Abstract
Background
Cardiac magnetic resonance imaging (CMR) has become a diagnostic modality that allows for prognostic risk stratification in various cardiac diseases. CMR derived detection of myocardial necrosis by late gadolinium enhancement (LGE) and assessment of left ventricular functional parameters such as left-ventricular ejection fraction (LVEF) have been proven to be significantly associated with outcome and prognosis. Our study focusses on the validation of specific thresholds for these parameters in a multi-center daily all-comers cohort of stable coronary artery disease (CAD) patients.
Methods
Multi-center data from tertiary high-volume CMR centers were pooled. Patients referred for viability testing for known or suspected CAD were enrolled. Functional parameters of both ventricles and myocardial necrosis were assessed. The primary endpoint was defined as cardiac death and non-fatal myocardial infarction. A multi-model approach was used for the evaluation of the predictive power of several LVEF thresholds and LGE.
Results
The study cohort consisted of 2422 patients. Median age was 66 years; 25.9 % were female. Median follow-up was 2.86 years. During the follow-up period, 187 primary endpoints occurred. On multi-model testing, optimal thresholds for LVEF could be defined at ≤50 and ≤35 %. The addition of LGE as categorical variable further lead to a significant improvement of each risk prediction model, whilst quantification of LGE affection had no additional prognostic impact.
Conclusion
LVEF thresholds at ≤50 and ≤35 % in combination with the assessment of LGE presence allows for excellent discrimination between low, mid and high prognostic risk in stable CAD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiac magnetic resonance imaging (CMR) has become a diagnostic modality of choice for good risk stratification of patients with various cardiac diseases, including coronary artery disease (CAD) [1, 2]. Especially, CMR derived detection of myocardial necrosis by late gadolinium enhancement (LGE) has been proven to be significantly associated with major cardiovascular endpoints and poor prognosis [3, 4]. In patients suffering from ventricular tachycardia, LGE detection has substantial influence on the choice of the ablation strategy as well as on the probability of success [5]. Recently, the cost-effectiveness of CMR in the management of CAD patients could also be demonstrated [6]. There are recent meta-analyses trying to clarify the exact role of this parameter in terms of risk stratification and prognosis prediction, though there is a certain inhomogeneity throughout the studies that form the evidence base. Most of them are single-center studies with varying definitions of study populations and endpoints, which hinders comparison to a certain extent [7].
Furthermore, CMR is considered the gold standard for evaluation and quantification of left ventricular function and ejection fraction (LVEF) [8]. LVEF is known to be one of the strongest parameters regarding outcome and prognosis. Several studies sought to determine age and gender specific normal values of LVEF [9]. They report a lower limit for normal LVEF from 49 to 55 %, which results in a relatively large “grey zone” [9]. Again, these values are mainly derived from single-center studies with less than 100 subjects per group and are not specifically validated in large all-comers CAD cohorts [10].
Aim of the present study was to validate prognostic thresholds for LVEF in a routine all-comers cohort of stable CAD patients. We ought to analyze the potential additional prognostic impact of LVEF and LGE when combined with traditional risk factors. Therefore, multi-center data of high volume tertiary CMR centers were pooled and analyzed.
Methods
Patients
The present study contains patient data from three tertiary high volume CMR centers (University Hospital Ulm, University Hospital of Heidelberg, German Heart Center Berlin). Data was collected from 2000 to 2007. The study is a retrospective analysis of patients consecutively referred for viability testing by CMR imaging for known or suspected CAD. All subjects were considered eligible for enrollment unless they exhibited predefined exclusion criteria such as cardiac or respiratory instability, concomitant limiting disease (e.g. cancer, high grade heart valve disease, pulmonary disease), pregnancy, inability to give informed consent, age <18 years, or myocardial infarction within the last 3 months. In- and exclusion criteria were the same at each site. All patients gave written informed consent. The institutional ethics committee of each CMR site approved the study, respectively.
CMR study
In all centers, CMR imaging was performed on a 1.5-T whole body clinical magnetic resonance scanner (Intera; Philips Medical Systems, Best, The Netherlands) using a cardiac five-element phased-array receiver coil.
For functional imaging, the heart was covered from apex to base in contiguous short-axis orientation using a steady-state free precession sequence. LGE images were acquired approximately 10–15 min after a bolus injection of gadolinium based contrast agent with an inversion-recovery gradient-echo sequence. Sequence details have been published previously [2, 11, 12].
