Abstract
Objectives
We aimed to investigate the diagnostic accuracy of a standardized computed tomography angiography (CTA) for the identification of significant coronary artery disease (CAD) in patients evaluated for transcatheter aortic valve implantation (TAVI).
Background
The diagnostic performance of CTA for the detection of CAD in patients with aortic stenosis referred for TAVI has thus far not been validated.
Methods
A consecutive series of 475 patients (194 male, mean age: 82 ± 6 years) with CTA data sets obtained during the routine diagnostic work-up before TAVI were included. A total of 6,603 coronary segments in 1,899 coronary arteries ≥1.5 mm in diameter and 271 grafts were evaluated for the presence of significant CAD defined as ≥50 % luminal narrowing. Results were compared with invasive coronary angiography as the standard of reference.
Results
Prevalence of significant CAD was 57 % (270/475), and 5,925 coronary segments (90 %) and 257 bypass grafts (95 %) were evaluable by CTA. In the per-patient analysis, sensitivity (Se), specificity, and positive and negative predictive values (NPV) were 98, 37, 67 and 94 %, respectively. CTA showed satisfactory ability to exclude significant CAD in the following subgroups: (1) patients (221/475) without prior known CAD (Se: 97 %, NPV: 97 %), (2) patients (13/475) without prior known CAD and absent coronary calcification (NPV: 100 %) and (3) bypass grafts (Se: 97 %, NPV: 99 %).
Conclusions
Comprehensive evaluation of a pre-TAVI CTA could prove to be a useful rule-out test for significant CAD in selected subgroups of patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transcatheter aortic valve implantation (TAVI) is accepted as a valuable treatment option for patients with severe aortic valve stenosis and a high peri-operative risk for open heart surgery [1]. Among the imaging modalities available for the evaluation of patients prior to TAVI, computed tomography angiography (CTA) plays a central role in patient selection and procedural planning by providing accurate information on the aortic dimensions for appropriate prosthesis sizing, selection of the best fluoroscopic projection angles, and evaluation of the peripheral access vessels [2, 3]. To acquire all of this information in a single CTA examination, a large anatomical volume needs to be covered using standardized imaging protocols. A recent expert consensus document endorses a comprehensive evaluation of all concomitant findings obtained from the CTA data [3].
In the diagnostic work-up of patients evaluated for TAVI, a pre-procedural assessment of coronary artery disease (CAD) is mandatory to determine both the baseline risk characteristics and the need for coronary revascularization [4]. Currently, invasive coronary angiography (ICA) remains the gold standard diagnostic modality for the detection of significant CAD in patients scheduled for TAVI; however, it still carries a non-negligible risk for catheter-related complications as well as increased contrast dye use, both of which should be of special concern in the frail TAVI population. Until now, there is very limited data on the potential application of pre-procedural CTA for the detection of CAD before TAVI [5]. We, thus, retrospectively investigated the diagnostic accuracy of a standardized CTA for the identification of significant CAD as compared with the reference ICA in a large cohort of patients referred for TAVI at a single, high-volume institution.
Materials and methods
Study design and population
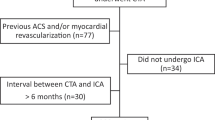
From January 2011 to November 2013, a consecutive series of 645 patients with severe aortic stenosis were referred for a standard diagnostic work-up, of which 510 met the study inclusion criteria of both CTA and ICA data availability. In all patients CTA was performed within 4 weeks of ICA. Of 510 available patients, we excluded 35 patients (7 %) due to potentially preventable technical and/or human-related factors encountered during the CTA examination (such as significant patient movements or contrast extravasation) resulting in significant motion artifacts in 21 cases (4 %) and poor contrast opacification in 14 cases (3 %), and thus precluding reliable evaluation of most coronary segments. The final analysis was, thus, performed on 475 patients. Patients with arrhythmias, including atrial fibrillation and pacemaker-dependent rhythm, were not excluded, and no additional medications for heart rate (HR) control and/or vasodilation were administered prior to the CTA scan. All clinical data were documented in a prospective database according to local site protocol and patient risk stratification was determined using the logistic European System for Cardiac Operative Risk Evaluation [6]. The study was approved by the institutional ethics committee, and all participants gave written informed consent.
