Abstract
Background
The present prospective study investigated whether a combined approach integrating two different stress imaging modalities may improve the diagnostic accuracy and prognostic impact of non-invasive coronary artery disease (CAD) tests in postmenopausal women. In women non-invasive tests for detecting CAD are less accurate than in men, leading to a high proportion of unnecessary coronary angiographies (CAs).
Methods
424 consecutive postmenopausal women (mean 61 ± 7 years, mean Reynolds Risk Score 13 ± 3 %) with symptoms suggestive of CAD were prospectively included and followed up for 4 ± 1 years. Each patient underwent CA, stress cardiovascular magnetic resonance (CMR) by adenosine, dobutamine stress echocardiography (DSE) and single-photon emission computed tomography (SPECT) within 7 ± 3 days.
Results
Anatomically obstructive coronary artery disease (≥50 % diameter stenosis) was present in 157 women (37 %). The combination of two stress imaging modalities significantly increased the positive predictive values (PPV) to 90 ± 3, 88 ± 3 and 87 ± 2 % for CMR/DSE, DSE/SPECT and CMR/SPECT, respectively. For patients with negative combined test results, the survival analysis showed a 4-year cumulative event-free survival rate of 96–97 % for all combinations. This new approach is cost effective due to the resulting reduction in unnecessary CAs (with potential side effects and corresponding therapies) as well as reducing hospitalization time.
Conclusions
In symptomatic postmenopausal women, combination of two negative stress imaging results significantly increases the PPV for detection of CAD and excludes future cardiovascular events with high accuracy. This approach may be applied to improve the prognostic precision of non-invasive CAD tests and to avoid unnecessary CAs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite advances in diagnostic and therapeutic techniques, coronary artery disease (CAD) is the leading cause of death in women. Compared to men, non-invasive evaluation of CAD in females remains challenging for several reasons: the lower prevalence of CAD even in the presence of chest pain [1, 2], the frequent incidence of single-vessel disease [3, 4], and less predictive and atypical symptoms [5]. These difficulties are even augmented in postmenopausal women in whom physiological and pathological changes occur that have significant influence on cardiovascular risk factors partly due to estrogen deficiency [6]. Notably, women with CAD have more adverse outcomes compared to men [7]. Thus, accurate and early diagnostic assessment of CAD are crucial to improve prognoses in women.
Following current recommendations for symptomatic women with suspected CAD [8], exercise ECG is the initial diagnostic test due to cost and feasibility in the setting of a normal resting ECG and good exercise tolerance. For this test, lower predictive values are reported in women compared to men [9, 10]. However, studies focusing on women and especially on symptomatic postmenopausal patients are limited with a subsequent shortage of available evidence for contemporary non-invasive CAD tests such as dobutamine stress echocardiographie (DSE), single-photon emission computed tomography (SPECT) or cardiovascular magnetic resonance (CMR) [11]. At the time of initial diagnosis women are older than men and age-related comorbidities limit exercise capacity, which in combination with smaller heart sizes handicap the analysis of stress tests. Additional limitations of these test modalities are false-positive ECG response by the molecular similarity of estrogen and digitalis (regarding exercise ECG), the dependency on image quality and investigators experience (regarding DSE), limited spatial resolution and radiation exposure (regarding SPECT) and high costs and contraindications for assigned patients (regarding CMR). Coronary angiograms (CA) demonstrating the absence of pathological findings are 2–3 times more common in women than men [12, 13]. This leads to avoidable interventional risks and preventable expenses [14]. Nevertheless, symptomatic women are at elevated risk for cardiovascular events despite the absence of obstructive CAD [1, 15] and are readmitted for chest pain or acute coronary syndrome, four times more frequently compared to men [12]. Even so, female sex is associated with underutilization of guideline-based therapy with ACE inhibitors and statins [16].
The present prospective study evaluated the diagnostic accuracy and prognostic impact of various common stress imaging tests in the patient cohort of postmenopausal women and determined whether combining the results of two stress imaging tests may improve the diagnostic and prognostic accuracy.
Methods
Patients
Postmenopausal women (last menstrual period ≥1 year or surgical menopause) with symptoms suggestive of CAD (typical or atypical chest pain, prolonged discomfort or shortness of breath) who were referred to the University Hospital Aachen between 2005 and 2008 were screened for study enrollment. We excluded all women with known CAD or acute coronary syndrome, valvular heart disease, significant arrhythmia, or contraindications to CMR or dobutamine administration. Overall cardiovascular risk was assessed by the Reynolds Risk Score, a sex-specific tool recently devised from large cohorts of women [17].
Study design
This study was approved by the local ethical committee. After signing informed consent forms, all women underwent a standard protocol (Fig. 1) for CMR, DSE, SPECT and CA within 7 ± 3 days. Stress for DSE and SPECT was induced by dobutamine (maximum dose of 40 µg/kg per min) under continuous ECG and blood pressure monitoring. Additional atropine (total dose ≤2 mg) was administered at the start of the 40 µg/kg per min dobutamine stage if needed to augment the heart rate. All patients were instructed to refrain from β-blockers, calcium antagonists or nitrates, 3 days before the initiation of the study. Stress endpoints were attainment of ≥85 % of the age-predicted maximal heart rate or development of limiting chest pain, significant arrhythmia or relevant hypertension or hypotension. Stress perfusion CMR images were acquired during intravenous adenosine infusion for 4 min at 140 μg/kg/min and an intravenous bolus of 0.075 mmol/kg Gd-DTPA (Magnevist, Schering, Berlin, Germany). All patients were asked to avoid coffeine for 24–48 h before the test. Detailed follow-up of the patients was performed by telephone contact using a scripted interview.
