Abstract
The diagnosis of rheumatoid arthritis (RA) is primarily based on clinical symptoms, so it is often difficult to diagnose RA in very early stages of the disease. A disease-specific autoantibody that could be used as a serological marker would therefore be very useful. Most autoimmune diseases are characterized by a polyclonal B-cell response targeting multiple autoantigens. These immune responses are often not specific for a single disease. In this review, the most important autoantibody/autoantigen systems associated with RA are described and their utility as a diagnostic and prognostic tool, including their specificity, sensitivity and practical application, is discussed. We conclude that, at present, the antibody response directed to citrullinated antigens has the most valuable diagnostic and prognostic potential for RA.
Similar content being viewed by others
Introduction
RA is a common systemic autoimmune disease with a prevalence of about 1% worldwide. Although the etiology of the disease is still unknown, several risk factors have been identified. Like many autoimmune diseases, RA occurs more frequently in women than in men (3:1 ratio), suggesting a role for sex hormones. Genetic studies have demonstrated that a genetic predisposition resides in the HLA-DR locus. There is also evidence that environmental factors, such as infectious agents, oral contraceptives and smoking, may play a role [1].
RA is characterized by inflammation of the synovial membrane of diarthrodial joints. Early indications of RA are swelling and pain of the proximal interphalangeal and metacarpophalangeal joints. Later, the larger joints become affected, especially those of the knee, elbow and ankle. Large numbers of activated leukocytes infiltrate the synovial membrane, causing hyperplasia and inflammation, which in most cases leads to progressive destruction of cartilage and bone. Since RA is a systemic autoimmune disease, other parts/organs of the body may become affected at a later stage. An example of this is the formation of rheumatoid noduli. Peak onset typically occurs in the fourth and fifth decades of life.
With more sophisticated types of therapy becoming available, it is becoming more important to diagnose RA at an early stage of the disease, so that earlier treatment can be applied and major damage of joint tissue can be prevented. It is during the first period of the disease, when not all clinical parameters are manifest, that a specific and sensitive serological test is needed. Even more helpful would be the serological test being able to predict, in an early phase of RA, the erosive or nonerosive progression of the disease.
Over the past 25 years, many autoantibody activities in RA have been described. This review summarizes the most relevant, and attempts to discuss their specificity and possible diagnostic and prognostic value. We shall distinguish between RA-associated antibodies, which are present in RA but also in other diseases, and RA-specific autoantibodies, which appear to be exclusively present in RA. It is, of course, the category of RA-specific antibodies that is most relevant for the clinician.
Autoantibodies associated with RF
Rheumatoid factor
The so-called 'rheumatoid factor' (RF) was first described about 75 years ago; since then a vast amount of work has been performed on the incidence, nature and specificity of RF (reviewed in [2]). The RF antibody is present in about 75% of RA patients, but its specificity is limited since RF is also found in patients with other autoimmune diseases (e.g. Sjögren's syndrome), infectious diseases (e.g. hepatitis, tuberculosis), and to a certain extent in the healthy population (3–5%) and healthy elderly individuals (10–30%). Despite its relatively low specificity, the presence of RF is widely used as a diagnostic marker for RA.
RFs are antibodies directed to the crystallizable fragment of IgG molecules. They are found in every immunoglobulin subclass (IgE, IgM, IgA and IgG). IgG RF has a self-binding capacity that can result in the formation of very large immune complexes, which are able to (further) activate the immune system (reviewed in [3]). It is not clear whether RF is directly related to the symptoms of RA, although RF is found significantly more often in cases of aggressive joint inflammation. In those cases, RF titers are linearly related with the severity of inflammation. The clinical relevance of RF has been reviewed frequently (see, for example, [3,4]). Since the presence of RF is one of the American College of Rheumatology criteria for RA, the test is performed on a routine basis in most clinical laboratories. Some reports mention raised IgA-RF levels as a parameter for disease activity [5,6]. A combined routine determination of IgM-RF, IgG-RF and IgA-RF is recommended for an improved sensitivity, for diagnostic specificity and for predictive value [7,8].
Anti-RA33 antibodies
Hassfeld et al. [9] described a 33 kDa antigen recognized by sera from RA patients on immunoblots from soluble nuclear extracts of HeLa cells. The antigen, referred to as RA33, was recognized by 36% of the RA sera and by only 1% of the normal sera. Characterization of RA33 revealed that RA33 is identical to the A2 protein of the heterogeneous nuclear ribonucleoprotein complex [10]. Heterogeneous nuclear ribonucleoproteins are large nuclear structures present in every eukaryotic cell composed of long stretches of heterogeneous nuclear RNA associated with about 30 different proteins, with molecular weights varying between 34 and 120 kDa. The most abundant proteins in the heterogeneous nuclear ribonucleoprotein complexes, the so-called 'core' proteins, are named A1, A2, B1, B2, C1 and C2.
It has been suggested that RA33 is a marker for early arthritis [11]. However, the autoantibodies to RA33/A2 protein are not exclusively found in RA patients. They are also present in systemic lupus erythematosus (SLE) (25% of investigated sera) and mixed connective tissue disease sera [11,12].
