity of 68%. Guidelines dictate that due to its relatively high specificity of 77%, a stress ECG should be carried out in the initial diagnostic phase if CAD is suspected [1, 5]. Nevertheless, the stress test has many diagnostic weaknesses due to potential sources of interference.
Stress echocardiography is another diagnostic measure that can yield information about cardiovascular morbidity and aid in the detection of ischemia [1, 6]. Computed tomography may also be useful in diagnosing CAD [7, 8]. Various types of functional investigations of the myocardium are possible with magnetic resonance imaging (MRI), such as myocardial perfusion stress MRI with adenosine administration or dobutamine stress MRI [9–13]. In spite of the value of these noninvasive methods in terms of their high sensitivity and specificity (stress echocardiography approx. 90%, stress MRI 80–90%/80–86%), they should only be carried out with sufficient expertise [14]. Myocardial scintigraphy provides information about the perfusion of the myocardium at rest as well as under pharmacological stress and can differentiate between scar tissue and reversible ischemia. It can also help to determine the functional significance of stenosis, for example when the results of an angiogram are inconclusive. Although these methods demonstrate high sensitivity, they are not diagnostic methods of first choice due to their enormous cost, complexity, and radiation exposure [6]. Coronary angiography remains the gold standard in CAD diagnostic testing [15].
However, angiographic severity of CAD correlates poorly with functional significance. To further evaluate functional significance of intermediate stenosis, measuring the fractional flow reserve (FFR) is an option [11, 16–18].
Important disadvantages of invasive diagnostics, however, include sometimes serious but rarely occurring complications such as bleeding, arrhythmias, embolism, myocardial ischemia, or anaphylactic reactions [19].
Cardiogoniometry (CGM) according to Sanz was first reported in the 1980s. It is based on the principle of vectorcardiography, which was first described in 1937 by Schellong et al. After several studies were carried out to determine the maximal vectors of the QRS and T intervals, there followed a lapse in reports concerning CGM [20–24]. It was not until 2007 that further methodological studies were carried out using new-generation equipment. With three-dimensional graphics and positioning of the cardiac potential, over 300 new parameters are available for use in the diagnosis of CAD. The difference between CGM and conventional vector ECG is mainly the position of the axes of the vectors [25]. This simple method is carried out with only four electrodes that are applied in a particular arrangement. According to the manufacturer of the apparatus, CGM constitutes a straightforward, rapid, and inexpensive technique that can complement other noninvasive methods to diagnose CAD.
One advantage of CGM is the brief duration of the test and the fact that it can be carried out at rest, which means that it can be applied to patients who are unable to undergo a stress test. The simple and rapid application as well as the automated interpretation of the results shows the great potential of this method. Thus, CGM could be used for patients with either stable or unstable angina pectoris and also as a possible screening test for asymptomatic patients.
During physical exercise, however, CGM would show earlier signs of CAD than at rest as coronary artery stenosis can result in acute ischemia under these conditions. The use of CGM during exercise was addressed only in an older study with outdated analytical methods [26]. This application of CGM was tested in our study using modern methods. Current basic diagnostics employing exercise ECG could be augmented by CGM.
Methods
Study design
The study was approved by the ethics committee of the Otto von Guericke University of Magdeburg. The study was conducted according in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Between March 2011 and October 2013, 123 patients aged 18 to 75 who had symptoms of stable angina pectoris or a positive exercise ECG result with preserved systolic function were prospectively enrolled in the study. Exclusion criteria were the previous cardiac disease, renal insufficiency, or the inability to undergo physical stress. All patients were referred for elective coronary angiography by general practitioners or smaller hospitals. 29.3% of patients had a myocardial scintigraphy. 71.4% had an external bicycle testing.
Upon admission, a patient history was taken, patients were given a physical examination, and routine laboratory blood tests were performed. A 12-lead ECG recording was made and transthoracic echocardiography was carried out to exclude a reduced ejection fraction or advanced cardiac disease. Patients gave written informed consent for participation in the study.
