Abstract
Anti-citrullinated peptide antibodies (ACPAs) play an important pathogenic role both at the onset and during the disease course. These antibodies precede the clinical appearance of rheumatoid arthritis (RA) and are associated with a less favorable prognosis, both clinically and radiologically. The objective of this work was to conduct a comprehensive review of studies published through September 2015 of ACPAs’ role as a predictor of the therapeutic response to the biological agents in RA patients. The review also includes summary of the biology and detection of ACPAs as well as ACPAs in relation to joint disease and CV disease and the possible role of seroconversion. The reviews of studies examining TNF inhibitors and tocilizumab yielded negative results. In the case of rituximab, the data indicated a greater probability of clinical benefit in ACPA+ patients versus ACPA− patients, as has been previously described for rheumatoid factor. Nonetheless, the effect is discreet and heterogeneous. Another drug that may have greater effectiveness in ACPA+ patients is abatacept. Some studies have suggested that the drug is more efficient in ACPA+ patients and that those patients show greater drug retention. In a subanalysis of the AMPLE trial, patients with very high ACPA titers who were treated with abatacept had a statistically significant response compared to patients with lower titers. In summary, the available studies suggest that the presence of or high titers of ACPA may predict a better response to rituximab and/or abatacept. Evidence regarding TNFi and tocilizumab is lacking. However, there is a lack of studies with appropriate designs to demonstrate that some drugs are superior to others for ACPA+ patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is an autoimmune disease that affects 0.5 % of the Spanish population [1]. Seventy percent of patients present autoantibodies (seropositive RA), mainly rheumatoid factor (RF) and anti-citrullinated peptide antibodies (ACPAs), which generally indicate a more serious illness compared with patients with seronegative RA. This indicates de facto that there are two different types of RA from the etiopathogenic and the evolutionary point of view [2].
Furthermore, apart from the role that RF plays in RA, ACPA is relevant to crucial aspects of RA. Because of their high specificity, ACPAs play a very important role in the diagnosis of the disease, are involved in pathogenesis, and are associated with a greater radiographic progression, the increased risk of pulmonary complications, and an increased risk of cardiovascular (CV) events [2–7].
However, despite the development of new biological therapeutic agents, there is a lack of robust scientific evidence to assessing the clinical response of biologic therapies in patients with ACPAs. Studies of rituximab (RTX) have yielded conflicting results that can be summarized as follows: seropositive patients, including those with ACPAs, are likely to have a better, although modest, clinical response than seronegative patients [8, 9]. Recently, some data for abatacept suggest the possibility that this drug will have greater effectiveness in ACPA+ patients. However, these data come from records or subanalyses of clinical trials, some of which were presented at conferences and others that were recently published [10–12].
This circumstance and the absence of a thorough review of all of the available biological agents, for which ACPA+ patients’ responses have been analyzed, have prompted us to review in detail the existing literature and to analyze the possible predictive value of the clinical response to biologic therapies according to the ACPA status (positive vs. negative) and ACPA levels changes.
Methodology
The project coordinator (EMM) selected 5 rheumatologists with expertise in RA and in the management of RA patients with biological therapies. These experts had also published scientific articles on this topic, including consensus documents. In addition to these characteristics, the panelists were selected for their geographical distribution (representing different regions of the country); efforts were made to ensure that they were as representatively distributed as possible.
A narrative search of articles published through September 2015 was performed to find studies that analyzed RA patients treated with any biologic therapy approved in our country, including (a) the predictive value of the therapeutic response of ACPAs and (b) the clinical value of seroconversion (defined as the change from ACPA+ to ACPA−).
One reviewer (EL) used clinical queries that included medical subject headings (MeSH) terms and free text in MEDLINE for the article search. Systematic reviews and meta-analyses, clinical trials, and observational studies were selected. There were no restrictions on language, and only articles including the drugs’ effects in humans were selected. This search was complemented by experts’ advice on the publications and other related works on this topic. The results were presented and discussed at a meeting of the panel of experts.
In this meeting, the literature addressing the clinical and the predictive value of the ACPAs response to different biological therapies was presented and discussed. Additionally, the sections, scope, and the format of the review document were agreed upon, and tasks were distributed. Each expert was responsible for drafting one or more sections of the review document. Once combined, the sections were circulated among the panelists for comments, corrections, and suggestions. The coordinator was responsible for editing the final document. When questions arose, the expert who was responsible for the section was contacted.
Antibodies in RA
Both the anti-IgG-Fc antibody (Ab) RF and ACPA are highly characteristic Abs of RA. There are other autoantibodies associated with RA, such as RA33, anti-calpastatin, ANCA, ANA, anti-collagen II, and anti-glucose-6-phosphate isomerase (GPI), but these are less informative than RF [13].
An important step in the study of RA autoimmunity was the discovery of the post-translationally modified Ab anti-protein. ACPAs have been used in the diagnosis of RA since the discovery of the anti-perinuclear factor [14] and anti-keratin Abs a few years later [15]. Both Abs recognize the same antigen, filaggrin [16]. Although many authors have recognized ACPAs testing’s diagnostic and prognostic value, its use never spread because the technique for detection was more laborious and less reproducible than RF detection [17–19]. A significant step was the discovery that the reactivity of these Abs depended on the presence of citrulline residues [20, 21].
The next step was the use of citrullinated proteins (filaggrin, fibrinogen, or myelin basic protein) to identify RA-specific anti-citrulline Abs; however, these proteins were difficult to isolate in large quantities and with sufficient purity [22, 23]. In the first generation of the assay, a citrullinated peptide derived from filaggrin was used [24]; while it was better than the previous methods for detecting anti-citrullinated peptide antibodies, it was less sensitive than RF. Because filaggrin is not localized in the synovium, other synthetic peptides rich in citrulline were assayed, leading to the discovery of the second-generation assay, which uses a cyclic peptide that exposes the epitopes (CCP2) more efficiently. This assay has a sensitivity of up to 80 % and a specificity similar to that of the previous generation [25]. Subsequently, other assays were developed that differed slightly in sensitivity and specificity but did not seem to perform better than the CCP2 assay [26, 27].
All of the anti-citrullinated protein Abs recognize a wide variety of citrullinated proteins and are thus currently known as ACPAs [28]. These recognized proteins include fibrinogen, vimentin, alpha enolase, the peptidyl arginine deiminase enzyme, or enolase derived from Porphyromonas gingivalis [3]. Although ACPAs generally cross-react with multiple citrullinated proteins and share little homology, such characteristics are not absolute [29].
Recently, anti-carbamylated protein antibodies have been described. These antibodies represent a post-translational modification that converts lysine to homocitrulline and that cross-reacts with ACPAs [30].
Citrullinated protein formation
Citrulline is a post-translational modification of arginine catalyzed by the peptidyl arginine deiminase (PAD) enzyme [31]. Typically, PAD is inactive because of very low concentrations of Ca2+. During apoptosis, there is an influx of Ca2+ into the interior of the cell, which activates PAD in a physiological process that causes the citrullination of intracellular proteins, thus facilitating their degradation. This reaction probably does not provoke an immune reaction because the neoantigens are not exposed to the immune system [32]. In the inflammatory processes, when cells die via necrosis, the cellular membrane is ruptured, and PAD is released into the extracellular space, where high concentrations of Ca2+ and citrullinated proteins exist. The inflamed synovium contains macrophages that express PAD2 and granulocytes that express PAD4; these enzymes cause the citrullination of extracellular proteins, such as fibrinogen [33], or intracellular proteins, such as vimentin [34]. However, the synovial citrullination of proteins is associated with inflammation in both animal models [35] and humans [36, 37] and is not specific for RA.
Infectious agents such as Porphyromonas gingivalis, a bacterial species directly related to the development of periodontitis, are capable of producing bacterial peptidylarginine deiminases causing the citrullination of proteins such as human fibrinogen and alpha enolase [38].
Although inflammatory processes are very common, only a small proportion of the population develops ACPAs, which are very specific to RA and are related to the pathogenesis of the disease [4].
ACPAs in the pathogenesis of RA
Several items of evidence link the presence of ACPAs to the pathogenesis of RA. The first is their high specificity: they appear infrequently and usually at low titers in other autoimmune diseases [25, 27, 39, 40]. The efficacy of selective B cell depletion in the treatment of RA provides evidence that favors the role of autoantibodies in the disease’s pathogenesis [41].
The second item supporting the link between ACPAs and RA is based on findings that ACPAs precede the clinical manifestations of the disease. In an animal model of collagen-induced arthritis, anti-collagen Ab and ACPA preceded the appearance of joint inflammation [42]. In healthy people, ACPAs precede the development of RA by several years [43–45], and very few individuals become ACPA+ after the clinical development of arthritis [46]. Recent studies have shown that these Abs appear gradually and that the recognized epitopes increase just before the onset of symptoms [47, 48]. This finding is interesting, but still poorly explained, as high ACPA titers in patients with arthralgias are a very important risk factor for the development of arthritis in the near future [49]. At the same time, it appears clear that only a small group of individuals who develop ACPAs will ultimately develop RA [49]. However, external factors, such as obesity and tobacco use, are predictive of the development of the clinical manifestations [50].
ACPAs in the classification of RA
There is a relationship between ACPA production and the presence of certain HLA-DR alleles associated with RA susceptibility, also called shared epitope (SE) [51, 52]. The association is located in the third hypervariable region of the β chain and is found mostly in the DRB*0101, *0102, *0401, *0404, *0405, *0408, *1001, and *1402 alleles [53]. In HLA-DRB1*0401 transgenic mice, the conversion of arginine to citrulline in selected peptides increases their affinity for HLA and induces the very efficient collaboration of T lymphocytes in the production of Abs [54].
In several cohorts of patients with RA, it has been shown that when patients are stratified by the presence or absence of ACPA, HLA-DR alleles with SE are found in the presence of ACPAs and not with ACPA− RA [55–57], which indicates that the HLA-DR alleles with SE are not associated with RA in general, but with a phenotypic subtype defined by the presence of ACPAs [56, 57].
Another risk allele for the development of RA and the production of ACPAs is the protein tyrosine phosphatase, non-receptor type 22 (PTPN22), which is involved in the stimulation, activation, and differentiation of T lymphocytes [58].
ACPA in joint disease
The fact that ACPAs appear years before the onset of symptoms suggests that the production of Abs and the development of the disease are different processes. A theory with several steps has been proposed as a model for RA pathogenesis [4] (Fig. 1).
Model for the pathogenesis of rheumatoid arthritis: the exposure to certain environmental factors (e.g., smoking, periodontitis due to an infection with Porphyromonas gingivalis or silica dust exposure) leads to local protein modification by citrullination and/or carbamylation. In genetically susceptible individuals, inflammatory process caused by these factors elicits an immune response to citrullinated and/or carbamylated proteins. A secondary or non-related event associated with damage and inflammation in synovial joints results in citrullination and/or carbamylation of synovial proteins with the formation of immune complexes which will boost the inflammatory process, leading to the development of arthralgia first and then arthritis
The first step is the production of ACPAs. The citrullination of proteins, a physiological process that is characteristic of RA, represents the capacity to initiate an immune response against these antigens. Until recently, the roles of genes, environmental factors, and autoimmunity in the etiology of RA were studied independently. In this model, it is necessary to understand how the known risk factors interact with genes in the development of the disease. Some risk factors associated with the development of RA and ACPAs are known, such as tobacco use, occupational exposure to silica dust, and periodontitis [59, 60]. A case–control study showed that the appearance of ACPAS was associated with the presence of HLA-DR alleles with SE in a dose-dependent manner and that tobacco was a risk factor for ACPA+ RA but not for ACPA− RA. This study also showed that ACPA+ RA was not completely dependent on SE. [58]. The importance of this work is that the authors demonstrated that tobacco is capable of initiating the citrullination of proteins in the lungs and that in the local inflammatory environment, it can act as a trigger for the development of ACPAs [58]. Additionally, a similar interaction between exposure to silica dust has been described [59], while periodontitis, especially as a result of Porphyromonas gingivalis and its capacity for causing citrullination, might, to some extent, be related to the initiation of the autoimmune process that will ultimately develop into RA in some patients [60].
Once the ACPAs have been produced, it is necessary to explain how an organ-specific disease, such as RA, can be produced by non-organ specific Abs. Research has shown that the Abs and immune complexes are deposited in the joints but only persist and initiate an inflammatory reaction if the antigen is located in the joint [4]. This could explain how ACPAs can present many years before the onset of symptoms and not produce arthritis until the occurrence of an intercurrent episode that produces a small synovial lesion with the citrullination of synovial proteins.
Finally, a third step is needed for the disease to become chronic. The vast majority of immune responses are self-limiting because of autoregulatory mechanisms. RA is known to be a polygenic disease in which HLAs confer only part of the known risk [61]. Among the many genes that have been associated with RA, a polymorphism of the PTPN22 gene is one that has been replicated most consistently [62, 63]. The association between the presence of ACPAs and the C1858T polymorphism of the PTPN22 gene is fully specific for RA [64].