CTA acquisition and image reconstruction
All scans were performed using a dual-source scanner (Somatom Definition, Siemens, Erlangen, Germany). All CTA measurements were performed using an electrocardiogram-gated retrospective acquisition protocol at the level of the heart and aortic root with a second non-gated acquisition covering the remaining aorta and iliofemoral arteries. Contrast-enhanced scans were obtained by administration of 80–120 ml iodinated contrast material through an antecubital vein at a rate of 4 ml/s followed by a bolus of 50 ml isotonic saline. Scan timing was coordinated by peak enhancement detection with a region of interest in the ascending aorta. After coronary artery bypass grafting (CABG), the scanning range routinely included the entire course of all venous and arterial grafts. Scan parameters were: tube voltage 120 kV, tube current 320–400 mAs/rotation, and gantry rotation time 330 ms. Scan data were reconstructed in end-systole and end-diastole (30–40 % and 60–70 % of the R–R interval). The slice thickness was 0.6 mm. The mean dose length product was 2,336 ± 1,036 mGy cm.
CTA data analysis
All reconstructed images were evaluated offline using a dedicated workstation (Leonardo Workstation, Siemens, Erlangen, Germany). One experienced cardiologist who was blinded to angiographic findings analyzed all coronary segments with the use of curved multiplanar reconstructions and thin-slab maximum intensity projections in two phases of the cardiac cycle. In patients with prior CABG, the observer was aware of the surgical report specifying the type and location of bypass grafts. Each coronary segment or graft was described as interpretable or not. If interpretable, all coronary segments with a diameter ≥1.5 mm were visually evaluated for the presence of occlusions (100 %), or significant stenoses defined as a lumen reduction of ≥50–99 % according to the 18-segment coronary model of the Society of Cardiovascular Computed Tomography [7]. Segmental coronary calcification was ranked as absent, moderate (isolated calcium spots and calcification covering <50 % of lumen in cross section), or severe (extensive calcification covering ≥50 % of lumen in cross section) as previously described [8]. In case of a jump graft (≥2 anastomoses per graft), all graft segments between the proximal anastomoses and each coronary insertion were analyzed separately [9]. Grafted coronary segments were defined as all segments located proximally to the segment of graft insertion, while distal runoffs included the segment at which the graft was inserted and all segments located distally to graft insertion [10]. Coronary arteries or grafts with stents were not excluded. The interobserver variability was assessed by a second experienced reader in 20 % of randomly selected patients.
Coronary angiography
ICA was performed using a standard angiography system (Axiom Artis, Siemens, Germany) and served as the reference for comparison with CTA. All standard views for native coronary arteries and at least two orthogonal views for each graft were obtained. Angiograms were evaluated by two highly experienced cardiologists blinded to the CTA data. Lesions with a lumen reduction of ≥50 % by visual assessment were considered to represent significant stenoses. All coronary or graft segments located distally to a total occlusion (100 % lumen reduction) and not supplied by collaterals were excluded from analysis [10].
Statistical analysis
Continuous variables were reported as means ± standard deviations, and categorical variables were expressed as frequencies and percentages. The diagnostic performance of CTA for the detection of significant CAD in comparison with that of ICA was expressed as sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and positive and negative likelihood ratios with corresponding 95 % confidence intervals. Analyses were performed on a (1) per-segment basis comparing each segment in every native coronary artery, (2) per-vessel basis evaluating the presence of significant stenoses in each major coronary artery, and (3) per-patient basis. In the per-segment analyses, segments classified as non-diagnostic were excluded. In the per-vessel and per-patient analyses the presence of at least one non-diagnostic coronary segment was classified as a positive finding (because the stenosis could not be ruled out by CTA and ICA would be necessary) as previously described [11]. In patients with prior CABG, per-patient analysis assessed the presence of any significant stenosis in a combination of bypass grafts, non-grafted coronary arteries, and distal runoffs in a given patient [12]. The medians of HR and the body-mass-index (BMI) were calculated to subdivide patients into separate groups. The differences in diagnostic accuracies between groups were tested for significance by using a χ 2 test with Yates correction for comparison of cross tables. Because the same patients were assigned to three different groups and compared three times each in relation with BMI, HR, and the burden of calcification, the Bonferroni method was used to account for the increased probability of experiment-wise Type I error. Thus, the α-level of 0.05 was corrected for three planned comparisons with a statistical significance level of <0.016 for two-sided probability values. Interobserver variability for the detection of significant stenoses was determined by Cohen’s κ coefficient. Statistical analyses were performed with SPSS 20.0 (SPSS Inc., Chicago, IL, USA) and using the VassarStats website for statistical computation.