Before the stress test, an initial CGM recording was made at rest in a supine position. Exercise ECG was then carried out in a sitting position using a bicycle ergometer according to current guidelines. Another CGM recording was then made in resting, supine patients after the stress test. For CGM measurements, a CGM device was used along with the computer software CGM-CARDIOLOGIC EXPLORER 1.7.1.0 (both from enverdis® GmbH). With use of three-dimensional graphics and mapping of the cardiac potential, CGM yields over 300 novel parameters such as scattering or the angle of depolarization events that can be used in diagnosing CAD [27]. The procedure essentially entails the evaluation of various parameters in different combinations that are then summarized in a final score. Different combinations of parameters are used for men and women. If a deviation from normal depolarization spreading is recorded, an appropriate set of parameters is automatically chosen according to that difference and used for the analysis [28]. Due to the high degree of complexity of the individual factors, manual interpretation would have a high risk of subjective influence and could only be carried out by operators with great expertise; thus, manual analysis would be impractical. For this reason, this study was designed to investigate results obtained only via the automated analysis.
Coronary angiography was used as a reference method and provided the possibility of intervention with balloon angioplasty or stent implantation. Coronary stenosis of more than 75% was taken as confirmation of coronary disease. The control group was made up of patients with a medium level of stenosis (50–75%), insignificant coronary disease (<50% stenosis), or non-stenosed vessels. Coronary angiography was performed by different physicians. Grading of angiographically detected stenosis was done by visual estimation. The decision to further treatment (CABG, conservative, PCI) was left to the discretion of the treating physician and was dependent on clinical presentation, functional testing (ambulatory bicycle testing and/of myocardial scintigraphy) and morphology of the stenosis. The treating physician was blinded to the results of CGM.
Following retrospective exclusion of several patients due to technical difficulties, the data from a total of 109 patients were analyzed in the study.
Statistical analysis was carried out with the software SPSS Statistics Student Version 18.0. For constant variables mean, standard deviation, minimum, and maximum were calculated and expressed as \(\dot x \pm s\). The level of significance in the comparison of means was determined by Student’s t test. In cases of significant differences in variance (Levene test), Welch’s t test was applied. Correlation analysis was performed using Pearson’s correlation coefficient, and for non-linear relationships, Spearman’s rank correlation was applied. The level of significance for small sample sizes was determined by Fischer’s exact test. For more than two variables, the Chi-squared test was applied, and in some cases, two of the variables were tested against each other. In general, if α = 0.05 (error of the first type), a difference was considered significant. Each test was carried out without α adjustments. For each of the noninvasive methods, e.g., resting ECG, stress ECG, or CGM, sensitivity, and specificity were determined with regard to coronary angiography, considered the gold-standard method. The predictive value and false positive and false negative case numbers were also calculated. For cases with a positive test result, an odds ratio was determined to estimate the risk of disease. Finally, binary logistic regression analysis (SPSS Version 22) was used to determine the test efficiency of individual parameters in relation to CAD.
Results
Significant coronary disease was observed for 28.4% (n = 31) of the study participants. Accordingly, the control group consisted of 71.6% (n = 78) patients (8.3% medium grade stenosis; 22.9% insignificant stenosis; 40.4% no stenosis). Table 1 shows a summary of basic clinical characteristics of the groups.
In 12 patients, a PCI was performed, 16 patients were treated with CABG, the remaining patients were managed by optimal medical treatment. Mean Gensini score was 64.82 (±47.4) in the CAD group vs. 2.16 (±4.5) in the control group.
Patients with a positive diagnosis of CAD were significantly more often male (83.8 vs. 52.6% in the control group; p = 0.002). Significantly, more CAD patients had arterial hypertension (96.8 vs. 78.2%; p = 0.021) and diabetes mellitus (41.9 vs. 24.4%, p = 0.016). Angina pectoris was significantly more frequent among CAD patients (p = 0.028); a typical APS was present in almost half of the group with CAD. Patients with CAD also had a significantly higher pre-test probability (p < 0.001); this was 62.2 ± 17.8% for CAD patients and 42.3 ± 21.0% for control patients. Risk was stratified into low (<15%), medium (two subgroups of 15–66% and 67–85%), and high (>85%). Most participants in the study fell into the medium risk category. Among patients with relevant CAD 45.2% had lower medium risk (15–66%) and 54.8% had upper medium risk (67–85%). In the control group, almost 80% were in the 15–66% risk subcategory and the remaining approximately 20% were in the subcategory 67–85% (Table 1).
