Abstract
Purpose
The medial meniscus is a secondary stabilizer of anterior tibial translation in anterior cruciate ligament (ACL)-deficient knees. ACL reconstruction effectively restores an increased anterior tibial translation in the ACL-deficient knee. However, knee osteoarthritis sometimes develops in ACL-reconstructed patients during a long-term follow-up period. We hypothesized that the medial meniscal position would be different between the ACL-deficient and reconstructed knees. The aim of this study was to investigate pre-operative and postoperative location of the medial meniscus in patients who underwent ACL reconstruction.
Methods
ACL-reconstructed knees (28 knees) and normal knees (27 knees) were investigated. Medial tibial plateau length (MTPL) and medial tibial plateau width (MTPW) were determined using radiographic images. Magnetic resonance imaging (MRI)-based medial meniscal length (MML), medial meniscal width (MMW), and medial meniscal extrusion (MME) were measured. Postoperative change in the MML, MMW, and MME were evaluated and compared with those in normal knees.
Results
No significant differences between the ACL-deficient (pre-operative) and normal groups were noted. The ACL-reconstructed (postoperative) group showed an increase in the MML, in the percentage of the MML (%MML = 100 MML/MTPL), and in the MME. Significant differences between postoperative and normal groups were observed in the MML, %MML, and MME. MMW and MMW percentage (100 MMW/MTPW) were similar in all groups.
Conclusions
The anteroposterior length and radial extrusion of the medial meniscus increased after ACL reconstruction. Transposition of the medial meniscus may be a possible cause of developing further degenerative knee joint disorders after ACL reconstruction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The medial meniscus is an important secondary stabilizer for excessive anterior tibial translation in anterior cruciate ligament (ACL)-deficient knees [1–5]. Abnormal anterior tibial translation influences the anatomical relationship between the femoral condyle, meniscus, and tibia [6]. This is considered a mechanism for the increased incidence of medial meniscal tears observed in patients with chronic ACL insufficiency [2]. ACL-injured patients with concomitant medial meniscal tears have more frequent knee instability episodes than those without medial meniscal tears [7]. Therefore, reducing the resultant force in the medial meniscus is another motive of ACL reconstruction. However, in a systematic literature review, there is no reason to believe that ACL reconstruction reduces the incidence of further medial meniscal tears [8]. In addition, knee osteoarthritis sometimes develops in ACL-reconstructed patients during a long-term follow-up period [9]. The risk of knee arthroplasty following ACL reconstruction is seven times greater than that of control patients [10]. Based on this literature, we considered that ACL reconstruction would change the medial meniscal status involved in the medial meniscal position and extrusion.
Assessment of the meniscal size is useful for evaluating extrusion, movement, and tibial plateau coverage of the meniscus [11, 12]. The meniscal size is determined by measuring the meniscal margins obtained by magnetic resonance imaging (MRI) [13]. However, sizing inaccuracies that result from difficulty differentiating meniscal margins, radiographic errors in magnification, and the incorrect identification of bony landmarks have been reported [14, 15]. Furthermore, the transverse, sagittal, and coronal planes of the knee observed using MRI often vary among patients and MRI scans. We previously established a MRI-based multi-slice assessment technique to compare the pre-operative and postoperative length of the meniscus in the same patient [15]. We also reported that the percentage of MRI-based medial meniscal length (MML) against the radiographic measurement of the medial tibial plateau length (MTPL), defined as MML percentage (%MML), significantly changed when all-inside medial meniscal repair concomitant with ACL reconstruction was performed in patients with peripheral longitudinal tears of the medial meniscus and ACL insufficiency [15]. However, it is unclear whether the ACL reconstruction itself affects the increase of %MML, or whether the concurrent all-inside meniscal suture with ACL reconstruction excessively elongates the MML. We hypothesized that ACL reconstruction affects the length and width of the medial meniscus in ACL-injured knees. The aim of this study was to investigate the preoperative and postoperative position of the medial meniscus in patients who underwent only primary ACL reconstruction and compare these measurements with those in normal knees.