For the clinician, a useful test is one that has high sensitivity and specificity, detects the majority of patients with few false positives, is positive in the initial stages of the disease, thus facilitating early diagnosis, and is capable of predicting disease outcomes that are relevant for the clinician. ACPAs have all of these characteristics [65]. A systematic review of the literature that included 151 articles that used the anti-CCP2 test was published in 2010. The sensitivity and specificity of ACPAs in RA were 57 % (95 % CI 51–63 %) and 96 % (95 % CI 93–97 %), respectively. Anti-CCP2 had a higher specificity than RF (96 vs. 86 %), with a similar sensitivity. No evidence in the analysis indicated that the combination of the anti-CCP2-positive and RF assays had a higher diagnostic yield than the CCP2 assay alone [66].
ACPAs’ importance for the clinician lies in its relationship with distinct disease outcomes. Approximately 50–70 % of RA patients are ACPA+ [29], and although the ACPA+ and ACPA− patients present some similar clinical characteristics in the initial stages of the disease [5], the subsequent clinical course is different; furthermore, histological differences have been described wherein ACPA+ patients have higher lymphoid infiltration and less fibrosis [67]. Some extra-articular manifestations and comorbidities are clearly influenced by the presence of ACPA; for example, the risk of suffering CV [6] or pulmonary disease [7] is increased in these patients, but it appears that RF and not ACPA is associated with extra-articular manifestations, such as nodules and vasculitis [68].
It is likely that the most important clinical repercussion is that ACPA+ patients have a more destructive disease course [5, 69–73], and the ACPA titer has been linked to the potential of these autoantibodies to cause bone damage [74, 75]. However, all of these findings have also been described in relation to RF. Given the considerable overlap of the effects of these two autoantibodies in RA patients, it is difficult to separate their effect on disease characteristics. Both RF and ACPA are associated with a more active disease, which partly explains the structural deterioration and which requires more intense treatment [73]. Recently, it has been suggested that the presence of RF is significant to the development of erosions when ACPA is present [76].
The involvement of ACPA in bone damage
Synovitis is the principal trigger for bone loss in RA. Synovitis produces proinflammatory cytokines, which are very effective in the activation and maturation of osteoclasts. These cytokines induce osteoclast differentiation either directly or indirectly by increasing the expression of the RANK ligand, which explains the abundance of osteoclasts in inflamed joints and especially at erosion sites.
While it is clear that inflammation is a risk factor for bone destruction, the impact of autoimmunity, in this case the presence of ACPAs, is another important factor [5, 70, 73, 77–79]. In addition to local bone destruction in the form of erosions, patients with RA have a greater loss of trabecular bone. The presence of ACPAs is a risk factor independent of bone resorption [80–82], which suggests that autoimmunity actively contributes to bone loss, both focal and generalized. A recent study showed that healthy but ACPA+ people had greater bone loss in metacarpal bones, especially at the cortical level, compared with controls, suggesting that ACPAs have a direct role in bone loss that is independent of inflammation [83].
One recently published explanation for these findings showed that purified ACPAs from patients with RA recognize citrullinated vimentin and were capable of inducing the differentiation of mononuclear cells into osteoclasts and directly activating bone resorption [84]. The expression of citrullinated vimentin in osteoclasts is caused by PAD enzyme expression (2 and 4) in these cells, and the expression of this protein on the cell surface makes them accessible to autoantibodies that are capable of activating the differentiation of osteoclasts.
These findings provide new insights into the development of bone lesions in RA. The preclinical phase, which is marked by the presence of autoimmunity (i.e., the presence of ACPAs), induces changes in and activation of osteoclasts even before clinical manifestations appear. The presence of synovitis, which is associated with the development of various proinflammatory cytokines capable of activating the osteoclasts, increases previously activated process [85].
ACPAs and CV disease in RA
RA is a chronic inflammatory disease prototype characterized by increased morbidity and CV mortality compared with the general population of the same age and sex [86–88]. This increased incidence of CV events is the result of a process of accelerated atherosclerosis [89–92]. It has been demonstrated that both an altered immune response and the proinflammatory state that characterizes patients in the early stages of the disease constitute important pathogenic factors of vascular dysfunction in these patients [93].
When establishing the CV risk of a patient with RA, it is important to determine whether there are markers that can identify patients who face an increased risk of experiencing such events. Carotid ultrasound studies have shown a higher frequency of atheromatous plaques in RA patients with extra-articular manifestations [94]. This finding has great impact because the presence of ultrasonographic morphological alterations in the carotid artery is a true reflection of the existence of underlying atherosclerotic disease, which is primarily associated with ischemic heart disease and stroke.
In addition to clinical data that may indicate an increased CV risk, it is important to identify serological markers that may be useful for identifying groups with an increased CV risk. Markers such as elevated levels of angiopoietin-2 or osteoprotegerin are elevated in patients with RA who experience CV events [95, 96], and they also correlate with a higher frequency of atheromatous plaques in the carotid artery [97].
Furthermore, the European League Against Rheumatism (EULAR) guidelines for CV risk management confer greater CV risk when the patient presents RF or ACPA positivity [98]. This guideline has practical clinical implications because these two serological tests are routinely used in everyday clinical practice.
In this section, we will focus on establishing evidence supporting the possible role of ACPA in the development of CV disease in RA patients.
Clinical evidence of an increased risk of CV events associated with ACPAs
In a Madrid cohort, Lopez-Longo et al. discovered that patients with ACPA+ RA developed ischemic cardiopathy more frequently than those who were ACPA− (6.5 vs. 2.6 %, odds ratio 2.58). Furthermore, ACPA positivity was associated with a higher mortality rate (11.2 vs. 6.8 %, hazard ratio 1.72). A multivariate analysis of their cohort also demonstrated that the development of ischemic cardiopathy was independently associated with ACPA positivity (RR = 2.8, p = 0.009) [6].
ACPA involvement in the subclinical atherosclerosis process in patients with RA
It has been postulated that the development of subclinical vascular disease may be linked to ACPAs in patients with RA [99]. Consistent with this, an association between the presence of ACPA and a greater presence of subclinical atherosclerotic disease has also been observed [100].
Endothelial dysfunction is the initial process in the development of atherosclerosis, and impaired endothelial function in patients with RA has been linked to ACPA positivity [101]. Sokolove et al. [102] demonstrated via immunohistochemistry that citrullinated proteins were present within the damaged endothelium of atherosclerotic plaques.
When defining CV risk (and therefore predicting an increased susceptibility of developing CV events), a number of noninvasive subclinical markers may be useful for predicting future CV events. In the English-language literature, these markers are described as “surrogate markers” of CV disease. Such surrogate markers have proven useful in both the general population and RA patients for predicting the risk of CV events. One such marker is carotid ultrasound. The use of this technique verified that the carotid intima-media thickness (cIMT) predicts the risk of future CV events in patients with RA [103]. In line with this observation, it is known that ACPA positivity is associated with an increased cIMT on carotid ultrasound [104–106]. Given these data, Vazquez-Del Mercado et al. [107] analyzed the relationship between ACPA levels, inflammation markers, and the presence of subclinical atherosclerosis, determined using cIMT values, in a cohort of patients with RA who presented no comorbidities. In addition to confirming previous data that showed an increased cIMT in patients with RA without classic CV risk factors compared to controls [94], the stratification of patients with RA according to ACPA positivity showed that the ACPA+ patients had cIMT values that were significantly higher than those of the ACPA− patients [107]. Furthermore, multivariate studies revealed that the clinical variables that were positively associated with the cIMT were C-reactive protein (CRP) and ACPA [107]. This study suggests that ACPAs are markers of a poor clinical prognosis, and their strong correlation with the cIMT supports that value’s association with atherosclerotic disease.
Role of ACPAs in CV disease development
Barbarroja et al. [108] analyzed the specific role that ACPAs have in the pro-oxidative, inflammatory, and proatherogenic profiles observed in leukocytes from patients with RA. These authors demonstrated that elevated titers of ACPA were associated with the altered expression of prothrombotic and inflammatory markers. A high degree of oxidative stress was also associated with abnormal cIMT values in patients with RA [108]. Based on gene expression analysis, these authors ascertained that lymphocytes played a fundamental role in altering the inflammatory profile. The monocytes were responsible for the prothrombotic and atherogenic state, and the neutrophils were involved mainly in the pro-oxidative events. Furthermore, in vitro treatment with purified ACPAs reproduced this previously described profile and promoted leukocyte activation [108]. This study verifies that ACPAs act as direct inductors of a pro-oxidative state and of the inflammatory and pro-atherogenic profile of the lymphocytes, monocytes, and neutrophils that play a role in CV disease in patients with RA [108].
Consistent with the above-mentioned findings, a recent study suggested that the excess CV risk observed in patients with RA is caused in part by immunocomplexes of antibodies against citrullinated proteins that perpetuate inflammation and the progression of atherosclerotic plaques on the local level [109]. Nonetheless, although there is the possibility that immunocomplexes linked to ACPA play a predominant role in the progression and local inflammation of atherosclerotic plaques, these data need to be replicated in an independent cohort.
In conclusion, ACPAs have been linked to an increased risk of subclinical atherosclerotic disease and CV events. Recent studies indicate that ACPAs have a direct pathogenic role in the development of atherosclerotic disease in patients with RA. Immunocomplexes linked to ACPAs played a predominant role in the progression and local inflammation of atherosclerotic plaques in patients with RA.
Predictive value of the response to ACPAs by different biological agents
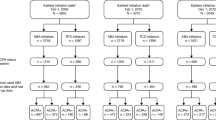
Tables 1 and 2 show a brief summary of some of the articles that are described and referenced in the review.
The predictive value of ACPAs status and levels in response to TNF antagonists
ACPAs predict the evolution of undifferentiated arthritis into RA [110–116]. A systematic review of the value of the second-generation ACPAs concludes that these Abs have a high predictive value for the development of RA in both healthy individuals and in patients with undifferentiated arthritis [117]. However, their predictive value for other outcomes, particularly the response to treatment, is questionable [39, 70, 78, 79, 117–129]. The analysis of the published results regarding the predictive value of several important demographic, clinical, serum marker, and genetic markers shows that the results cannot be generalized because of the heterogeneity of the studies [130]. As mentioned in the previous section, there is a relationship between the presence of ACPAs and RF [5, 44, 131].
RF status predicts a better response to rituximab and tocilizumab in RA [132], but not to abatacept and TNF (tumor necrosis factor) antagonists [132, 133]. However, the value of ACPAs for predicting the response to TNF antagonists is a subject of dispute. A recent systematic review of the predictive value of the response of IgM-RF status and of ACPA as a response-predictive variable in patients with RA identified 10 studies with infliximab, 8 with adalimumab, 6 with etanercept, and 1 with golimumab [134]. The mean duration of disease prior to treatment with the biologic was between 5 and 12 years. The ACPA status did not predict the EULAR, Disease Activity Score 28 joints examined (DAS28), or ACR20 response. However, the heterogeneity of the analyses was high, and only two studies were of high quality. A sensitivity study that eliminated conflicting results did not change the predictive value results, but the causes of the heterogeneity were not identified.
The value of the changes in levels has been also reported. In a randomized 3-month study of 52 patients with long-duration RA who were treated with etanercept combined with disease-modifying anti-rheumatic drugs (DMARDs), or with DMARDs alone, the levels of ACPA and RF decreased more markedly in the first group, and this finding was consistent with a greater reduction in clinical activity [135]. In another prospective study examining a 24-week treatment with adalimumab in 72 patients with RA who had not responded to DMARDs, those patients who met the American College of Rheumatology 20 % improvement criteria (ACR20) for response showed a significant decrease in ACPA levels; however, no such decrease occurred in those who did not achieve the same level of response [126]. This result was similar to that obtained in 188 consecutive patients with Abs with IgM-RF and ACPAs who were treated with adalimumab and followed for 28 weeks [136]. Additionally, in another prospective study of 12-month duration in 57 patients who had not responded to MTX (methotrexate) and were treated with adalimumab, the IgM-RF and ACPA levels decreased in parallel to clinical improvement during the observation period. These changes did not occur in a parallel group of patients with stable clinical activity who were treated with MTX [137]. The results observed with etanercept and adalimumab differed from those observed in studies of infliximab use in patients with variable disease durations [135, 138, 139]. A recent systematic review of the predictive value of the response of IgM-RF status and of ACPA as a response-predictive variable in patients with RA identified 10 studies with infliximab, 8 with adalimumab, 6 with etanercept, and 1 with golimumab [134]. The mean duration of disease prior to treatment with the biologic was between 5 and 12 years. The ACPA status did not predict the EULAR, Disease Activity Score 28 joints examined (DAS28), or ACR20 response. However, the heterogeneity of the analyses was high, and only two studies were of high quality. A sensitivity study that eliminated conflicting results did not change the predictive value results, but the causes of the heterogeneity were not identified.
In summary, the ACPA status in RA patients upon the initiation of therapy with TNF antagonists appears not to predict the response to treatment. However, in several studies, in patients with a long disease evolution and a favorable response, the antibody levels decrease in parallel to the improvement of the disease.