Anticalpastatin
Calpains are calcium-ion-dependent neutral cysteine proteinases. Two forms of calpains exist: μ-calpains (calpain I, which needs micromolar concentrations of Ca2+ for activity) and m-calpains (which require millimolar amounts of Ca2+ for activity). Substrates of these enzymes are highly diverse and include cytoskeletal proteins, nuclear proteins, cytokines and extracellular matrix proteins including proteoglycans [13]. Elevated levels of extracellular calpain in the inflamed synovium have been reported, which suggests that calpains might be secreted by synovial cells and could play a role in cartilage degradation in RA [14,15].
Calpastatin is the natural inhibitor of calpains. Using immunoblots of recombinant protein, autoantibodies directed to calpastatin can be found in about 45% of the RA sera, but also sera from SLE, myositis and systemic sclerosis contain antibodies directed to calpastatin [16,17]. A recent study using recombinant fusion proteins with truncated forms of calpastatin showed that anticalpastatin antibodies can also be found in sera from healthy individuals, even in comparable numbers, relative to RA patients [18]. Autoantibodies directed to calpastatin could increase calpain activity, leading to enhanced cartilage damage, and could therefore contribute to the severity of the disease [14].
Other RA-associated autoantibodies
RA patients produce autoantibodies directed to many autoantigens, but most of them are not specific for RA. Among these nonspecific antibodies are those directed to a wide variety of cartilage proteins such as collagen and fibronectin, but also antiphospholipid antibodies and antineutrophil cytoplasmic antibodies (ANCA) can often be found.
Although autoantibodies against several types of collagens have been described, the autoimmune reaction directed to collagen type II (anti-CII) seems predominant. Anticollagen antibodies are present in about 30% of RA patients and only in HLA-DR4-positive ones [19]. Although anti-CII autoantibodies can be found in serum of only a small proportion of the RA patients, these antibodies and anti-CII-producing B cells are present in the joints of the majority of these patients [20]. It is not clear whether the occurrence of anticollagen autoantibodies plays a role in the pathogenesis of RA or is merely a result of the disease [3,19]. Anticollagen autoantibodies show a low specificity and can also be found in other autoimmune disorders (e.g. SLE, 20% occurrence; systemic sclerosis, 15% occurrence; relapsing polychondritis, 50% occurrence) and infectious diseases (e.g. leprosy, 50% occurrence). Anti-CII IgG titers in serum and synovial fluid appear to directly correlate with levels of acute-phase reactants, and of cytokines such as tumor necrosis factor-α and interleukin-6 [21]. A possible explanation for these findings is cross-reactivity with the first complement component, C1q, which has a collagen-like tail [22].
Fibronectin is a dimeric glycoprotein that interacts with collagens, fibrin(ogen), heparin and various cell surface adhesion molecules. It is present in connective tissue matrices and on the surface of epithelial cells. The protein is also (in a soluble form) present in plasma and other body fluids. Autoantibodies to fibronectin are found in about 14% of RA patients and show a low specificity (SLE, 34%) [23].
ANCA were initially discovered in serum of RA patients by immunofluorescence on neutrophilic granulocytes and can be subdivided into two groups depending on their localization: cytoplasmic ANCA, and perinuclear ANCA (reviewed in [24]). ANCA can be found in up to one-third of the RA patients, but can also be detected in other autoimmune conditions and various infectious diseases [25,26,27].
Autoantibodies directed to the nonhistone chromosomal proteins HMG1 and HMG2 can be detected in about 25–40% of the RA patients, but similar frequencies have also been reported for SLE, Sjögren's syndrome and scleroderma patients (see references in [28]).
Antiphospholipid antibodies, like autoantibodies directed to cardiolipin, are not only found in autoimmune diseases such as RA (4–49% occurrence) and SLE (~40% occurrence), but are also present in many infectious diseases (e.g. syphilis, 75% occurrence; leprosy, 67% occurrence). The incidence in RA can vary strongly, depending on the methodology of detection and the selection of patients (reviewed in [29]).
Autoantibodies specific for RF
Sa protein
The antigen Sa is recognized by autoantibodies in about 40% of the RA sera with a rather high specificity [30,31]. These antibodies can already be detected at an early stage of the disease, albeit with a rather low sensitivity (23%) [30,32]. The antigen is a 48–50 kDa protein, predominantly present in human placenta extracts [31]. It can also be detected in human spleen and RA pannus tissue, but not in cultured cells. As explained by Menard et al. [33], Sa possibly is a citrullinated form of the intermediate filament protein vimentin (in cultured cells, vimentin is normally not citrullinated). Other workers have postulated that part of the Sa activity could be identical to human α-enolase [34]. If the Sa protein indeed is citrullinated, the antigen can be categorized in the filaggrin/cyclic citrullinated peptide (CCP) family of citrullinated autoantigens (see below).