Methods
Between January 2009 and November 2012, 32 knees (25 %) of 29 patients among 128 knees of consecutive patients who underwent primary ACL reconstructions did not contain the tears of the medial and lateral menisci. A total of 28 knees (88 %) were observed on the pre-operative and postoperative MRI scans; four knees were excluded due to lack of appropriate MRI scans. The patients in the ACL-reconstructed group (men, 13; women, 13) had a mean age of 23 years (range, 15–38 years). The mean time from injury to pre-operative MRI was two weeks (range, one to four weeks). The mean time at which the ACL reconstruction was performed was three months after injury (range, one to ten months). Postoperative MRI was performed at a mean of 11 months (range, 11–12 months). The mean follow-up period was 26 months (range, 18–51 months). Twenty-six knees with a mean age of 23 years (range, 15–38 years) and with normal menisci observed on MRI scans were considered the normal group (men, 15; women 11); the MRI scans of these knees were compared with those of the ACL-reconstructed knees. Medical records were reviewed retrospectively to examine the age, sex, height, body weight, Lysholm score [16], radiographic findings, and MRI findings. A side-to-side distance in the KT-2000 arthrometer measurement at 134 N was adopted as a parameter in the anteroposterior stability assessment at the time of surgery and final follow-up examination (HI and SM). This study received the approval of our Institutional Review Board and patients gave their informed consent for this research. Patient demographics are shown in Table 1.
Surgical procedure and postoperative care
Routine arthroscopic evaluation was performed before each ACL reconstruction. No tears, instability, and degenerative changes in the menisci were observed in the ACL-reconstructed group. Small chondral injuries in three knees were untreated. ACL reconstruction was performed using a hamstring tendon autograft (semitendinosus and/or gracilis muscles, anatomic double-bundle reconstruction). Femoral and tibial bone tunnels were created within the ACL footprints as described [17, 18]. Graft fixation on the femoral side was achieved using an Endobutton CL (Smith & Nephew, Andover, MA, USA). Graft fixation on the tibial side was performed using a Double Spike Plate and a screw (Meira, Aichi, Japan). An initial force of 30 N for the anteromedial bundle (20 N for the posterolateral bundle) was applied to the graft at 10° of knee flexion. Postoperative rehabilitation protocols were similar in all patients. All patients began knee motion exercises and partial weight-bearing at two weeks postoperation. Full weight-bearing was allowed at one month and running was allowed at five months post-operation. Return to competitive sports was allowed at eight months [17].
Measurement of bony landmarks and the medial meniscus
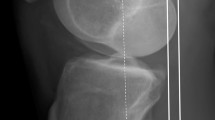
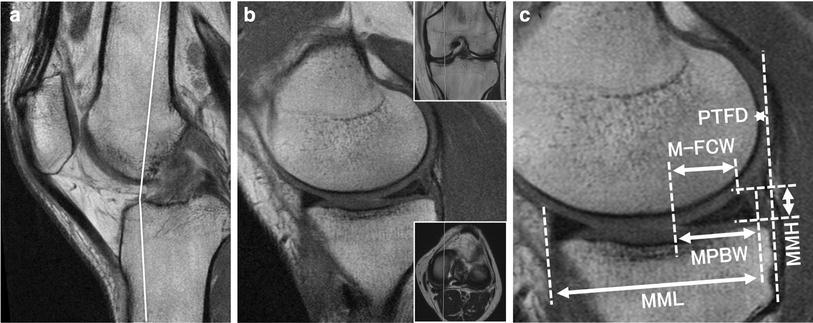
Measurements of the radiographic images and MRI scans were performed as described previously [15]. MTPL was measured from the maximum anteroposterior dimension of the medial plateau in the lateral radiographic view (Fig. 1a) [19, 20]. An anteroposterior radiograph was used to measure the medial tibial plateau width (MTPW). MTPW was measured as the distance from the medial margin of the tibial plateau to the peak of the medial intercondylar eminence (Fig. 1b) [19, 20]. MRI was performed using an Achieva 1.5 T (Philips, Amsterdam, The Netherlands) or an EXCELART Vantage powered by Atlas 1.5 T (Toshiba Medical Systems, Tochigi, Japan) with a coil under the 10°-flexed knee position. Standard sequences of the Achieva included sagittal (repetition time [TR]/echo time [TE], 601/14), coronal (TR/TE, 553/14) T2-weighted multi echo with a 30° flip angle, and axial (TR/TE, 4330/104) T2 BLADE fat saturation with a 150° flip angle. Standard sequences of the Vantage included sagittal and coronal proton-density fast spin echo (TR/TE, 2300/18) and axial T2-weighted fat suppression (TR/TE, 3500/60) with a 90° flip angle. The slice thickness was 3 mm with a 0.6-mm gap. The field of view was 18 cm (or 17 cm) with an acquisition matrix size of 384 × 269 (or 200 × 368) [21–23]. Four orthopaedic surgeons (SN, TT, YS, and KS) retrospectively reviewed the radiographic images and MRI scans in a blinded manner. The MML and medial meniscal width (MMW) were measured in the transverse, sagittal, and coronal views using the MRI-based multi-slice assessment technique [15]. The distance from the anterior to the posterior margin of the medial meniscus on the transverse image was the MML (Fig. 1c). MMW was measured as the distance from the outer border of the medial meniscus to the medial edge of the medial intercondylar eminence on the coronal image that crossed the center of the MML (Fig. 1d). Medial meniscal extrusion (MME) was measured as the distance from the medial edge of the tibial plateau cartilage to the outer border of the medial meniscus (Fig. 1e). Both intra- and interobserver reliabilities were excellent (ICC > 0.92) in each measurement. A mean value of each observer’s measurement was obtained. To compare the MML and MMW among the different groups, we normalized the MRI-based meniscal measurements using radiographic measurements of the medial tibial plateau. The percentage of MML to each MTPL was calculated as the MML percentage (%MML = 100 MML/MTPL). The percentage of MMW to each MTPW was determined as the MMW percentage (%MMW = 100 MMW/MTPW) [15]. Correlations between MTPL and MML as well as that between MTPW and MMW were examined. The MML, %MML, MMW, %MMW, and MME were compared among the ACL-deficient (pre-operative), ACL-reconstructed (postoperative), and normal knees.