Standard study protocol: all stress tests (CMR cardiac magnetic resonance, DSE dobutamine stress echocardiography, SPECT single-photon emission computed tomography) and CAs were performed within 7 ± 3 days. The follow-up period was 4 ± 1 years. * Stress was performed using dobutamine and additionally atropine if needed to augment heart rate. # Stress was performed using intravenous adenosine infusion for 4 min at 140 μg/kg/min
Definitions of endpoints
We defined the primary endpoint as changes in positive predictive value (PPV) compared to single stress imaging techniques to detect CAD. The secondary endpoint was the occurrence of: (1) cardiovascular death, defined as any death with a demonstrable cardiovascular cause or any death that was not clearly attributable to a noncardiovascular cause or (2) hospitalization for myocardial infarction or coronary catheterization due to unstable angina.
Study procedures
Cardiovascular magnetic resonance
CMR was performed on a 1.5-T whole-body MR scanner (Intera, Best, Philips, the Netherlands) as described before [18]. A perfusion defect was diagnosed if reduced contrast uptake was seen at stress but not rest with more than 25 % transmurality in at least two coherent slices. Ischemia was only reported if the perfusion defect occurred outside any scar. Perfusion defects were scored visually and semiquantitatively as normal (negative result), starting and up to moderately reduced (intermediate result) and severely reduced (positive result).
Dobutamine stress echocardiography
Two-dimensional echocardiography was performed using commercially available equipment (Vivid E9, General Electrics, Horton, Norway). Standard parasternal long- and short-axis views and apical two, three and four chamber views were recorded. Rest, stress and recovery studies were assessed for the presence of normal wall motion, starting (up to moderate hypokinetic) or severe (at least severe hypokinetic up to akinetic or dyskinetic) wall motion abnormalities based on systolic thickening and excursion using a 17 segment model. A normal result was defined as normal wall motion at rest and normal or hyperkinetic wall motion at peak stress. A stress test was considered positive for ischemia in the presence of a biphasic response or new/worsening wall motion abnormalities with at least severe hypokinesia up to akinesia or dyskinesia. A starting impairment of wall motion with up to moderate hypokinesia was labeled as an intermediate result. All classifications required at least two affected myocardial segments and did not change in case of higher quantity of affected segments.
While echocardiographic dobutamine examination an ECG was recorded. At peak stress, the ECG was graded as normal or ischemic. An ischemic response was defined as ≥1 mm of horizontal or down-sloping ST depression 80 ms after J point in a lead with normal ST section at rest, an intermediate response was presumed when these data were marginal lower. The Duke Treadmill Score was not applied.
Single-photon emission computed tomography
At peak dobutamine stress (during the echocardiographic study), 400–600 MBq 99 m-technetium methoxy-isobutyl-isonitril (99mTc-MIBI) was injected. Gated acquisitions (64 × 64 matrix) were acquired on a MultiSPECT 3 (triple-head gamma camera; Siemens Gammasonics Inc.) 1 h post-injection with 60 views at 30 s/view using a zoom factor of 1.23. The next day, rest examinations were performed following an analogous acquisition protocol. The different scores used for quantification of perfusion are based on a segmental comparison of the individual counts of the patient with the corresponding counts of a normal collective. Using a 17-segment model analyses and graduation into negative, intermediate or positive results were operated visually and semiquantitatively as normal (counts >80 % in comparison to normal collective), starting (up to moderate) reduction in counts (50–80 % in comparison to normal collective) and severe reduction in counts (<50 % in comparison to normal collective).
All intermediate results (CMR: starting and up to moderate reduced perfusion; DSE: starting and up to moderate hypokinetic wall motion abnormalities; ECG: marginal lower data referring to ST depression and J point; SPECT: starting and up to moderate reduction in counts) were considered positive for ischemia to provide for daily practice that symptomatic patients with borderline results would rather be transferred to CA [19].
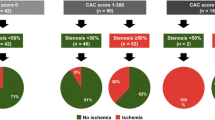
Integrated analysis
The results of the two stress imaging modalities were combined and considered negative for ischemia if both stress imaging modalities showed normal results or one technique showed an intermediate result. A positive finding for ischemia was considered if at least one technique showed an abnormal result or both modalities were classified into the intermediate group (Fig. 2).
Coronary angiography
X-ray CA was performed using standard techniques. The severity of coronary stenosis was determined quantitatively using the software QuantCor (CASS II, Siemens, Erlangen, Germany). Referring to the WISE study coronary artery stenosis was considered obstructive when ≥50 % reduction of the vessel diameter was observed in any epicardial coronary artery. Furthermore, we defined non obstructive coronary arteries (1–49 % stenosis in any epicardial coronary artery) and normal coronary arteries (0 % stenosis). Fractional flow reserve (FFR) was determined in case of intended revascularization (to define hemodynamic relevance of the stenosis) and measured during peak hyperemia induced by an intra-coronary bolus of adenosine (18 μg the left main or 12 μg in the right coronary artery). Hemodynamic relevance was defined as a FFR < 0.80 [20]. The decision to use FFR, to implant a stent and to select subsequent clinical care was based on the discretion of the treating cardiologist who was blinded to the results of the stress imaging test results.
Comparison of stress imaging tests to CA
Left ventricular segments were defined according to the standardized myocardial segmentation model of the American Heart Association [21]. To compare wall motion or perfusion analysis to CA, segmental results were related to the corresponding coronary artery territories. The territory of the left anterior descending (LAD) included the anterior, septal and apical segments, and the combined territory of the circumflex and right coronary artery (LCX/RCA) included the lateral, posterior and inferior segments and the basal inferior septum. Corresponding data for the stress ECG were: LAD: deduction V1–V6, I and aVL; LCX/RCA: deduction II, III and aVF. All data were analyzed by two experienced observers without any knowledge of identity, clinical information or results of the other stress tests. To define interobserver variability in 50 randomly chosen subjects, analyses were repeated by expert off site readers on the same data set. The Cohen´s kappa coefficient was calculated to evaluate the agreement between these two reads [22].
Clinical follow-up
All follow-up interviews were performed by an experienced nurse or physician. During this interview, the patient or a family member was queried for the occurrence of the above-stated cardiac events. If such an event was identified, the referring general practitioner was contacted for detailed information. These interviews were performed annually.