Heavy chain binding protein (p68)
Autoantibodies directed to the p68 protein, recently identified as heavy chain binding protein (BiP), occur in about 64% of RA patients and appear to be highly specific for the disease [35,36,37]. The reported specificity of these antibodies still awaits further confirmation by clinical studies. The BiP antigen is also a target of RA-specific T-cell and B-cell immune responses [38], and is over-expressed in RA synovial tissue compared with control tissue. BiP is a ubiquitously expressed chaperone protein predominantly localized in the endoplasmic reticulum. The major B-cell epitope of this antigen appears to be a N-acetylglucosamine carbohydrate group, which is possibly important for its cellular localization [39]. The BiP protein can be detected in the cytoplasm and endoplasmic reticulum of cultured cells, but also in low abundance at the cell surface. Under stress (especially heat shock) conditions, the antigen can relocalize to the nucleus [39]. This nonphysiological localization of the antigen, accompanied by a shift in its glycosylation pattern, might trigger antigenicity of BiP during the pathogenesis of RA. Anti-BiP antibodies can also be detected in mice with established collagen-induced or pristane-induced arthritis [37].
Glucose-6-phosphate isomerase
The household enzyme glucose-6-phosphate isomerase (GPI) was recently described as a novel autoantigen in RA [40]. The antibodies could be detected in 64% of RA patients but not in controls. Interestingly, anti-GPI antibodies are also present in T-cell receptor-transgenic mice. In this mouse model system, GPI can serve as an autoantigen for both B and T cells, and passive transfer of anti-GPI to normal healthy animals induces arthritis. The anti-GPI antibodies in humans appear to be produced locally, since anti-GPI titers were higher in RA synovial fluids as compared with RA sera. Immunohistochemistry of synovia from RA patients showed high concentrations of GPI on the surface of the synovial lining and on the endothelial cell surface of arterioles [40]. It is intriguing and significant that the same autoantigen is targeted by autoantibodies in RA patients and in a mouse model of RA.
Antiperinuclear factor/antikeratine antibodies/antifilaggrin/anti-CCP
In 1964 a highly specific RA antibody system directed to a protein component present in the keratohyaline granules in the cytoplasm of differentiating buccal mucosa cells was described. The antigen was referred to as perinuclear factor, and the antibody activity became known as antiperinuclear factor (APF) [41]. APF antibodies combined a relative high sensitivity (depending on the cohort of patients being studied, they were present in 49–91% of RA patients) with a strong specificity (73–99%, reviewed in [42]). The APF test never became popular because of several practical inconveniences. Only a few percent of an average (laboratory) population can donate buccal mucosa cells differentiated far enough to contain the peri-nuclear factor. Another inconvenience is the fact that the antibody activity can only be measured by indirect immunofluorescence, making interpretation of test results sometimes very difficult [42].
A related group of RA-specific autoantibodies, the so-called antikeratine antibodies (AKA), was first described in 1979 [43]. These antibodies stain keratin-like structures in the cornified layer of esophagus cryostat sections but do not recognize cytokeratins, as is suggested by the name. AKA can be detected by indirect immunofluorescence in 36–59% of RA sera with a specificity of 88–99% (reviewed in [42]). Several studies have shown that the APF and AKA antibodies target the same antigen, the epithelial protein filaggrin (for references see [44]).
Filaggrin (filament aggregating protein) is involved in the organization of cytoskeletal structures in epithelial cells and is synthesized as a large, heavily phosphorylated precursor protein, profilaggrin. During differentiation of epithelial cells, profilaggrin is partly dephosphorylated and proteolytically cleaved into 10–12 filaggrin subunits. Finally, about 20% of the arginine residues are enzymatically deiminated to citrulline residues [45]. Conversion of the basic amino acid arginine into the neutral residue citrulline is catalyzed by the enzyme peptidylarginine de-iminase (Fig. 1). It is this modification that has been shown to be essential for the autoantigenicity of filaggrin [46,47].
Immunoblotting assays and an enzyme-linked immunosorbent assay (ELISA) using filaggrin purified from human skin as an antigen have been developed for the detection of antifilaggrin antibodies (AFA). Vincent et al. [48] could detect AFA in 41% of RA sera with 99% specificity. When combining the AFA immunoblot assay with AKA testing, a much higher sensitivity (64%), without loss of specificity, could be achieved [48]. However, the sensitivity of the assay appears to be dependent on the method for purification of the filaggrin. Slack et al. calculated sensitivities of 12 and 16% for two different filaggrin preparations, while only one of five positive sera reacted with both preparations [49]. The AFA-ELISA is somewhat more sensitive (47–54%) than the immunoblot assay [50,51], but the results are in good agreement with APF data obtained with the same set of sera [52]. Using in vitro deiminated recombinant filaggrin, Nogueira et al. [53] could detect AFA in about 52% of RA sera. The differences in AFA, APF and AKA results and the influence of the antigen preparation imply that several (rather than one single) epi-topes are recognized.
The AFA-ELISA test detected 45% of RF-negative erosive cases, in particular those with larger numbers of erosive joints. Testing for AFA could therefore supplement RF in the prediction of erosive disease. The test could also be helpful in the diagnosis of RA in those cases that do not completely fulfill the 1987 American College of Rheumatology criteria [52]. In a case-control study, pre-illness AFA titers were found to directly be related to the risk of developing RF-positive RA, but not RF-negative arthritis [54]. AFA are present early in the disease, as is the case with APF and anti-CCP antibodies (see below), and raised AFA levels correlate with the severity of the disease. However, there is discussion whether disease activity and radiological damage can be predicted by AFA levels [51,52,55].