Results
Baseline characteristics and CTA feasibility
Patient characteristics and scan demographics are listed in Table 1. The mean BMI was 27.5 ± 5.1 kg/m2 (range 16.8–45.5 kg/m2), and the mean HR during CTA was 74 ± 12 beats/min (range 36–123 beats/min). Ten patients (2 %) had HR above 100 beats/min.
Of the potential 8,550 coronary segments in 475 patients, 1,222 segments were absent due to their chance occurrence in the 18-segment coronary model, while 531 segments with a diameter <1.5 mm, and 194 segments distal to 156 complete vessel occlusions were excluded. Thus, potentially 6,603 assessable coronary segments remained in the analysis. Of these, 678 segments (10 %) were classified as non-diagnostic by CTA due to: the presence of severe calcification with beam hardening artifacts in 261 segments (4 %), low-contrast opacification in 163 segments (2 %), motion artifacts in 141 segments (2 %), and stent artifacts in 113 segments (2 %) (Fig. 1). The final statistical analysis was, thus, performed on 5,925 comparable segments. Non-diagnostic segments were most commonly present in the right coronary artery (RCA) (262/2,083; 13 %) and less often in the left anterior descending artery (LAD) (216/2,092; 10 %), left circumflex (LCX) (174/1,954; 9 %), and left main (26/474; 5 %). Non-diagnostic segments were found in 259 patients (54 %), of which 31 post-CABG patients (7 %) showed non-conclusive CTA images restricted to grafted coronary segments only; therefore, not influencing the per-patient analysis assessed for the combination of bypass grafts, non-grafted coronary arteries and distal runoffs (because the presence of a stenosis in a grafted coronary segment located proximally to the graft insertion would not affect the decision on coronary angiography). Thus, non-diagnostic CTA was present in 228 patients (47 %), whereas the remaining 247 patients (53 %) showed interpretable CTA data on a per-patient analysis.
Most common computed tomographic artifacts—curved multiplanar reconstruction displaying severe calcification (yellow asterisk) in the left main and proximal segments of the left anterior descending artery (a). Curved multiplanar reconstruction showing significant motion artifacts (yellow asterisk) in the proximal right coronary artery (b). Curved multiplanar reconstruction of non-diagnostic stent (yellow asterisk) in the proximal right coronary artery (c)
Prevalence of CAD
On the basis of ICA, 5,134 (87 %) segments were free of stenosis; while the remaining 791 (13 %) segments presented with significant CAD. Overall significant CAD was present in 270 of 475 patients (57 %). Coronary stenosis was most commonly present in the LAD (227/475; 48 %) and less often in the RCA (192/475; 40 %), LCX (167/475; 35 %), and left main (39/474; 8 %).
Accuracy of CTA for detection of CAD
Agreement between observers for the evaluation of significant CAD on a per-segment (κ value 0.66) and per-patient levels (κ value 0.67) was good. On a per-segment basis, 4,097 of 5,134 stenoses (80 %) were correctly ruled out by CTA; whereas in 1,037 cases, false-positive findings were observed. The presence of significant CAD was correctly recognized in 638 of 791 segments (81 %), while 153 lesions were underestimated using CTA. In the per-patient analysis, CTA correctly identified at least 1 significant stenosis in 265 of 270 patients (98 %), while diagnosis was missed in 5 patients (2 %). Of 205 patients without stenoses, the presence of significant CAD was correctly ruled out in 76 patients (37 %); whereas in 129 patients (63 %), false-positive findings were observed. Thus, for the detection of significant CAD on a per-patient basis, a sensitivity of 98 % (265/270), specificity of 37 % (76/205), PPV of 67 % (265/394), and NPV of 94 % (76/81) were found. Accuracy of CTA on a per-segment, per-vessel, and per-patient basis is shown in Table 2.
