Abstract
Objective
Chiari I malformation is treated with suboccipital craniectomy with cervical laminectomy, a procedure which has been associated with the possibility of pre-existing or iatrogenic occipitocervical instability. The long-term risk of subsequent spinal deformity and need for occipito cervical fusion after standard Chiari decompression in pediatric patients has not yet been characterized.
Methods
We queried our institutional electronic database for patients aged 18 and under, with at least 5 years of follow-up, that underwent surgical decompression for Chiari I malformation. Occurrence of subsequent occipitocervical fusion at follow-up comprised the primary endpoint. Cases with myelomeningocele, Chiari II, or fusion at time of decompression were excluded.
Results
A total of 30 patients (median age 5.5 years, 60% males) were analyzed. Age distribution was as follows: n = 3 for 0–1 years, n = 11 for 1–5 years, n = 4 for 5–10 years, and n = 12 for 10–18 years. Median tonsillar descent below the foramen magnum was 12.5 mm (interquartile range [IQR]: 10.8–19.5 mm). Syringomyelia was observed in 43%, retroflexion of the dens in 55%, basilar invagination in 6.7%, and medullary kinking in 27%. The median clivo-axial angle was 142° (132–150°). The majority of patients underwent C1 laminectomy (n = 24, 80%), followed by C1-C2 laminectomy (n = 4, 13%), while one patient had C1-upper C2 and C1-C3 laminectomy each, respectively. At a median follow-up of 6.3 years, there was only one patient (3.3% of overall cohort) that underwent subsequent occipitocervical fusion. The patient (4-year-old male) initially had a suboccipital craniectomy with C1 laminectomy and duraplasty and presented with recurrence of posterior headaches and neck pain 4 months after original surgery. We proceeded with occiput-C2 fusion with subsequent resolution of his symptoms.
Conclusion
Current analysis shows that in the absence of clinical or imaging features suggestive of craniocervical instability, Chiari I decompressive surgery is associated with very low long-term risk of requiring occipitocervical fusion. This observance can be used to guide surgical treatment decisions, especially in young children with Chiari I malformations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chiari I malformation is defined radiologically as herniation of the cerebellar tonsils below the foramen magnum, often with peg-like appearance of the tonsils and syringomyelia [1, 2]. Prevalence of Chiari I malformation is estimated between 0.5 and 1% in the adult population, while prior work in children found a prevalence of 3.6% in children undergoing imaging of the brain and spine [3, 4]. Symptoms of syringobulbia or syringomyelia, lower cranial nerve dysfunction, and refractory occipital headache prompt consideration of surgical management in these patients [1, 2]. Posterior fossa decompression and C1 laminectomy with or without additional cervical laminectomy are employed as a surgical treatment for symptomatic patients. This procedure and associated underlying pathology have traditionally been considered risk factors for subsequent occipitocervical instability, particularly in the rapidly growing spines of young children [5,6,7]. The occurrence of and risk factors for delayed occipitocervical fusion following this decompression are not well understood with fusion rates in prior studies varying substantially [8,9,10]. With this study, we seek to further define the long-term requirements for occipitocervical fusion in this young patient population.
Materials and methods
Data source and selection criteria
Following Institutional Review Board approval (#21–000,426), we queried our institutional electronic database for all years available for pediatric patients (defined as less than 18 years of age) with Chiari malformation (ICD-9 code 741.90, ICD-10 code Q07.01) that underwent surgical decompression. We excluded cases with Chiari II malformation or concurrent myelomeningocele, patients that underwent surgery for another reason or underwent fusion at the same time with decompressive surgery. We also excluded cases with less than 5 years of postoperative follow-up.
Primary outcome
Occurrence of subsequent fusion (i.e., at follow-up) at our institution or outside institution comprised the primary outcome of interest. We also recorded the occurrence of new axial neck or arm pain or cervical spine deformity.