There were no significant differences between the two groups for age, BMI, nicotine use, hyperlipidemia, family history, comorbidities, medical therapy, outpatient diagnostics, resting ECG, or echocardiography.
A total of 82.4% of the exercise ECG tests were analyzed; the remaining test results were not evaluated, because the level of performance was submaximal. There were a significantly higher proportion of positive test results (p = 0.003) among patients in the CAD group than among control patients (Table 2).
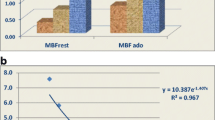
In the group of patients with CAD, 38.7% had a positive result in the CGM test conducted under resting conditions. Thus, the majority of this group had a negative test result. In the control group of patients, 37.2% had a positive CGM result (Fig. 1). In summary, there were no significant differences between the groups for the CGM test at rest (p = 1.000).
A similar distribution of results was obtained for CGM tests conducted during exercise (p = 1.000). A total of 41.9% of CAD patients had a positive test, nearly the same proportion of patients with no relevant CAD (42.9%). There were also no differences between patient groups when they were divided according to the severity of coronary stenosis. In addition, the CGM results, both at rest and during exertion, were evaluated as a whole, such that a positive result for one test was counted as an overall positive result. For this evaluation, 61.3% of the CAD group and 52.6% of the non-CAD group had a positive CGM result; thus, there were no differences between the groups (p = 0.523). There were only slight, insignificant differences between the various subgroups based on degree of stenosis in this analysis.
The score of the automated analysis gives the number of parameters that differ from the physiological norm. A total of 61.2% of the CAD patients displayed no abnormal parameters; a further 22.6% had one pathological result and 16.1% had two or more results outside of the reference values (Fig. 2). The control group with no CAD had a similar distribution of parameters (p = 0.466).
Following exercise, 58.1% of the CAD patients had CGM parameters within the normal range and would have been diagnosed as healthy using this test. In the group of patients without coronary disease, 57.1% had normal values. Hence, with the gradations having similar percentages, there were no significant differences noted between the groups at rest or post-exercise in evaluating the score.
The automated results also give information about the parameter sets used. These are chosen automatically according to the vector loop of the potential. Here, too, there were no significant differences between the two groups of patients.
A nonspecifically localized ischemia was registered in 28.4% of the findings. The CGM device allowed more precise localization (e.g., apical, lateral, and septal) in only 6.6% of the data sets. In 2.8% of the results, there was a positive CGM that gave no automatic evaluation of the position. The displayed localization of the inadequate perfusion was incorrect or there was no relevant CAD present (Table 3).
The test quality criteria and odds ratios are summarized in Table 4. The pre-test probability and the stress ECG showed the highest sensitivity and specificity and demonstrated a high probability that CAD was present when there was a positive test result. CGM had a markedly lower efficiency, both at rest and after exercise. Altering the definition of CAD (>50% stenosis) did not change this result.
The pre-test risk evaluation allowed a correct diagnosis in a total of 73.1% of all patients. In combination with exercise ECG results, 75.9% of the patient collective was correctly diagnosed. The variables diabetes mellitus, arterial hypertension, and CGM showed no additional advantage for diagnostic accuracy.
A further analysis was carried out to test the second working hypothesis. The test efficiency of the exercise ECG was 71.3%. Addition of CGM results did not yield a better test efficiency (Table 5).
Conclusions
Owing to the significant risk of mortality posed by CAD, a considerable number of cardiac catheterizations are carried out in Germany, also compared with international figures. In 2011, only one-third of these examinations were performed in patients with angina pectoris [29]. In the present study, 28.4% of patients were shown via catheterization to have coronary disease. This level rose to 36.7% if patients were included who had a moderate level of stenosis. Patel et al. reported in 2010 results for nearly 400,000 patients who underwent diagnostic coronary angiography; a similar level of 37.6% showed relevant CAD [30]. Aside from the individual risk of coronary angiography for patients, these tests place an enormous financial burden on the healthcare system. It would be advantageous to prevent or limit this burden by reducing the number of cardiac catheterizations; however, there is a lack of definitive noninvasive diagnostic methods. Patient history and clinical findings as well as the results of noninvasive diagnostics provide evidence that can support a suspicion of CAD or dismiss it.