Influence of BMI, HR, and coronary calcium on accuracy of CTA
The medians of BMI and HR were 26.8 kg/m2 and 71 beats/min, respectively. Non-diagnostic segments were present in 8 % of segments (285/3,398) in patients with a BMI ≤26.8 kg/m2, and in 12 % of segments (393/3,205) in patients with a BMI >26.8 kg/m2 (p < 0.001). Non-diagnostic segments were present in 10 % of segments (337/3,342) in patients with a HR ≤71 beats/min, and in 10 % of segments (341/3,261) in patients with a HR >71 beats/min (p = 0.647). Diagnostic accuracies in the segment-based analysis were comparable in both BMI and HR subgroups (χ 2 = 3.48, p = 0.062 and χ 2 = 0.1, p = 0.752, respectively). Absent, moderate, and severe calcifications were observed in 2,648 (45 %), 1,947 (33 %), and 1,330 (22 %) diagnostic coronary segments, respectively. The accuracies were 97, 84, and 41 % in segments with absent, moderate, and severe calcifications, respectively (Fig. 2), and reached the level of significance for subgroup comparison (χ 2 = 1,723, p < 0.001, Table 3).
Conclusive computed tomographic images—curved multiplanar reconstructions of the non-stenotic and non-calcified left anterior descending artery, left circumflex, and right coronary artery (a–c). Corresponding invasive coronary angiography findings (d–f). LAD left anterior descending artery, LCX left circumflex, RCA right coronary artery
Accuracy of CTA after CABG
Overall, 257 of 271 graft segments (95 %) were evaluable by CTA. Of the 14 non-diagnostic graft segments (5 %), four segments (1 %) were located in the left internal mammary artery; whereas ten segments (4 %) were found in venous grafts. Non-diagnostic graft segments were most commonly due to the presence of metallic clip artifacts (5 grafts) and followed by motion artifacts (4 grafts), stent artifacts (3 grafts), and poor contrast opacification (2 grafts). According to ICA, 223 (87 %) bypass grafts were patent and non-stenotic, while the remaining 34 (13 %) presented with either complete occlusion (28 grafts, 11 %) or significant stenosis (6 grafts, 2 %). The presence of significant stenosis or occlusion was correctly recognized in 33 of 34 grafts (97 %), while one very short and membranous-like stenosis located at the distal anastomotic site of the left internal mammary artery graft to the LAD was underestimated using CTA. Of the patent and non-stenotic grafts, 210 of 223 (94 %) stenoses were correctly ruled out by CTA (Fig. 3); whereas in 13 cases, false-positive findings were observed. Overall, the accuracy of CTA for the detection of significant graft disease was 95 %, with an average of 97 and 93 % in arterial and venous grafts, respectively. Additionally, four grafts in four patients were not demonstrated by ICA but were accurately detected by CTA and found to be widely patent: two arterial grafts of the right internal mammary artery grafted to the first marginal branch and the distal RCA, and two venous grafts originating from the lateral part of the aortic arch that were grafted to the RCA and the LAD. If analysis was restricted to non-grafted and distal runoff segments, a total of 472 of 558 coronary segments (85 %) were evaluable by CTA; whereas 13 of 235 runoffs (5 %) and 73 of 323 non-grafted segments (23 %) were non-diagnostic. The accuracy of CTA for the detection of significant CAD in distal runoffs and in a combination of non-grafted and distal runoff segments was 86 and 80 %, respectively (Table 4).
Computed tomography images of bypass grafts—curved multiplanar reconstruction of the patent and non-stenotic left internal mammary artery graft to the left anterior descending artery confirmed by the corresponding invasive coronary angiography (a, b). Curved multiplanar reconstruction of the patent and non-stenotic venous jump graft to the first obtuse marginal branch confirmed by the corresponding invasive coronary angiography (c, d). LAD left anterior descending artery, LIMA left internal mammary artery, OM obtuse marginal branch, SVG saphenous vein graft
Accuracy of CTA in patients with and without prior CAD
Patients without prior known CAD showed significantly less non-diagnostic coronary segments (113/3,135; 4 %) compared with patients with prior CAD (565/3,468; 16 %, p < 0.001). Among patients without prior known CAD, CTA correctly identified 74 of 76 patients (97 %) with at least one significant lesion on ICA, while diagnosis was underestimated in two patients (3 %). In the subgroup of patients (13/475; 3 %) without prior CAD and absent coronary calcification, the presence of significant CAD was correctly ruled out in 11 of all 13 (85 %) subjects by CTA; whereas in two patients, false-positive findings were obtained. Table 5 summarizes the accuracy of CTA as a function of the presence or absence of prior known CAD on a per-patient basis.
Discussion
The present study investigated the diagnostic accuracy of pre-procedural CTA for the detection of significant CAD in a large, unselected cohort of TAVI patients. Our findings demonstrate that the limited feasibility and the overall moderate accuracy (driven by the high rate of false-positive observations) of a pre-TAVI CTA for the identification of significant CAD preclude its general use as a surrogate test for the ICA. However, comprehensive evaluation of a pre-TAVI CTA could prove to be a useful rule-out test for significant CAD in some selected clinical scenarios including the assessment of bypass grafts, and patients without prior known CAD, particularly in the absence of coronary calcification.