Statistical analysis
Changes in positive predictive value (PPV) were defined as the primary endpoint. The hypothesis was that the integration of two stress imaging methods would significantly increase the PPV. There is some evidence regarding the PPV of each single stress imaging technique but no evidence for the PPV of a combined method. Hence, it was not possible to calculate a sample size. Instead, a commonly accepted population size for comparable studies was sought during the enclosure interval.
Clinical characteristics of the study population are presented using the frequencies or means ± standard deviations (SD). Continuous variables were compared using Student’s t test, Wilcoxon’s test or analysis of variance, as appropriate. We used the χ2-test or Fisher’s test to test the null hypothesis that two dichotomous variables were independent. The ability of each stress test to detect relevant CAD was explored with a random-effects model to address the issue of repeated observations (data on multiple segments per patient used in the analysis). Sensitivity, specificity and PPV and negative predictive value (NPV) of each stress test to detect significant CAD defined by CA (diameter stenosis ≥50 %) were calculated according to the usual definitions. Analyses included comparing single and multi vessel coronary diseases as well as single and integrated stress imaging tests. SD for the PPV was calculated using the standard formula for a proportion.
The Kaplan–Meier method was used to compare the 4-year event-free survival rates for (1) all patients among the same groups (normal/abnormal integrated stress imaging tests and normal/abnormal single stress imaging tests) and (2) for patients with normal or non obstructive CAD (normal integrated/normal single stress imaging tests). With the use of stepwise procedures, multivariable Cox proportional hazards regression models, which include risk factors and clinical history, were developed to estimate freedom from events. Untransformed values as well as logarithmic transformations were entered for variables violating the normality assumption.
Facing internationally and within the US wide ranges for costs for stress imaging modalities and coronary angiography the current study used for comparability reason the cost of an echocardiogram equal 1 as a cost comparator as reported before [23]: corresponding cost of a SPECT was judged 3.27 times higher compared to echocardiogram (cost of a CMR 5.51 times and of a CA 19.96 times higher, respectively). Amount (Table 4) denotes the sum of cost comparator “points” for stress imaging modality (single or integrated) and may be multiplied with the local rate of a DSE examination to calculate the real amount of money. Finally, average amounts for three single and for three integrated stress imaging tests were calculated and compared.
The McNemar test was used to compare the sensitivities, specificities and diagnostic accuracy of the techniques. From the Cox model, relative RRs (95 % confidence intervals) were calculated. To evaluate the agreement between observer analyses, Cohen’s kappa coefficient and weighted Cohen’s kappa coefficient with 95 % confidence intervals, as appropriate, were calculated.
All tests were two-sided, and a p-value <0.05 was considered statistically significant (italic values in Tables 2 and 3). All statistical analyses were performed using SPSS software (SPSS 19.0, Chicago, USA).
Results
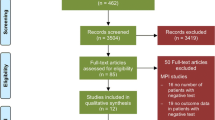
Patients
522 postmenopausal women were screened. Following the stated exclusion criteria, 461 women were included. 424 subjects (mean age 61 ± 7 years) underwent the complete protocol and formed the study group (Fig. 3). Peak stress was obtained using 35 ± 6 µg/kg/min dobutamine; in 78 women, an additional injection of atropine was necessary to reach the target heart rate (146 ± 12 bpm). Systolic blood pressure at peak stress was 161 ± 9 mmHg. 365 women had a low to intermediate overall cardiovascular risk as determined by a mean Reynolds Risk Score of 9 ± 2 %; an intermediate to high risk was calculated in 59 women (mean Reynolds Risk Score of 17 ± 3 %). The mean risk score was 13 ± 3 % regarding the complete study population.
Coronary angiography
Anatomically obstructive coronary artery disease was present in 157 women (37 %): 97 women (62 %) had one vessel, 43 (27 %) had two vessel and 17 (11 %) exhibited three vessel disease. 223 women had non obstructive CAD and 44 women had normal coronary arteries. Baseline clinical characteristics are given in Table 1 and were not different between women with CAD and those without CAD except for concomitant diabetes (p = 0.045). FFR reading was performed in 59 women, in 22 women a hemodynamic relevant stenosis was detected (FFR = 0.74 ± 0.4). These 22 patients and another 29 patients with a ≥90 % reduction of the coronary diameter were treated with a stent implantation using 1.5 ± 0.2 stents (89 % drug eluting) per patient.
All women with non obstructive or obstructive CAD were advised to take aspirin and statins as long-run medication. 91 % of these women followed this recommendation to the point of final interview contact.
Cardiovascular magnetic resonance
Perfusion abnormalities occurred in 140/424 (33 %) women, 44 results (7 %) were classified as intermediate. These segmental results were matched with CA: the PPV and NPV for the diagnosis of CAD were 72 ± 2 and 89 %. Table 2 shows further data. The kappa value was 0.88 (95 % CI 0.83–0.92) for interobserver agreement.
Dobutamine stress echocardiography
New or worsening stress-induced wall motion abnormalities were detected in 138/424 (33 %) women, 46 women (11 %) were determined as intermediate result. These segmental results were compared to CA: the PPV and NPV for the diagnosis of CAD were 72 ± 3 and 88 %. Additional data are given in Table 2. The kappa value was 0.86 (95 % CI 0.82–0.91) for interobserver agreement.
Stress ECG
New or worsening changes of ST-segments were reported in 228/424 (54 %), 17 women (4 %) were classified as intermediate. These results were compared to CA results: the PPV was 58 ± 3 % and the NPV was 77 % for the diagnosis of CAD. The kappa value was 0.84, 95 % CI 0.77–0.90 for interobserver agreement.
Single-photon emission computed tomography
Abnormal results were observed in 135/424 (32 %) women, of that 53 findings (12 %) were classified as intermediate. These segmental results were matched with CA: the PPV was 71 ± 2 %, and the NPV was 87 %. Table 2 shows additional results. The kappa value was 0.84 (95 % CI 0.80–0.89) for interobserver agreement.