The value of ACPAs in predicting the response to rituximab
As we can infer from the above-mentioned robust evidence, different proteins that are present in the synovial tissue or even in the pulmonary tissue can be citrullinated [140]. They might become targets for B cells in RA and undifferentiated arthritis triggering a specific antibody response with pathogenic potential [141]. Rituximab (RTX) is a monoclonal Ab with high affinity for the CD20 molecule expressed in B and pre-B cells. RTX has demonstrated efficacy in RA that is linked to the rapid depletion of circulating B lymphocytes until they begin to reconstitute 6–9 months later [142].
The first randomized placebo-controlled clinical trials in patients refractory to MTX [143] or to DMARDs/biologics [144] have already indicated a better response to RTX in RF-positive patients. However, the REFLEX trial, which included patients with an insufficient response to anti-TNF, showed no significant differences between RF+ and RF− patients in the ACR20 response at 24 weeks [145]. These discrepancies, combined with knowledge about the mechanisms of action of RTX, have led to an extensive exploration of serological status (RF+ and/or ACPA+) as a predictor of the response to RTX, including subanalyses of the first pivotal trials.
The first of these subanalyses in seronegative patients indicated that this subpopulation’s response was not significantly different from their response to placebo. However, this finding was likely related to an insufficient sample of seronegative patients [144–146] and/or a high response in the placebo group [144]. In an attempt to correct this limitation, a new analysis of the REFLEX trial with a more exigent measure of efficacy (the American College of Rheumatology 50 % improvement criteria, ACR50) demonstrated that the presence of Abs with any isotype of RF and/or IgG anti-CCP, together with an elevated CRP, identified a subgroup of patients with a greater response to RTX [147]. These findings were replicated in samples of patients with early RA and an insufficient response to MTX in the SERENE trial [148], which previously had not successfully demonstrated a greater response among seropositive patients through week 48 [148].
In the same sense, the results of the IMAGE study after 102 weeks demonstrated that in patients without previous MTX therapy, a higher percentage of RF+ and/or ACPA+ patients achieved an ACR50 response with RTX and suffered minor structural damage compared with seronegative RA patients [149]. Again, the limited sample of seronegative patients leads the authors to interpret the high placebo response rate in this population with caution.
In an attempt to correct this situation, Isaacs et al. conducted a meta-analysis published in 2013 [8] that included four randomized placebo-controlled clinical trials—REFLEX [145], DANCER [144], SERENE [148], and IMAGE [146] and gathered 2177 patients with RA (1416 RTX and 761 placebo; of them, 1253 and 681 were seropositive, respectively). The meta-analysis of global data according to a fixed effects model included 2139 patients, with a similar proportion of seropositive patients (RF+ and/or ACPA+) in each of the four studies. The demographic and baseline disease characteristics of the included populations were similar, and they included patients who had never received MTX [146], those who were refractory to MTX or other DMARDs [144, 149], and those who were previously refractory to biologics [144, 145]. The overall effect of the model indicates that the response to RTX, as measured by the reduction in the DAS28 based on erythrocyte sedimentation rate (DAS28-ESR) at week 24, is higher in seropositive patients, but the effect of ACPA+ serological status is modest. In ACPA+ patients, RTX (n = 1243) achieved a reduction in 0.24 units (95 % CI −0.45 to −0.04), which was not observed in the placebo group’s (n = 640) with a reduction in 0.02 units (95 % CI −0.18 to 0.23). The results using the ACR20 and ACR50 criteria were similar. There was no relationship between the RF and ACPA titers and the magnitude of the effect, nor did one individual serotype dominate. Furthermore, the impact of the positive serotype on the response to RTX in different studies is not homogeneous. The greatest effect on the reduction in the DAS28 was observed in patients who were refractory to anti-TNF in the REFLEX study. The effect was modest in those not exposed to MTX (IMAGE study), and no effect was observed in the SERENE and DANCER studies. An additional meta-regression analysis with individual patient data identified some covariables that influence heterogeneity, but were not able to explain differences across all the studies. Thus, the higher baseline values for the Health Assessment Questionnaire (HAQ) and/or pain and/or the number of swollen joints were cited to explain the better response to RTX among seropositive patients who had not been exposed to MTX. When the groups were stratified for low values of these covariates, only the seropositive patients who were refractory to anti-TNF (REFLEX study) obtained an additional benefit compared to the seronegatives. In any case, the conclusions of this meta-analysis were that in terms of the overall effect of the study, the seropositive patients responded better to the RTX than the seronegatives did, although the difference was modest.
In agreement with the conclusions of this meta-analysis, a recent systematic review [9] described very similar findings. The review included a meta-analysis, this time with a random effects model, of the DANCER, IMAGE, and REFLEX studies, and incorporated the SUNRISE study of patients refractory to anti-TNF [150].
Although the methodological quality of both meta-analyses was high, the included trials were not designed to demonstrate that ACPA+ serological status is a predictor of the response to RTX, and in many of the trials, outcomes were measured before sufficient time had elapsed to observe an effect of RTX [151]. Both meta-analyses agreed that the effect was discrete and heterogeneous.
Alongside these findings in clinical trials, the capacity of ACPA to predict a greater response to RTX has also been identified via multivariate analysis in an open multicenter trial [152]; the collaborative CERRERA study, which includes patients with RA from ten European registries [153]; and several prospective observational studies [154, 155]. In a retrospective observational study, statistical significance was only obtained with high titers of ACPA [156]. Conversely, in another retrospective multicenter study, only positivity for RF and not for ACPA predicted the predetermined outcomes [157].
The differences in the outcomes used as the response variable (including the time frame) or in the predictor variable could partly explain some contradictory data; other explanations include the heterogeneity of the populations studied and the limited presence of ACPA− patients. In summary, although there ACPA− patients may benefit somewhat from RTX treatment, the data indicate that seropositive patients are more likely to experience clinical benefit. Until new data in seronegative patients are available, it appears reasonable to maintain the recommendations of the 2011 consensus document for the use of RTX [158], which advocates the use of another mechanism of action, such as a first-line biologic, in this subpopulation.
ACPA seroconversion as a predictor of response
Evidence indicates that the efficacy of RTX in RA depends not so much on the dose used as on the depletion of circulating B lymphocytes [159] and the reduction in both circulating and bone marrow memory B cells [160]. Additionally, the analysis of the effect of RTX in synovial cell populations shows that the reduction in plasma synovial cells predicts clinical improvement at 24 weeks in responder patients and coincides with a significant decline in serum IgM-RF titers at 24 weeks or in ACPA at 36 weeks [161]. The kinetics of the responders’ clinical and serological response suggests that the benefit of RTX may result in part from an indirect effect on the plasma cells associated with the production of pathogenic autoantibodies.
However, the modulation of ACPA titers by RTX has been explored in few studies, often with very limited sampling and considerable heterogeneity in design, population, and treatment regimens; furthermore, ACPA modulation was not always studied in relation to the clinical response [162–168]. The follow-up exceeded 6 months in only two of the studies [162, 168]. Although reductions with respect to the base level were generally observed over time, only Cambridge et al. [162] found significant titer reduction in responder patients (8/12 ACPA+), with an ACR20 response at 6 months. In 7 of these responders, relapse was accompanied by a variable recovery of ACPA titers [162]. A later study (n = 15) failed to replicate these results [163]. In another recent study of 77 patients (75 % ACPA+), Vancsa et al. [168] describe a progressive sustained reduction in serum ACPA levels that was only meaningful after 2 treatment cycles (i.e., starting at 12 months) and was not correlated with the DAS28. A recent article suggests that the restrictive IgG seropositivity against epitopes of modified citrullinated vimentin, along with the decrease in its titers, can select RTX responder patients at 24 weeks [169]. Further well-designed studies are needed to determine the modulation of ACPA serum levels as predictors of RTX response.
ACPAs and tocilizumab
Tocilizumab (TCZ) is a humanized monoclonal antibody directed against the IL-6 receptor. It impedes IL-6 from binding to its receptor and, therefore, from signaling.
Among its multiple immunomodulatory effects, IL-6 promotes the differentiation of activated B cells into immunoglobulin-producing cells and has been involved in the pathogenesis of RA, Castleman syndrome, and other diseases with significant B cell lymphoproliferation [170]. However, information on the effect of TCZ in relation to ACPA status is limited, and only two prospective observational studies have explored the ability of these Ab to predict response in patients with RA. The first study analyzed remission, as measured with the Clinical Disease Activity Index (CDAI) at 24 weeks, in 58 patients with evolved RA; more than 40 % of the patients were refractory to anti-TNF, and 91 % were positive for RF and ACPA [171]. The univariate and logistic regression analyses showed that the only variable associated with CDAI remission was high titers of IgM-RF, but not of ACPA. Pers et al. [172] published similar findings for ACPA in a recent multicenter French study that recruited 204 patients with evolved RA, most of them previously exposed to biologics. In that case, the outcomes studied were EULAR response and remission at 24 weeks, but neither RF+ (in 71 % of the patients) nor ACPA+ (65.6 % of the patients) status was able to predict the response in the univariate or multivariate analysis. Therefore, current data do not support a different response to TCZ in patients with basal ACPA+ serological status. We have not found information on TCZ’s effect on the modulation of ACPA levels.
Abatacept and ACPAs
In the registry studies of abatacept in RA patients who failed to respond to MTX and TNF antagonists according to AIM and ATTAIN assays, respectively [173, 174], the frequency of ACPA positivity was not detailed, nor did the studies specifically analyze whether there was an association between clinical response and ACPA status. In other studies of the efficacy of abatacept in RA, most of the included population was ACPA+, so differences between populations with and without autoantibodies could not be studied. This was the case in the AGREE study, in which the higher efficacy of abatacept combined with MTX compared to MTX monotherapy was examined in early RA [175]. In some studies, the presence of ACPAs was an inclusion requirement; such was the case in the ADJUST trial [176], a randomized, double-blind comparative study of abatacept (treatment for 6 months) versus placebo in ACPA+ patients with undifferentiated arthritis. This study found that after 1 year of follow-up, 46 % of the patients treated with abatacept completely fulfilled the criteria for RA (ACR 1987), a lower percentage than those treated with placebo (67 %), although the differences did not reach statistical significance. The same happened in the AVERT study, which analyzed the efficacy (clinical remission, DAS28-CRP < 2.6) of abatacept + MTX versus abatacept and MTX monotherapy in patients with early RA at 1 year and at 18 months after 6 months of totally abandoning therapies (clinical remission with no drugs, or drug-free remission). In this study, 100 % of the patients were ACPA+ [177]. A recent systematic review and meta-analysis of three clinical trials with abatacept concluded that the presence of RF was not associated with greater clinical efficacy, but no data were based on the presence of ACPAs [132].
Thus, none of the randomized controlled trials of abatacept attempted to determine whether there is an association between ACPA status and clinical response. The first evidence that abatacept shows better efficacy rates in the ACPA+ population was described in an observational investigation of the French Orencia and Rheumatoid Arthritis (ORA) registry [110]. The ORA registry is a prospective registry that analyzes the efficacy and safety of abatacept in RA, starting in 2008. The study analyzed all patients treated with abatacept who had a minimum follow-up of 6 months (773 patients). It is worth noting that the included patients were selected from routine clinical practice, and the authors emphasize that only 21 % of them had fulfilled the inclusion criteria for clinical trials for drug indication registry. A total of 72.5 % of the patients were positive for RF, and 70.2 % were ACPA positive. Only 11 % of the patients had received prior treatment with TNF antagonists. A total of 59.1 % of the patients obtained a EULAR response at 6 months (20.4 % good and 38.7 % moderate). The RF frequency among responders was 75.6 %, compared with 66.7 % of the non-responders (p = 0.03); the ACPA+ frequency was 75.9 % among the responders versus 62.2 % among the non-responders (p < 0.001). In the multivariate analysis adjusted for DAS28 and CRP, the presence of ACPA was associated with a EULAR response with an odds ratio (OR) of 1.9 (95 % CI 1.2–2.9), but no similar results were associated with the presence of RF (OR of 1, 95 % CI 0.6–1.6). The authors also analyzed the retention rate of abatacept, a surrogate marker of the effectiveness of the drug, and found that it was higher in ACPA+ patients than in ACPA− patients (72.5 vs. 62.4 %, p = 0.02); no such differences were observed for RF. A greater reduction in the dose of glucocorticoids was also observed in both RF+ or ACPA+ patients compared to those without autoantibodies. This study of routine clinical practice is the first to definitively report a higher rate of clinical response and drug retention at 6 months in ACPA+ patients treated with abatacept.
This higher retention rate of abatacept in ACPA+ patients was also demonstrated in an analysis of a prospective multicenter clinical practice study, ACTION, that included patients treated with abatacept after the failure of TNF antagonists and studied the factors that predicted the retention of the biologic drug [178]. A total of 865 patients were analyzed, and the multivariate analysis showed a decreased risk of abatacept discontinuation in ACPA+ patients compared with ACPA− patients: hazard ratio (HR) of 0.55 (95 % CI 0.4–0.75). However, differences related to the patients’ origin (e.g., the Italian and Greek patients were less likely to discontinue treatment than, for example, the Germans) were observed. The failure of two or fewer TNF antagonists was also associated with greater continuation of abatacept in this study.