Feasibility and accuracy of CTA for the detection of CAD
The pre-procedural assessment of CAD is required to determine both the baseline risk characteristics and the need for coronary revascularization in the TAVI population [4]. Currently, ICA remains the gold standard for the identification of CAD before TAVI; however, it still carries a non-negligible risk for contrast-induced nephropathy that should be of special concern in the frail TAVI population [13, 14]. Thus, assuming availability of CTA data as a part of a routine diagnostic work-up before TAVI, implementation of a non-invasive CTA as a reliable rule-out test for significant CAD should have a relevant safety priority in this population. Further, the ability of planning ICA and/or percutaneous coronary intervention based on CTA data sets in case of a positive observation is clearly advantageous with regard to shortening the procedural time and limiting the use of contrast dye. To date, the utility of CTA for the identification of significant CAD in patients with severe aortic stenosis has been investigated almost exclusively prior to open heart surgery [15–18]. Most of these studies using 64-detector CTA technology were limited to a small number of highly selected patients and reported variable sensitivities between 68 and 100 % with specificities between 81 and 91 % for the detection of significant CAD. Of note, despite strict patient selection criteria and frequent beta-blocker administration before CTA scan, up to 25 % of the CTA images were found to be not fully evaluable. Further, it should be noted that patients with aortic stenosis undergoing conventional open heart surgery have significantly fewer comorbidities, including lower prevalence of CAD, compared with the high-risk TAVI population, which might further contribute to reduced CTA feasibility and diagnostic performance in the latter. In the only study assessing the diagnostic accuracy of a standardized CTA for the detection of significant CAD in 60 highly selected TAVI candidates, Pontone et al. [5] reported a feasibility of 87 % with sensitivity, specificity, and NPV of 88, 88, and 91 %, respectively. In our study, the feasibility of CTA was 53 % with the per-patient sensitivity, specificity, and NPV of 98, 37, and 94 %, respectively. This corresponds well with the moderate diagnostic accuracy obtained by Pontone et al., further substantiating the additional need for ICA to confirm or refute CTA findings in most TAVI candidates. Contrary to the report of Pontone et al., our study included a large number of unselected TAVI candidates (without excluding patients with arrhythmias, high HR, and stents), resulting in a reduced feasibility of CTA and thus a higher frequency of false-positive observations with lower specificity on a per-patient basis. However, our study thereby much better reflects daily clinical routine.
The inclusion of “all-comers” in our analysis allowed a broad-spectrum assessment of the diagnostic performance of a pre-TAVI CTA in various clinical scenarios, including subgroup comparison and identification of target populations yielding the highest CTA applicability. Indeed, by demonstrating satisfactory sensitivity (97 %) and NPV (97 %) for the exclusion of significant CAD in patients without prior known CAD, we suggest that ICA might be avoided in this subgroup of patients on condition that CTA result is negative. Moreover, provided that coronary calcification is the major confounding factor precluding sufficient image interpretation by CTA [19], we demonstrated excellent NPV (100 %) for a pre-TAVI CTA for the exclusion of significant CAD in the subgroup of patients without prior CAD and no coronary calcification. Another TAVI subpopulation that might benefit from application of CTA includes patients after CABG who showed high sensitivity (97 %) and NPV (99 %) for CTA for the exclusion of significant graft disease with good feasibility (95 %) for conclusive graft evaluation. Similar to Jabara et al. [20], we demonstrated a clear advantage of CTA over ICA in the detection of technically challenging bypass grafts with failed visualization on ICA. However, as the diagnostic work-up of post-CABG patients should include both the assessment of bypass grafts and native coronary vessels, the reduced diagnostic accuracy and feasibility of a pre-TAVI CTA in native coronary circulation after CABG cannot fully justify obviating the need for ICA. Despite this, for non-invasive exclusion of significant graft disease, CTA might serve as a gatekeeper for prolonged ICA by guiding and/or omitting selective graft cannulation.