Integration of stress imaging results
Overall, combining two stress imaging tests significantly increased the PPV for CAD to 87–90 %. Integrating the CMR and DSE significantly increased the PPV to 90 ± 3 % (Fig. 4); the NPV decreased slightly to 87 %. This approach showed an increased specificity and accuracy and a slightly decreased sensitivity (Table 3). The data for the other combinations were as follows. The combination of DSE and SPECT tests resulted in a PPV of 88 ± 3 % and a NPV of 85 %. Integration of CMR and SPECT yielded a PPV of 87 ± 2 % and a NPV of 85 %; further data are given in Table 3. No further gain in diagnostic accuracy was achieved by integrating all three stress imaging methods. Additionally, PPV and NPV were calculated separately for women with intermediate to high and with low to intermediate pretest likelihood of CAD. The results were not significantly different, but there was a trend towards better discriminatory power for women with higher pretest probability.
Integration of stress ECG and the other stress imaging modalities resulted only in a slight increase of the PPV (ECG/DSE: 65 ± 3 %, ECG/CMR: 67 ± 4 %, ECG/SPECT: 66 ± 3 %) and slight decrease of NPV (ECG/DSE: 74 %, ECG/CMR: 75 %, ECG/SPECT: 74 %).
Clinical follow-up
The average follow-up period was 4 ± 1 years. At follow-up, the integration of stress imaging modalities emphasized an additional benefit with an excellent cumulative event-free survival for individuals with normal (defined as two negative or one negative and one intermediate finding) compared to women with pathological (defined as two intermediate or one positive finding) results: CMR/DSE: 97 vs. 72 %, p = 0.003; DSE/SPECT: 96 vs. 74 %, p = 0.002; CMR/SPECT: 97 vs. 73 %, p = 0.002 (Fig. 5a). The prediction of events by single stress tests was significantly worse compared to the integrated approach with combined stress tests (after 4-year follow-up: 9–11 % events vs. 3–4 % events, p = 0.027–0.036 according to the particular stress test) (Fig. 5b).
Furthermore, a subgroup of women with normal coronary arteries and non obstructive CAD was analyzed regarding event-free survival: women with normal integrated stress results had an excellent event-free survival (98–99 %) compared to women with normal single stress results (79–82 %, p < 0.001). Most of these women were rehospitalized for acute coronary syndrome with repeat cardiac catheterization, one heart failure admission, no myocardial infarction and no death occurred.
Simplified analysis of cost efficiency
The cost efficiency was calculated using the cost of an echocardiogram equal 1 as a cost comparator, cost of a SPECT was judged 3.27 times, of a CMR 5.51 times and of a CA 19.96 times higher compared to echocardiogram as reported before [23] using two approaches (Table 4): (1) employing the standard approach whereby the patient undergoes one stress imaging modality and CA if the test result is positive or intermediate for ischemia (Table 4a). (2) employing the introduced study approach, whereby each patient undergoes a combination of two stress imaging modalities and CA if one test result is positive or two test results are intermediate for ischemia. Due to the significantly increased PPV less patients undergo an unnecessary CA (Table 4b). The average cost comparator “points” for the standard and the new approaches were calculated and compared. Using the average cost comparator “points” for all three combined stress imaging techniques this approach is cost effective (p = 0.073). To calculate the real amount of money one has to multiply the amount of cost comparator “points” with the local rate of a DSE examination.
Discussion
The major findings of this study are as follows: (1) Combined non-invasive imaging analysis compared to a single stress imaging modality significantly increased the PPV for CAD. (2) Normal integrated stress imaging results are associated with an excellent 4-year event-free survival.
Non-invasive evaluation of myocardial ischemia in women is more difficult than in men [11, 24–26]. Women frequently present chest pain, but angina is more often atypical [25], and assessment of symptoms is of limited use because obstructive CAD is less often detected during CA, even in the presence of typical angina [2, 27, 31]. Furthermore, women exhibit a higher incidence of single-vessel disease than men [3, 4] and a more frequent occurrence of intermediate-grade stenosis [2]. Worth mentioning, greater health care costs are incurred in women by more frequent office visits, greater myocardial infarction mortality and higher rates of heart failure hospitalization [29].
Although exercise ECG is the recommended initial diagnostic test for symptomatic women with suspected CAD [7, 32] due to cost and feasibility considerations in the setting of a normal resting ECG and a good exercise tolerance, this method was not integrated in the current study. Due to the rather poor PPV and only moderate NPV of stress ECG [9], false-positive and -negative results would be detected in one out of two to four women, resulting in unnecessary CAs in the false-positive women and potentially detrimental effects in the false-negative women. This is partly related to their lower CAD prevalence and impossibility to attain ≥85 % of age-predicted maximal heart rate due to impaired functional capacity [33]. Other reasons for the diminished accuracy may include a lower QRS voltage (due to obesity and breast tissue) and hormone replacement therapy that may result in false-negative results by vasodilatory properties [10] or false-positive results by the molecular similarity between digitalis and estrogen [34]. Omission of these medications and inclusion of stress testing variables to determine the Duke Treadmill Score may increase accuracy and provide important data on risk of cardiac events [35].
The current study focused on DSE, CMR and SPECT for non-invasive stress testing as these modalities are used in daily routine with an excellent expertise at the study center and are widely spread internationally. The two other possible contemporary stress imaging modalities cardiac computer tomography (CT) and positrone emission tomography (PET) were disregarded due to a limited operational availability at the study center, high costs and high radiation exposure (up to 14 mSv, a doubled dose compared to CA with about 7 mSv) [36]. Exercise ECG was not performed to spare the women an additive examination that is dependent on the patients motivation for maximal exercise and that is often not optimal performable [35] in women due to reduced physical capacity as women present approximately 10 years later in life than men [11]. Furthermore an exercise ECG shows only rather poor PPV [9] without the Duke Score that is not operated in the study center. The current study provide data of medicinal induced stress ECG that circumvent the first aforementioned issues but include no information about the functional capacity that is a powerful prognostic parameter: an exercise capacity <5 METs or the inability to achieve ≥85 % of age-related exercise level has been shown to predict cardiac events in women [37]. The given ECG data are disappointing even in the setting of the introduced approach of combining test modalities with a PPV between 58 % (single test) and 67 % (integrated approach). Further studies should pick up this approach and apply exercise ECG operating the Duke Treadmill Score.