There are no other studies published to date on the possible association between the presence of ACPAs and the efficacy of abatacept, although there are preliminary communications, presented at congresses and published in abstract form, with results that go in the same direction as the two aforementioned studies; namely, they report a greater effectiveness of abatacept in ACPA+ patients. In one study [11] that analyzed 9 European registries, including the Spanish registry BIOBADASER, a total of 3641 patients (5475 patients/year) treated with abatacept were identified. Of these patients, there was information about RF status for 69.6 % and about ACPA status for 46 %. The primary objective was the retention rate of the drug and its association with the positivity of these autoantibodies. RF and ACPA positivity was associated with better survival of the drug, with HRs (95 % CI) for the suspension of abatacept for any reason of 0.8 (0.73–0.94) and 0.79 (0.69–0.82), respectively, and for inefficiency of 0.70 (0.60–0.81) and 0.69 (0.58–0.82) for the presence of RF and ACPAs, respectively. However, although the EULAR responses at 1 year were numerically higher in RF+ and ACPA+ patients, these differences did not reach statistical significance.
The AMPLE study is a randomized trial comparing the efficacy of abatacept with that of adalimumab, both in combination with MTX. No differences were observed between the two drugs in different clinical efficacy parameters or in the kinetics of response or the radiologic progression [179]. A newly published subanalysis of this study reported that patients treated with abatacept who had very high basal levels of ACPAs (upper quartile) had a statistically significant decrease in the DAS28 and CRP compared with patients with lower ACPA levels who were treated with abatacept. This outcome was not observed for adalimumab [12].
Moreover, three Japanese studies showed some discordant results. In a recently published study of clinical practice conditions, high RF titers were associated with a major clinical response in patients treated with abatacept and no change in those treated with tocilizumab. However, ACPAs were not analyzed in this study [180]. In another study that included only a small number of patients treated with abatacept (n = 60), a higher rate of remissions occurred in RF+ patients compared to RF− patients, but no association was found with ACPA status [181]. However, in the ABROAD study [182], which aimed to determine the factors that predicted clinical remission in patients treated with abatacept who had not previously received biologic therapy, an association between ACPA status and a better clinical response was found. In this prospective study of clinical practice, 155 patients with RA were included, and clinical remission rates were analyzed using the Simplified Disease Activity Index (SDAI; 3.3), as a function of the presence and concentration of ACPAs: low titer (<3 times the normal limit), high (<22 times), and very high (>22 times). SDAI remission was only observed in 16 % of the patients, and only two variables were associated with its presence: (a) a short disease duration (<1 year) and (b) a very high ACPA titer (OR 4.4, 95 % CI 1.38–15.3). The presence of high or low titers was not associated with higher indices of remission.
An interesting aspect to consider is the possible effect of the biologic treatments, and abatacept in particular, on the evolution of ACPA titers after the initiation of treatment and whether this evolution could have clinical implications. A recently published Italian study with a small sample of patients with RA (n = 30) demonstrated a reduction in the levels of immunoglobulins, RF, and ACPA (both IgG and IgA) after 6 months of treatment with abatacept. This decrease was only significant in patients who achieved clinical remission. Seroconversion (from positive to negative) was infrequent for ACPAs (7 %) and more frequent for RF (from 23 to 31 %, depending on the isotype) [183]. At the 2014 ACR congress, the results of a subanalysis of the AVERT study [177] that analyzed the impact of abatacept on different antigenic specificities and isotypes (IgA, IgG, IgM) of ACPA after the initiation of treatment were reported. A reduction in all ACPA isotypes and of the specificities was observed after 1 year of treatment for all three treatment branches; however, these reductions were most evident in the group treated with abatacept + MTX when compared to the groups treated with monotherapy. The authors concluded that abatacept can have an effect on the maturation of the response to ACPAs in patients with early RA and that this could alter the course of the autoimmune process in this disease [184]. Recently, at the 2015 EULAR congress, the data from a subanalysis of this study were presented; these data verified that ACPA+ patients with the IgM isotype respond more favorably to abatacept. Particularly interesting were the highest observed remission rates, particularly in those patients in whom the IgM isotype antibodies become negative with treatment; however, this change did not affect the overall negativization of ACPAs. A total of 61.5 % of the patients treated with abatacept + MTX in whom the ACPA IgM isotype became seronegative were in clinical remission at 12 months of treatment, compared with 41.5 % of the patients who did not experience seroconversion. These differences were not demonstrated in the patients who were assigned to treatment with MTX monotherapy [10]).
This probable association between the presence of ACPA and the greater clinical efficacy of abatacept and its possible effect on the maturation of the immune response to these autoantibodies serves to underscore abatacept’s mechanism of action. The inhibition of T lymphocyte activation through costimulatory signal blocking would have relevant effects on the B lymphocytes and plasma cells responsible for antibody production. The production of different immunoglobulins (antibodies) by the B lymphocytes develops after the antigen presents in the lymphoid tissues, which requires the help of the T lymphocytes [185]. The production of ACPAs by the B lymphocytes depends on the activation of antigen-specific CD4+ T helper cells. This activation requires costimulation signals that result from the binding of the T lymphocyte receptor CD28 with CD80/CD86 on antigen-presenting cells, which is blocked by abatacept [186]. A Japanese study confirmed that this drug reduces the CD25+ (a marker of lymphocyte activation) proportion of the T helper lymphocytes (CD4+), but only in ACPA+ patients [187]. In addition, these T lymphocytes are more activated in ACPA+ patients who respond to abatacept than in non-responders [187]. Moreover, a significant decrease in antibody-producing memory B lymphocytes has been shown in patients treated with abatacept [182].
Definitively, the results of different clinical studies that analyze the relationship between the presence of ACPAs and clinical response suggest greater efficacy and/or retention of abatacept in ACPA+ patients in concordance with the mechanism of action of this biologic agent. Preliminary data suggest that the presence of ACPAs and their concentrations, isotypes, and behavior (decline of the concentration) after the initiation of abatacept therapy may be relevant to the effectiveness of this biologic agent. However, the results of the majority of the studies are not published and are only communicated at congresses; furthermore, most are observational studies that are neither controlled nor randomized or are subanalyses of clinical trials, which calls for caution about reaching definitive conclusions.
Discussion
ACPAs have considerable clinical relevance in the diagnosis of RA. Their specificity is superior to that of RF (96 vs. 86 %); furthermore, ACPA-positive patients have a more aggressive clinical course with an increased risk of pulmonary and CV complications. In contrast, RF is strongly linked to extra-articular manifestations [2–7].
ACPAs (and RF) may be present for years before the disease onset. However, it should be noted that not all people with these Abs develop RA. In a recent 5-year study, 819 healthy relatives of 252 RA patients were studied. Of these, 1.3 % were positive for RF and anti-CCP2, 1.4 % for anti-CCP2 only, and 2 % for RF only. RA occurred in 17 people. The positive predictive value was 64 % when both antibodies were positive and 58 % when only anti-CCP2 was positive. Children of RA patients had 3 times higher independent risk of developing RA [188]. The presence of ACPAs could be decisive for the development of RA when a concatenation of risk factors associated with a genetic predisposition occurs. Among these risk factors, the best known is tobacco, which facilitates the citrullination of certain proteins in the lungs. Other risk factors capable of the citrullination are silica powder and the periodontitis caused by Porphyromonas gingivalis. In any case, these risk factors must find a propitious genetic terrain, such as the HLA-DR shared epitope alleles.
In addition, ACPAs have a relevant role in the development of subchondral bone lesions and CV events [82, 94]. The latter result from the accelerated atherosclerosis that occurs in RA; additionally, ACPAs have been demonstrated to be an independent risk factor for ischemic heart disease [6]. Furthermore, ACPAs are associated with an increase in the cIMT, which can predict the risk of CV events [103].
The main objective of this review was to evaluate ACPAs as a predictor of response in RA patients treated with biologics. With respect to anti-TNF, the results are disparate and inconclusive. Apart from isolated studies, in an extensive systematic literature review on the predictive value of the response in IgM-RF and ACPA+ patients [134], ACPA status did not predict the EULAR, DAS28, or ACR20 response. Given the heterogeneity among studies, a sensitivity analysis was performed, but the result did not change. Therefore, based on the current evidence, it cannot be confirmed that ACPAs predict anti-TNF response.
Concerning RTX, from the first trials, the results suggested a greater response in RF+ patients, although some studies, such as REFLEX [145, 147], gave controversial results; this was probably due to the limited number of RF− patients. However, a further analysis of this trial demonstrated that RF seropositivity and/or IgG anti-CCP with elevated CRP detected a subgroup of patients with greater response to RTX [145]. These results were corroborated in the SERENE and IMAGE trials [146, 148]. However, the limitation of the small number of seronegative patients led Isaacs et al. [8] to perform a meta-analysis of REFLEX, DANCER, SERENE, and IMAGE. The authors concluded that although small, the overall effect on seropositive patients was higher than the effect on the seronegative patients. This predictor effect has also been observed in other types of studies (open, registries, and observational) [153–157]. Therefore, at the present, seropositive patients continue to be a target population for treatment when considering RTX. On the other hand, studies addressing the reduction in the RF and ACPA titers and the response to RTX, have produced discrepant results [162, 168].
With respect to tocilizumab, neither of the two studies that evaluated the ability to predict the response in the ACPA+ patients yielded significant results [171, 172].
Regarding to abatacept, some studies like the AIM and ATTAIN [173, 174] did not address this issue and others recruited a vast majority of ACPA+ patients [175], or the presence of ACPA was required to be included in the study [176]. The first data to suggest that abatacept may be more effective in ACPA+ patients is a French observational study [110]. The analysis was carried out in 773 patients on abatacept for a minimum of 6 months and reported a higher rate of clinical response and drug retention in ACPA+ patients. A higher retention rate of abatacept has been also observed in other studies [11, 178]. In a subanalysis of the AMPLE study [12], those patients having a very high ACPA titer (upper quartile) had a significantly greater decrease in DAS28-CRP than patients with lower ACPA titers also treated with this drug. Three Japanese studies also reported divergent results [180–182]. In the ABROAD study [182], predictors of remission in patients treated with abatacept were a short disease evolution and a very high ACPA titer.
All ACPA isotypes are reduced after treating RA with abatacept [177]. However, recent data suggest that ACPA+ for IgM responded more favorably to abatacept [10]. Seroconversion (from positive to negative) is more common in the case of RF than ACPAs (from 23 to 31 % in RF vs. 7 % in ACPA) [183]. Although the clinical significance of the reduction in the Ab titer or the negativization was not established, it is logical that the reduction and/or absence of antibodies would be beneficial for the evolution of the disease. The possible effect of abatacept on the ACPA patients might result from the inhibition of costimulation, which would affect antibody production. The CD4+ T helper lymphocytes activate the B cells responsible for the production of ACPAs. A decrease in the memory B cells, which produce Abs, has also been demonstrated, and this could be affected by abatacept [182].
In summary: no predictive value has been demonstrated in ACPA+ RA patients treated with anti-TNF and tocilizumab. There are favorable data suggesting that with RTX, RF+ and/or ACPA+ patients would respond better than seronegatives, but no study has compared the efficacy of this drug in ACPA+ versus ACPA− patients. Finally, data have suggested a better response with abatacept in patients with high ACPA titers. However, there is no conclusive evidence of the superiority of this drug compared with other biologics. To extract a definitive conclusion, it would be necessary to conduct a comparative study to demonstrate the superiority of abatacept to other biologics in ACPA+ patients. The modification of ACPA concentrations and the possible negativization of some isotypes after the initiation of treatment with abatacept are of maximum interest, as it could have direct consequences on immunological mechanisms that perpetuate arthritis. However, the data provided to date are very preliminary, and it is difficult to determine their current clinical implications.
References
Carmona L, Villaverde V, Hernandez-Garcia C, Ballina J, Gabriel R, Laffon A (2002) The prevalence of rheumatoid arthritis in the general population of Spain. Rheumatology 41(1):88–95
Klareskog L, Catrina AI, Paget S (2009) Rheum Arthritis. Lancet 373(9664):659–672
Klareskog L, Amara K, Malmstrom V (2014) Adaptive immunity in rheumatoid arthritis: anticitrulline and other antibodies in the pathogenesis of rheumatoid arthritis. Curr Opin Rheumatol 26(1):72–79
van Gaalen F, Ioan-Facsinay A, Huizinga TW, Toes RE (2005) The devil in the details: the emerging role of anticitrulline autoimmunity in rheumatoid arthritis. J Immunol 175(9):5575–5580
van der Helm-van Mil AH, Verpoort KN, Breedveld FC, Toes RE, Huizinga TW (2005) Antibodies to citrullinated proteins and differences in clinical progression of rheumatoid arthritis. Arthritis Res Ther 7(5):R949–R958
Lopez-Longo FJ, Oliver-Minarro D, de la Torre I, Gonzalez-Diaz de Rabago E, Sanchez-Ramon S, Rodriguez-Mahou M et al (2009) Association between anti-cyclic citrullinated peptide antibodies and ischemic heart disease in patients with rheumatoid arthritis. Arthritis Rheum 61(4):419–424
Zhu J, Zhou Y, Chen X, Li J (2014) A metaanalysis of the increased risk of rheumatoid arthritis-related pulmonary disease as a result of serum anticitrullinated protein antibody positivity. J Rheumatol 41(7):1282–1289
Isaacs JD, Cohen SB, Emery P, Tak PP, Wang J, Lei G et al (2013) Effect of baseline rheumatoid factor and anticitrullinated peptide antibody serotype on rituximab clinical response: a meta-analysis. Ann Rheum Dis 72(3):329–336
de Lemos LL, Costa Jde O, Machado MA, Almeida AM, Barbosa MM, Kakehasi AM et al (2014) Rituximab for rheumatoid arthrits treatment: a systematic review. Rev Bras Reumatol 54(3):220–230
Huizinga TWJ, Connolly SE, Johnsen A, Zhu J, Furst DE, Bykerk VP et al (2015) Effect of anti-cyclic citrullinated peptide 2 immunoglobulin M serostatus on efficacy outcomes following treatment with abatacept plus methotrexate in the AVERT trial. Ann Rheum Dis 74(Suppl2):234–235
Gottenberg JE, Neto D, Gomez-Reino J, Iannone F, Lie E, Canhão H et al (2014) Positivity for rheumatoid factor and anti-cyclic citrullinated peptide is associated with a better drug retention of abatacept: data from a paneuropean analysis of RA registries. Ann Rheum Dis 73(suppl2):502–503
Sokolove J, Schiff M, Fleischmann R, Weinblatt ME, Connolly SE, Johnsen A, et al (2016) Impact of baseline anti-cyclic citrullinated peptide-2 antibody concentration on efficacy outcomes following treatment with subcutaneous abatacept or adalimumab: 2-year results from the AMPLE trial. Ann Rheum Dis 75(4):709–714
van Boekel MA, Vossenaar ER, van den Hoogen FH, van Venrooij WJ (2002) Autoantibody systems in rheumatoid arthritis: specificity, sensitivity and diagnostic value. Arthritis Res 4(2):87–93
Nienhuis RL, Mandema E (1964) A new serum factor in patients with rheumatoid arthritis: the antiperinuclear factor. Ann Rheum Dis 23:302–305
Young BJ, Mallya RK, Leslie RD, Clark CJ, Hamblin TJ (1979) Anti-keratin antibodies in rheumatoid arthritis. Br Med J 2(6182):97–99
Sebbag M, Simon M, Vincent C, Masson-Bessiere C, Girbal E, Durieux JJ et al (1995) The antiperinuclear factor and the so-called antikeratin antibodies are the same rheumatoid arthritis-specific autoantibodies. J Clin Invest 95(6):2672–2679
Munoz-Fernandez S, Alvarez-Doforno R, Cuesta M, Balsa A, Fontan G, Gijon-Banos J (1995) Antiperinuclear factor: a useful test for the diagnosis of rheumatoid arthritis. Rheumatol Int 15(4):145–149
Munoz-Fernandez S, Alvarez-Doforno R, Gonzalez-Tarrio JM, Balsa A, Richi P, Fontan G et al (1999) Antiperinuclear factor as a prognostic marker in rheumatoid arthritis. J Rheumatol 26(12):2572–2577
Vincent C, de Keyser F, Masson-Bessiere C, Sebbag M, Veys EM, Serre G (1999) Anti-perinuclear factor compared with the so called “antikeratin” antibodies and antibodies to human epidermis filaggrin, in the diagnosis of arthritides. Ann Rheum Dis 58(1):42–48
Schellekens GA, de Jong BA, van den Hoogen FH, van de Putte LB, van Venrooij WJ (1998) Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J Clin Invest 101(1):273–281
Girbal-Neuhauser E, Durieux JJ, Arnaud M, Dalbon P, Sebbag M, Vincent C et al (1999) The epitopes targeted by the rheumatoid arthritis-associated antifilaggrin autoantibodies are posttranslationally generated on various sites of (pro)filaggrin by deimination of arginine residues. J Immunol 162(1):585–594
Nogueira L, Sebbag M, Vincent C, Arnaud M, Fournie B, Cantagrel A et al (2001) Performance of two ELISAs for antifilaggrin autoantibodies, using either affinity purified or deiminated recombinant human filaggrin, in the diagnosis of rheumatoid arthritis. Ann Rheum Dis 60(9):882–887
Vincent C, Nogueira L, Sebbag M, Chapuy-Regaud S, Arnaud M, Letourneur O et al (2002) Detection of antibodies to deiminated recombinant rat filaggrin by enzyme-linked immunosorbent assay: a highly effective test for the diagnosis of rheumatoid arthritis. Arthritis Rheum 46(8):2051–2058
Schellekens GA, Visser H, de Jong BA, van den Hoogen FH, Hazes JM, Breedveld FC et al (2000) The diagnostic properties of rheumatoid arthritis antibodies recognizing a cyclic citrullinated peptide. Arthritis Rheum 43(1):155–163
Zendman AJ, van Venrooij WJ, Pruijn GJ (2006) Use and significance of anti-CCP autoantibodies in rheumatoid arthritis. Rheumatology 45(1):20–25
Damjanovska L, Thabet MM, Levarth EW, Stoeken-Rijsbergen G, van der Voort EI, Toes RE et al (2010) Diagnostic value of anti-MCV antibodies in differentiating early inflammatory arthritis. Ann Rheum Dis 69(4):730–732
Sanmarti R, Graell E, Perez ML, Ercilla G, Vinas O, Gomez-Puerta JA et al (2009) Diagnostic and prognostic value of antibodies against chimeric fibrin/filaggrin citrullinated synthetic peptides in rheumatoid arthritis. Arthritis Res Ther 11(5):R135
Ioan-Facsinay A, el-Bannoudi H, Scherer HU, van der Woude D, Menard HA, Lora M et al (2011) Anti-cyclic citrullinated peptide antibodies are a collection of anti-citrullinated protein antibodies and contain overlapping and non-overlapping reactivities. Ann Rheum Dis 70(1):188–193
Willemze A, Trouw LA, Toes RE, Huizinga TW (2012) The influence of ACPA status and characteristics on the course of RA. Nat Rev Rheumatol 8(3):144–152
Shi J, Willemze A, Janssen GM, van Veelen PA, Drijfhout JW, Cerami A et al (2013) Recognition of citrullinated and carbamylated proteins by human antibodies: specificity, cross-reactivity and the ‘AMC-Senshu’ method. Ann Rheum Dis 72(1):148–150
Vossenaar ER, Zendman AJ, van Venrooij WJ, Pruijn GJ (2003) PAD, a growing family of citrullinating enzymes: genes, features and involvement in disease. BioEssays 25(11):1106–1118
Asaga H, Yamada M, Senshu T (1998) Selective deimination of vimentin in calcium ionophore-induced apoptosis of mouse peritoneal macrophages. Biochem Biophys Res Commun 243(3):641–646
Masson-Bessiere C, Sebbag M, Girbal-Neuhauser E, Nogueira L, Vincent C, Senshu T et al (2001) The major synovial targets of the rheumatoid arthritis-specific antifilaggrin autoantibodies are deiminated forms of the alpha- and beta-chains of fibrin. J Immunol 166(6):4177–4184
Vossenaar ER, Despres N, Lapointe E, van der Heijden A, Lora M, Senshu T et al (2004) Rheumatoid arthritis specific anti-Sa antibodies target citrullinated vimentin. Arthritis Res Ther 6(2):R142–R150
Vossenaar ER, Nijenhuis S, Helsen MM, van der Heijden A, Senshu T, van den Berg WB et al (2003) Citrullination of synovial proteins in murine models of rheumatoid arthritis. Arthritis Rheum 48(9):2489–2500
Vossenaar ER, Smeets TJ, Kraan MC, Raats JM, van Venrooij WJ, Tak PP (2004) The presence of citrullinated proteins is not specific for rheumatoid synovial tissue. Arthritis Rheum 50(11):3485–3494
De Rycke L, Nicholas AP, Cantaert T, Kruithof E, Echols JD, Vandekerckhove B et al (2005) Synovial intracellular citrullinated proteins colocalizing with peptidyl arginine deiminase as pathophysiologically relevant antigenic determinants of rheumatoid arthritis-specific humoral autoimmunity. Arthritis Rheum 52(8):2323–2330
Wegner N, Wait R, Sroka A, Eick S, Nguyen KA, Lundberg K et al (2010) Peptidylarginine deiminase from Porphyromonas gingivalis citrullinates human fibrinogen and alpha-enolase: implications for autoimmunity in rheumatoid arthritis. Arthritis Rheum 62(9):2662–2672
Avouac J, Gossec L, Dougados M (2006) Diagnostic and predictive value of anti-cyclic citrullinated protein antibodies in rheumatoid arthritis: a systematic literature review. Ann Rheum Dis 65(7):845–851
Riedemann JP, Munoz S, Kavanaugh A (2005) The use of second generation anti-CCP antibody (anti-CCP2) testing in rheumatoid arthritis—a systematic review. Clin Exp Rheumatol 23(5 Suppl 39):S69–S76
Edwards JC, Leandro MJ, Cambridge G (2005) B lymphocyte depletion in rheumatoid arthritis: targeting of CD20. Curr Dir Autoimmun 8:175–192
Kuhn KA, Kulik L, Tomooka B, Braschler KJ, Arend WP, Robinson WH et al (2006) Antibodies against citrullinated proteins enhance tissue injury in experimental autoimmune arthritis. J Clin Invest 116(4):961–973
Nielen MM, van Schaardenburg D, Reesink HW, van de Stadt RJ, van der Horst-Bruinsma IE, de Koning MH et al (2004) Specific autoantibodies precede the symptoms of rheumatoid arthritis: a study of serial measurements in blood donors. Arthritis Rheum 50(2):380–386
Rantapaa-Dahlqvist S, de Jong BA, Berglin E, Hallmans G, Wadell G, Stenlund H et al (2003) Antibodies against cyclic citrullinated peptide and IgA rheumatoid factor predict the development of rheumatoid arthritis. Arthritis Rheum 48(10):2741–2749
Berglin E, Padyukov L, Sundin U, Hallmans G, Stenlund H, Van Venrooij WJ et al (2004) A combination of autoantibodies to cyclic citrullinated peptide (CCP) and HLA-DRB1 locus antigens is strongly associated with future onset of rheumatoid arthritis. Arthritis Res Ther 6(4):R303–R308
Ronnelid J, Wick MC, Lampa J, Lindblad S, Nordmark B, Klareskog L et al (2005) Longitudinal analysis of citrullinated protein/peptide antibodies (anti-CP) during 5 year follow up in early rheumatoid arthritis: anti-CP status predicts worse disease activity and greater radiological progression. Ann Rheum Dis 64(12):1744–1749
Sokolove J, Bromberg R, Deane KD, Lahey LJ, Derber LA, Chandra PE et al (2012) Autoantibody epitope spreading in the pre-clinical phase predicts progression to rheumatoid arthritis. PLoS One 7(5):e35296
Brink M, Hansson M, Mathsson L, Jakobsson PJ, Holmdahl R, Hallmans G et al (2013) Multiplex analyses of antibodies against citrullinated peptides in individuals prior to development of rheumatoid arthritis. Arthritis Rheum 65(4):899–910
van de Stadt LA, Witte BI, Bos WH, van Schaardenburg D (2013) A prediction rule for the development of arthritis in seropositive arthralgia patients. Ann Rheum Dis 72(12):1920–1926
de Hair MJ, Landewe RB, van de Sande MG, van Schaardenburg D, van Baarsen LG, Gerlag DM et al (2013) Smoking and overweight determine the likelihood of developing rheumatoid arthritis. Ann Rheum Dis 72(10):1654–1658
Gregersen PK, Silver J, Winchester RJ (1987) The shared epitope hypothesis. An approach to understanding the molecular genetics of susceptibility to rheumatoid arthritis. Arthritis Rheum 30(11):1205–1213
Balsa A, Cabezon A, Orozco G, Cobo T, Miranda-Carus E, Lopez-Nevot MA et al (2010) Influence of HLA DRB1 alleles in the susceptibility of rheumatoid arthritis and the regulation of antibodies against citrullinated proteins and rheumatoid factor. Arthritis Res Ther 12(2):R62
Zanelli E, Breedveld FC, de Vries RR (2000) HLA class II association with rheumatoid arthritis: facts and interpretations. Hum Immunol 61(12):1254–1261
Hill J, Cairns E, Bell DA (2004) The joy of citrulline: new insights into the diagnosis, pathogenesis, and treatment of rheumatoid arthritis. J Rheumatol 31(8):1471–1473
Huizinga TW, Amos CI, van der Helm-van Mil AH, Chen W, van Gaalen FA, Jawaheer D et al (2005) Refining the complex rheumatoid arthritis phenotype based on specificity of the HLA-DRB1 shared epitope for antibodies to citrullinated proteins. Arthritis Rheum 52(11):3433–3438
Irigoyen P, Lee AT, Wener MH, Li W, Kern M, Batliwalla F et al (2005) Regulation of anti-cyclic citrullinated peptide antibodies in rheumatoid arthritis: contrasting effects of HLA-DR3 and the shared epitope alleles. Arthritis Rheum 52(12):3813–3818
Aarden LA, Helle M, Boeije L, Pascual-Salcedo D, de Groot E (1991) Differential induction of interleukin-6 production in monocytes, endothelial cells and smooth muscle cells. In: Bienvenu J, Fradezeli D (eds) Cytokines and inflammation. John Libbey Eurotext, Paris, pp 15–27
Klareskog L, Stolt P, Lundberg K, Kallberg H, Bengtsson C, Grunewald J et al (2006) A new model for an etiology of rheumatoid arthritis: smoking may trigger HLA-DR (shared epitope)-restricted immune reactions to autoantigens modified by citrullination. Arthritis Rheum 54(1):38–46
Klareskog L, Padyukov L, Ronnelid J, Alfredsson L (2006) Genes, environment and immunity in the development of rheumatoid arthritis. Curr Opin Immunol 18(6):650–655
Scher JU, Bretz WA, Abramson SB (2014) Periodontal disease and subgingival microbiota as contributors for rheumatoid arthritis pathogenesis: modifiable risk factors? Curr Opin Rheumatol 26(4):424–429
Gomez-Reino Carnota JJ, Maceiras Pan F (2000) Genetics of rheumatoid arthritis. Med Clin 114(1):16–18
Plenge RM, Padyukov L, Remmers EF, Purcell S, Lee AT, Karlson EW et al (2005) Replication of putative candidate-gene associations with rheumatoid arthritis in >4000 samples from North America and Sweden: association of susceptibility with PTPN22, CTLA4, and PADI4. Am J Hum Genet 77(6):1044–1060
Orozco G, Sanchez E, Gonzalez-Gay MA, Lopez-Nevot MA, Torres B, Caliz R et al (2005) Association of a functional single-nucleotide polymorphism of PTPN22, encoding lymphoid protein phosphatase, with rheumatoid arthritis and systemic lupus erythematosus. Arthritis Rheum 52(1):219–224
Johansson M, Arlestig L, Hallmans G, Rantapaa-Dahlqvist S (2006) PTPN22 polymorphism and anti-cyclic citrullinated peptide antibodies in combination strongly predicts future onset of rheumatoid arthritis and has a specificity of 100% for the disease. Arthritis Res Ther 8(1):R19
Vossenaar ER, van Venrooij WJ (2004) Anti-CCP antibodies, a highly specific marker for (early) rheumatoid arthritis. Clin Appl Immunol Rev 4:239–262
Whiting PF, Smidt N, Sterne JA, Harbord R, Burton A, Burke M et al (2010) Systematic review: accuracy of anti-citrullinated Peptide antibodies for diagnosing rheumatoid arthritis. Ann Intern Med. 152(7):456–464 W155-66
van Oosterhout M, Bajema I, Levarht EW, Toes RE, Huizinga TW, van Laar JM (2008) Differences in synovial tissue infiltrates between anti-cyclic citrullinated peptide-positive rheumatoid arthritis and anti-cyclic citrullinated peptide-negative rheumatoid arthritis. Arthritis Rheum 58(1):53–60
De Rycke L, Peene I, Hoffman IE, Kruithof E, Union A, Meheus L et al (2004) Rheumatoid factor and anticitrullinated protein antibodies in rheumatoid arthritis: diagnostic value, associations with radiological progression rate, and extra-articular manifestations. Ann Rheum Dis 63(12):1587–1593
Jansen LM, van Schaardenburg D, van der Horst-Bruinsma I, van der Stadt RJ, de Koning MH, Dijkmans BA (2003) The predictive value of anti-cyclic citrullinated peptide antibodies in early arthritis. J Rheumatol 30(8):1691–1695
Syversen SW, Gaarder PI, Goll GL, Odegard S, Haavardsholm EA, Mowinckel P et al (2008) High anti-cyclic citrullinated peptide levels and an algorithm of four variables predict radiographic progression in patients with rheumatoid arthritis: results from a 10-year longitudinal study. Ann Rheum Dis 67(2):212–217
Machold KP, Stamm TA, Nell VP, Pflugbeil S, Aletaha D, Steiner G et al (2007) Very recent onset rheumatoid arthritis: clinical and serological patient characteristics associated with radiographic progression over the first years of disease. Rheumatology 46(2):342–349
Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Allaart CF, van Zeben D, Kerstens PJ, Hazes JM et al (2005) Clinical and radiographic outcomes of four different treatment strategies in patients with early rheumatoid arthritis (the BeSt study): a randomized, controlled trial. Arthritis Rheum 52(11):3381–3390
de Vries-Bouwstra JK, Goekoop-Ruiterman YP, Verpoort KN, Schreuder GM, Ewals JA, Terwiel JP et al (2008) Progression of joint damage in early rheumatoid arthritis: association with HLA-DRB1, rheumatoid factor, and anti-citrullinated protein antibodies in relation to different treatment strategies. Arthritis Rheum 58(5):1293–1298
Berglin E, Johansson T, Sundin U, Jidell E, Wadell G, Hallmans G et al (2006) Radiological outcome in rheumatoid arthritis is predicted by presence of antibodies against cyclic citrullinated peptide before and at disease onset, and by IgA-RF at disease onset. Ann Rheum Dis 65(4):453–458
Forslind K, Ahlmen M, Eberhardt K, Hafstrom I, Svensson B (2004) Prediction of radiological outcome in early rheumatoid arthritis in clinical practice: role of antibodies to citrullinated peptides (anti-CCP). Ann Rheum Dis 63(9):1090–1095
Hecht C, Englbrecht M, Rech J, Schmidt S, Araujo E, Engelke K et al (2015) Additive effect of anti-citrullinated protein antibodies and rheumatoid factor on bone erosions in patients with RA. Ann Rheum Dis 74(12):2151–2156
Kroot EJ, de Jong BA, van Leeuwen MA, Swinkels H, van den Hoogen FH, van’t Hof M et al (2000) The prognostic value of anti-cyclic citrullinated peptide antibody in patients with recent-onset rheumatoid arthritis. Arthritis Rheum 43(8):1831–1835
van Gaalen FA, Linn-Rasker SP, van Venrooij WJ, de Jong BA, Breedveld FC, Verweij CL et al (2004) Autoantibodies to cyclic citrullinated peptides predict progression to rheumatoid arthritis in patients with undifferentiated arthritis: a prospective cohort study. Arthritis Rheum 50(3):709–715
Meyer O, Labarre C, Dougados M, Goupille P, Cantagrel A, Dubois A et al (2003) Anticitrullinated protein/peptide antibody assays in early rheumatoid arthritis for predicting five year radiographic damage. Ann Rheum Dis 62(2):120–126
Cui J, Saevarsdottir S, Thomson B, Padyukov L, van der Helm-van Mil AH, Nititham J et al (2010) Rheumatoid arthritis risk allele PTPRC is also associated with response to anti-tumor necrosis factor alpha therapy. Arthritis Rheum 62(7):1849–1861
Guler H, Turhanoglu AD, Ozer B, Ozer C, Balci A (2008) The relationship between anti-cyclic citrullinated peptide and bone mineral density and radiographic damage in patients with rheumatoid arthritis. Scand J Rheumatol 37(5):337–342
Boyesen P, Hoff M, Odegard S, Haugeberg G, Syversen SW, Gaarder PI et al (2009) Antibodies to cyclic citrullinated protein and erythrocyte sedimentation rate predict hand bone loss in patients with rheumatoid arthritis of short duration: a longitudinal study. Arthritis Res Ther 11(4):R103
Kleyer A, Finzel S, Rech J, Manger B, Krieter M, Faustini F et al (2014) Bone loss before the clinical onset of rheumatoid arthritis in subjects with anticitrullinated protein antibodies. Ann Rheum Dis 73(5):854–860
Harre U, Georgess D, Bang H, Bozec A, Axmann R, Ossipova E et al (2012) Induction of osteoclastogenesis and bone loss by human autoantibodies against citrullinated vimentin. J Clin Invest 122(5):1791–1802
Kleyer A, Schett G (2014) Arthritis and bone loss: a hen and egg story. Curr Opin Rheumatol 26(1):80–84
Goodson N, Marks J, Lunt M, Symmons D (2005) Cardiovascular admissions and mortality in an inception cohort of patients with rheumatoid arthritis with onset in the 1980s and 1990s. Ann Rheum Dis 64(11):1595–1601
Solomon DH, Karlson EW, Rimm EB, Cannuscio CC, Mandl LA, Manson JE et al (2003) Cardiovascular morbidity and mortality in women diagnosed with rheumatoid arthritis. Circulation 107(9):1303–1307
Avina-Zubieta JA, Choi HK, Sadatsafavi M, Etminan M, Esdaile JM, Lacaille D (2008) Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis Rheum 59(12):1690–1697
Zinger H, Sherer Y, Shoenfeld Y (2009) Atherosclerosis in autoimmune rheumatic diseases-mechanisms and clinical findings. Clin Rev Allergy Immunol 37(1):20–28
Gonzalez-Gay MA, Gonzalez-Juanatey C, Martin J (2005) Rheumatoid arthritis: a disease associated with accelerated atherogenesis. Semin Arthritis Rheum 35(1):8–17
Shoenfeld Y, Gerli R, Doria A, Matsuura E, Cerinic MM, Ronda N et al (2005) Accelerated atherosclerosis in autoimmune rheumatic diseases. Circulation 112(21):3337–3347
del Rincon I, Escalante A (2003) Atherosclerotic cardiovascular disease in rheumatoid arthritis. Curr Rheumatol Rep 5(4):278–286
Bartoloni E, Shoenfeld Y, Gerli R (2011) Inflammatory and autoimmune mechanisms in the induction of atherosclerotic damage in systemic rheumatic diseases: two faces of the same coin. Arthritis Care Res 63(2):178–183
Gonzalez-Juanatey C, Llorca J, Testa A, Revuelta J, Garcia-Porrua C, Gonzalez-Gay MA (2003) Increased prevalence of severe subclinical atherosclerotic findings in long-term treated rheumatoid arthritis patients without clinically evident atherosclerotic disease. Medicine 82(6):407–413
Lopez-Mejias R, Corrales A, Genre F, Hernandez JL, Ochoa R, Blanco R et al (2013) Angiopoietin-2 serum levels correlate with severity, early onset and cardiovascular disease in patients with rheumatoid arthritis. Clin Exp Rheumatol 31(5):761–766
Lopez-Mejias R, Ubilla B, Genre F, Corrales A, Hernandez JL, Ferraz-Amaro I et al (2015) Osteoprotegerin concentrations relate independently to established cardiovascular disease in rheumatoid arthritis. J Rheumatol 42(1):39–45
Dessein PH, Lopez-Mejias R, Gonzalez-Juanatey C, Genre F, Miranda-Filloy JA, Llorca J et al (2014) Independent relationship of osteoprotegerin concentrations with endothelial activation and carotid atherosclerosis in patients with severe rheumatoid arthritis. J Rheumatol 41(3):429–436
Peters MJ, Symmons DP, McCarey D, Dijkmans BA, Nicola P, Kvien TK et al (2010) EULAR evidence-based recommendations for cardiovascular risk management in patients with rheumatoid arthritis and other forms of inflammatory arthritis. Ann Rheum Dis 69(2):325–331
Szekanecz Z, Kerekes G, Der H, Sandor Z, Szabo Z, Vegvari A et al (2007) Accelerated atherosclerosis in rheumatoid arthritis. Ann NY Acad Sci 1108:349–358
Gerli R, Sherer Y, Bocci EB, Vaudo G, Moscatelli S, Shoenfeld Y (2007) Precocious atherosclerosis in rheumatoid arthritis: role of traditional and disease-related cardiovascular risk factors. Ann NY Acad Sci 1108:372–381
Hjeltnes G, Hollan I, Forre O, Wiik A, Mikkelsen K, Agewall S (2011) Anti-CCP and RF IgM: predictors of impaired endothelial function in rheumatoid arthritis patients. Scand J Rheumatol 40(6):422–427
Sokolove J, Brennan MJ, Sharpe O, Lahey LJ, Kao AH, Krishnan E et al (2013) Brief report: citrullination within the atherosclerotic plaque: a potential target for the anti-citrullinated protein antibody response in rheumatoid arthritis. Arthritis Rheum 65(7):1719–1724
Gonzalez-Juanatey C, Llorca J, Martin J, Gonzalez-Gay MA (2009) Carotid intima-media thickness predicts the development of cardiovascular events in patients with rheumatoid arthritis. Semin Arthritis Rheum 38(5):366–371
Gerli R, Bartoloni Bocci E, Sherer Y, Vaudo G, Moscatelli S, Shoenfeld Y (2008) Association of anti-cyclic citrullinated peptide antibodies with subclinical atherosclerosis in patients with rheumatoid arthritis. Ann Rheum Dis 67(5):724–725
Gkaliagkousi E, Gavriilaki E, Doumas M, Petidis K, Aslanidis S, Stella D (2012) Cardiovascular risk in rheumatoid arthritis: pathogenesis, diagnosis, and management. J Clin Rheumatol 18(8):422–430
Papadopoulos NG, Tsiaousis GZ, Pavlitou-Tsiontsi A, Giannakou A, Galanopoulou VK (2008) Does the presence of anti-CCP autoantibodies and their serum levels influence the severity and activity in rheumatoid arthritis patients? Clin Rev Allergy Immunol 34(1):11–15
Vazquez-Del Mercado M, Nunez-Atahualpa L, Figueroa-Sanchez M, Gomez-Banuelos E, Rocha-Munoz AD, Martin-Marquez BT et al (2015) Serum levels of anticyclic citrullinated peptide antibodies, interleukin-6, tumor necrosis factor-alpha, and C-reactive protein are associated with increased carotid intima-media thickness: a cross-sectional analysis of a cohort of rheumatoid arthritis patients without cardiovascular risk factors. Biomed Res Int 2015:342649
Barbarroja N, Perez-Sanchez C, Ruiz-Limon P, Castro-Villegas C, Aguirre MA, Carretero R et al (2014) Anticyclic citrullinated protein antibodies are implicated in the development of cardiovascular disease in rheumatoid arthritis. Arterioscler Thromb Vasc Biol 34(12):2706–2716
Sokolove J, Johnson DS, Lahey LJ, Wagner CA, Cheng D, Thiele GM et al (2014) Rheumatoid factor as a potentiator of anti-citrullinated protein antibody-mediated inflammation in rheumatoid arthritis. Arthritis Rheumatol 66(4):813–821
Gottenberg JE, Ravaud P, Cantagrel A, Combe B, Flipo RM, Schaeverbeke T et al (2012) Positivity for anti-cyclic citrullinated peptide is associated with a better response to abatacept: data from the ‘Orencia and Rheumatoid Arthritis’ registry. Ann Rheum Dis 71(11):1815–1819
Bobbio-Pallavicini F, Caporali R, Alpini C, Moratti R, Montecucco C (2007) Predictive value of antibodies to citrullinated peptides and rheumatoid factors in anti-TNF-alpha treated patients. Ann NY Acad Sci 1109:287–295
Braun-Moscovici Y, Markovits D, Zinder O, Schapira D, Rozin A, Ehrenburg M et al (2006) Anti-cyclic citrullinated protein antibodies as a predictor of response to anti-tumor necrosis factor-alpha therapy in patients with rheumatoid arthritis. J Rheumatol 33(3):497–500
Bizzaro N, Bartoloni E, Morozzi G, Manganelli S, Riccieri V, Sabatini P et al (2013) Anti-cyclic citrullinated peptide antibody titer predicts time to rheumatoid arthritis onset in patients with undifferentiated arthritis: results from a 2-year prospective study. Arthritis Res Ther 15(1):R16
Elrefaei M, Boose K, McGee M, Tarrant TK, Lin FC, Fine JP et al (2012) Second generation automated anti-CCP test better predicts the clinical diagnosis of rheumatoid arthritis. J Clin Immunol 32(1):131–137
Kokkonen H, Mullazehi M, Berglin E, Hallmans G, Wadell G, Ronnelid J et al (2011) Antibodies of IgG, IgA and IgM isotypes against cyclic citrullinated peptide precede the development of rheumatoid arthritis. Arthritis Res Ther 13(1):R13
Mjaavatten MD, van der Heijde D, Uhlig T, Haugen AJ, Nygaard H, Sidenvall G et al (2010) The likelihood of persistent arthritis increases with the level of anti-citrullinated peptide antibody and immunoglobulin M rheumatoid factor: a longitudinal study of 376 patients with very early undifferentiated arthritis. Arthritis Res Ther 12(3):R76
Emad Y, Shehata M, Ragab Y, Saad A, Hamza H, Abou-Zeid A (2010) Prevalence and predictive value of anti-cyclic citrullinated protein antibodies for future development of rheumatoid arthritis in early undifferentiated arthritis. Mod Rheumatol 20(4):358–365
van der Linden MP, van der Woude D, Ioan-Facsinay A, Levarht EW, Stoeken-Rijsbergen G, Huizinga TW et al (2009) Value of anti-modified citrullinated vimentin and third-generation anti-cyclic citrullinated peptide compared with second-generation anti-cyclic citrullinated peptide and rheumatoid factor in predicting disease outcome in undifferentiated arthritis and rheumatoid arthritis. Arthritis Rheum 60(8):2232–2241
Hafstrom I, Engvall IL, Ronnelid J, Boonen A, van der Heijde D, Svensson B (2014) Rheumatoid factor and anti-CCP do not predict progressive joint damage in patients with early rheumatoid arthritis treated with prednisolone: a randomised study. BMJ Open 4(7):e005246
Esalatmanesh K, Jamali R, Jamali A, Jamali B, Nikbakht M (2012) Serum anti-cyclic citrullinated peptide antibodies may predict disease activity in rheumatoid arthritis. Rheumatol Int 32(12):3799–3805
da Mota LM, Dos Santos Neto LL, de Carvalho JF, Pereira IA, Burlingame R, Menard HA et al (2012) The presence of anti-citrullinated protein antibodies (ACPA) and rheumatoid factor on patients with rheumatoid arthritis (RA) does not interfere with the chance of clinical remission in a follow-up of 3 years. Rheumatol Int 32(12):3807–3812
Marasovic-Krstulovic D, Martinovic-Kaliterna D, Fabijanic D, Morovic-Vergles J (2011) Are the anti-cyclic citrullinated peptide antibodies independent predictors of myocardial involvement in patients with active rheumatoid arthritis? Rheumatology 50(8):1505–1512
Shidara K, Inoue E, Hoshi D, Sato E, Nakajima A, Momohara S et al (2012) Anti-cyclic citrullinated peptide antibody predicts functional disability in patients with rheumatoid arthritis in a large prospective observational cohort in Japan. Rheumatol Int 32(2):361–366
Cader MZ, Filer AD, Buckley CD, Raza K (2010) The relationship between the presence of anti-cyclic citrullinated peptide antibodies and clinical phenotype in very early rheumatoid arthritis. BMC Musculoskelet Disord 11:187
Farragher TM, Lunt M, Plant D, Bunn DK, Barton A, Symmons DP (2010) Benefit of early treatment in inflammatory polyarthritis patients with anti-cyclic citrullinated peptide antibodies versus those without antibodies. Arthritis Care Res 62(5):664–675
Cuchacovich M, Catalan D, Wainstein E, Gatica H, Soto L, Aravena O et al (2008) Basal anti-cyclic citrullinated peptide (anti-CCP) antibody levels and a decrease in anti-CCP titres are associated with clinical response to adalimumab in rheumatoid arthritis. Clin Exp Rheumatol 26(6):1067–1073
Mathsson L, Mullazehi M, Wick MC, Sjoberg O, van Vollenhoven R, Klareskog L et al (2008) Antibodies against citrullinated vimentin in rheumatoid arthritis: higher sensitivity and extended prognostic value concerning future radiographic progression as compared with antibodies against cyclic citrullinated peptides. Arthritis Rheum 58(1):36–45
Bukhari M, Thomson W, Naseem H, Bunn D, Silman A, Symmons D et al (2007) The performance of anti-cyclic citrullinated peptide antibodies in predicting the severity of radiologic damage in inflammatory polyarthritis: results from the Norfolk Arthritis Register. Arthritis Rheum 56(9):2929–2935
Vencovsky J, Machacek S, Sedova L, Kafkova J, Gatterova J, Pesakova V et al (2003) Autoantibodies can be prognostic markers of an erosive disease in early rheumatoid arthritis. Ann Rheum Dis 62(5):427–430
Salgado E, Maneiro JR, Gomez-Reino JJ (2015) Predictors of response to TNF antagonists. Curr Pharm Des 21(2):221–232
van der Heijde DM, van Riel PL, van Leeuwen MA, van’t Hof MA, van Rijswijk MH, van de Putte LB (1992) Prognostic factors for radiographic damage and physical disability in early rheumatoid arthritis. A prospective follow-up study of 147 patients. Br J Rheumatol 31(8):519–525
Maneiro RJ, Salgado E, Carmona L, Gomez-Reino JJ (2013) Rheumatoid factor as predictor of response to abatacept, rituximab and tocilizumab in rheumatoid arthritis: systematic review and meta-analysis. Semin Arthritis Rheum 43(1):9–17
Salgado E, Maneiro JR, Carmona L, Gomez-Reino J (2014) Rheumatoid factor and response to TNF antagonists in rheumatoid arthritis: systematic review and meta-analysis of observational studies. Joint Bone Spine 81(1):41–50
Lv Q, Yin Y, Li X, Shan G, Wu X, Liang D et al (2014) The status of rheumatoid factor and anti-cyclic citrullinated peptide antibody are not associated with the effect of anti-TNFalpha agent treatment in patients with rheumatoid arthritis: a meta-analysis. PLoS One 9(2):e89442
Chen HA, Lin KC, Chen CH, Liao HT, Wang HP, Chang HN et al (2006) The effect of etanercept on anti-cyclic citrullinated peptide antibodies and rheumatoid factor in patients with rheumatoid arthritis. Ann Rheum Dis 65(1):35–39
Bos WH, Bartelds GM, Wolbink GJ, de Koning MH, van de Stadt RJ, van Schaardenburg D et al (2008) Differential response of the rheumatoid factor and anticitrullinated protein antibodies during adalimumab treatment in patients with rheumatoid arthritis. J Rheumatol 35(10):1972–1977
Atzeni F, Sarzi-Puttini P, Dell’ Acqua D, de Portu S, Cecchini G, Cruini C et al (2006) Adalimumab clinical efficacy is associated with rheumatoid factor and anti-cyclic citrullinated peptide antibody titer reduction: a one-year prospective study. Arthritis Res Ther 8(1):R3
Alessandri C, Bombardieri M, Papa N, Cinquini M, Magrini L, Tincani A et al (2004) Decrease of anti-cyclic citrullinated peptide antibodies and rheumatoid factor following anti-TNFalpha therapy (infliximab) in rheumatoid arthritis is associated with clinical improvement. Ann Rheum Dis 63(10):1218–1221
De Rycke L, Verhelst X, Kruithof E, Van den Bosch F, Hoffman IE, Veys EM et al (2005) Rheumatoid factor, but not anti-cyclic citrullinated peptide antibodies, is modulated by infliximab treatment in rheumatoid arthritis. Ann Rheum Dis 64(2):299–302
Kelly CA, Saravanan V, Nisar M, Arthanari S, Woodhead FA, Price-Forbes AN et al (2014) Rheumatoid arthritis-related interstitial lung disease: associations, prognostic factors and physiological and radiological characteristics—a large multicentre UK study. Rheumatology 53(9):1676–1682
Amara K, Steen J, Murray F, Morbach H, Fernandez-Rodriguez BM, Joshua V et al (2013) Monoclonal IgG antibodies generated from joint-derived B cells of RA patients have a strong bias toward citrullinated autoantigen recognition. J Exp Med 210(3):445–455
Leandro MJ, Cambridge G, Ehrenstein MR, Edwards JC (2006) Reconstitution of peripheral blood B cells after depletion with rituximab in patients with rheumatoid arthritis. Arthritis Rheum 54(2):613–620
Edwards JC, Szczepanski L, Szechinski J, Filipowicz-Sosnowska A, Emery P, Close DR et al (2004) Efficacy of B-cell-targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med 350(25):2572–2581
Emery P, Fleischmann R, Filipowicz-Sosnowska A, Schechtman J, Szczepanski L, Kavanaugh A et al (2006) The efficacy and safety of rituximab in patients with active rheumatoid arthritis despite methotrexate treatment: results of a phase IIB randomized, double-blind, placebo-controlled, dose-ranging trial. Arthritis Rheum 54(5):1390–1400
Cohen SB, Emery P, Greenwald MW, Dougados M, Furie RA, Genovese MC et al (2006) Rituximab for rheumatoid arthritis refractory to anti-tumor necrosis factor therapy: Results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial evaluating primary efficacy and safety at twenty-four weeks. Arthritis Rheum 54(9):2793–2806
Tak PP, Rigby WF, Rubbert-Roth A, Peterfy CG, van Vollenhoven RF, Stohl W et al (2011) Inhibition of joint damage and improved clinical outcomes with rituximab plus methotrexate in early active rheumatoid arthritis: the IMAGE trial. Ann Rheum Dis 70(1):39–46
Lal P, Su Z, Holweg CT, Silverman GJ, Schwartzman S, Kelman A et al (2011) Inflammation and autoantibody markers identify rheumatoid arthritis patients with enhanced clinical benefit following rituximab treatment. Arthritis Rheum 63(12):3681–3691
Emery P, Deodhar A, Rigby WF, Isaacs JD, Combe B, Racewicz AJ et al (2010) Efficacy and safety of different doses and retreatment of rituximab: a randomised, placebo-controlled trial in patients who are biological naive with active rheumatoid arthritis and an inadequate response to methotrexate (Study Evaluating Rituximab’s Efficacy in MTX iNadequate rEsponders (SERENE)). Ann Rheum Dis 69(9):1629–1635
Tak PP, Rigby W, Rubbert-Roth A, Peterfy C, van Vollenhoven RF, Stohl W et al (2012) Sustained inhibition of progressive joint damage with rituximab plus methotrexate in early active rheumatoid arthritis: 2-year results from the randomised controlled trial IMAGE. Ann Rheum Dis 71(3):351–357
Mease PJ, Cohen S, Gaylis NB, Chubick A, Kaell AT, Greenwald M et al (2010) Efficacy and safety of retreatment in patients with rheumatoid arthritis with previous inadequate response to tumor necrosis factor inhibitors: results from the SUNRISE trial. J Rheumatol 37(5):917–927
Shetty S, Fisher MC, Ahmed AR (2013) Review on the influence of protocol design on clinical outcomes in rheumatoid arthritis treated with rituximab. Ann Pharmacother 47(3):311–323
Sellam J, Hendel-Chavez H, Rouanet S, Abbed K, Combe B, Le Loet X et al (2011) B cell activation biomarkers as predictive factors for the response to rituximab in rheumatoid arthritis: a six-month, national, multicenter, open-label study. Arthritis Rheum 63(4):933–938
Chatzidionysiou K, Lie E, Nasonov E, Lukina G, Hetland ML, Tarp U et al (2011) Highest clinical effectiveness of rituximab in autoantibody-positive patients with rheumatoid arthritis and in those for whom no more than one previous TNF antagonist has failed: pooled data from 10 European registries. Ann Rheum Dis 70(9):1575–1580
Narvaez J, Diaz-Torne C, Ruiz JM, Hernandez MV, Torrente-Segarra V, Ros S et al (2011) Predictors of response to rituximab in patients with active rheumatoid arthritis and inadequate response to anti-TNF agents or traditional DMARDs. Clin Exp Rheumatol 29(6):991–997
Couderc M, Mathieu S, Pereira B, Glace B, Soubrier M (2013) Predictive factors of rituximab response in rheumatoid arthritis: results from a French university hospital. Arthritis Care Res 65(4):648–652
Gardette A, Ottaviani S, Tubach F, Roy C, Nicaise-Roland P, Palazzo E et al (2014) High anti-CCP antibody titres predict good response to rituximab in patients with active rheumatoid arthritis. Joint Bone Spine 81(5):416–420
Quartuccio L, Salvin S, Saracco M, Lombardi S, Fabris M, Mansutti E et al (2009) Rheumatoid factor positivity rather than anti-CCP positivity, a lower disability and a lower number of anti-TNFalpha agents failed are associated with response to rituximab in rheumatoid arthritis. Reumatismo 61(3):182–186
Buch MH, Smolen JS, Betteridge N, Breedveld FC, Burmester G, Dorner T et al (2011) Updated consensus statement on the use of rituximab in patients with rheumatoid arthritis. Ann Rheum Dis 70(6):909–920
Vital EM, Rawstron AC, Dass S, Henshaw K, Madden J, Emery P et al (2011) Reduced-dose rituximab in rheumatoid arthritis: efficacy depends on degree of B cell depletion. Arthritis Rheum 63(3):603–608
Nakou M, Katsikas G, Sidiropoulos P, Bertsias G, Papadimitraki E, Raptopoulou A et al (2009) Rituximab therapy reduces activated B cells in both the peripheral blood and bone marrow of patients with rheumatoid arthritis: depletion of memory B cells correlates with clinical response. Arthritis Res Ther 11(4):R131
Thurlings RM, Vos K, Wijbrandts CA, Zwinderman AH, Gerlag DM, Tak PP (2008) Synovial tissue response to rituximab: mechanism of action and identification of biomarkers of response. Ann Rheum Dis 67(7):917–925
Cambridge G, Leandro MJ, Edwards JC, Ehrenstein MR, Salden M, Bodman-Smith M et al (2003) Serologic changes following B lymphocyte depletion therapy for rheumatoid arthritis. Arthritis Rheum 48(8):2146–2154
Cambridge G, Stohl W, Leandro MJ, Migone TS, Hilbert DM, Edwards JC (2006) Circulating levels of B lymphocyte stimulator in patients with rheumatoid arthritis following rituximab treatment: relationships with B cell depletion, circulating antibodies, and clinical relapse. Arthritis Rheum 54(3):723–732
Toubi E, Kessel A, Slobodin G, Boulman N, Pavlotzky E, Zisman D et al (2007) Changes in macrophage function after rituximab treatment in patients with rheumatoid arthritis. Ann Rheum Dis 66(6):818–820
Tsiakalos AP, Avgoustidis NK, Moutsopoulos HM (2008) Rituximab therapy in Greek patients with rheumatoid arthritis. Biologics 2(4):911–916
Rosengren S, Wei N, Kalunian KC, Zvaifler NJ, Kavanaugh A, Boyle DL (2008) Elevated autoantibody content in rheumatoid arthritis synovia with lymphoid aggregates and the effect of rituximab. Arthritis Res Ther 10(5):R105
Kormelink TG, Tekstra J, Thurlings RM, Boumans MH, Vos K, Tak PP et al (2010) Decrease in immunoglobulin free light chains in patients with rheumatoid arthritis upon rituximab (anti-CD20) treatment correlates with decrease in disease activity. Ann Rheum Dis 69(12):2137–2144
Vancsa A, Szabo Z, Szamosi S, Bodnar N, Vegh E, Gergely L et al (2013) Longterm effects of rituximab on B cell counts and autoantibody production in rheumatoid arthritis: use of high-sensitivity flow cytometry for more sensitive assessment of B cell depletion. J Rheumatol 40(5):565–571
Lindenberg L, Spengler L, Bang H, Dorner T, Maslyanskiy AL, Lapin SV et al (2015) Restrictive IgG antibody response against mutated citrullinated vimentin predicts response to rituximab in patients with rheumatoid arthritis. Arthritis Res Ther 17:206
Tanaka T, Kishimoto T (2012) Immunotherapeutic implication of IL-6 blockade. Immunotherapy 4(1):87–105
Kawashiri SY, Kawakami A, Iwamoto N, Fujikawa K, Aramaki T, Tamai M et al (2011) Disease activity score 28 may overestimate the remission induction of rheumatoid arthritis patients treated with tocilizumab: comparison with the remission by the clinical disease activity index. Mod Rheumatol 21(4):365–369
Pers YM, Fortunet C, Constant E, Lambert J, Godfrin-Valnet M, De Jong A et al (2014) Predictors of response and remission in a large cohort of rheumatoid arthritis patients treated with tocilizumab in clinical practice. Rheumatology 53(1):76–84
Kremer JM, Genant HK, Moreland LW, Russell AS, Emery P, Abud-Mendoza C et al (2006) Effects of abatacept in patients with methotrexate-resistant active rheumatoid arthritis: a randomized trial. Ann Intern Med 144(12):865–876
Genovese MC, Becker JC, Schiff M, Luggen M, Sherrer Y, Kremer J et al (2005) Abatacept for rheumatoid arthritis refractory to tumor necrosis factor alpha inhibition. N Engl J Med 353(11):1114–1123
Bathon J, Robles M, Ximenes AC, Nayiager S, Wollenhaupt J, Durez P et al (2011) Sustained disease remission and inhibition of radiographic progression in methotrexate-naive patients with rheumatoid arthritis and poor prognostic factors treated with abatacept: 2-year outcomes. Ann Rheum Dis 70(11):1949–1956
Emery P, Durez P, Dougados M, Legerton CW, Becker JC, Vratsanos G et al (2010) Impact of T-cell costimulation modulation in patients with undifferentiated inflammatory arthritis or very early rheumatoid arthritis: a clinical and imaging study of abatacept (the ADJUST trial). Ann Rheum Dis 69(3):510–516
Emery P, Burmester GR, Bykerk VP, Combe BG, Furst DE, Barre E et al (2015) Evaluating drug-free remission with abatacept in early rheumatoid arthritis: results from the phase 3b, multicentre, randomised, active-controlled AVERT study of 24 months, with a 12-month, double-blind treatment period. Ann Rheum Dis 74(1):19–26
Nusslein HG, Alten R, Galeazzi M, Lorenz HM, Boumpas D, Nurmohamed MT et al (2014) Real-world effectiveness of abatacept for rheumatoid arthritis treatment in European and Canadian populations: a 6-month interim analysis of the 2-year, observational, prospective ACTION study. BMC Musculoskelet Disord 15:14
Weinblatt ME, Schiff M, Valente R, van der Heijde D, Citera G, Zhao C et al (2013) Head-to-head comparison of subcutaneous abatacept versus adalimumab for rheumatoid arthritis: findings of a phase IIIb, multinational, prospective, randomized study. Arthritis Rheum 65(1):28–38
Kubo S, Nakayamada S, Nakano K, Hirata S, Fukuyo S, Miyagawa I et al (2015) Comparison of the efficacies of abatacept and tocilizumab in patients with rheumatoid arthritis by propensity score matching. Ann Rheum Dis [Epub ahead of print]
Anno S, Inui K, Mamoto K, Okano T, Sugioka Y, Tada M et al (2015) Abatacept might not alter anti-cyclic citrullinated peptide levels in established rheumatoid arthritis patients. Ann Rheum Dis 74(Suppl2):1058
Fujii T, Sekiguchi M, Matsui K, Kitano M, Hashimoto M, Ohmura K et al (2013) Very high titer of anti-citrullinated protein antibodies is associated with the achievement of clinical remission by abatacept in biologic-naïve patients with rheumatoid arthritis (the Abroad study). Ann Rheum Dis 72(Suppl3):889
Scarsi M, Paolini L, Ricotta D, Pedrini A, Piantoni S, Caimi L et al (2014) Abatacept reduces levels of switched memory B cells, autoantibodies, and immunoglobulins in patients with rheumatoid arthritis. J Rheumatol 41(4):666–672
Huizinga TWJ, Connolly SE, Furst DE, Bykerk VP, Burmester G, Combe B et al (2014) The impact on anti-citrullinated protein antibody isotypes and epitope fine specificity in patients with early RA treated with abatacept and methotrexate. Arthritis Rheum 66(Supl 10):S666
Klein U, Rajewsky K, Kuppers R (1998) Human immunoglobulin (Ig)M+ IgD+ peripheral blood B cells expressing the CD27 cell surface antigen carry somatically mutated variable region genes: CD27 as a general marker for somatically mutated (memory) B cells. J Exp Med 188(9):1679–1689
Martin Mola E, Balsa A, Martinez Taboada V, Sanmarti R, Marenco JL, Navarro Sarabia F et al (2013) Abatacept use in rheumatoid arthritis: evidence review and recommendations. Reumatol Clin 9(1):5–17
Matsutani T, Murakami M, Sekiguchi M, Matsui K, Kitano M, Namiki M et al (2013) Abatacept treatment suppresses T cell activation in anti-cyclic citrullinated peptide antibody (ACPA) positive RA patients but not in ACPA negative RA patients. Ann Rheum Dis 72(Suppl3):614
Ramos-Remus C, Castillo-Ortiz JD, Aguilar-Lozano L, Padilla-Ibarra J, Sandoval-Castro C, Vargas-Serafin CO et al (2015) Autoantibodies in predicting rheumatoid arthritis in healthy relatives of rheumatoid arthritis patients. Arthritis Rheum 67(11):2837–2844
Onishi S, Yoshio T, Nagashima T, Minota S (2010) Decrease in the levels of anti-cyclic citrullinated peptide antibody in Japanese patients with rheumatoid arthritis who responded to anti-tumor necrosis factor-α. Mod Rheumatol 20(5):528–530
Funding
We received an unrestricted grant from BMS to perform this review. They did not intervene in the discussions or in the elaboration of the manuscript. BMS only support us updating references when required.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E.M.M. received grants as advisor and honorarium as speaker bureau from: MSD, Roche, BMS, Hospira; Kern Pharma, Biogen, and Janssen. A.B. received funding for research from Roche, Abbvie, Pfizer, and UCB, has participated on advisory boards for BMS, UCB, Pfizer, and Roche, and has participated as speakers for Roche, BMS, MSD, Pfizer, UCB, and Abbvie. R.G.V. received funding for research or teaching from MSD, Roche, BMS, Abbvie, and UCB, has participated on advisory boards for Actelion, BMS, UCB, Pfizer, Roche, Hospira, Janssen, and Sandoz, and has delivered presentations sponsored by Roche, BMS, Pfizer, UCB, and Sandoz. J.G.R. is on the advisory boards of AbbVie, BMS, Hospira, Jansen, MSD, Pfizer, Roche, and UCB, has received lecture fees from BMS, Roche, MSD, and Pfizer, and has received research grants from Pfizer and Roche. M.A.G.-G. received grants/research support from Abbott, MSD, and Roche and consultation/ participation fees in company-sponsored speaker’s bureaus from Abbott, Pfizer, Roche, and MSD. R.S. is member of the Advisory Board of the la MHDA Evaluation Committee, Cat-Salut, Generalitat de Catalunya; conferences/advisory boards sponsored by Abbott/Abbvie, BMS, MSD, Roche, UCB, Pfizer, funding for research projects from BMS, MSD, Roche, UCB, Pfizer, FER, and SCR, and funding for training projects from MSD, BMS, and Abbvie. E.L. received funding for research projects from BMS, Abbvie, Roche, MSD, Pfizer, UCB, Gebro, and Novartis.
Ethical standard
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Martin-Mola, E., Balsa, A., García-Vicuna, R. et al. Anti-citrullinated peptide antibodies and their value for predicting responses to biologic agents: a review. Rheumatol Int 36, 1043–1063 (2016). https://doi.org/10.1007/s00296-016-3506-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-016-3506-3