Radiographic and MRI-based measurements. a Medial tibial plateau length (MTPL). b Medial tibial plateau width (MTPW). Coronal reference lines (red) are parallel to the posterior condylar line. c Medial meniscal length (MML, yellow double-headed arrow). d Medial meniscal width (MMW). e Medial meniscal extrusion (MME)
Statistical analysis
Linear regression analysis was used to assess the correlations among the indicated values. A good correlation was represented by R² ≥ 0.65, fair correlation by R² ≥ 0.50, and poor correlation by R² < 0.50 [15]. Meniscal measurements and clinical values at the pre-operative and postoperative examinations were assessed using the Wilcoxon signed-rank test. The Mann–Whitney U test was used to study the variables compared with normal knees. Power and statistical analyses were performed using EZR-WIN. Data are presented as the mean ± standard deviation. Significance was set at P < 0.05.
Results
Correlation between MRI-based measurement of the medial meniscus and radiographic measurement of the medial tibial plateau
Good correlations were observed between (i) MTPL and pre-operative MML (R² = 0.77), (ii) MTPL and postoperative MML (R² = 0.67), and (iii) MTPL and normal MML (R² = 0.76). Fair correlations were observed between (i) MTPW and pre-operative MMW (R² = 0.61) and (ii) MTPW and postoperative MMW (R² = 0.60). A good correlation was also observed between MTPW and normal MMW (R² = 0.83). The best fit equations for predicting each value were as follows: (i) pre-operative MML = 1.02 MTPL – 4.70 mm; (ii) postoperative MML = 0.94 MTPL – 0.25 mm; (iii) normal MML = 0.79 MTPL + 6.65 mm; (iv) preoperative MMW = 0.66 MTPW + 7.07 mm; (v) postoperative MMW = 0.82 MTPW + 2.75 mm; and (vi) normal MMW = 0.88 MTPW + 0.81 mm.
Physical features and radiographic measurement of the medial tibial plateau
The height of the patients was similar between the ACL-reconstructed (1.68 ± 0.07 m) and normal (1.65 ± 0.08 m) groups. Body weight of the patients was 65.7 ± 7.7 kg and 64.8 ± 12.5 kg in the ACL-reconstructed and normal groups, respectively (Table 2). The radiograph-based MTPL was 46.2 ± 2.9 mm and 45.3 ± 2.8 mm in the ACL-reconstructed and normal groups, respectively. The MTPW was also similar between the ACL-reconstructed (31.5 ± 2.3 mm) and normal (30.6 ± 2.1 mm) groups (Table 2). There were no significant differences between the two groups considering the height, body weight, and medial tibial plateau measurement (Table 2).
Clinical evaluation
ACL reconstruction improved knee-associated symptoms. No physical signs such as knee-joint swelling, joint-line tenderness, or locking were observed at the time of final follow-up evaluation. Median Lysholm score was 62.5 (range, 36–73) before ACL reconstruction and improved to 95.5 (range, 80–100) at the final follow-up examination. Mean side-to-side distance in the KT-2000 measurement was 5.3 ± 1.8 mm (range, 2–9 mm) before ACL reconstruction and decreased to 1.3 ± 1.1 mm (range, 0–3 mm) at the final follow-up examination. Significant differences between preoperative and postoperative values were observed in these items (P < 0.001).