CMR analysis
A cine short-axis stack was acquired in each patient. Epi- and endocardial contours were drawn manually. Volumetric end-diastolic and end-systolic left and right ventricular volumes and ejection fractions were assessed in every patient using the standard software provided by the manufacturer (ViewForum®, Philips Medical Systems, Best, The Netherlands) [13, 14]. Two experienced readers in consensus assessed myocardial necrosis visually at each site.
In a subgroup of patients, assessment of regional wall motion and number of LGE affected myocardial segments was performed. According to a recommended wall motion score, each myocardial segment was scored as normal or hyperkinetic = 1, hypokinetic = 2, akinetic = 3, dyskinetic = 4 or aneurysmal = 5 [15]. Wall motion score was expressed as sum as well as normalized to the number of segments. Analogously, the numbers of LGE affected segments were reported.
Follow-up
Follow-up information was acquired from patients’ interviews by telephone or from outpatient clinics, hospital chart reviews or by contact with the patients’ general practitioner or hospital. Primary endpoint was defined as cardiac death or non-fatal myocardial infarction. Cardiac death was defined as death from any cardiac cause (e.g. myocardial infarction, ventricular fibrillation or other lethal arrhythmia, heart failure) and sudden non-explainable death. Non-fatal myocardial infarction was defined according to the current universal definition [16]. An endpoint was considered early when it took place within 45 days after baseline examination. Patients were censored at the occurrence of the first primary event.
Statistical analysis
To test the relationship between two categorical classification factors, the Chi squared test was applied.
Continuous variables were tested for normal distribution by the D’Agostino–Pearson test. In case a normal distribution was given, variables were reported as mean ± standard deviation and a two-tailed t test was applied for comparison. Variables without normal distribution were reported as median with percentiles and compared by the Mann–Whitney rank sum test.
Univariate regression analyses using Cox’s proportional hazard models were performed to estimate the predictive value of the variables. Hazard ratio (HR) and corresponding 95 % confidence interval (CI) are provided.
To test for incremental predictive power, following approach was applied: Multivariate models based on the results of univariate testing were defined and compared. Chi-square values were calculated with Cox’s proportional hazard overall model fit. Integrated discrimination index and net reclassification index were assessed as well. In case of a significant increase in these variables, a particular model was judged superior [17]. Cumulative event curves were compared by the Kaplan–Meier method using a log-rank test.
Thresholds for the continuous parameter LVEF were defined to create categorical variables. To yield optimal thresholds with regard to risk prediction, we calculated statistical significance, hazard ratios and corresponding annual event rates.
Overall, a p value ≤0.05 was judged significant. Statistical analysis was performed using commercially available software (Stata13, College Station, USA, MedCalc, Mariakerke, Belgium).
Results
Patients
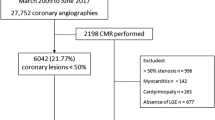
A total of 2501 patients were screened for enrollment, 56 had to be excluded due to insufficient image quality (2.2 %). Of the remaining 2444 patients, 20 cases were lost to follow-up. Thus, the study cohort consisted of 2422 subjects. The University Hospital of Ulm included 502 patients; the German Heart Center Berlin included 153 patients; the University Hospital of Heidelberg enrolled 1767 patients.
Median age was 66.0 (41.2; 82.1) years, 627 (25.9 %) of the patients were women. Median follow-up was 2.86 (0.85; 5.63) years. Clinical and demographic patients’ characteristics, including cardiovascular risk factors and prior cardiac events, are provided in Table 1.
CMR results
There were no major complications in association with CMR examinations. Median left ventricular end-diastolic volume (LVEDV) was 156 ml (98; 263); median left ventricular ejection fraction (LVEF) was 61.0 % (32.0 %; 75.2 %), LGE was seen in 1182 (48.8 %) cases.
In a subgroup of 655 patients, median wall motion score at rest was 18 (17; 38), median normalized wall motion score was 1.06 (1.0; 2.4). LGE was present in 351 (53.8 %) cases, median number of LGE affected segments were 1 (0; 8), median normalized LGE affection was 0.059 (0; 0.47). Table 1 shows CMR results in more detail.
