Abstract
Background
Chiari malformation type 1 (CM1) is a congenital hindbrain malformation characterized by herniation of the cerebellar tonsils below the foramen magnum. The term Chiari type 1.5 is used when herniation of the brainstem under the McRae line and anomalies of the craniovertebral junction are also present. These conditions are associated with several symptoms and signs, including headache, neck pain, and spinal cord syndrome. For symptomatic patients, surgical decompression is recommended. When radiographic indicators of craniovertebral junction (CVJ) instability or symptoms related to ventral brainstem compression are present, CVJ fixation should also be considered.
Case description
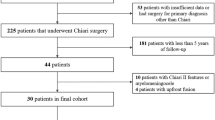
We report the case of a 13-year-old girl who presented with severe tetraparesis after posterior decompression for Chiari malformation type 1.5, followed 5 days later by partial C2 laminectomy. Several months after the initial surgery, she underwent two fixations, first without and then with intraoperative cervical traction, leading to significant neurological improvement.
Discussion and conclusion
This case report underscores the importance of meticulous radiological analysis before CM surgery. For CM 1.5 patients with basilar invagination, CVJ fixation is recommended, and C2 laminectomy should be avoided. In the event of significant clinical deterioration due to nonadherence to these guidelines, our findings highlight the importance of traction with increased extension before fixation, even years after initial destabilizing surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chiari malformation type 1 (CM1) is a congenital hindbrain malformation characterized by herniation of the cerebellar tonsils below the foramen magnum [1, 2]. When herniation of the brainstem under the McRae line and anomalies of the craniovertebral junction (CVJ) as basilar invagination or retroversion of the odontoid process are also present, the term Chiari type 1.5 (bulbar variant of CM 1) is used [3, 4]. Chiari malformations are associated with several symptoms and signs, including Valsalva-related headache, neck pain, and spinal cord syndrome. For symptomatic patients, surgical decompression with or without dural peeling or duraplasty is recommended to restore normal posterior fossa cerebrospinal fluid dynamics [1, 5, 6]. Moreover, when radiographic indicators of CVJ instability or symptoms related to ventral brainstem compression are present, CVJ fixation should also be considered [7]. Several studies have reported criteria for deciding which patients should undergo CVJ deformity correction and fixation, including the clivo-axial angle (CXA), Grabb-Oakes index (GOI), Chamberlain line, McRae line, Harris measurement, and C1-C2 facet alignment [1, 8,9,10,11,12,13,14,15].
In this article, we present an original case of severe neurological degradation after posterior decompression for Chiari malformation type 1.5, followed 5 days later by partial C2 laminectomy. Afterwards, two fixations, first without and then with intraoperative cervical traction, led to significant neurological improvement.
Case report
A 13-year-old girl presented at another institution with progressive headache, visual blur, and vomiting. Head MRI revealed Chiari type 1.5 malformation with platybasia (basal angle of the skull base of 151°, normal 125–143°), basilar invagination (tip of the dent 1.3 cm above the Chamberlain line and at the level of the McRae line), and other signs of CVJ instability [16]. The clivo-axial angle was 99.8° (normal 145–160°), the Grabb-Oakes index was 10 mm (normal ≤ 9 mm), and the Harris measurement was 15 mm (normal < 12 mm) (Fig. 1).
She initially underwent in this first center an occipital craniectomy, C1 laminectomy, and duraplasty, followed 5 days later by cerebellar tonsil resection, C2 partial laminectomy, and extension of the duraplasty, because of cervical pain not manageable with medical treatment. After the second procedure, the patient woke up with severe tetraparesis (Medical Research Council (MRC) Scale 1–2/5), severe hypoesthesia of the whole body except the head, vertical and horizontal diplopia, and complete paralysis of the vocal cords and of the tongue. She required tracheostomy, continuous oxygen therapy, and aspiration. Postoperative MRI (Fig. 2) showed destabilization of the cervical spine, especially as demonstrated by a decrease in the clivo-axial angle from 95 to 81°. Afterwards, she developed obstructive hydrocephalus, which was treated by an external ventricular drain and subsequently by a ventriculoperitoneal shunt.