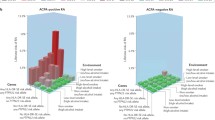
One disadvantage of the AFA test is the difficulty of obtaining an antigen preparation that is pure and contains a reproducible citrulline content. These problems do not occur when citrullinated peptides are used as the antigen, as has been shown by Schellekens et al. [46]. RA sera, however, show different patterns of reactivity with the citrullinated peptide variants, which emphasizes the heterogeneous nature of the autoimmune response. With a combination of nine citrullinated peptide variants, a sensitivity of 76% could be reached with a specificity of 96% [46]. The test could be improved and simplified using a single cyclic peptide that has a three-dimensional structure optimally recognized by the heterogeneous population of RA autoantibodies [56]. Recent studies indicate that this anti-CCP test (manufactured by Euro-Diagnostica BV, Arnheim, The Netherlands) is extremely specific (~98%) and has a reasonable sensitivity of 68–75% [57,58] (van Boekel and de Jong, unpublished observations, 2001). Anti-CCP antibodies can be detected very early in RA, although with a somewhat lower sensitivity (40–60%) [32,57,58,59,60]. Anti-CCP appears to be a good prognostic marker and has a high discriminating power between erosive and nonerosive RA [61]. RA patients positive for anti-CCP develop significantly more radiological damage than anti-CCP-negative patients [59,60], although anti-CCP combined with RF appears to be an even better prognostic marker [56,58,61].
The results described (supported by the fact that nonfilaggrin-like citrulline-containing antigens are also recognized by RA sera [62]) suggest that, in principle, most citrullinated proteins/peptides will be recognized by autoantibodies in RA sera, all be it with different sensitivities and specificities. Since filaggrin is not present in the joint, it is reasonable to assume that other citrulline-containing proteins are present in the RA synovium. In RA pannus tissue, AFA are produced by local plasma cells and constitute a higher proportion of IgG than in serum [63]. Furthermore, B cells from the synovial fluid of anti-CCP-positive RA patients spontaneously produce anti-CCP antibodies, while peripheral blood B cells or B cells from anti-CCP-negative RA patients do not [64]. This suggests an antigen-driven maturation of CCP-specific B cells at the site of inflammation in RA. One of these possible autoantigens, citrullinated fibrin, has recently been identified [65]. The possible role of citrullinated fibrin and other citrullinated antigens in the pathophysiology of RA remains to be elucidated [66].
Conclusions and discussion
RA is accompanied by the occurrence of many autoantibodies in the serum of the patient. Most of these antibodies are not specific for RA because they also occur in other inflammatory conditions. Other antibodies appear to be more specific and are, in some cases, almost exclusively present in RA.
The possible pathogenic nature of autoantibodies in RA is still controversial (reviewed in [67]). The evidence for the pathogenic involvement of RF in RA can, at best, be considered indirect [67]. There is an association of RF with the severity of RA, and RF-positive patients can turn RF-negative following therapy [3,68]. Administration of human IgG or IgM monoclonal RF to mice (suffering from collagen-induced arthritis) results in an enhanced activity and severity of the disease and in an increase in anticollagen antibody levels [69]. RF has the capacity to activate the complement cascade, which could be an important factor in the disease activity and the chronic character of RA [3,70]. RF is also found in healthy individuals, however, and possibly even plays a physiological role in immune complex clearance [3].
Anticollagen antibodies possibly have pathogenic potential. Injection of serum IgG from a RF-negative patient with high levels of anti-CII antibodies induces a mild form of inflammatory arthritis in mice [71,72], but the pathogenic involvement of anti-CII antibodies is much less evident in human RA. Anticalpastatin antibodies could contribute to the pathology by inhibiting calpastatin functioning [13]. The participation of other autoantibody systems (such as anticitrullinated protein, anti-GPI and anti-Sa antibodies) in RA pathogenesis is still unclear, although their high specificity adds to the increasing body of evidence that they may be important in maintaining RA.
Some of the RA-specific antibodies might be very helpful in the early diagnosis and prognosis of the disease. These antibodies are presented in Table 1. Most promising for the future appears to be the growing family of antigens containing one or more citrulline residues. Some of these antigens (i.e. filaggrin and CCP) have recently been applied in simple and easy-to-use ELISA tests, and have been shown to be very specific for RA, to be able to diagnose RA in a very early phase of the disease, and to predict erosive disease. As such, this class of anticitrullinated protein autoantibodies has the potential to become the serological marker for RA of the future.
Although we know that the anticitrullinated protein antibodies are locally generated in the inflamed joint, we also know that both filaggrin and CCP are not present in this tissue. It was recently shown that fibrin in the pannus tissue is citrullinated. This intriguing finding underlines the idea that local citrullination of extravascular proteins might be one of the initiating event(s) leading to autoimmunity in RA.
The key question why only patients with RA develop antibodies to citrullinated (synovial) proteins remains to be answered. Further research will hopefully reveal the significance of protein citrullination in the immunopathology of RA.