Covariates of interest
We recorded the following variables: age, sex, comorbidities (prematurity, sleep apnea, presence of spinal deformity), baseline radiographic parameters (length of tonsillar descent through the foramen magnum, presence of syrinx, basilar invagination (defined as the tip of the odontoid process projecting above the line connecting the basion with the opisthion), retroflexed dens (defined as posterior angulation of the odontoid process in relation to the body of the axis), medullary kinking, clivo-axial angle (defined as the angle created between a line drawn along the lower third of the clivus and a line drawn along the posterior surface of the odontoid process), and operative variables (levels of laminectomy). The clivo-axial angle in most individuals lies in the range 145–160° in the neutral position, and may increase up to 180° in extension [11, 12].
Statistical analysis
Descriptive statistics (continuous variables using medians with interquartile ranges and categorical variables using frequencies with proportions) were used to summarize the available information. Given our limited sample size, univariate analysis with p values was not conducted. Statistical analysis was conducted using R open software, version 3.4.3 (R Development Core Team (2008). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline demographics and clinical symptoms
A total of 278 patients were identified through the electronic search. After applying exclusion criteria (n = 53 for a primary diagnosis other than Chiari, n = 181 with less than 5 years of follow-up, n = 10 patients with Chiari II features, and n = 4 with upfront fusion), thirty patients remained in the final cohort and were further analyzed [Fig. 1]. The four upfront fusion patients had the following characteristics (in addition to Chiari malformation): (1) a 4-year-old female with mild cognitive delay, severe basilar invagination, 20 mm of tonsillar displacement, and retroverted dens who underwent both transoral decompression of the dens and posterior occiput to C4 fusion; (2) a 7-year-old male with dental retroversion, 10 mm of tonsillar displacement, 140° of clivo-axial angle, and ventral brainstem compression who underwent occiput to C2 fusion; (3) a 6-year-old male with torticollis at age 4, 6 mm of tonsillar descent, Klippel-Feil syndrome, diminutive C1 posterior arch, occipitalization of the atlas, and enlarged atlantodental interval who underwent occiput to C3 fusion; and (4) an 18-year-old female with platybasia, high position of dens and C1 arch, and hypoplastic occipital condyles with early degenerative changes who underwent occiput to C3 fusion.
In the final cohort, median age was 6 years (IQR: 2–14) and 58% were males (n = 18). Age distribution was as follows: n = 3 for 0–1 years, n = 11 for 1–5 years, n = 4 for 5–10 years, and n = 13 for 10–18 years. One patient had scoliosis and one patient was diagnosed with sleep apnea preoperatively. No patient was born prematurely. A summary of this information per age group is presented in Table 1.
Imaging characteristics
With regard to MRI characteristics, median tonsillar descent below the foramen magnum was 13 mm (IQR: 11–21 mm). Syringomyelia was observed in 13 cases (42%), retroflexion of the dens in 17 cases (57%), basilar invagination in 2 cases (6.7%), and medullary kinking in 8 cases (27%). The median clivo-axial angle was 142° (IQR: 132–150°).
Operative parameters
All patients had suboccipital craniectomy with allograft duraplasty. In terms of cervical decompression, the overwhelming majority of patients underwent C1 laminectomy (n = 25, 81%), followed by C1-C2 laminectomy (n = 4, 13%), while one patient had C1-upper C2 and C1-C3 laminectomy, respectively.