Eleven months later, in a second center, she underwent a fifth surgery consisting of simple occipito-C2-C3 fixation without cervical traction. Neurological improvement was significant: she recovered the ability to stand, walk, and write the very week following surgery, with mean global MRC score ranging from 2–3 to 4–5/5. She also reported hypoesthesia improvement (mild); she subsequently regained continence, and the continuous oxygen supplies could be stopped.
Fifteen months after the fifth surgery, the patient came to our center in a rolling chair (because of significant axial ataxia), still needing tracheotomy and digestive aspiration, and presenting severe diplopia. Sensorimotor status was stable. However, the patient wished further neurological improvement, and the senior author (CR) proposed the realization of cervical traction with additional extension and fixation.
During this sixth surgery, traction with 1/10th of the patient’s weight was applied. The nuts holding the rods were gradually removed. On the starting side, a longer rod with a more open angle was designed and substituted to the old one, allowing cervical traction to be maintained and opening of the clivo-axial angle to be performed. The same procedure was then reproduced on the contralateral side. Intraoperative fluoroscopic control confirmed the desired modification of the clivo-axial angle and the efficacy of traction. Immediately after surgery, the patient described an almost complete regression of her horizontal dipoplia.
A CT scan performed 2 days after the procedure and a 6-month follow-up MRI of the cervical spine (Fig. 3) both confirmed a partial correction of the clivo-axial angle (82° from 77°) and a regression of the basilar invagination and of the kinking effect on the brainstem (Fig. 4).
At the 6-month follow-up, several neurological improvements were observed, including regression of sensory ataxia, the ability to walk without falling (which occurred weekly preoperatively), the ability to climb stairs alone by holding onto the railing (which was completely impossible preoperatively), and progress at the respiratory and swallowing levels, with the possibility of swallowing saliva and chewing aliments without the risk of choking. This had a great positive psychological impact on her after 2 years of oral alimentary privation. Hypoesthesia remained stable (mild), as well as MRC score of the limb muscles (4–5/5). The negative point noted by the patient was pain (Visual Analogue Scale score of 2) at the level of the screw heads protruding under the skin. The patient considered herself to have improved by 75%.
Discussion
The presence of basilar invagination or signs of craniocervical instability is crucial to consider in the strategical management of Chiari malformations. The recommendations of the 2019 Chiari & Syringomyelia Consensus Conference are summarized hereafter [7, 17]. Posterior decompression and CVJ fixation are the preferred surgical options for CM patients with CVJ instability and related symptoms. In the case of basilar invagination with atlantoaxial dislocation, posterior fixation is recommended [17]. Anterior decompression may be indicated for persistent compression with symptoms. Fixation by C0–C3 or C1–C2 in CM patients with CVJ instability should be decided on the basis of local anatomy [17]. Regarding the extent of posterior fossa decompression, panelists recommend wide bony decompression on the foramen magnum, including C1 laminectomy, and never extended to C2 for the risk of CVJ instability. When a patient has basilar invagination, cervical traction should always be considered since it can itself clinically improve the condition (in 82% of patients when not associated with Chiari malformation and in 5% if present), especially in children [18, 19].
Conclusion
This case report underscores the importance of meticulous radiological analysis before CM surgery. For CM 1.5 patients with basilar invagination, CVJ fixation is recommended, and C2 laminectomy should be avoided. In the event of significant clinical deterioration due to nonadherence to these guidelines, our findings highlight the importance of traction with increased extension before fixation, even years after initial destabilizing surgery.
Data availability
No datasets were generated or analyzed during the current study.
Code availability
Not applicable.