Abbreviations
- AFA:
-
antifilaggrin antibodies
- AKA:
-
antikeratine antibodies
- ANCA:
-
antineutrophil cytoplasmic antibodies
- anti-CII:
-
antibody response to collagen type II
- APF:
-
antiperinuclear factor
- BiP:
-
heavy chain binding protein
- CCP:
-
cyclic citrullinated peptide
- ELISA:
-
enzyme-linked immunosorbent assay
- GPI:
-
glucose-6-phosphate isomerase
- RA:
-
rheumatoid arthritis
- RF:
-
rheumatoid factor
- SLE:
-
systemic lupus erythematosus
References
Gabriel SE: The epidemiology of rheumatoid arthritis. Rheum Dis Clin North Am. 2001, 27: 269-281.
Mageed RA: The RF antigen. In Manual of Biological Markers of Disease. Edited by van Venrooij WJ & Maini RN. Dordrecht: Kluwer Academic Publishers;. 1996, 1-27. section B1.1
Smolen JS: Autoantibodies in rheumatoid arthritis. In Manual of Biological Markers of Disease. Edited by van Venrooij WJ & Maini RN. Dordrecht: Kluwer Academic Publishers;. 1996, 1-18. section C1.1
Sutton B, Corper A, Bonagura V, Taussig M: The structure and origin of rheumatoid factors. Immunol Today. 2000, 4: 177-183. 10.1016/S0167-5699(00)01589-9.
Pai S, Pai L, Birkenfeldt R: Correlation of serum IgA rheumatoid factor levels with disease severity in rheumatoid arthritis. Scand J Rheumatol. 1998, 27: 252-256. 10.1080/030097498442352.
Hoessien DA, Jonsson T, Davies E, Scott DL: Clinical significance of IgA rheumatoid factor subclasses in rheumatoid arthritis. J Rheumatol. 1997, 24: 2119-2122.
Jonsson T, Steinsson K, Jonsson H, Geirsson AJ, Thorsteinsson J, Valdimarsson H: Combined elevation of IgM and IgA rheumatoid factor has a high diagnostic specificity for rheumatoid arthritis. Rheum Int. 1998, 18: 119-122. 10.1007/s002960050069.
Swedler W, Wallman J, Froelich CJ, Teodorescu M: Routine measurement of IgM, IgG and IgA rheumatoid factors: High sensitivity, specificity and predictive value for rheumatoid arthritis. J Rheumatol. 1997, 24: 1037-1044.
Hassfeld W, Steiner G, Hartmuth K, Kolarz G, Scherak O, Graninger W, Thumb N, Smolen JS: Demonstration of a new antinuclear antibody (anti-RA33) that is highly specific for rheumatoid arthritis. Arthritis Rheum. 1989, 32: 1515-1520.
Steiner G, Hartmuth K, Skriner K, Maurer FI, Sinski A, Thalmann E, Hassfeld W, Barta A, Smolen JS: Purification and partial sequencing of the nuclear autoantigen RA33 shows that it is indistinguishable from the A2 protein of the heterogeneous nuclear ribonucleoprotein complex. J Clin Invest. 1992, 90: 1061-1066.
Hassfeld W, Steiner G, Graninger W, Witzmann G, Schweitzer H, Smolen JS: Autoantibody to the nuclear antigen RA33: a marker for early rheumatoid arthritis. Br J Rheumatol. 1993, 32: 199-203.
Skriner K, Sommergruber WH, Tremmel V, Fischer I, Barta A, Smolen JS, Steiner G: Anti-A2/RA33 autoantibodies are directed to the RNA binding region of the A2 protein of the heterogeneous nuclear ribonucleoprotein complex. Differential epitope recognition in rheumatoid arthritis, systemic lupus erythematosus, and mixed connective tissue disease. J Clin Invest. 1997, 100: 127-135.
Menard HA, El-Amine M: The calpain–calpastatin system in rheumatoid arthritis. Immunol Today. 1996, 17: 545-547. 10.1016/S0167-5699(96)30064-9.
Yamamoto S, Shimizu K, Suzuki K, Nakagawa Y, Yamamuro T: Calcium-dependent cysteine proteinase (calpain) in human arthritic synovial joints. Arthritis Rheum. 1992, 35: 1309-1317.
Szomor Z, Shimizu K, Fujimori Y, Yamamoto S, Yamamuro T: Appearance of calpain correlates with arthritis and cartilage destruction in collagen induced arthritic knee joints of mice. Ann Rheum Dis. 1995, 54: 477-483.
Despres N, Talbot G, Plouffe B, Boire G, Menard HA: Detection and expression of a cDNA clone that encodes a polypeptide containing two inhibitory domains of human calpastatin and its recognition by rheumatoid arthritis sera. J Clin Invest. 1995, 95: 1891-1896.
Mimori T, Suganuma K, Tanami Y, Nojima T, Matsumura M, Fujii T, Yoshizawa T, Suzuki K, Akizuki M: Autoantibodies to calpastatin (an endogenous inhibitor for calcium-dependent neutral protease, calpain) in systemic rheumatic diseases. Proc Natl Acad Sci USA. 1995, 92: 7267-7271.
Lackner KJ, Schlosser U, Lang B, Schmitz G: Autoantibodies against human calpastatin in rheumatoid arthritis: epitope mapping and analysis of patient sera. Br J Rheumatol. 1998, 37: 1164-1171. 10.1093/rheumatology/37.11.1164.