The relationship between CAD and arterial hypertension, gender, and diabetes mellitus is well known and was demonstrated in the present study. The highly predictive value of angina pectoris as a classical symptom of CAD was confirmed in our study, as expected [31–34].
The diagnostic efficiency of the 12-lead ECG in the present study was similar to that reported in the literature, with a sensitivity of 50% [35]. In spite of its low test efficiency, use of the 12-lead ECG in diagnosing CAD is justified, as with this simple method, important differential diagnoses can be ruled out or a high probability for CAD can be demonstrated [2].
The pre-test risk assessment, with a combination of angina pectoris and patient age and gender, showed the best predictive power. A comprehensive patient history and thorough physical examination including assessment of cardiovascular risk factors are thus essential tools of the clinician.
A large meta-analysis of 147 studies that included a total of approximately 24,000 patients demonstrated a mean sensitivity of 68% for exercise ECG testing. The mean specificity was found to be 77%. Notably, there was great variation in both of these parameters: 23–100% for sensitivity and 17–100% for specificity [5]. If one compares these values with our data, both sensitivity (52.0%) and specificity (81.3%) are within the simple standard deviation (68 ± 16 and 77 ± 17%, respectively). Therefore, the insufficient sensitivity of this diagnostic method is not only a problem demonstrated in the present study but must be viewed as a fundamental shortcoming. The combination of pre-test risk assessment and exercise ECG leads to a slight improvement in diagnostic yield.
In theory, CGM is a promising diagnostic method to simply and quickly arrive at a diagnosis of CAD. Schüpbach et al. determined retrospectively a sensitivity of 73% and a specificity of 87%. In the prospective part of the study, the diagnostic accuracy of CGM was 71%, significantly higher than that of resting ECG [25′]. In a smaller study, the method was tested in a cohort of 109 female patients; here, a sensitivity of 78.9% and a specificity of 87.1% were reached [36]. Sanz and Schüpbach tested 1027 patients for rhythm and T-wave amplitude with five parameters each. For roughly 700 patients with a NORM score, CGM had a sensitivity of 84% and a specificity of 90% [37]. In comparison with the present work, the studies discussed here showed a higher diagnostic accuracy of CGM. A reason for the apparently higher test quality in the latter study could be that the evaluation was performed exclusively under NORM score conditions. Thus, only results without any cardiac rhythm disturbances were included. In 2010, Huebner et al. published a meta-analysis of six studies of vector ECG and CGM. The mean sensitivity and specificity were 73 and 84%, respectively [38]. Due to the high proportion of studies using vector ECG, these results cannot be interpreted as being representative. An older study from 1988 evaluated the use of CGM during rest and exercise, similar to the present study. The results of this meanwhile outdated study showed a sensitivity and specificity of 62 and 64% under resting conditions. The second test, administered directly after exercise with a load of 50 W on a bicycle ergometer, showed an improved accuracy (sensitivity 72% and specificity 73%). The combined analysis resulted in a higher sensitivity at the cost specificity (sensitivity 78%, specificity 64%) [26]. In the present study, these values were not achieved. There was also no difference between the results obtained before and after exercise.
It is difficult to account for the in-part great divergence between the findings of the current study and those in the literature. Evaluation of a defined level of CAD with at least 50% coronary stenosis, as commonly found in other studies, showed little if any improvement in the results. In addition, use of the values after exercise or combined analysis with CGM did not increase the accuracy.
Compared with CGM, exercise ECG and pre-test probability had a higher specificity of 81.3% each. The value for resting ECG, 63.6%, was similar to that of resting CGM. The sensitivity was the highest for the pre-test probability, 53.1%, with the exercise and resting ECG values being comparable (52.0 and 50.0%, respectively). The sensitivity of resting (38.7%) and post-exercise CGM (41.9%) was markedly lower. In the combined analysis of CGM results sensitivity was the highest at 61.3%; however, as it had the lowest specificity (47.4%), this test would have little use in daily clinical practice. The addition of CGM to exercise ECG did not lead to an improvement in diagnostic yield.