A meta-analysis of DSE studies including gender-specific evaluations reported an overall sensitivity of 76 % and a specificity of 86 % to detect CAD [38]. DSE is limited by dependency on the image quality and the investigators experience. However, this modality provides important data to estimate cardiac prognosis in women as survival of patients with no evidence of ischemia was found to be 99.4 % [39]. Sensitivity and specificity using CMR [40] were reported to be 83 and 83 %. Furthermore, stress CMR is an effective risk-stratifying tool whereat women without inducible ischemia exhibit very low cardiac event rates up to 4 years after the examination [41–43]. This modality is limited by high costs and inexpediency for patients with implanted devices. Finally, studies for SPECT [44] reported similar data: sensitivity was found to be 82 % and specificity was 75 %. This stress test effectively risk stratifies women with an annual event rate of 0.6 % in the case of a normal study [45] but is limited by radiation exposure (about 9mS) [36], false-normal perfusion in the setting of global flow reduction by severe multivessel CAD or microvascular dysfunction and possible missing of minor perfusion defects by limited spatial resolution in combination with smaller female heart sizes.
However, the data on test accuracy in women are limited due to a lack of specific studies, which leads to a high number of normal CAs in symptomatic women. Along these lines, Johnston and colleagues [14] analyzed the Swedish registry data of 5005 women and reported a CA without pathological findings in 64 % of these women. Therefore, the use of non-invasive stress tests to reliably detect CAD would be desirable.
To the best of our knowledge, this study is the first to systematically combine stress imaging tests in a large prospective population of symptomatic postmenopausal women with intermediate to high risk of CAD. In daily routine symptomatic patients with intermediate (borderline) results would rather be treated as a positive finding and transferred to CA. The current study postulated two intermediate results to assume a need for CA and classified patients with an intermediate and a negative result as “negative”. Thus, this approach significantly improves the discriminatory power and increases the chance that a symptomatic woman with a positive combined test result has a relevant CAD and does need a CA. Within the current study this resulted in an identification of additional 16–19 % of patients classified as true-positive for ischemia (PPV). Using the standard single stress test approach, this amount of patients would have been detected as false-positive for ischemia, resulting in numerous unnecessary CA. Therefore, the high number of CAs with normal findings could be reduced, thus limiting potential side effects of the invasive strategy and higher expenses. This is of critical importance given recent data that women are more prone to develop procedural complications than men [14].
However, the NPV plays an important role in reducing unnecessary admissions as well. The new approach of combining stress tests has the advantage to increase the PPV without decreasing the NPV significantly and gives additional safety by the excellent 4-year cumulative event-free survival for women with a normal test result (defined as two negative or one negative and one intermediate finding).
The large amount of symptomatic women without obstructive CAD (63 % within the current study) remains a challenge for physicians caring for such patients. Evidence shows that these women with symptoms of angina in the setting of normal or non obstructive coronary arteries have a high risk for further cardiovascular events [1, 10, 46, 47]. It is hypothesized from the WISE study [1] that the reason for the poor prognosis is endothelial and microvascular dysfunction supported by a combination of smaller arterial size, risk factor clustering, vascular inflammation, hormonal alterations and more positive remodeling in women [29]. This abnormal vascular response may be the earliest marker of atherosclerosis [48] and has prognostic implications [49]. Further studies should apply the integrated approach and focus to this special cohort. Nevertheless, the current study found an excellent event-free survival (98–99 %) for symptomatic women with normal or non obstructive coronary arteries and normal integrated stress tests. In contrast, women with abnormal integrated stress modalities had a 18–21 % cardiovascular event rate during the next 4 years. Thus, the approach of integrated stress imaging tests is an additional tool for risk stratification and may help to differentiate between non-cardiac chest pain, cardiac chest pain (in case of obstructive CAD) and Cardiac Syndrome X (non obstructive CAD with angina and pathologic myocardial perfusion) [50] for optimal treatment and to avoid unnecessary hospitalization and catheterization.
Therefore, diagnostic algorithms should consider including combined stress imaging tests for the accurate diagnosis of CAD in postmenopausal women with an intermediate to high-risk profile. Figure 6 shows a user-friendly flow chart that may help in daily routine to interpret combined test results. Following this proposal it is evident that symptomatic women with a negative or an intermediate result may profit from the introduced approach while women with a primary positive test result do not need a combined approach and can be transferred to CA immediately.
User-friendly flow chart to interpret combined test results. A CA is only required in case of two intermediate or one positive finding. The current standard approach using single stress modalities would imply a CA in case of a positive or an intermediate result and a medical treatment in case of a negative result
By blinding the treating cardiologist and keeping the subsequent clinical care dissociated from the stress test results the total amount of cardiac events was not changed compared to current standard approach. Further studies should determine whether the introduced approach using two stress modalities may improve the outcome by guaranty of event-free survival and avoiding an unnecessary coronary angiography in case of normal results and by scheduling an intensified medical care in case of abnormal results.
Limitation
The Reynolds’ risk score is not frequently used in daily practice. However, risk scores are often developed for a population that differs from the particular study population. The Framingham risk score is preferred to predict the risk of ischemic heart disease but often underestimates this risk in women [51]. Thus, the current study focused on the Reynolds’ score that was generated especially for women [17].
Stress in SPECT and DSE was induced only with dobutamine. Adenosine stress echocardiography is known to have higher specificities but lower sensitivities than DSE for detection of CAD [52]. Exercise stress was not performed as experimental set-up is more time-consuming and more dependent on patient´s cooperation. As recently most CMR studies are performed with perfusion and vasodilators, we choose this approach for CMR as well and used adenosine. Another benefit of the current study is the analysis of different pathophysiological phenomena in combining dobutamine stimulated wall motion or perfusion abnormalities with perfusion heterogeneity during vasodilatation.