MRI-based measurement of the medial meniscus
The MML increased from 42.6 ± 3.5 to 43.8 ± 3.5 mm after ACL reconstruction (P < 0.001, Table 3). %MML significantly increased from 92.1 ± 4.3 to 94.6 ± 4.3 % postoperatively (P < 0.001). The MME changed from 1.2 ± 1.1 to 1.8 ± 0.9 mm (P = 0.007). All parameters were similar between the pre-operative ACL-deficient and normal groups (Table 3). On the other hand, significant differences between the postoperative and normal groups were observed in the MML (P = 0.018), %MML (P = 0.030), and MME (P = 0.021). Effective statistical power (>0.08) was obtained in each parameter showing significant difference.
Discussion
The present study demonstrated that MML and %MML, which showed anteroposterior expansion of the individual medial meniscus on each medial tibial plateau, changed after ACL reconstruction. ACL reconstruction also affected an extra-articular radial displacement (extrusion) of the medial meniscus. Many studies have reported that MME is associated with progression of symptomatic knee osteoarthritis [24–26]. Meniscus-to-femoral condyle congruity is essential for the development of circumferential hoop stresses and meniscal function. Abnormalities in the position of the medial meniscus and its coverage, such as meniscal root tear, substantial meniscal extrusion, and meniscectomy-related meniscal defects, can alter knee joint congruity and are associated with the progression of tibiofemoral osteoarthritis and cartilage degradation [24, 27, 28]. Accurate positioning of the meniscus is critical in meniscal repair and replacement for restoring the physiological relationships among the femur, meniscus, and tibia [29]. The ACL also resists valgus knee joint laxity [30] by preventing internal rotation of the tibia [31]. Although several authors have stated that prompt operative intervention reduces long-term osteoarthritis after ACL injury [32], the theory that ACL reconstruction is valuable as a way to prevent knee joint degradation remains controversial [8]. The tibia is over-constrained (posterior displacement and external rotation) three weeks after anatomic triple-bundle ACL reconstruction, but returns to the normal position six months postoperatively [33]. We consider that ACL reconstruction itself may not directly affect the MRI-based measurements of the medial meniscus. Other factors such as graft tensioning and tibiofemoral rotational mismatch might have influenced the medial meniscal status. Postoperative changes in MML and MME may be caused by an excessive external rotation of the tibia. In our study, a total of 50 N of initial tension was applied for the graft fixation. Graft tensioning may also affect postoperative change in the MML and MME. There was no significant correlation between the pre-operative interval and each meniscal measurement (data not shown). In addition, the pre-operative and postoperative KT-2000 measurements had no correlation with the medial meniscal measurements (data not shown). ACL deficiency that had no meniscal injuries may not directly affect the measurements of the medial meniscus under the 10°-flexed and unloaded knee position during a short-term preoperative interval. Concurrent and post traumatic meniscal damage involved in the root tears and severe radial tears might affect the transposition of the meniscus in the ACL-deficient knees. A follow-up study and further MRI examinations will be needed to understand the relationship among pre-operative and postoperative shift of the medial meniscus, the tibiofemoral rotation, and the development of post-traumatic osteoarthritis in the ACL-reconstructed knees.
In this study, the measurement of the medial meniscus in the pre-operative ACL-deficient and normal groups was similar to those in earlier reports [13, 14, 19, 20]. Several variables such as height of the patient and measurements of the tibial plateau are considered good candidates for determining the medial meniscal size [13, 15]. In these studies, the tibial plateau measurements were more closely correlated with the MRI-based measurements of the medial meniscus than each patient’s height [13, 15]. However, the actual meniscal dimensions (MML and MMW) can be predicted with a mean error of 5.0 ± 6.4 % using the measurements of the tibial plateau (MTPL and MTPW) [20]. In addition, the measurements for left and right knees in the same patient show that the mean percentage difference for the meniscal dimensions (length, width, body width, and circumference) was 4.5–9.5 % [20]. In our study, height was poorly correlated with the MRI-based measurements of the medial meniscus than the measurements of the tibial plateau of all groups (data not shown). Therefore, we normalized the MRI-based meniscal measurement using the radiographic measurements of the medial tibial plateau, as %MML and %MMW, to precisely compare the medial meniscal measurements. This study demonstrated that MME increased after ACL reconstruction. However, significant differences in MMW and %MMW were not observed. The MMW may not be predicted accurately from height, skeletal size, and contralateral meniscal measurements. We consider that the MME would be more useful to assess the mediolateral change in the MRI-based meniscal measurements than the MMW.