In addition to the poor test efficiency, CGM has some technical issues. In the present study, after other exclusion criteria were considered, further four patients had to be excluded. CGM proved to be very prone to technical disturbances, and the execution of the test was not as straightforward as expected. Furthermore, the mapping of the ischemic regions [27] could not be confirmed. Whereas most of the ischemic signals were rated as unspecific, for the remaining values, there was either no information or they were localized to the wrong regions. Considering test implementation and quality, CGM appears to have even less validity than the conventional resting ECG.
Based on our experience, CGM in its present state of development is not a meaningful method for diagnosing stable CAD. A possible source of error may be the automated analysis. Manual interpretation, however, is not objective and due to the high complexity of the test method difficult to learn.
Due to the complexity of the automated analysis, only the manufacturer of the CGM may be able to improve sensitivity and specificity by enhancing and optimizing the underlying algorithm.
References
Bundesärztekammer (BÄK) (2014) Nationale VersorgungsLeitlinie Chronische KHK - Langfassung, 2. Auflage. Version 2. 2013 zuletzt verändert: 2014. http://www.leitlinien.de/mdb/downloads/nvl/khk/khk-2aufl-vers2-lang.pdf. Accessed Nov 13
Tunstall-Pedoe H, Kuulasmaa K, Mähönen M, Tolonen H, Ruokokoski E (1999) Contribution of trends in survival and coronar y-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA Project populations. Lancet 353(9164):1547–1557
Scottish Intercollegiate Guidelines Network (SIGN) (2014) Management of stable angina. (SIGN Guideline No 96). http://www.sign.ac.uk/pdf/sign96.pdf. Accessed Nov 27
Montalescot G, Sechtem U, Achenbach S, et al. (2013) ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 34(38):2949–3003. http://eurheartj.oxfordjournals.org/content/ehj/33/6/734.full.pdf. Accessed Nov 14
Gianrossi R, Detrano R, Mulvihill D et al (1989) Exercise-induced ST Depression in the diagnosis of coronary artery disease: a meta-analysis. Circulation 80(1):87–98 (Accessed 16 Jan 2015)
Brown KA (1991) Prognostic value of thallium-201 myocardial perfusion imaging. A diagnostic tool comes of age. Circulation. 83(2):363–381. http://ac.els-cdn.com/S0735109707022073/1-s2.0-S0735109707022073-main.pdf?_tid=9ce2ef84-7704-11e4-b55c-00000aab0f6b&acdnat=1417182422_874e6937c9b40d49b2768310142cf72c. Accessed 28 Nov 2014
Muhlestein JB, Lappé DL, Lima JA et al (2014) Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA 312(21):2234–2243
Opolski MP, Kim WK, Liebetrau C, Walther C, Blumenstein J, Gaede L, Kempfert J, Van Linden A, Walther T, Hamm CW, Möllmann H (2015) Diagnostic accuracy of computed tomography angiography for the detection of coronary artery disease in patients referred for transcatheter aortic valve implantation. Clin Res Cardiol 104(6):471–480. doi:10.1007/s00392-014-0806-z
Waha S de, Eitel I, Desch S et al (2013) Diagnostik und Therapie der chronischen Myokardischämie. Rolle der kardialen Magnetresonanztomographie. Herz 38(4):350–358
Buckert D, Kelle S, Buss S, Korosoglou G, Gebker R, Birkemeyer R, Rottbauer W, Katus H, Pieske B, Bernhardt P (2017) Left ventricular ejection fraction and presence of myocardial necrosis assessed by cardiac magnetic resonance imaging correctly risk stratify patients with stable coronary artery disease: a multi-center all-comers trial. Clin Res Cardiol 106:219