Incidence of subsequent fusion
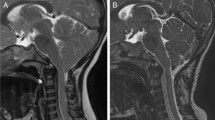
At a median follow-up of 6.3 years, there was only one patient that underwent subsequent occipitocervical fusion. The patient was an otherwise healthy 4-year-old male who presented with a year history of debilitating holocephalic headaches, predominantly occipital, and no other neurological symptoms [Fig. 2]. Preoperative MRI showed tonsillar descent of 14 mm and retroflexed dens with mild medullary kinking. Syrinx or basilar invagination was not present. The clivo-axial was 118.7°. He underwent uneventful suboccipital craniectomy with C1 laminectomy and duraplasty. Although improved initially, his headaches returned 4 months after surgery. He complained of debilitating posterior occipital headaches and neck pain exacerbated by neck movement. He did not have any neurological deficits on physical exam. Follow-up MRI continued to show tightness around the cervicomedullary junction. The working hypothesis was C2 nerve irritation due to micro-instability at the craniocervical region (although not evident in plain flexion–extension cervical spine x-rays); therefore, the decision was made to proceed with fusion. He underwent uneventful occiput-C2 arthrodesis with subsequent complete resolution in his symptoms at 5-year follow-up. A summary of the characteristics of this case is presented in Table 2.
Images of the 4-year-old male that underwent subsequent occiput-C2 arthrodesis following O-C1 laminectomy. A Preoperative sagittal T2 MRI showed tonsillar descent of 14 mm and retroflexed dens with mild medullary kinking. The clivo-axial was 118.7°, B postoperative sagittal T2 MRI, C extension and D flexion cervical spine radiographs due to neck pain recurrence following the Chiari decompression showing stepwise subluxation in upper cervical levels but no overt hypermobility at the C1-C2 complex, E postoperative neutral cervical spine radiograph following O-C2 fusion
Review of the clinical course of the remainder of the patient did not reveal subsequent fusion at our or outside institutions. Only one other patient complained of neck pain. Postoperative x-rays were obtained for various reasons (residual headache, evaluate potential development of deformity, brainstem compression) in 15 (50%) of patients, and no patient developed worrisome findings, such as subluxation from occiput to C2, loss of cervical kyphosis or new lordosis, or new basilar invagination).
Discussion
In the present analysis, we reviewed the long-term outcomes of our institutional series of pediatric patients with Chiari I malformation and found the risk of subsequent fusion to be extremely low, i.e., 3.3% (1/30 patients). Only one patient underwent O-C2 fusion after a short interval after decompression due to persistent symptoms which resolved after fusion.. The remainder of this surgical cohort did not acquire instability or need for fusion during long-term follow-up.
The overall risk for spinal instability following cervical laminectomies in children and particularly those spanning 2 levels or more remains a controversial issue. Along these lines, Yasuoka et al. examined the incidence of spinal column deformity (kyphoscoliosis and/or instability) following multilevel laminectomy in patients younger than 25 years of age [9]. There were no instances of spinal deformity in 68 Chiari patients undergoing occiput-C1/C2 laminectomy. On the other hand, Bell et al. investigated the association between the development and progression of spinal deformity after multilevel cervical laminectomy in 89 children, of which 65 had Chiari malformation (I or II) [5]. Significant kyphosis developed in 46 patients (53%) at a mean follow-up of 5.1 years. Interestingly, the development of kyphosis did not significantly correlate with the number of resected levels.
Chiari I malformation rarely co-exists with concurrent spinal deformities; however, a proportion are considered “complex” and therefore necessitate more thorough evaluation before offering decompression alone [8, 10, 13]: (1) basilar invagination (7% in our series), (2) clivo-axial angle less than 125° (10% in our series), and (3) the condylar-C2 sagittal vertical alignment (defined as the position of a plumb line from the midpoint of the O-C1 joint relative to the posterior aspect of the C2-C3 disc space). These variations in craniovertebral anatomy may represent a manifestation of underlying occipitocervical instability, thereby necessitating static and dynamic cervical spine radiographics and consideration for possible arthrodesis. Observances from the Park-Reeves Syringomyelia Research Consortium have revealed an overall occurrence of occipitocervical fusion in the Chiari population of 1.8% [14]. Platybasia, Klippel-Feil syndrome, and basilar invagination were found to be risk factors for fusion. Most fusions were upfront, and the delayed fusions occurred at a median interval of 27 months.