Univariate prediction of primary endpoint
During the follow-up period, 187 primary endpoints occurred (over-all event rate 2.62 %). Only six endpoints (0.3 % of total events) happened within 45 days after baseline examination, and thus had to be considered early. Clinical features and CMR derived parameters were analyzed with regard to endpoint prediction. Results are depicted in Table 2. There were significant associations for age, sex, hypertension, hyperlipidemia, diabetes mellitus and previous revascularization. Concerning CMR derived parameters, LVEF and presence of LGE were variables with highly significant associations. Presence of LGE resulted in the highest hazard ratio of all evaluated variables (hazard ratio 3.29, p < 0.0001).
The subgroup analysis also revealed wall motion score and number of LGE affected segments to be significantly correlated with the occurrence of primary endpoints (hazard ratios of 3.20 and 12.76, respectively).
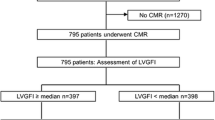
Multivariate analysis and evaluation of optimal LVEF categories
For further evaluation, multivariate models were defined (Table 3 for total cohort; Table 4 for subgroup). All models contained the clinical cardiovascular risk factors with significant results on univariate testing (age, sex, hypertension, hyperlipidemia, diabetes mellitus, and previous revascularization). In addition to that, Model 1 included the CMR derived parameter LVEF. This model yielded a χ 2 value of 62.805 (p < 0.0001). In model 2, the continuous variable LVEF was replaced by for LVEF categories (LVEF <35 %, 35 % ≤ LVEF <45 %, 45 % ≤ LVEF <55 %, 55 % ≤ LVEF), which resulted in an increase of χ 2 up to 69.093 (p < 0.0001). In model 3, LVEF categories were defined as LVEF <30 %, 30 % ≤ LVEF <40 %, 40 % ≤ LVEF <50 % and 50 % ≤ LVEF. A further increase of χ 2 value could be observed (79.029, p < 0.0001). Model 4 included only three LVEF categories (LVEF <35 %, 35 % ≤ LVEF <50 % and 50 % ≤ LVEF) which resulted in a χ 2 value of 76.045 (p < 0.0001). Of the clinical risk factors, only hypertension and diabetes mellitus maintained their statistical significance throughout the different models with hazard ratios between 1.4 and 1.6. The different LVEF categories exhibited higher hazard ratios between 2.5 and 4.3. Furthermore, the addition of LGE resulted in an improvement of each model with an increase of χ 2 values of 12–18 and significant results for integrated discrimination index and net reclassification index. Presence of LGE yielded hazard ratios between 2.3 and 2.5 (p < 0.0001). Table 3 depicts the results in more detail.
Analogously, multivariate testing was performed in the subgroup of 655 patients (Table 4). In principle, comparable results could be observed with models 2 and 3 exhibiting highest overall χ 2 values. Addition of LGE as categorical variable also lead to a significant improvement of each model, whilst the addition of the normalized LGE affection did not (Table 4).
Risk stratification and event rates
Table 5 shows number of events and event rates in dependency of LVEF category. Event rates were similar for patients with LVEF ≥55 vs. LVEF ≥50 % (1.92 vs. 1.82 %, respectively). A significant increase in event rates could be observed in subjects with LVEF <35 vs. LVEF <30 % (7.06 vs. 5.95 %), most probably because of the significant greater number of patients with LVEF <35 % (n = 143) than with LVEF <30 % (n = 89).
Event-free survival
Event-free survival in dependency of LVEF is depicted in Fig. 1. Panel A shows LVEF categories according to model 2 (LVEF <35 %, 35 % ≤ LVEF <45 %, 45 % ≤ LVEF <55 %, 55 % ≤ LVEF), panel B illustrates model 3 (LVEF <30 %, 30 % ≤ LVEF <40 %, 40 % ≤ LVEF <50 %, 50 % ≤ LVEF) and panel C model 4 (LVEF <35 %, 35 % ≤ LVEF <50 %, 50 % ≤ LVEF).