Hussain ST, Morton G, De Silva K, Jogiya R, Schuster A, Paul M, Perera D, Nagel E (2016) The assessment of ischaemic burden: validation of a functional jeopardy score against cardiovascular magnetic resonance perfusion imaging. Clin Res Cardiol. doi:10.1007/s00392-016-1047-0
Petrov G, Kelle S, Fleck E, Wellnhofer E (2015) Incremental cost-effectiveness of dobutamine stress cardiac magnetic resonance imaging in patients at intermediate risk for coronary artery disease. Clin Res Cardiol 104(5):401–409. doi:10.1007/s00392-014-0793-0
Becker M, Hundemer A, Zwicker C, Altiok E, Krohn T, Mottaghy FM, Lente C, Kelm M, Marx N, Hoffmann R (2015) Detection of coronary artery disease in postmenopausal women: the significance of integrated stress imaging tests in a 4-year prognostic study. Clin Res Cardiol 104(3):258–271. doi:10.1007/s00392-014-0780-5
Gibbons RJ (2003) ACC/AHA 2002 guideline update for the management of patients with chronic stable angina–summary article: a report of the american college of cardiology/american heart association task force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina) Circulation. 107(1):149–158. http://circ.ahajournals.org/content/107/1/149.full.pdf+html. Accessed 27 Nov 2014
Gensini GG (1980) Coronary arteriography. In: Braunwald E (ed) Heart disease, pp 352–353. 1980. Philadelphia
Härle T, Zeymer U, Hochadel M, Zahn R, Kerber S, Zrenner B, Schächinger V, Lauer B, Runde T, Elsässer A (2017) Real-world use of fractional flow reserve in Germany: results of the prospective ALKK coronary angiography and PCI registry. Clin Res Cardiol 106:140
Reith S, Battermann S, Hellmich M, Marx N, Burgmaier M (2014) Impact of type 2 diabetes mellitus and glucose control on fractional flow reserve measurements in intermediate grade coronary lesions. Clin Res Cardiol 103(3):191–201. doi:10.1007/s00392-013-0633-7
Poerner TC, Duderstadt C, Goebel B, Kretzschmar D, Figulla HR, Otto S (2017) Fractional flow reserve-guided coronary angioplasty using paclitaxel-coated balloons without stent implantation: feasibility, safety and 6-month results by angiography and optical coherence tomography. Clin Res Cardiol 106:18
De Bono D (1993) Complications of diagnostic cardiac catheterisation: results from 34,041 patients in the United Kingdom confidential enquiry into cardiac catheter complications. Br Heart J. 70(3):297–300. http://www.ncbi.nlm.nih.gov.pubmedmitsfx.han.med.uni-magdeburg.de/pmc/articles/PMC1025320/. Accessed 1 Dec 2014
Sanz E, Steger JP, Thie W (1983) Cardiogoniometry. Clin Cardiol 6(5):199–206
Saner H, Baur HR, Sanz E, Gurtner HP (1983) Cardiogoniometry: a new noninvasive method for detection of ischemic heart disease. Clin Cardiol 6(5):207–210
Sanz E, Kinser J (1984) Die Kardiogoniometrie als Methode zur Diagnose der KHK. Vergleichsstudie mit der Myokardszintigraphie. Schweizerische Rundschau für Medizin Praxis =. Revue suisse de médecine Praxis 73(39):1169–1173
Meier A, Höflin F, Herrmann HJ, Wolf C, Gurtner HP, Rösler H (1987) Comparative diagnostic value of a new computerized vectorcardiographic method (cardiogoniometry) and other noninvasive tests in medically treated patients with chest pain. Clin Cardiol 10(5):311–316
Vontobel H, Schmid JJ, Steinbrunn W (1988) Kardiogoniometrie nach E. Sanz. Schweizerische medizinische Wochenschrift 118(44):1603–1608
Schüpbach, Michael WM, Emese B, Loretan P et al (2008) Non-invasive diagnosis of coronary artery disease using cardiogoniometry performed at rest. Swiss Med Wkly 138(15–16):230–238
Vontobel H, Tartini R, Steinbrunn W (1988) Kardiogoniometrie bei koronarer Herzkrankheit. Eine klinische Studie. Schweizerische medizinische Wochenschrift 118(44):1609–1611