In the absence of the aforementioned factors, other authors have attributed the risk of postoperative spinal instability and/or subsequent deformity to violation of the suboccipital muscle and semispinalis capitis and cervicis (i.e., when C2 decompression is performed) or facet violation if laminectomy is too wide [15,16,17,18]. According to an older series of 32 pediatric patients from Pittsburgh, the frequency of postoperative kyphosis was 9%, and the one case with cervical instability had inadvertent violation of the facet joint [18]. Elsewhere in the literature, there are mainly single case reports of subsequent fusion in children, which reflects the rarity of this need as demonstrated in our series. Willhuber et al. presented a case of a 9-year-old female who presented with symptomatic torticollis due to new C1/2 rotatory subluxation and C2/3 anterolisthesis at 4 months following uncomplicated O-C2 laminectomy [19]. She went to receive O-C4 fusion and was pain- and symptom-free at 12-month follow-up. Bekelis et al. reported a case of a 6-year-old female with past surgical history of Chiari decompression surgery at 22 months of age that presented with neck pain on flexion and extension. She underwent occiput-C2 fusion with occipital condyle screws and resolution of her neck pain on last follow-up [7].
In retrospective review, the one patient in our series that underwent later fusion had radiographic (clivo-axial angle less than 125°) and clinical (persistent occipital and neck pain despite adequate decompression) factors for need for arthrodesis. While preoperative x-rays are not routinely obtained in all Chiari I cases, patients with a “complex” phenotype, i.e., basilar invagination, clivo-axial angle less than 125°, and condylar-C2 sagittal vertical alignment greater than 5 mm, could benefit from standing and flexion–extension plain radiographs to evaluate for spinal instability and consideration of upfront fusion. In our institutional experience, we have found that children who do not display such “high-risk” features can be safely observed with minimal risk of requiring long-term subsequent occipitocervical fusion.
Limitations
The first limitation of this study is the retrospective design. Second, many patients in our institutional surgical cohort did not have 5 years of follow-up, which led to a limited sample size. As shown in Fig. 1, there were 180 patients excluded with less than 5-year follow-up out of 225 patients who underwent surgery for Chiari malformation. Although this reduced our sample size, we deemed 5 years a reasonable minimum time frame for monitoring for development of occipitocervical instability. Third, the need for subsequent arthrodesis was based on clinical signs, and dynamic x-rays were not routinely performed in Chiari patients postoperatively. Therefore, the incidence of sub-clinical radiographic evidence of kyphotic deformity was not determined. Finally, a small number of patients in our surgical series underwent upfront occipitocervical fusion, which may have introduced selection bias in the remaining cohort of patients that were studied.
Conclusion
The long-term risk of subsequent fusion following decompressive surgery for non-complex pediatric Chiari I patients is extremely low. Although this operation has traditionally been associated with the need for subsequent fusion in the developing spine of young children, our institutional experience suggests otherwise in the overwhelming majority of our patients with long-term follow-up. This information can guide the caregivers of patients during preoperative discussions about long-term risks, especially in young children.