Kaplan–Meier-plot depicting event-free survival in dependency of left ventricular ejection fraction. a LVEF categories corresponding to model 2 (LVEF <35 %, 35 % ≤ LVEF <45 %, 45 % ≤ LVEF <55 %, 55 % ≤ LVEF); b LVEF categories corresponding to model 3 (LVEF <30 %, 30 % ≤ LVEF <40 %, 40 % ≤ LVEF <50 %, 50 % ≤ LVEF); c LVEF categories corresponding to model 4 (LVEF <35 % and 35 % ≤ LVEF <50 %, 50 % ≤ LVEF). LVEF left-ventricular ejection fraction
In Panel A, a good separation could be observed between the survival curves of the groups with mildly impaired LVEF (45 % ≤ LVEF < 55 %) and moderately impaired LVEF (35 % ≤ LVEF < 45 %). In contrast, the curves depicting patients with normal LVEF (LVEF ≥55 %) and mildly impaired LVEF were basically identical. The same is true when looking at the curves of subjects with moderately and severely impaired LVEF (LVEF <35 %).
In panel B, an early separation could be observed between patients with normal LVEF (LVEF ≥50 %) and mildly impaired LVEF (40 % ≤ LVEF < 50 %). There was also a good distinction between patients with mild and moderate impairment of LVEF (30 % ≤ LVEF < 40 %). In contrast, there was no further separation of patients with severely impaired LVEF (LVEF <35 %),
In panel C, the model with only two categories of LVEF impairment is depicted. A good separation of the different groups could be observed.
Discussion
The most important finding of this multi-center trial is the fact that reduced LVEF and presence of LGE are parameters with high prognostic potential predictability. Addition of either of these parameters to a multivariate risk prediction model resulted in significant improvement of the respective model over conventional risk factors (increase in χ 2 values, significant NRI- and IDI-estimates). Hence, proving the incremental prognostic prediction.
Several studies have shown significant association of CMR derived parameters with major cardiovascular endpoints such as myocardial death, myocardial infarction and ventricular arrhythmias [4, 7]. Especially, presence of reversible ischemia, reduced LVEF, and myocardial scar assessed by LGE were prognostic parameters of paramount importance [18]. Attempts to quantify these parameters to improve predictive power lead to varying results. Most of the studies forming the current evidence base are single-center studies with diverging numbers of patients being included. A study containing 376 patients with stable CAD who underwent LVEF and LGE assessment by CMR reported thresholds for LVEF of ≤30 % and for LGE of ≥45 % of left ventricular mass as being most predictive [19]. Patients fulfilling both criteria exhibited annual event rates of 43 %, which rather can be called an ultra-high-risk group and does not account for high-risk patients in clinical routine. In a larger single-center study following up 908 patients for 2.6 ± 1.2 years, patients with abnormal LVEF (defined <50 %) or any presence of LGE had annual event rates of 5.6–6.1 % [20]. Annual event rates in these patients were slightly higher when both parameters were fulfilled (6.5–7.0 %). This study showed an incremental predictive power of these variables when added to risk models containing conventional clinical risk factors.
Recently, annual event rates have been proposed to correctly identify patient risk groups with comparable risks throughout different studies and imaging modalities [21]. A general recommendation derived from these results is to set the threshold for high-risk patients at an annual event rate of 5 % whilst patients with low risk should exhibit event rates of about 1 %.
Within our study, several LVEF thresholds and categories have been evaluated in a multi-model approach. Model 3 which defined a threshold between normal and mildly impaired LVEF at <50 % proved to be superior in correctly identifying patients at increased risk in comparison to model 2 which used the more common threshold at <55 %. Hence, annual event rates for patients with normal LVEF in model 3 (e.g. ≥50 %) were similar to those in model 2 (e.g. ≥55 %). In these models, annual event rates for patients with “normal” LVEF were 1.92 % (model 2) and 1.89 % (model 3), which was in concordance with the above mentioned definition for low risk. On the other hand, model 2 showed better results in the high-risk area: a threshold of LVEF at <35 % (event rate 7.06 %, model 2) proved to be superior concerning the identification of patients at very high risk than a threshold at <30 % (event rate 5.95 %, model 3). In conclusion, we set up model 4, which only used 3 LVEF categories (normal: LVEF ≥50 %, moderately impaired: 35 % ≤ LVEF <50 %, severely impaired: LVEF <35 %). Within this model, it was possible to include the advantages of the former models which translated into proper risk stratification according to the current recommendations (event rates for patients with LVEF ≥50 %: 1.89 %, for patients with 35 % ≤ LVEF <50 %: 5.35 %; for patients with LVEF <35 %: 7.06 %). Whether these three LVEF categories will form a sufficient basis for decision making in any situation CAD patients will possibly experience obviously remains to be clarified in other studies with designated design.