Influence of BMI, HR, and coronary calcium on accuracy of CTA
The concept of an ideal diagnostic test for reliable exclusion of CAD presumes that the entire coronary artery tree can be imaged with a diagnostic image quality and no segment must be excluded from analysis. We, thus, investigated the influence of calcium load, BMI, and HR on CTA feasibility and diagnostic accuracy. In all, we found a total of 10 % non-diagnostic coronary segments in our cohort, most of which were caused by calcium artifacts. Similar to prior study on coronary CTA [11], we showed a significant deterioration in diagnostic accuracy for a higher calcium load. Large calcified plaques result in a virtual increase of plaque volume, and thus, may obscure the coronary lumen representing the main contributor to stenosis overestimation and false-positive findings [21]. Moreover, we showed a significantly higher rate of non-conclusive coronary segments on CTA in patients with higher BMI (12 %) when compared with patients with lower BMI (8 %). This deterioration of diagnostic feasibility might be explained by scattering and absorption of the radiation beam in obese patients, resulting in an increase in image noise and decrease in signal-to-noise ratio reflected by poor vessel opacification [22]. In contrast, we did not observe a relevant influence of BMI on the accuracy of CTA in evaluable coronary segments. Finally, there were no differences regarding the number of non-diagnostic coronary segments or diagnostic accuracy of CTA in patients with high and low HR, as in the prior study performed among patients with suspected CAD [23].
Study limitations
Our study has some limitations. First, the reported study was a single-center observational experience. Nevertheless, by performing CTA in a large number of unselected TAVI patients our results represent a realistic clinical diagnostic applicability of a pre-TAVI CTA without significant patient selection bias. Second, because of the retrospective nature of our study, it was not our intention to enhance the diagnostic performance of pre-TAVI CTA for the detection of CAD by providing dedicated contrast injection or reconstruction protocols and improving patient preparation via heart rhythm control and rehearsal of the breath-holding instructions. Further, we believe that the new-generation computed tomography scanners with improved temporal and spatial resolution should significantly reduce the number of motion- and calcium-related artifacts, and thus, improve the diagnostic feasibility of pre-TAVI CTA. Third, stenosis assessment was restricted to visual estimation, and no automated quantification of the degree of stenosis was performed. Finally, we performed a qualitative rather than quantitative coronary calcium assessment due to the reduced feasibility of accurate calcium scoring calculation in patients after coronary revascularization.
Conclusions
The limited feasibility and the overall moderate accuracy of CTA for the identification of significant CAD preclude its common use as a surrogate test for ICA in patients evaluated for TAVI. However, pre-TAVI CTA may be a potentially valuable alternative to ICA for non-invasive exclusion of significant CAD in selected subgroups of patients, including patients without prior known CAD and patients with bypass grafts. Our study, therefore, emphasizes the relevance of a comprehensive CAD evaluation based on CTA data sets obtained during the routine diagnostic work-up of TAVI patients.
References
Haussig S, Schuler G, Linke A (2014) Worldwide TAVI registries: what have we learned? Clin Res Cardiol 103(8):603–612. doi:10.1007/s00392-014-0698-y
O’Sullivan CJ, Stortecky S, Buellesfeld L, Wenaweser P, Windecker S (2014) Preinterventional screening of the TAVI patient: how to choose the suitable patient and the best procedure. Clin Res Cardiol 103(4):259–274. doi:10.1007/s00392-014-0676-4
Achenbach S, Delgado V, Hausleiter J, Schoenhagen P, Min JK, Leipsic JA (2012) SCCT expert consensus document on computed tomography imaging before transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR). J Cardiovasc Comput Tomogr 6(6):366–380. doi:10.1016/j.jcct.2012.11.002
Abdel-Wahab M, Zahn R, Horack M et al (2012) Transcatheter aortic valve implantation in patients with and without concomitant coronary artery disease: comparison of characteristics and early outcome in the German multicenter TAVI registry. Clin Res Cardiol 101(12):973–981. doi:10.1007/s00392-012-0486-5