Visual assessment for the presence of normal or abnormal regional wall motion (visual and quantitative analyses in SPECT, respectively) is subjective but considered reliable due to an adequate image quality in most cases and due to a high interobserver agreement in this study. All studies were analyzed by designated experts for corresponding imaging techniques.
In routine practice the combined stress test approach is not usual and not widespread available. The current study may effect a rethinking of diagnostic challenges in this patient cohort and propagate the introduced approach as recommended exercise ECG quotes unsatisfying predictive values. Assumably the majority of hospitals can offer at least two of the three stress imaging tests if necessary in combination with an out-patient treatment. Thus the question of which imaging technique may be combined should be discussed individually based on availability of these modalities, observer expertise, patient characteristic, and contraindications for the respective technique. Furthermore, certain disadvantages must be acknowledged for each combination of techniques. The combination of CMR/DSE requires two settings of stress, with possible side effects [51], whereas the combination of CMR/SPECT or DSE/SPECT requires only one stress injection but includes exposure to radiation, which may be reduced by new software and dedicated cardiac SPECT cameras [53].
Awareness of increasing healthcare costs may lead to eschewing the use of the combined non-invasive stress imaging approaches. However, due to the resulting reduction in unnecessary CAs (with potential side effects and corresponding therapies) as well as reducing hospitalization time, this approach is cost effective. The cost ratio used in this study with echocardiogram as a cost comparator has been reported for resting cardiac imaging tests [23]. Nevertheless, the given multiplier effect shall be transferable to stress with the same facultative misperceptions for both approaches within the simplified analysis of cost efficiency. In many countries stress CMR or SPECT are settled per diem thus the choice between adenosine or dobutamine may be not relevant in respect of charges.
Conclusion
In symptomatic postmenopausal women, combination of two negative stress imaging results significantly increases the PPV for detection of CAD and excludes future cardiovascular events with high accuracy. This approach may be applied to improve the prognostic precision of non-invasive CAD tests and to avoid unnecessary CAs.
Abbreviations
- CA:
-
Coronary angiography
- CAD:
-
Coronary artery disease
- CMR:
-
Cardiovascular magnetic resonance
- DSE:
-
Dobutamine stress echocardiography
- LV:
-
Left ventricle/ventricular
- MI:
-
Myocardial infarction
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- PCI:
-
Percutaneous coronary intervention
- SPECT:
-
Single-photon emission computed tomography
- SD:
-
Standard deviation
References
Johnson BD, Shaw LJ, Buchthal SD, Bairey Merz CN, Kim HW, Scott KN, Doyle M, Olson MB, Pepine CJ, den Hollander J, Sharaf B, Rogers WJ, Mankad S, Forder JR, Kelsey SF, Pohost GM, National Institutes of Health-National Heart, Lung, and Blood Institute (2004) Prognosis in women with myocardial ischemia in the absence of obstructive coronary disease: results from the National Institute of Health-National Heart, Lung, and Blood Institute Sponsored Women’s Ischemia Syndrome Evaluation (WISE). Circulation 109:2993–2999
Shaw LJ, Shaw RE, Merz CN, Brindis RG, Klein LW, Nallamothu B, Douglas PS, Krone RJ, McKay CR, Block PC, Hewitt K, Weintraub WS, Peterson ED, American College of Cardiology-National Cardiovascular Data Registry Investigators (2008) Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in-hospital mortality in the American College of Cardiology—National Cardiovascular Data Registry. Circulation 117:1787–1801
Shaw LJ, Bairey Merz CN, Pepine CJ, Reis SE, Bittner V, Kelsey SF, Olson M, Johnson BD, Mankad S, Sharaf BL, Rogers WJ, Wessel TR, Arant CB, Pohost GM, Lerman A, Quyyumi AA, Sopko G, WISE Investigators (2006) Insights from the NHLBI-Sponsored Women,s Ischemia Syndrome Evaluation (WISE) study: part I: gender differences, in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostics strategies. J Am Coll Cardiol 47:S4–S20
Bairey Merz CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, Olson M, Johnson BD, Pepine CJ, Mankad S, Sharaf BL, Rogers WJ, Pohost GM, Lerman A, Quyyumi AA, Sopko G, WISE Investigators (2006) Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) study: part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol 47:S21–S29
Douglas PS, Ginsburg GS (1996) The evaluation of chest pain in women. N Engl J Med 334:1311–1315
Matthews KA, Meilahn E, Kuller LH, Kelsey SF, Caggiula AW, Wing RR (1989) Menopause and risk factors for coronary heart disease. N Engl J Med 321:641–646
Ni H, Coady S, Rosamond W, Folsom AR, Chambless L, Russell SD, Sorlie PD (2009) Trends from 1987 to 2004 in sudden death due to coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J 157:46–52
Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, Douglas PS, Foody JM, Gerber TC, Hinderliter AL, King SB 3rd, Kligfield PD, Krumholz HM, Kwong RY, Lim MJ, Linderbaum JA, Mack MJ, Munger MA, Prager RL, Sabik JF, Shaw LJ, Sikkema JD, Smith CR Jr, Smith SC Jr, Spertus JA, Williams SV, Anderson JL, American College of Cardiology Foundation/American Heart Association Task Force (2012) 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2012(126):e354–e471