Presence of LGE is known to be a strong predictor of clinical events in patients with stable CAD [3, 4]. In our study, this finding could be confirmed. By adding presence of LGE to the former elaborated risk prediction models, a significant improvement in prognostic power could be observed. In the past, several attempts have been made to evaluate the potential benefit that would arise from quantification of this important variable [22]. Still, the studies available provide inconclusive results and a uniform way of assessing and reporting the extent of LGE could not be elaborated, yet. One study evaluating the prevalence and prognosis of LGE in 1148 patients with known or suspected CAD and normal wall motion defined a study-specific median size of LGE of 6.25 % of myocardium [23]. Patients with LGE lower than the median had no significant increase in risk for cardiac death and non-fatal myocardial infarction on multivariate testing compared to patients without LGE. LGE greater than the median resulted in a hazard ratio of 7.96 which was a significant increase (p = 0.001). It is of note, that only patients with normal wall motion score, and thus normal LVEF were included in this study. Another study evaluating the prognostic value of LGE in a comparable cohort of 1644 patients came to similar results pointing out the strong association between LGE and hard clinical events. Moreover, it could be demonstrated that an increase in LGE resulted in a further increase of risk (patients with LGE ≤20 %: hazard ratio 2.49, p = 0.032; patients with LGE >20 %: hazard ratio 7.77, p < 0.001) [24]. In our study, quantification of LGE was performed on a segmental basis in a subgroup of 655 patients. According to general recommendations, the number of LGE affected segments were normalized to the total number of myocardial segments [25]. Quantification of LGE yielded highly significant results on univariate testing (hazard ratio 12.76, p < 0.0001). Interestingly, it lost its significance on multivariate testing when added to models that contained the variable LVEF. It could be supposed that this finding could be explained because of the strong collinearity between these variables, nevertheless, presence of LGE remained a strong predictor of clinical endpoints in this large cohort of CAD patients.
Limitations
Our study exhibits several limitations that need to be addressed. Because of its retrospective character, it is not possible to conclude information beyond risk stratification. Especially, consequences concerning patient management could not be drawn, yet. It has to be mentioned that information on quantification of LGE only was available in a subgroup of patients and that no quantitative assessment of the extent of LGE or evaluation of transmurality was performed. Nevertheless, the subgroup consisted of 655 patients that were representative for the whole study cohort. Thus, above described analysis can considered to be acceptable and rational. Anticipatory, emerging techniques, such as T1- and T2-mapping are thought to have the potential to improve automatic quantification of injured myocardium, and thus might further ameliorate the understanding of the complex interactions concerning prognosis prediction and patient management [26].
Conclusion
In this study, a large cohort of patients with stable CAD derived from three experienced CMR centers was analyzed. LVEF thresholds at 50 and 35 % could be defined as being most useful and predictive concerning risk stratification. These LVEF thresholds in combination with the assessment of LGE allowed for excellent discrimination between low, mid and high risk prognosis.
References
Wolk MJ, Bailey SR, Doherty JU et al (2014) ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol 4(63):380–406
Becker M, Hundemer A, Zwicker C et al (2015) Detection of coronary artery disease in postmenopausal women: the significance of integrated stress imaging tests in a 4-year prognostic study. Clin Res Cardiol 104:258–271
Buckert D, Dewes P, Walcher T et al (2013) Intermediate-term prognostic value of reversible perfusion deficit diagnosed by adenosine CMR: a prospective follow-up study in a consecutive patient population. JACC Cardiovasc Imaging 6:56–63
Zemrak F, Petersen SE (2011) Late gadolinium enhancement CMR predicts adverse cardiovascular outcomes and mortality in patients with coronary artery disease: systematic review and meta-analysis. Prog Cardiovasc Dis 54:215–229
Reithmann C, Herkommer B, Fiek M (2016) Epicardial ventricular tachycardia substrate visualized by magnetic resonance imaging: need for a transpericardial ablation approach? Clin Res Cardiol (Epub ahead of print)
Petrov G, Kelle S, Fleck E, Wellnhofer E (2015) Incremental cost-effectiveness of dobutamine stress cardiac magnetic resonance imaging in patients at intermediate risk for coronary artery disease. Clin Res Cardiol 104:401–409