Rönnelid J, Lysholm J, Engstrom LA, Klareskog L, Heyman B: Local anti-type II collagen antibody production in rheumatoid arthritis synovial fluid. Evidence for an HLA-DR4-restricted IgG response. Arthritis Rheum. 1994, 37: 1023-1029.
Tarkowski A, Klareskog L, Carlsten H, Herberts P, Koopman WJ: Secretion of antibodies to types I and II collagen by synovial tissue cells in patients with rheumatoid arthritis. Arthritis Rheum. 1989, 32: 1087-1092.
Kim W-U, Yoo W-H, Park W, Kang Y-M, Kim S-I, Park J-H, Lee S-S, Joo Y-S, Min J-K, Hong Y-S, Lee S-H, Park S-H, Cho C-S, Kim H-Y: IgG antibodies to type II collagen reflect inflammatory activity in patients with rheumatoid arthritis. J Rheumatol. 2000, 27: 575-581.
Reid KB: Complete amino sequences of the three collagen-like regions present in subcomponent C1q of the first component of human complement. Biochem J. 1979, 179: 367-371.
Atta MS, Lim KL, Ala'Aldeen DA, Powell RJ, Todd I: Investigation of the prevalence and clinical associations of antibodies to human fibronectin in systemic lupus erythematosis. Ann Rheum Dis. 1995, 54: 117-124.
Charles PJ, Maini RN: Antibodies to neutrophil cytoplasmic antigens in rheumatoid arthritis. Adv Exp Med Biol. 1993, 336: 367-370.
Schnabel A, Hauschild S, Gross WL: Anti-neutrophil cytoplasmic antibodies in generalized autoimmune diseases. Int Arch Allergy Immunol. 1996, 109: 201-206.
Kallenberg CG, Mulder AH, Tervaert JW: Antineutrophil cytoplasmic antibodies: a still-growing class of autoantibodies in inflammatory disorders. Am J Med. 1992, 93: 675-682.
Mulder AH, Horst G, van-Leeuwen MA, Limburg PC, Kallenberg CG: Antineutrophil cytoplasmic antibodies in rheumatoid arthritis. Characterization and clinical correlations. Arthritis Rheum. 1993, 36: 1054-1060.
Uesugi H, Ozaki S, Sobajima J, Osakada F, Shirakawa H, Yoshida M, Nakao K: Prevalence and characterization of novel pANCA, antibodies to the high mobility group non-histone chromosomal proteins HMG1 and HMG2, in systemic rheumatic diseases. J Rheumatol. 1998, 25: 703-709.
Morris V, Mackworth-Young C: Antiphospholipid antibodies: clinical aspects. In Manual of Biological Markers of Disease. Edited by van Venrooij WJ & Maini RN. Dordrecht: Kluwer Academic Publishers;. 1996, 1-14. section C2.5
Hayem G, Chazerain P, Combe B, Elias A, Haim T, Nicaise P, Benali K, Eliaou JF, Kahn MF, Sany J, Meyer O: Anti-Sa antibody is an accurate diagnostic and prognostic marker in adult rheumatoid arthritis. J Rheumatol. 1999, 26: 7-13.
Despres N, Boire G, Lopez-Longo FJ, Menard HA: The Sa system: a novel antigen–antibody system specific for rheumatoid arthritis. J Rheumatol. 1994, 21: 1027-1033.
Goldbach-Mansky R, Lee J, McCoy A, Hoxworth J, Yarboro C, Smolen JS, Steiner G, Rosen A, Zhang C, Ménard HA, Zhou ZJ, Palosuo T, van Venrooij WJ, Wilder RL, Klippel JH, Schumacher HR, El-Gabalawy HS: Rheumatoid arthritis associated autoan-tibodies in patients with synovitis of recent onset. Arthritis Res. 2000, 2: 236-243. 10.1186/ar93.
Menard HA, Boire G, Lopez-Longo FJ, Lapointe S, Larose A: Insights into rheumatoid arthritis derived from the Sa immune system. ArthritisRes. 2000, 2: 429-432. 10.1186/ar122.
Saulot V, Yon G, Vittecoq O, Charlionnet R, Machour N, Lange C, Marvin L, Gilbert D, Le Loet X: Sa, Alpha-enolase and rheumatoid arthritis [abstract]. Arthritis Rheum. 2000, 43(suppl): S68-
Bläβ S, Specker C, Lakomek HJ, Schneider EM, Schwochau M: Novel 68 kDa autoantigen detected by rheumatoid arthritis specific antibodies. Ann Rheum Dis. 1995, 54: 355-360.
Bläβ S, Union A, Raymackers J, Schumann F, Ungethüm U, Müller-Steinbach S, De Keyser F, Engel J-M, Burmester GR: The stress protein BiP is overexpressed and is a major B and T cell target in rheumatoid arthritis. Arthritis Rheum. 2001, 44: 761-771. 10.1002/1529-0131(200104)44:4<761::AID-ANR132>3.3.CO;2-J.
Corrigall VM, Bodman-Smith MD, Fife MS, Canas B, Myers LK, Wooley PH, Soh C, Staines NA, Pappin DJC, Berlo SE, van Eden W, van der Zee R, Lanchbury JS, Panayi GS: The human endoplasmatic reticulum molecular chaperone BiP is an autoanti-gen for rheumatoid arthritis and prevents the induction of experimental arthritis. J Immunol. 2001, 166: 1492-1498.