Weiner DA, Ryan TJ, McCabe CH, Kennedy JW, Schloss M, Tristani F, Chaitman BR, Fisher LD (1979) Exercise stress testing. Correlation among history of angina, ST-segment response and prevalence of coronary-artery disease in the coronary artery surgery study (CASS). N Engl J Med 301:230–235
Morise AP, Dalal JN, Duval RD (1993) Frequency of oral estrogen replacement therapy in women with normal and abnormal exercise electrocardiograms and normal coronary arteries by angiogram. Am J Cardiol 72:1197–1199
Wenger NK (2011) Women and coronary heart disease: a century after Herrick: understudied, underdiagnosed, and undertreated. Circulation 126:604–611
Mega JL, Hochman JS, Scirica BM, Murphy SA, Sloan S, McCabe CH, Merlini P, Morrow DA (2010) Clinical features and outcomes of women with unstable ischemic heart disease: observations from metabolic efficiency with ranolazine for less ischemia in non-ST-elevation acute coronary syndromes-thrombolysis in myocardial infarction 36 (MERLIN-TIMI 36). Circulation 1(21):1809–1817
Shaw LJ, Gibbons RJ, McCallister B (2002) Gender differences in extent and severity of coronary disease in the ASS-National Cardiovascular Data Registry (abstract). J Am Coll Cardiol 39:321A
Johnston N, Schenck-Gustafsson K, Lagerqvist B (2011) Are we using cardiovascular medications and coronary angiography appropriately in men and women with chest pain? Eur Heart J 32:1331–1336
Gulati M, Cooper-DeHoff RM, McClure C, Johnson BD, Shaw LJ, Handberg EM, Zineh I, Kelsey SF, Arnsdorf MF, Black HR, Pepine CJ, Merz CN (2009) Adverse Cardiovascular outcomes in women with nonobstructive coronary artery disease. Arch Intern Med 169:843–850
Bugiardini R, Yan AT, Yan RT, Fitchett D, Langer A, Manfrini O, Goodman SG, Canadian Acute Coronary Syndrome Registry I and II Investigators (2011) Factors influencing underutilization of evidence-based the rapies in women. Eur Heart J 32:1337–1344
Ridker PM, Buring JE, Rifai N, Cook NR (2007) Development and validation of improved algorithms for the assessment of global cardiovascular risk in women : the Reynolds Risk Score. JAMA 297:611–619
Thiele H, Paetsch I, Schnackenburg B, Bornstedt A, Grebe O, Wellnhofer E, Schuler G, Fleck E, Nagel E (2002) Improved accuracy of quantitative assessment of left ventricular volume and ejection fraction by geometric models with steady-state free precession. J Cardiovasc Magn Reson 4:327–339
Shaw LJ, Mieres JH, Hendel RH, Boden WE, Gulati M, Veledar E, Hachamovitch R, Arrighi JA, Merz CN, Gibbons RJ, Wenger NK, Heller GV, WOMEN Trial Investigators (2011) Comparative effectiveness of exercise electrocardiography with or without myocardial perfusion single photon emission computed tomography in women with suspected coronary artery disease: results from the What Is the Optimal Method for Ischemia Evaluation in Women (WOMEN) trial. Circulation 124:1239–1249
Reith S, Battermann S, Hellmich M, Marx N, Burgmaier M (2014) Impact of type 2 diabetes mellitus and glucose control on fractional flow reserve measurements in intermediate grade coronary lesions. Clin Res Cardiol 103(3):191–201
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS, American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for the healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105:539–542
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46
Picano E (2005) Economic and biological cost of cardiac imaging. Cardiovasc Ultrasound 3:11–13
Kwok Y, Kim C, Grady D, Segal M, Redberg R (1999) Meta-analysis of exercise testing to detect coronary artery disease in women. Am J Cardiol 83:660–666
Sketch MH, Mohiuddin SM, Lynch JD, Zencka AE, Runco V (1975) Significant sex differences in the correlation of electrocardiographic exercise testing and coronary arteriograms. Am J Cardiol 36:169–173
Gulati M, Shaw LJ, Merz NB (2012) Myocardial ischemia in women-lessons from NHLBI WISE study. Clin Cardiol 35:141–148
Rose G, McCartney P, Reid DD (1977) Self-administration of a questionnaire on chest pain and intermittent claudication. Br J Prev Soc Med 31:42–48
Cheng AS, Pegg TJ, Karamitsos TD, Searle N, Jerosch-Herold M, Choudhury RP, Banning AP, Neubauer S, Robson MD, Selvanayagam JB (2007) Cardiovascular magnetic resonance imaging at 3-tesla for the detection of coronary artery disease: a comparison with 1.5-tesla. J Am Coll Cardiol 49:2440–2449
Shaw LJ, Burgiardini R, Bairey Merz CN (2009) Women and Ischemic heart disease. J Am Coll Cardiol 54:1561–1575
Klem I, Greulich S, Heitner JF, Kim H, Vogelsberg H, Kispert EM, Ambati SR, Bruch C, Parker M, Judd RM, Kim RJ, Sechtem U (2008) Value of cardiovascular magnetic resonance stress perfusion testing for the detection of coronary artery disease in women. J Am Coll Cardiol Img 1:436–445
Shaw LJ, Lewis JF, Hlatky MA, Hsueh WA, Kelsey SF, Klein R, Manolio TA, Sharrett AR, Tracy RP, National Heart, Lung and Blood Institute; American College of Cardiology Foundation (2004) Women’s Ischemic Syndrome Evaluation: current status and future research directions, report of the National Heart Lung Blood Institute (NHLBI) workshop, section 5: gender-related risk factors for ischemic heart disease. Circulation 109:e56c–e58c
Kohli P, Gulati M (2010) Exercise stress testing in women: going back to the basics. Circulation 122:2570–2580
Phillips LM, Mieres JH (2010) Noninvasive assessment of coronary artery disease in women: what’s next? Curr Cardiol Rep 12:147–154
Clark PI, Glasser SP, Lyman GH, Krug-Fite J, Root A (1988) Relation of results of exercise stress tests in young women to phases of the menstrual cycle. Am J Cardiol 61:197–199
Alexander KP, Shaw LJ, Shaw LK, Delong ER, Mark DB, Peterson ED (1998) Value of exercise treadmill testing in women. J Am Coll Cardiol 32:1657–1664