Huebner T, Schuepbach, Michael WM, Seeck A et al (2010) Cardiogoniometric parameters for detection of coronary artery disease at rest as a function of stenosis localization and distribution. Med Biol Eng Compu 48(5):435–446
enverdis GmbH—Medical Solutions. CGM BASICS: Eine Einführung in die Cardiogoniometrie. http://www.enverdis.com. Accessed 1 Dec 2014
Einecke D. Hohes Versorgungsniveau bei Herzkatheter-Untersuchungen - SpringerMedizin. [basierend auf Herbsttagung der Deutschen Gesellschaft für Kardiologie und Jahrestagung der Arbeitsgruppe Rhythmologie vom 9.-11. Oktober in Düsseldorf]. 2014. http://www.springermedizin.de/dgk-2014-herbst_aktuelle-daten-zeigen-herzkatheter-interventionen-sind-in-deutschland-gut-und-sicher/5367442.html?linktyp=teaser2&newsletterID=13&sendID=17980&cm_mmc=ecircleNL-_-LM_Update+Kardiologie-_-S_DGK+bezieht+Position%3A+Welche+Herzklappe+f%C3%BCr+welchen+Patienten%3F-_-L_18. Accessed 14 Nov 2014
Patel MR, Peterson ED, Dai D et al (2010) Low diagnostic yield of elective coronary angiography. New Engl J Med 362(10):886–895. http://www.ncbi.nlm.nih.gov.pubmedmitsfx.han.med.uni-magdeburg.de/pmc/articles/PMC3920593/pdf/nihms540259.pdf. Accessed 16 Jan 2015
Law MR, Wald NJ, Morris JK, Jordan RE (2003) Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ (Clin Res ed) 326(7404):1427. (Accessed 21 Jan 2015)
van den Hoogen PC, Feskens EJ, Nagelkerke NJ, Menotti A, Nissinen A, Kromhout D (2000) The relation between blood pressure and mortality due to coronary heart disease among men in different parts of the world. Seven Countries Study Research Group. N Engl J Med 342(1):1–8 (Accessed 21 Jan 2015)
Emond M, Mock MB, Davis KB et al (1994) Long-term survival of medically treated patients in the coronary artery surgery study (CASS) registry. Circulation 90(6):2645–2657. http://circ.ahajournals.org/content/90/6/2645.long. Accessed 26 Nov 2014
Vijan S (2004) Pharmacologic lipid-lowering therapy in type 2 diabetes mellitus: background paper for the American College of Physicians. Ann Intern Med. 140(8):650. http://annals.org/article.aspx?articleid=717379. Accessed 21 Jan 2015
Erdmann E (2011) Klinische Kardiologie: Krankheiten des Herzens, des Kreislaufs und der herznahen Gefäße. 8., vollständig überarbeitete und aktualisierte Auflage. Springer, Berlin. SpringerLink: Bücher
Seeck A, Garde A, Schuepbach M et al (2009) Diagnosis of ischemic heart disease with cardiogoniometry: linear discriminant analysis versus support vector machines. [4th European Conference of the International Federation for Medical and Biological Engineering 2008. Vander Sloten J, Verdonck P, Marc Nyssen M, Haueisen J.IFMBE]. Springer, Berlin
Sanz E, Schüpbach M (2009) Cardiogoniometry: a non-invasive electrocardiographic method to diagnose ischemic heart disease at rest. GMDS: Medizinische Informatik, Biometrie und Epidemiologie 5(3). http://www.egms.de/static/en/journals/mibe/2009-5/mibe000099.shtml#Abstract. Accessed 2 Dec 2014
Huebner T, Goernig M, Schuepbach M et al (2010) Electrocardiologic and related methods of non-invasive detection and risk stratification in myocardial ischemia: state of the art and perspectives. German Med Sci GMS e-J 8:Doc27
Acknowledgements
The manufacturer of the Goniometry Device, Enverdis GmbH, supported the study with the Goniometry device free of charge.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no relationships that could be construed as a conflict of interest.
Rights and permissions
About this article
Cite this article
Weber, A., Smid, J., Luani, B. et al. Role of exercise cardiogoniometry in coronary artery disease diagnostics. Clin Res Cardiol 106, 573–581 (2017). https://doi.org/10.1007/s00392-017-1087-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1087-0