Pontone G, Andreini D, Bartorelli AL et al (2011) Feasibility and accuracy of a comprehensive multidetector computed tomography acquisition for patients referred for balloon-expandable transcatheter aortic valve implantation. Am Heart J 161(6):1106–1113. doi:10.1016/j.ahj.2011.03.003
Roques F, Michel P, Goldstone AR, Nashef SA (2003) The logistic EuroSCORE. Eur Heart J 24(9):881–882
Raff GL, Abidov A, Achenbach S et al (2009) SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr 3(2):122–136. doi:10.1016/j.jcct.2009.01.001
Nazeri I, Shahabi P, Tehrai M, Sharif-Kashani B, Nazeri A (2009) Assessment of patients after coronary artery bypass grafting using 64-slice computed tomography. Am J Cardiol 103(5):667–673. doi:10.1016/j.amjcard.2008.10.040
Kepka C, Opolski M, Kruk M et al (2012) Diagnostic accuracy of dual-source coronary computed tomography angiography in patients after bypass grafting. Postep Kardiol Inter 3(29):183–192. doi:10.5114/pwki.2012.30396
Weustink AC, Nieman K, Pugliese F et al (2009) Diagnostic accuracy of computed tomography angiography in patients after bypass grafting: comparison with invasive coronary angiography. JACC Cardiovasc Imaging 2(7):816–824. doi:10.1016/j.jcmg.2009.02.010
Alkadhi H, Scheffel H, Desbiolles L et al (2008) Dual-source computed tomography coronary angiography: influence of obesity, calcium load, and heart rate on diagnostic accuracy. Eur Heart J 29(6):766–776. doi:10.1093/eurheartj/ehn044
Ropers D, Pohle FK, Kuettner A et al (2006) Diagnostic accuracy of noninvasive coronary angiography in patients after bypass surgery using 64-slice spiral computed tomography with 330-ms gantry rotation. Circulation 114(22):2334–2341
Bell RM, Rear R, Cunningham J, Dawnay A, Yellon DM (2014) Effect of remote ischaemic conditioning on contrast-induced nephropathy in patients undergoing elective coronary angiography (ERICCIN): rationale and study design of a randomised single-centre, double-blind placebo-controlled trial. Clin Res Cardiol 103(3):203–209. doi:10.1007/s00392-013-0637-3
Seiffert M, Sinning JM, Meyer A et al (2014) Development of a risk score for outcome after transcatheter aortic valve implantation. Clin Res Cardiol 103(8):631–640. doi:10.1007/s00392-014-0692-4
Gilard M, Cornily JC, Pennec PY et al (2006) Accuracy of multislice computed tomography in the preoperative assessment of coronary disease in patients with aortic valve stenosis. J Am Coll Cardiol 47(10):2020–2024
Meijboom WB, Mollet NR, Van Mieghem CA et al (2006) Pre-operative computed tomography coronary angiography to detect significant coronary artery disease in patients referred for cardiac valve surgery. J Am Coll Cardiol 48(8):1658–1665
Stagnaro N, Della Latta D, Chiappino D (2009) Diagnostic accuracy of MDCT coronary angiography in patients referred for heart valve surgery. Radiol Med 114(5):728–742. doi:10.1007/s11547-009-0403-9
Larsen LH, Kofoed KF, Dalsgaard M et al (2013) Assessment of coronary artery disease using coronary computed tomography angiography in patients with aortic valve stenosis referred for surgical aortic valve replacement. Int J Cardiol 168(1):126–131. doi:10.1016/j.ijcard.2012.09.057
Vanhecke TE, Madder RD, Weber JE, Bielak LF, Peyser PA, Chinnaiyan KM (2011) Development and validation of a predictive screening tool for uninterpretable coronary CT angiography results. Circ Cardiovasc Imaging 4(5):490–497. doi:10.1161/CIRCIMAGING.111.964205
Jabara R, Chronos N, Klein L et al (2007) Comparison of multidetector 64-slice computed tomographic angiography to coronary angiography to assess the patency of coronary artery bypass grafts. Am J Cardiol 99(11):1529–1534
Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA (2005) Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol 46(3):552–557
Husmann L, Leschka S, Boehm T et al (2006) Influence of body mass index on coronary artery opacification in 64-slice CT angiography. Rofo 178(10):1007–1013
Scheffel H, Alkadhi H, Plass A et al (2006) Accuracy of dual-source CT coronary angiography: first experience in a high pre-test probability population without heart rate control. Eur Radiol 16(12):2739–2747
Acknowledgments
We thank Elizabeth Martinson, Ph.D., for her help in editing this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. P. Opolski and W.-K. Kim contributed equally to this work.
Rights and permissions
About this article
Cite this article
Opolski, M.P., Kim, WK., Liebetrau, C. et al. Diagnostic accuracy of computed tomography angiography for the detection of coronary artery disease in patients referred for transcatheter aortic valve implantation. Clin Res Cardiol 104, 471–480 (2015). https://doi.org/10.1007/s00392-014-0806-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-014-0806-z