Gerber TC, Carr JJ, Arai AE, Dixon RL, Ferrari VA, Gomes AS, Heller GV, McCollough CH, McNitt-Gray MF, Mettler FA, Mieres JH, Morin RL, Yester MV (2009) Ionizing radiation in cardiac imaging: a science advisory from the American Heart Association Committee in Cardiac Imaging of the Council on Clinical Cardiology and Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention. Circulation 119:1056–1065
Gulati M, Black HR, Shaw LJ, Arnsdorf MF, Merz CN, Lauer MS, Marwick TH, Pandey DK, Wicklund RH, Thisted RA (2005) The prognostic value of a nomogram for exercise capacity in women. N Engl J Med 353:468–475
Kim C, Kwok YS, Heagerty P, Redberg R (2001) Pharmacologic stress testing for coronary disease diagnosis: a meta-analysis. Am Heart J 142:934–944
Shaw LJ, Vasey C, Sawada S, Rimmerman C, Marwick TH (2005) Impact of gender on risk stratification by exercise and dobutamine stress echocardiography: long-term mortality in 4,234 women and 6,989 men. Eur Heart J 26:447–456
Hundley WG, Hamilton CA, Thomas MS, Herrington DM, Salido TB, Kitzman DW, Little WC, Link KM (1999) Utility of fast cine magnetic resonance imaging and display for the detection of myocardial ischemia in patients not well suited for second harmonic stress echocardiography. Circulation 100:1697–1702
Jahnke C, Furundzija V, Gebker R, Manka R, Frick M, Schnackenburg B, Marx N, Paetsch I (2012) Gender-based prognostic value of pharmacological cardiac magnetic resonance stress testing: head-to-head comparison of adenosin perfusion and dobutamine wall motion imaging. In J Cardiovasc Imaging 28:1087–1098
Coelho-Filho OR, Seabra LF, Mongeon FP, Abdullah SM, Francis SA, Blankstein R, Di Carli MF, Jerosch-Herold M, Kwong RY (2011) Stress myocardial perfusion imaging by CMR provides strong prognostic value to cardiac events regardless of patient’s sex. J Am Coll Cardiol Img 4:850–861
Wallace EL, Morgan TM, Walsh TF, Dall’Armellina E, Ntim W, Hamilton CA, Hundley WG (2009) Dobutamine cardiac magnetic resonance results predict cardiac prognosis in women with known or suspected ischemic heart disease. J Am Coll Cardiol Img 2:299–307
Mieres JH, Makaryus AN, Cacciabaudo JM, Donaldson D, Green SJ, Heller GV, Maddahi J, Ong L, Rampersaud T, Rosen SE, Shaw LJ, Katz S (2007) Value of electrocardiographically gated single-photon emission computed tomographic myocardial perfusion scintigraphy in a cohort of symptomatic postmenopausal women. Am J Cardiol 99:1096–1099
Shaw LJ, Iskandrian AE (2004) Prognostic value of stress gated SPECT in patients with known or suspected coronary artery disease. J Nucl Cardiol 11:171–185
Jespersen L, Abildstrøm SZ, Peña A, Hansen PR, Prescott E (2014) Predictive value of the corrected TIMI frame count in patients with suspected angina pectoris but no obstructive coronary artery disease at angiography. Clin Res Cardiol 103:381–387
Jespersen L, Abildstrøm SZ, Hvelplund A, Prescott E (2013) Persistent angina: highly prevalent and associated with long-term anxiety, depression, low physical functioning, and quality of life in stable angina pectoris. Clin Res Cardiol 102:571–581
Verma S, Buchanan MR, Anderson TJ (2003) Endothelial function testing as a biomarker of vascular disease. Circulation 108:2054–2059
Ndrepepa G, Tada T, Fusaro M, Cassese S, King L, Hadamitzky M, Haase HU, Schömig A, Kastrati A, Pache J (2012) Association of coronary atherosclerotic burden with clinical presentation and prognosis in patients with stable and unstable coronary artery disease. Clin Res Cardiol 101:1003–1011
Ong P, Athanasiadis A, Mahrholdt H, Borgulya G, Sechtem U, Kaski JC (2012) Increased coronary vasoconstrictor response to acetylcholine in women with chest pain and normal coronary arteriograms (cardiac syndrome X). Clin Res Cardiol 101:673–681
Pasternak RC, Abrams J, Greenland P, Smaha LA, Wilson PW, Houston-Miller N (2003) Identification of coronary heart disease risk: is there a detection gap? J Am Coll Cardiol 41:1863–1874
Elhendy A, Geleijnse ML, van Domburg RT, Nierop PR, Poldermans D, Bax JJ, TenCate FJ, Nosir YF, Ibrahim MM, Roelandt JR (1997) Gender differences in the accuracy of dobutamine stress echocardiography for the diagnosis of coronary artery disease. Am J Cardiol 80:1414–1418
Garcia EV, Faber TL, Esteves FP (2011) Cardiac dedicated ultrafast SPECT cameras: new designs and clinical implications. J Nucl Med 52:210–217
Acknowledgments
MB designed the study and managed research process, MB and AH chaired data acquisition and analysis and interpretation of results, MB wrote the report. MB, AH and RH had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Data were analyzed by CZ (DSE), EA (CMR) and FMM and TK (SPECT). CL contributed to statistical interpretation of results. MK and AH contributed to data analysis and interpretation and reviewed the report. NM, AH and RH contributed to the writing of the report.
Conflict of interest
No conflicts of interest or financial disclosures to announce.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Becker, A. Hundemer distributed equally.
Number clinical trial: link: http://clinicaltrials.gov/ct2/show/NCT00763464?term=CAD++and+FEMCAD&rank=1 unique identifier: CAD-female 2006-MB NCT-number: NCT 00763464.
Rights and permissions
About this article
Cite this article
Becker, M., Hundemer, A., Zwicker, C. et al. Detection of coronary artery disease in postmenopausal women: the significance of integrated stress imaging tests in a 4-year prognostic study. Clin Res Cardiol 104, 258–271 (2015). https://doi.org/10.1007/s00392-014-0780-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-014-0780-5