Bläβ S, Haferkamp C, Specker C, Schwochau M, Schneider M, Schneider EM: Rheumatoid arthritis: autoreactive T cells recognising a novel 68k autoantigen. Ann Rheum Dis. 1997, 56: 317-322.
Bläβ S, Meier C, Vohr HW, Schwochau M, Specker C, Burmester GR: The p68 autoantigen characteristic of rheumatoid arthritis is reactive with carbohydrate epitope specific autoantibodies. Ann Rheum Dis. 1998, 57: 220-225.
Schaller M, Burton DR, Ditzel HJ: Autoantibodies to GPI in rheumatoid arthritis: linkage between an animal model and human disease. Nat Immunol. 2001, 2: 746-753. 10.1038/90696.
Nienhuis RLF, Mandena EA: A new serum factor in patients with rheumatoid arthritis. The antiperinuclear factor. Ann Rheum Dis. 1964, 23: 302-305.
Hoet RM, Van Venrooij WJ: The antiperinuclear factor and antikeratin antibodies in rheumatoid arthritis. In Rheumatoid Arthritis. Edited by Smolen J, Kalden J & Maini RN. Berlin: Springer Verlag;. 1992, 299-318.
Young BJJ, Mallya RK, Leslie RDG, Clark CJM, Hamblin TJ: Anti-keratin antibodies in rheumatoid arthritis. Br Med J. 1979, 2: 97-99.
Sebbag M, Simon M, Vincent C, Masson-Bessière C, Girbal E, Durieux JJ, Serre G: The antiperinuclear factor and the so-called antikeratin antibodies are the same rheumatoid arthritis-specific autoantibodies. J Clin Invest. 1995, 95: 2672-2679.
Gan SQ, McBride OW, Idler WW, Nedialka M, Steinert PM: Organization, structure, and polymorphisms of the human profillagrin gene. Biochemistry. 1990, 29: 9423-9440.
Schellekens GA, de Jong BAW, van den Hoogen FHJ, van de Putte LBA: Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J Clin Invest. 1998, 101: 273-281.
Girbal-Neuhauser E, Durieux J-J, Arnaud M, Dalbon P, Sebbag M, Vincent C, Simon M, Senshu T, Masson-Bessière C, Jolivet-Reynaud C, Jolivet M, Serre G: The epitopes targeted by the rheumatoid arthritis-associated antifilaggrin autoantibodies are posttranslationally generated on various sites of (pro)filaggrin by deimination of arginine residues. J Immunol. 1999, 162: 585-594.
Vincent C, Simon M, Sebbag M, Girbal-Neuhauser E, Durieux JJ, Cantagrel A, Fournie B, Mazieres B, Serre G: Immunoblotting detection of autoantibodies to human epidermis filaggrin: a new diagnostic test for rheumatoid arthritis. J Rheumatol. 1998, 25: 838-846.
Slack SL, Mannik M, Dale BA: Diagnostic value of antibodies to filaggrin in rheumatoid arthritis. J Rheumatol. 1998, 25: 847-851.
Palosuo T, Lukka M, Alenius H, Kalkkinen N, Aho K, Kurki P, Heikkila R, Nykanen M, von Essen R: Purification of filaggrin from human epidermis and measurement of antifilaggrin autoantibodies in sera from patients with rheumatoid arthritis by an enzyme-linked immunosorbent assay. Int Arch Allegy Immunol. 1998, 115: 294-302. 10.1159/000069460.
Paimela L, Palosuo T, Aho K, Lukka M, Kurki P, Leirisalo-Repo M, von Essen R: Association of autoantibodies to filaggrin with an active disease in early rheumatoid arthritis. Ann Rheum Disease. 2001, 60: 32-35. 10.1136/ard.60.1.32.
Aho K, Palosuo T, Lukka M, Kurki P, Isomaki H, Kautiainen H, von Essen R: Anti-filaggrin antibodies in recent-onset arthritis. Scand J Rheumatol. 1999, 28: 113-116. 10.1080/030097499442586.
Nogueira L, Sebbag M, Vincent C, Arnaud M, Fournié B, Cantagrel A: Performance of two ELISAs for antifilaggrin autoantibodies, using either affinity-purified or deiminated recombinant human filaggrin, in the diagnosis of rheumatoid arthritis. Ann Rheum Dis. 2001, 60: 882-887.
Aho K, Palosuo T, Heliovaara M, Knekt P, Alha P, von Essen R: Antifilaggrin antibodies within "normal" range predict rheumatoid arthritis in a linear fashion. J Rheumatol. 2000, 27: 2743-2746.
Forslind K, Vincent C, Serre G, Svensson B: Antifilaggrin autoantibodies in early rheumatoid arthritis. Scand J Rheumatol. 2000, 29: 320-322. 10.1080/030097400447714.
Schellekens GA, Visser H, de Jong BAW, van den Hoogen FH, Hazes JM, Breedeveld FC, van Venrooij WJ: The diagnostic properties of rheumatoid arthritis antibodies recognizing a cyclic citrullinated peptide. Arthritis Rheum. 2000, 43: 155-163. 10.1002/1529-0131(200001)43:1<155::AID-ANR20>3.0.CO;2-3.