References
Ciaramitaro P, Massimi L, Bertuccio A et al (2022) Diagnosis and treatment of Chiari malformation and syringomyelia in adults: international consensus document. Neurol Sci. Published online June 15, 2021. https://doi.org/10.1007/s10072-021-05347-3
Massimi L, Peretta P, Erbetta A et al (2021) Diagnosis and treatment of Chiari malformation type 1 in children: the international consensus document. Neurol Sci. Published online. https://doi.org/10.1007/s10072-021-05317-9
Tam SKP, Brodbelt A, Bolognese PA, Foroughi M (2021) Posterior fossa decompression with duraplasty in Chiari malformation type 1: a systematic review and meta-analysis. Acta Neurochir 163(1):229–238
Strahle J, Muraszko KM, Kapurch J, Bapuraj JR, Garton HJL, Maher CO (2011) Chiari malformation Type I and syrinx in children undergoing magnetic resonance imaging. J Neurosurg Pediatr 8(2):205–213
Bell DF, Walker JL, O’Connor G, Tibshirani R (1994) Spinal deformity after multiple-level cervical laminectomy in children. Spine 19(4):406–411
Flynn JM, Sodha S, Lou JE et al (2004) Predictors of progression of scoliosis after decompression of an Arnold Chiari I malformation. Spine 29(3):286–292
Bekelis K, Duhaime AC, Missios S, Belden C, Simmons N (2010) Placement of occipital condyle screws for occipitocervical fixation in a pediatric patient with occipitocervical instability after decompression for Chiari malformation. J Neurosurg Pediatr 6(2):171–176
Bollo RJ, Riva-Cambrin J, Brockmeyer MM, Brockmeyer DL (2012) Complex Chiari malformations in children: an analysis of preoperative risk factors for occipitocervical fusion. J Neurosurg Pediatr 10(2):134–141
Yasuoka S, Peterson HA, MacCarty CS (1982) Incidence of spinal column deformity after multilevel laminectomy in children and adults. J Neurosurg 57(4):441–445
Ravindra VM, Iyer RR, Yahanda AT et al (2021) A multicenter validation of the condylar--C2 sagittal vertical alignment in Chiari malformation type I: a study using the Park-Reeves Syringomyelia Research Consortium. J Neurosurg Pediatr 1(aop):1–7.
Nagashima C, Kubota S (1983) Craniocervical abnormalities. Neurosurg Rev 6(4):187–197
Smoker WR (1994) Craniovertebral junction: normal anatomy, craniometry, and congenital anomalies. Radiographics 14(2):255–277
Brockmeyer DL, Spader HS (2015) Complex Chiari malformations in children: diagnosis and management. Neurosurg Clin N Am 26(4):555–560
CreveCoeur TS, Yahanda AT, Maher CO et al (2020) Occipital-cervical fusion and ventral decompression in the surgical management of Chiari-1 malformation and syringomyelia: analysis of data from the Park-Reeves Syringomyelia Research Consortium. Neurosurgery 88(2):332–341
Katsumi Y, Honma T, Nakamura T (1989) Analysis of cervical instability resulting from laminectomies for removal of spinal cord tumor. Spine 14(11):1171–1176
Ishida Y, Suzuki K, Ohmori K, Kikata Y, Hattori Y (1989) Critical analysis of extensive cervical laminectomy. Neurosurgery 24(2):215–222
Aronson DD, Kahn RH, Canady A, Bollinger RO, Towbin R (1991) Instability of the cervical spine after decompression in patients who have Arnold-Chiari malformation. J Bone Joint Surg Am 73(6):898–906
McLaughlin MR, Wahlig JB, Pollack IF (1997) Incidence of postlaminectomy kyphosis after Chiari decompression. Spine 22(6):613–617
Camino Willhuber GO, Bosio ST, Puigdevall MH, Halliburton C, Sola CA, Maenza RA (2017) Craniocervical spinal instability after type 1 Arnold Chiari decompression: a case report. Journal of Pediatric Orthopaedics B 26(1):80
Author information
Authors and Affiliations
Contributions
P.K. Conceptualization and design, data collection, analysis, and drafting of manuscript. M.E. Conceptualization and design, data collection, analysis, and drafting of manuscript. K.J.M. Study supervision, reviewing, and revising original draft. D.J.D. Study supervision, reviewing, and revising original draft. E.S.A. Study supervision, reviewing, and revising original draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Approval was obtained from the ethics committee of Mayo Clinic. The procedures used in this study adhere to the tenets of the Declaration of Helsinki. The parents of the pediatric patients included in this study consented to research authorization according to State of Minnesota.
Conflict of interest
No funding sources or conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kerezoudis, P., Everson, M.C., Miller, K.J. et al. Low occurrence of long-term subsequent fusion in pediatric patients following decompressive surgery for Chiari malformation: an institutional review. Childs Nerv Syst 38, 1455–1460 (2022). https://doi.org/10.1007/s00381-022-05550-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05550-3