Lipinski MJ, McVey CM, Berger JS et al (2013) Prognostic value of stress cardiac magnetic resonance imaging in patients with known or suspected coronary artery disease: a systematic review and meta-analysis. J Am Coll Cardiol 27(62):826–838
Zamorano JL, Bax JJ, Rademakers FE et al (2010) Evaluation of systolic and diastolic LV function. In: The ESC textbook of cardiovascular imaging. Springer, New York, pp 307–320
Cain PA, Ahl R, Hedstrom E et al (2009) Age and gender specific normal values of left ventricular mass, volume and function for gradient echo magnetic resonance imaging: a cross sectional study. BMC Med Imaging 21(9):2
Wood PW, Choy JB, Nanda NC et al (2014) Left ventricular ejection fraction and volumes: it depends on the imaging method. Echocardiography 31:87–100
Korosoglou G, Elhmidi Y, Steen H et al (2010) Prognostic value of high-dose dobutamine stress magnetic resonance imaging in 1,493 consecutive patients: assessment of myocardial wall motion and perfusion. J Am Coll Cardiol 5(56):1225–1234
Kelle S, Roes SD, Klein C et al (2009) Prognostic value of myocardial infarct size and contractile reserve using magnetic resonance imaging. J Am Coll Cardiol 3(54):1770–1777
Kramer CM, Barkhausen J, Flamm SD et al (2013) Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J Cardiovasc Magn Reson 15:91
Schulz-Menger J, Bluemke DA, Bremerich J et al (2013) Standardized image interpretation and post processing in cardiovascular magnetic resonance: Society for Cardiovascular Magnetic Resonance (SCMR) board of trustees task force on standardized post processing. J Cardiovasc Magn Reson 15:35
Lang RM, Bierig M, Devereux RB et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Thygesen K, Alpert JS, Jaffe AS et al (2012) Third universal definition of myocardial infarction. Eur Heart J 33:2551–2567
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr et al (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 30(27):157–172
El Aidi H, Adams A, Moons KG et al (2014) Cardiac magnetic resonance imaging findings and the risk of cardiovascular events in patients with recent myocardial infarction or suspected or known coronary artery disease: a systematic review of prognostic studies. J Am Coll Cardiol 25(63):1031–1045
Catalano O, Moro G, Perotti M et al (2012) Late gadolinium enhancement by cardiovascular magnetic resonance is complementary to left ventricle ejection fraction in predicting prognosis of patients with stable coronary artery disease. J Cardiovasc Magn Reson 19(14):29
Bingham SE, Hachamovitch R (2011) Incremental prognostic significance of combined cardiac magnetic resonance imaging, adenosine stress perfusion, delayed enhancement, and left ventricular function over preimaging information for the prediction of adverse events. Circulation 12(123):1509–1518
Shaw LJ, Berman DS, Picard MH et al (2014) Comparative definitions for moderate-severe ischemia in stress nuclear, echocardiography, and magnetic resonance imaging. JACC Cardiovasc Imaging 7:593–604
Di Bella G, Siciliano V, Aquaro GD et al (2013) Scar extent, left ventricular end-diastolic volume, and wall motion abnormalities identify high-risk patients with previous myocardial infarction: a multiparametric approach for prognostic stratification. Eur Heart J 34:104–111
Krittayaphong R, Saiviroonporn P, Boonyasirinant T et al (2011) Prevalence and prognosis of myocardial scar in patients with known or suspected coronary artery disease and normal wall motion. J Cardiovasc Magn Reson 6(13):2
Krittayaphong R, Boonyasirinant T, Chaithiraphan V et al (2010) Prognostic value of late gadolinium enhancement in hypertensive patients with known or suspected coronary artery disease. Int J Cardiovasc Imaging 26(Suppl 1):123–131
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Myocardial segmentation and registration for cardiac imaging. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 29(105):539–542
Radunski UK, Lund GK, Säring D et al (2016) T1 and T2 mapping cardiovascular magnetic resonance imaging techniques reveal unapparent myocardial injury in patients with myocarditis. Clin Res Cardiol (Epub ahead of print)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state that there neither exists a conflict of interest nor that there are financial information to disclose.
Rights and permissions
About this article
Cite this article
Buckert, D., Kelle, S., Buss, S. et al. Left ventricular ejection fraction and presence of myocardial necrosis assessed by cardiac magnetic resonance imaging correctly risk stratify patients with stable coronary artery disease: a multi-center all-comers trial. Clin Res Cardiol 106, 219–229 (2017). https://doi.org/10.1007/s00392-016-1042-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-016-1042-5