References
Sangwanloy P, Vaniyapong T, Norasetthada T, Jetjumnong C (2022) Influence of clivo-axial angle on outcome after foramen magnum decompression in adult symptomatic Chiari type 1 malformation. Clin Neurol Neurosurg 216:107214
Chiari H (2008) Concerning alterations in the cerebellum resulting from cerebral hydrocephalus. Pediatr Neurosurg 13(1):3–8
Cools MJ, Wellons JC, Iskandar BJ (2023) The nomenclature of Chiari malformations. Neurosurg Clin N Am 34(1):1–7
Tubbs RS, Iskandar BJ, Bartolucci AA, Oakes WJ (2004) A critical analysis of the Chiari 1.5 malformation. J Neurosurg 101(2 Suppl):179–183
Del Gaudio N, Vaz G, Duprez T, Raftopoulos C (2018) Comparison of dural peeling versus duraplasty for surgical treatment of Chiari type I malformation: results and complications in a monocentric patients’ cohort. World Neurosurg 117:e595–602
Massimi L, Frassanito P, Bianchi F, Tamburrini G, Caldarelli M (2019) Bony decompression vs duraplasty for Chiari I malformation: does the eternal dilemma matter? Childs Nerv Syst 35(10):1827–1838
Ciaramitaro P, Massimi L, Bertuccio A, Solari A, Farinotti M, Peretta P et al (2022) Diagnosis and treatment of Chiari malformation and syringomyelia in adults: international consensus document. Neurol Sci 43(2):1327–1342
Kim LJ, Rekate HL, Klopfenstein JD, Sonntag VKH (2004) Treatment of basilar invagination associated with Chiari I malformations in the pediatric population: cervical reduction and posterior occipitocervical fusion. J Neurosurg Pediatr 101(2):189–195
Bollo RJ, Riva-Cambrin J, Brockmeyer MM, Brockmeyer DL (2012) Complex Chiari malformations in children: an analysis of preoperative risk factors for occipitocervical fusion: Clinical article. J Neurosurg Pediatr 10(2):134–141
Grabb PA, Mapstone TB, Oakes WJ (1999) Ventral brain stem compression in pediatric and young adult patients with Chiari I malformations. Neurosurgery 44(3):520
Felbaum D, Spitz S, Sandhu FA (2015) Correction of clivoaxial angle deformity in the setting of suboccipital craniectomy: technical note. J Neurosurg Spine 23(1):8–15
Henderson FC, Henderson FC, Wilson WA, Mark AS, Koby M (2018) Utility of the clivo-axial angle in assessing brainstem deformity: pilot study and literature review. Neurosurg Rev 41(1):149–163
Klekamp J (2015) Chiari I malformation with and without basilar invagination: a comparative study. Neurosurg Focus 38(4):E12
Goel A (2015) Is atlantoaxial instability the cause of Chiari malformation? Outcome analysis of 65 patients treated by atlantoaxial fixation. J Neurosurg Spine 22(2):116–127
Loe ML, Vivas-Buitrago T, Domingo RA, Heemskerk J, Tripathi S, Bendok BR et al (2020) Prognostic significance of C1–C2 facet malalignment after surgical decompression in adult Chiari malformation type I: a pilot study based on the Chicago Chiari Outcome Scale. J Neurosurg Spine 34(2):171–177
Koenigsberg RA, Vakil N, Hong TA, Htaik T, Faerber E, Maiorano T et al (2005) Evaluation of platybasia with MR imaging. AJNR Am J Neuroradiol 26(1):89–92
Massimi L, Peretta P, Erbetta A, Solari A, Farinotti M, Ciaramitaro P et al (2022) Diagnosis and treatment of Chiari malformation type 1 in children: the International Consensus Document. Neurol Sci 43(2):1311–1326
Goel A, Bhatjiwale M, Desai K (1998) Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg 88(6):962–968
Goel A (2004) Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine 1(3):281–286
Author information
Authors and Affiliations
Contributions
EV wrote the paper, reviewed the litterature and followed the patient; NdG and LdN reviewed the paper, followed the patient and assisted the senior surgeon during the surgery; CR defined the strategy, operated on the patient and reviewed the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Patient consent
The patient and her family consented to the submission of the case report to the journal.
Ethics approval
No financial support was received for this work. The patient and her family consented to the submission of the case report to the journal. Consent to participate: The patient and her family consented to the submission of the case report to the journal.
Consent for publication
The patient and her family have consented to the submission of the case report to the journal.
Additional information
The manuscript is an original contribution that has not been submitted simultaneously to another journal or published elsewhere, partially or in full in any form or language. The results are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation (including image-based manipulation).
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vigneul, E., Del Gaudio, N., de Nijs, L. et al. Neurological outcome following delayed traction and fixation in severe tetraparesis consecutive to posterior decompression for Chiari malformation: a case report. Childs Nerv Syst 40, 1943–1947 (2024). https://doi.org/10.1007/s00381-024-06327-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-024-06327-6