Bizzaro N, Mazzanti G, Tonutti E, Villalta D, Tozzoli R: Diagnostic accuracy of the anti-citrulline antibody assay for rheumatoid arthritis. Clin Chem. 2001, 47: 1089-1093.
Vencovský J, Šedová L, Machácek S, Kafková J, Gatterová J, Pešáková V, Ruzicková S: Autoantibodies can be prognostic markers of an erosive disease in early rheumatoid arthritis. Ann Rheum Dis. 2001,
van Jaarsveld CHM, ter Borg EJ, Jacobs JWG, Schellekens GA, Gmelig-Meyling FHJ, van Booma-Frankfort C, de Jong BAW, van Venrooij WJ, Bijlsma JWJ: The prognostic value of the antiperi-nuclear factor, anti-citrullinated peptide antibodies and rheumatoid factor in early rheumatoid arthritis. Clin Exp Rheumatol. 1999, 17: 689-697.
Kroot EJJA, de Jong BAW, van Leeuwen MA, Swinkels H, van den Hoogen FHJ, van't Hof M, van de Putte LBA, van Rijswijk MH, van Venrooij WJ, van Riel PLCM: The prognostic value of anti-cyclic citrullinated peptide antibody in patients with recent-onset rheumatoid arthritis. Arthritis Rheum. 2000, 43: 1831-1835. 10.1002/1529-0131(200008)43:8<1831::AID-ANR19>3.0.CO;2-6.
Visser H, le Cessie S, Vos K, Breedveld FC, Hazes JMW: How to diagnose rheumatoid arthritis early? A prediction model for persistent (erosive) arthritis. Arthritis Rheum. 2001,
Lapointe E, Déry U, Vaillanciurt F, Ménard HA: Rheumatoid sera potentially recognize all citrullinated proteins [abstract]. Arthritis Rheum. 1999, 42: S86-
Masson-Bessière C, Sebbag M, Durieux JJ, Norgueira L, Vincent C, Girbal-Neuhauser E, Durroux R, Cantagrel A, Serre G: In the rheumatoid pannus, anti-filaggrin autoantibodies are produced by local plasma cells and constitute a higher proportion of IgG than in synovial fluid and serum. Clin Exp Immunol. 2000, 119: 544-552. 10.1046/j.1365-2249.2000.01171.x.
Reparon-Schuijt CC, van Esch WJE, van Kooten C, Schellekens GA, de Jong BAW, van Venrooij WJ, Breedveld FC, Verweij CL: Secretion of anti-citrulline-containing peptide antibody by B lymphocytes in rheumatoid arthritis. Arthritis Rheum. 2001, 44: 41-47. 10.1002/1529-0131(200101)44:1<41::AID-ANR6>3.0.CO;2-0.
Masson-Bessière C, Sebbag M, Girbal-Neuhauser E, Nogueira L, Vincent C, Senshu T, Serre G: The major synovial targets of the rheumatoid arthritis-specific antifilaggrin autoantibodies are deiminated forms of the α and β-chains of fibrin. J Immunol. 2001, 166: 4177-4184.
Serre G: Autoantibodies to filaggrin/deiminated fibrin (AFA) are useful for the diagnosis and prognosis of rheumatoid arthritis, and are probably involved in the pathophysiology of the disease. Joint Bone Spine. 2001, 68: 103-105. 10.1016/S1297-319X(01)00259-7.
Smolen JS, Steiner G: Are autoantibodies active players or epiphenomena?. Curr Opin Rheumatol. 1998, 10: 201-206.
Cordonnier C, Meyer O, Palazzo E, de Bandt M, Elias A, Nicaise P, Haim T, Kahn MF, Chatellier G: Diagnostic value of anti-RA33 antibody, antikeratin antibody, perinuclear factor and antinuclear antibody in early rheumatoid arthritis: comparison with rheumatoid factor. Br J Rheumatol. 1996, 35: 620-624.
Ezaki E, Okada M, Yoshikawa Y, Fujikawa Y, Hashimoto M, Otsuka M, Nomura T, Yamamoto K, Watanabe T, Shingu M, Nobunaga M: Human monoclonal rheumatoid factors augment arthritis in mice by the activation of T-cells. Clin Exp Immunol. 1996, 104: 474-482. 10.1046/j.1365-2249.1996.55764.x.
Breitner S, Störkel S, Reichel W, Loos M: Complement components C1q, C1r/C1s and C1INH in rheumatoid arthritis. Arthritis Rheum. 1995, 38: 492-498.
Wooley PH, Luthra HS, Singh SK, Huse AR, Stuart JM, David CS: Passive transfer of arthritis to mice by injection of human anti-type II collagen antibody. Mayo Clin Proc. 1984, 59: 737-743.
Staines NA, Wooley PH: Collagen arthritis – what can it teach us?. Br J Rheumatol. 1994, 33: 798-807.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Boekel, M.A., Vossenaar, E.R., van den Hoogen, F.H. et al. Autoantibody systems in rheumatoid arthritis: specificity, sensitivity and diagnostic value. Arthritis Res Ther 4, 87 (2001). https://doi.org/10.1186/ar395
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar395