Abstract
Autoantibodies in early rheumatoid arthritis (RA) have important diagnostic value. The association between the presence of autoantibodies against cyclic citrullinated peptide and the response to treatment is controversial. To prospectively evaluate a cohort of patients with early rheumatoid arthritis (<12 months of symptoms) in order to determine the association between serological markers (rheumatoid factor (RF), anti-citrullinated protein antibodies) such as anti-cyclic citrullinated peptide antibodies (anti-CCP) and citrullinated anti-vimentin (anti-Sa) with the occurrence of clinical remission, forty patients diagnosed with early RA at the time of diagnosis were evaluated and followed for 3 years, in use of standardized therapeutic treatment. Demographic and clinical data were recorded, disease activity score 28 (DAS 28), as well as serology tests (ELISA) for RF (IgM, IgG, and IgA), anti-CCP (CCP2, CCP3, and CCP3.1) and anti-Sa in the initial evaluation and at 3, 6, 12, 18, 24, and 36 months of follow-up. The outcome evaluated was the percentage of patients with clinical remission, which was defined by DAS 28 lower than 2.6. Comparisons were made through the Student t test, mixed-effects regression analysis, and analysis of variance (significance level of 5%). The mean age was 45 years, and a female predominance was observed (90%). At the time of diagnosis, RF was observed in 50% of cases (RF IgA—42%, RF IgG—30%, and RF IgM—50%), anti-CCP in 50% (no difference between CCP2, CCP3, and CCP3.1) and anti-Sa in 10%. After 3 years, no change in the RF prevalence and anti-CCP was observed, but the anti-Sa increased to 17.5% (P = 0.001). The percentage of patients in remission, low, moderate, and intense disease activity, according to the DAS 28, was of 0, 0, 7.5, and 92.5% (initial evaluation) and 22.5, 7.5, 32.5, and 37.5% (after 3 years). There were no associations of the presence of autoantibodies in baseline evaluation and in serial analysis with the percentage of clinical remission during follow-up of 3 years The presence of autoantibodies in early RA has no predictive value for clinical remission in early RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Remission, or the absence of disease activity, is the desired therapeutic target during the treatment of patients with rheumatoid arthritis (RA), especially in its initial phase [1]. However, like the concept of RA diagnosis, the concept of remission is complex. Disease remission, as defined by the European League Against Rheumatism (EULAR), which is currently widely used, is simple and based on a disease activity score 28 joints (DAS 28) below 2.6 [2].
The possible association between certain autoantibodies (e.g., rheumatoid factor—RF; anti-cyclic citrullinated peptide—anti-CCP; and anti-citrullinated vimentin—anti-Sa) and parameters of clinical outcome, including the occurrence of remission in patients with early rheumatoid arthritis (ERA), is not known in patients with initial RA. Establishing the usefulness of serological markers, individually and collectively, in the evaluation of disease prognosis is of great importance because it could validate the need for routine dosage of these markers (and repetition during the follow-up period).
The objective of this study was to prospectively evaluate a cohort of patients with ERA (less than 12 months of symptoms) to determine the possible association between autoantibodies (RF, anti-CCP, and anti-Sa) and the occurrence of remission.
Patients and methods
We conducted a prospective incident cohort in which consecutive patients diagnosed with ERA were assessed and followed regularly for 36 months from diagnosis. Patients were evaluated at the ERA clinic of the University Hospital of Brasilia (HUB), Brazil.
ERA was defined as the occurrence of joint symptoms compatible with the disease (pain and swelling in an articular inflammatory pattern, with or without morning stiffness or other manifestations suggestive of chronic joint inflammation, as assessed by a single observer), lasting more than 6 weeks and less than 12 months, regardless of the fulfillment of the classification criteria of the American College of Rheumatology (ACR).
Demographic and clinical data and DAS 28 results were recorded, and the analysis was performed and titers were determined for positive reaction against several autoantibodies to RA at baseline and serially at 3, 6, 12, 18, 24, and 36 months of follow-up.
The RF (IgG, IgM, and IgA) study was performed using the Quanta Lite™ RF IgA ELISA, Quanta Lite™ IgG RF ELISA, and Quanta Lite™ IgM RF ELISA (Inova Diagnostics, CA, USA) tests, according to the manufacturer’s protocol. Values greater than 15 IU/ml (IgM and IgA) and 20 IU/ml (FR IgG) were considered as positive cutoff points.
Anti-CCP was studied using the Quanta Lite™ CCP IgG ELISA, Quanta Lite™ CCP3 IgG ELISA, and Quanta Lite™ CCP3.1 IgG/IgA ELISA (Inova Diagnostics, CA, USA) tests, according to the manufacturer’s protocol. The serum of each patient was initially diluted to 1:100 in sample diluent. If the result of a sample was above an OD (optical density) of 2.5, it was retested with 1:500 and 1:2,500 dilutions, and the resulting unit value was multiplied by the dilution factor. The results were expressed as units (U), with <20 U being negative, 20–39 U being weakly positive, 40–59 U being moderately positive, and ≥60 U being strongly positive for all tests.
The anti-Sa detection assay was performed on the original plates developed by the McGill University Autoimmune Research Laboratory—Bovine MBP (myelin basic protein) ELISA [3]. The results were calculated and expressed in units, with <20 U being negative, 21–79 U being doubtful, and ≥80 U being positive.
The clinical outcome considered was the occurrence of remission at any time during the 36-month follow-up period. The EULAR definition of remission was used (DAS 28 < 2.6) [2].
Throughout monitoring, patients received the standard treatment used at the service, including disease-modifying antirheumatic drugs (DMARDs) and traditional and/or biological response modifier therapy (BRMT) as needed. The standard regimen recommended by the Department of Rheumatology, Brasília University Hospital (HUB), for the treatment of patients with a RA diagnosis was used. The observer was free to modify the patient’s regimen at any time during follow-up.
Statistical analysis
We applied the Kolmogorov–Smirnov normality test, and the distribution was considered normal if P > 0.05. To detect differences between two means, the Student t test or paired t test was used for samples of normal distribution, and nonparametric Mann–Whitney or Wilcoxon tests were used for those samples for which the normality hypothesis was rejected.
For the purposes of analysis, a regression model of mixed effects was applied, with the occurrence of remission as an outcome, using the following statistical model:
where y ijk is a measure of RF, anti-CCP, or anti-Sa titers in time k, on the j-th patient group i, and \( \mu + \alpha_{i} + \gamma_{k} + (\alpha \gamma )_{ik} \) is the average of the RF, anti-CCP, or anti-Sa titers of group i at time k
b ij is the random effect associated with the patient j in group i, N(0, \( \sigma_{B}^{2} \))
\( \varepsilon_{ijk} \) is the random error associated with the patient j of group i at time k, with variance and covariance matrix of random intercept (RI). Significance was considered if P < 0.05.
The sample size calculation was performed using a pilot sample of 10 patients, assuming that the statistical methodology used was a multivariate analysis of variance for repeated measures with interaction between groups. Considering a significance level of 5%, a test power of 80%, and the information obtained from the pilot sample, the minimum sample size was calculated to be 36 patients.
The study was approved by the research ethics committee of the Faculty of Medicine, University of Brasília, Brazil.
Results
Characteristics of the population studied
Forty patients with a RA diagnosis were followed for 36 months from the time of diagnosis. In this group, female individuals (36 patients, 90%) and those of white ethnicity (14 patients, 35%) predominated, and the mean age was 45.3 years (range, 21–71 years). The average duration of joint symptoms at diagnosis was 27 weeks (±15.59), with 13 patients (32.5%) experiencing less than 12 weeks of symptoms at diagnosis. All patients met the classification criteria of the ACR in the initial evaluation. There was no loss to follow-up of patients during the 3 years of the study. Table 1 summarizes the characteristics of the populations studied.
Therapeutic regimens
In the initial evaluation, 40 patients were using nonsteroidal anti-inflammatory drugs (NSAIDs), and two (5%) used prednisone at a dose below 10 mg/day (mean duration of 14.6 ± 2.4 weeks). After the initial evaluation, 37 patients (92.5%) were initiated on methotrexate (initial dose of 7.5 mg/week), with folic acid (5 mg/week) and a hydroxychloroquine (400 mg/day) supplementation.
After 3 years of follow-up, 8 patients (20%) retained the use of the initially prescribed therapy, hydroxychloroquine (mean dose of 400 mg/day) and methotrexate (mean dose of 20.5 mg/week), and 23 individuals (57 5%) used a non-biological DMARDs scheme different from the one originally prescribed.
Evolution of disease activity
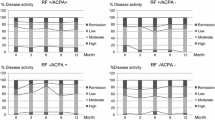
In the prospective evaluation of 40 patients diagnosed with RA who were followed for 3 years, the remission rates and low, moderate, and intense activity during follow-up, according to the EULAR criteria, were, respectively: at initial assessment (0, 0, 7.5, and 92.5%), at 3 months (2.5, 2.5, 52.5, and 42.5%), at 6 months (12.5, 5, 47,5, and 35%), at 12 months (17.5, 20, 47.5, and 15%), at 18 months (20.5, 30.7, 33.3, and 15.4%), at 24 months (20, 17.5, 35, and 27.5%), and at 36 months (22.5, 7.5, 32.5, and 37.5%).
Autoantibodies
Table 2 summarizes the basal serological characteristics and throughout the 3 years of cohort follow-up.
Serological markers and their association with remission in ERA
Negative RF, anti-CCP, and anti-Sa at baseline versus the occurrence of remission
Negative results for any of the three RF serotypes (IgA, IgG, and IgM) at baseline were not associated with the occurrence of remission in this population (IgA RF—relative risk 0.88, 95% IC: 0.64–1.22; IgG RF—relative risk 0.91, 95% IC: 0.67–1.26; and IgM RF—relative risk 0.74, 95% IC: 0.53–1.04). Similarly, we observed that a negative result for anti-CCP by any of the three techniques at the initial evaluation did not predict the occurrence of remission (CCP2—relative risk 0.84, 95% IC: 0.60–1.16; CCP3—relative risk 0.79, 95% IC: 0.55–1.12; and CCP3.1—relative risk 0.81, 95% IC: 0.58–1.14). A negative result for anti-Sa, at baseline, was also not a predictor for the occurrence of remission in our cohort (relative risk 0.92, 95% IC: 0.62–1.38).
Variation in the RF, anti-CCP, and anti-Sa titers over time versus the occurrence of remission
We analyzed anti-CCP (CCP2, CCP3, and CCP3.1) IgA, IgG, and IgM and anti-Sa RF behavior over time in the two groups, namely the “no remission” (patients who had not achieved remission during the period analyzed) versus the “remission” (patients who achieved remission at any time during follow-up) groups.
As shown in Table 3, which analyzes the significance of the effects of time, group, and the interaction between time and group and the estimate of the mean group and time log and the comparison between the log means of the three RF isotypes, anti-CCP, and anti-Sa by group over time, it was found that the interaction between time and group was not significant for RF IgA (P = 0.92), RF IgG (P = 0.92), RF IgM (P = 0.91), anti-CCP [CCP2 (P = 0.51), CCP3 (P = 0.66), and CCP3.1 (P = 0.71)], and anti-Sa (P = 0.74), suggesting that log changes in all autoantibodies evaluated over time were the same for the two groups.
Furthermore, the effect of the group was not significant, showing that the mean log of autoantibodies did not differ between those patients who achieved remission and those who did not (P = 0.21 for RF IgA, P = 0.25 for RF IgG, P = 0.13 for RF IgM, P = 1.39 for CCP2, P = 0.09 for CCP3, P = 0.08 for CCP3.1, and P = 0.35 for anti-Sa).
The effect of time was also not significant (P = 0.83 for RF IgA, P = 0.22 for RF IgG, P = 0.58 for RF IgM, P = 0.93 for CCP2, P = 0.91 for CCP3, P = 0.83 for CCP3.1, and P = 0.9 for anti-Sa); that is, the mean values tended to remain constant over time for all autoantibodies evaluated among patients who achieved or did not achieve remission.
As such, there was no difference between patients who achieved remission and those who did not by the EULAR criteria regarding the values of RF IgA, IgG, IgM, anti-CCP (CCP2 CCP3, and CCP3.1), and anti-Sa in our cohort over the 3 years of monitoring.
Discussion
In the population evaluated in our study, the negative results for any of the three RF serotypes (IgA RF, IgG RF, and IgM RF) in the initial evaluation were not predictive for the occurrence of remission during follow-up. The variation in the RF IgA, IgM, and IgG titers over the 3-year follow-up was not associated with the occurrence of remission according to the EULAR criteria.
Our results were similar to those of Vazquez et al. [4], who analyzed the factors associated with clinical remission in a cohort of 105 patients with early RA (less than 2 years of symptoms) who were followed for 2 years. They found no relationship between RF IgM and the occurrence of remission.
Also consistent with our findings were the results of Verschueren et al. [5], who followed 89 patients with early RA (less than 1 year of symptoms) for 1 year and found no relationship between the presence or absence of RF and the occurrence of clinical remission. Boire et al. [3] similarly found no relationship between a positive RF (RF IgM) result and the occurrence of remission (DAS 28 < 2.6) in 165 consecutive patients diagnosed with early RA (less than 1 year of symptoms) followed for 30 months. Contrary to these studies, Gossec et al. [6] followed 191 patients with early RA (less than 1 year of disease) for 5 years and reported that the negative RF (both IgA RF and IgM RF) results at baseline were associated with remission (defined as DAS < 1.6). Mancarella et al. [7] also showed that a negative baseline RF IgM would be a positive predictor of remission after 6 months of treatment with anti-TNF. However, these authors studied a cohort of patients with established RA and biological treatment, which does not allow for comparison of their data with our results.
Bas et al. [8] reported a negative association between the presence of FR IgA and IgM and the occurrence of remission in 27 patients with less than 1 year of RA who were followed for 8 years. It is possible that differences in the demographics of our population and those assessed in that study (white patients, Swiss, and French) and the longer follow-up in the study by Bas et al. may explain the difference in results.
There are no previous studies that have correlated RF IgG with clinical remission in early RA. In our cohort, the behavior of RF IgG, both at baseline and throughout time, was similar to the other serotypes analyzed; so, the study of RF IgG brought no additional information on the occurrence of clinical remission.
In our cohort, the negative baseline anti-CCP measured by any of the three techniques (CCP2, CCP3, and CCP3.1) was not a predictive factor for remission. There was no difference between patients who achieved remission or not according to EULAR criteria with regard to mean anti-CCP (CCP2, CCP3, and CCP3.1) throughout the 3 years of monitoring.
The association between anti-CCP and the occurrence of remission is controversial. Possible factors to explain the variation in results in the literature include differences in study populations and different remission criteria.
Consistent with our findings are those of Verschueren et al. [5], who followed 89 patients with early RA (less than 1 year of symptoms) for 1 year and found no relationship between the presence or absence of anti-CCP (CCP2) and the occurrence of clinical remission. Serdaroflu et al. [9] also found no association between anti-CCP (CCP2) and disease activity, including the occurrence of clinical remission. Gossec et al. [6], who followed 191 patients with early RA (less than 1 year of disease) for 5 years, found no relationship between the negative anti-CCP (CCP2) and the occurrence of remission in the third year, in contrast to what they reported for IgA and IgM. Boire et al. [3] evaluated 165 consecutive patients with early RA (less than 1 year of events) who were followed for 30 months, and found no relationship between the presence or the absence of anti-CCP (CCP2) and the occurrence of remission (DAS 28 < 2.6). Bas et al. [8], however, observed a negative association between the presence of anti-CCP (CCP2) and the occurrence of remission.
Our results with respect to CCP2 are in agreement with several other published studies [3, 5, 6, 9]. In our cohort, the performance of different techniques (CCP3 and CCP3.1) did not add information to the study of anti-CCP (CCP2) because none of them showed a correlation with the occurrence of remission in early RA.
In our study, we observed that the negative anti-Sa in the initial evaluation was not a risk factor for remission in the population evaluated. There was no difference between patients who did or did not achieve remission by EULAR criteria with regard to the mean anti-Sa in the studied cohort over the 3 years of monitoring.
There is little information on the relationship between anti-Sa and the occurrence of remission. Escalona et al. [10] reported that at least two subsets of autoantibodies are present in the serum of patients positive for anti-Sa: one directed against a 68-kDa protein and another against the 50/46-kDa typical bands of the Sa system. Both subsets of anti-SA antibodies showed fluctuations over time, with the 50/46-kDa antibodies being present during the RA activity period and the anti-68-KDa antibodies being present during the period of RA remission.
Boire et al. [3] did not find a relationship between the presence or absence of anti-Sa and the occurrence of remission (DAS 28 < 2.6), as assessed in 165 consecutive patients with early RA (less than 1 year of events) who were monitored for 30 months.
Wagner et al. [11] reported that anti-citrullinated vimentin, which was studied by another method (anti-MCV), would be a possible marker of disease activity because, in remission patients, the anti-MCV values often return to normal.
The findings allow us to conclude that the negative results for any of the three RF isotypes (IgA RF, IgG RF, and IgM RF), anti-CCP (CCP2, CCP3, and CCP3.1), and anti-Sa in the initial evaluation and the variation in antibody titers over 3 years were not predictors of the occurrence of remission during follow-up.
Investigations in larger cohorts of patients with early RA and with longer follow-up are needed to evaluate the characteristics of changes in the titers of the autoantibodies evaluated during the course of the disease, their correlation with disease prognosis, and the influence of specific therapies.
References
Sokka T, Envalds M, Pincus T (2008) Treatment of rheumatoid arthritis: a global perspective on the use of antirheumatic drugs. Mod Rheumatol 18:228–239
Smolen JS, Aletaha D (2008) Activity assessments in rheumatoid arthritis. Curr Opin Rheumatol 20:306–313
Boire G, Cossette P, de Brum-Fernandes AJ et al (2005) Anti-Sa antibodies and antibodies against cyclic citrullinated peptide are not equivalent as predictors of severe outcomes in patients with recent-onset polyarthritis. Arthritis Res Ther 7:R592–R603
Vázquez I, Graell E, Gratacós J, Cañete JD, Viñas O, Ercilla MG (2007) Prognostic markers of clinical remission in early rheumatoid arthritis after two years of DMARDs in a clinical setting. Clin Exp Rheumatol 25:231–238
Verschueren P, Esselens G, Westhovens R (2009) Predictors of remission, normalized physical function, and changes in the working situation during follow-up of patients with early rheumatoid arthritis: an observational study. Scand J Rheumatol 23:1–7
Gossec L, Dougados M, Goupille P, Cantagrel A, Sibila J, Meyer O (2004) Prognostic factors for remission in early rheumatoid arthritis: a multiparameter prospective study. Ann Rheum Dis 63:675–680
Mancarella L, Bobbio-Pallavicini F, Ceccarelli F et al (2007) Good clinical response, remission, and predictors of remission in rheumatoid arthritis patients treated with tumor necrosis factor alpha blockers: the GISEA study. J Rheumatol 34:1670–1673
Bas S, Genevay S, Meyer O, GAbay C (2003) Anti-cyclic citrullinated peptide antibodies, IgM and IgA rheumatoid factors in the diagnosis and prognosis of rheumatoid arthritis. Rheumatology 42:677–680
Serdaroflu M, ÇakÂrbay H, Defer O, Cengiz S, Kul S (2008) The association of anti-CCP antibodies with disease activity in rheumatoid arthritis. Rheumatol Int 28:965–970
Escalona M, López-Longo FJ, Gozález CM et al (2002) Anti-Sa sera from patients with rheumatoid arthritis contain at least 2 different subpopulations of anti-Sa antibodies. J Rheumatol 29:2053–2060
Wagner E, Skoumal M, Bayer PM, Klausofer K (2009) Antibody against mutated citrullinated vimentin: a new sensitive marker in the diagnosis of rheumatoid arthritis. Rheumatol Int 29:1315–1321
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
da Mota, L.M.H., dos Santos Neto, L.L., de Carvalho, J.F. et al. The presence of anti-citrullinated protein antibodies (ACPA) and rheumatoid factor on patients with rheumatoid arthritis (RA) does not interfere with the chance of clinical remission in a follow-up of 3 years. Rheumatol Int 32, 3807–3812 (2012). https://doi.org/10.1007/s00296-011-2260-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-011-2260-9