The risk of further meniscal injuries after ACL rupture is higher when the ACL is not reconstructed [34]. A reduced frequency of further meniscal damage after ACL reconstruction has also been stated in several studies [8, 9]. However, these observations in the prevention of postoperative meniscal injuries could not be explained only by ACL reconstruction but could also be a result of decreased involvement in strenuous sporting activities. Stable medial meniscal tears left in situ during ACL reconstructions result in the high prevalence of failures such as residual pain and subsequent meniscus repair (or partial meniscectomy) [35]. Moreover, the conservative treatment of peripheral stable meniscal tears in ACL-reconstructed knees is less effective for the medial meniscus than for the lateral meniscus [36]. Therefore, ACL reconstruction alone might not perfectly resolve complex mechanical stresses in the medial meniscus. Further investigations will be required to evaluate the effect of ACL reconstruction on restoring medial meniscal function.
In this study, we evaluated the MRI-based medial meniscal length, width, and extrusion in a single knee flexion angle (10°) under non-weight-bearing condition using 3-mm slice thickness. To compare the real function of the medial meniscus among the ACL-deficient, ACL-reconstructed, and normal groups, open MRI assessments of meniscal movement using thin slices in several knee flexion angles under loading condition will be required. In addition, three-dimensional reconstruction of the medial meniscus using dynamic MRI may be useful to understand postoperative change in medial meniscal position and morphology. Our study was a retrospective comparative study with a small sample size. Additional follow-up MRI scans involved in a larger sample size will be required to evaluate the real effect of ACL reconstruction on medial meniscal position.
In conclusion, postoperative changes in the anteroposterior length and radial extrusion of the medial meniscus (MML, %MML, and MME) were observed after ACL reconstruction. Although ACL reconstruction itself may not directly induce a distinct damage of the meniscus, the posttraumatic transposition and degeneration of the medial meniscus may not be completely prevented by ACL reconstruction alone.
References
Levy IM, Torzilli PA, Warren RF (1982) The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am 64:883–888
Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL (2000) Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res 18:109–115
Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH (2001) The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med 29:226–231
Seon JK, Gadikota HR, Kozanek M, Oh LS, Gill TJ, Li G (2009) The effect of anterior cruciate ligament reconstruction on kinematics of the knee with combined anterior cruciate ligament injury and subtotal medial meniscectomy: an in vitro robotic investigation. Arthroscopy 25:123–130
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38:1591–1597
Bylski-Austrow DI, Ciarelli MJ, Kayner DC, Matthews LS, Goldstein SA (1994) Displacements of the menisci under joint load: an in vitro study in human knees. J Biomech 27:421–431
Kluczynski MA, Marzo JM, Bisson LJ (2013) Factors associated with meniscal tears and chondral lesions in patients undergoing anterior cruciate ligament reconstruction: a prospective study. Am J Sports Med 41:2759–2765
Delincé P, Ghafil D (2012) Anterior cruciate ligament tears: conservative or surgical treatment? A critical review of the literature. Knee Surg Sports Traumatol Arthrosc 20:48–61
Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C (2008) Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med 36:1275–1282
Leroux T, Ogilvie-Harris D, Dwyer T, Chahal J, Gandhi R, Mahomed N, Wasserstein D (2014) The risk of knee arthroplasty following cruciate ligament reconstruction: a population-based matched cohort study. J Bone Joint Surg Am 96:2–10
Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM (1999) Meniscal movement. An in-vivo study using dynamic MRI. J Bone Joint Surg Br 81:37–41
Bloecker K, Guermazi A, Wirth W, Benichou O, Kwoh CK, Hunter DJ, Englund M, Resch H (2013) Eckstein F; OAI investigators. Tibial coverage, meniscus position, size and damage in knees discordant for joint space narrowing–data from the Osteoarthritis Initiative. Osteoarthritis Cartilage 21:419–427
Stone KR, Freyer A, Turek T, Walgenbach AW, Wadhwa S, Crues J (2007) Meniscal sizing based on gender, height, and weight. Arthroscopy 23:503–508
Haut TL, Hull ML, Howell SM (2000) Use of roentgenography and magnetic resonance imaging to predict meniscal geometry determined with a three-dimensional coordinate digitizing system. J Orthop Res 18:228–237
Furumatsu T, Miyazawa S, Tanaka T, Okada Y, Fujii M, Ozaki T (2014) Postoperative change in medial meniscal length in concurrent all-inside meniscus repair with anterior cruciate ligament reconstruction. Int Orthop 38:1393–1399
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154
Fujii M, Furumatsu T, Miyazawa S, Okada Y, Tanaka T, Ozaki T, Abe N (2014) Intercondylar notch size influences cyclops formation after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014 Feb 19. [Epub ahead of print]
Furumatsu T, Fujii M, Tanaka T, Miyazawa S, Ozaki T. The figure-of-nine leg position for anatomic anterior cruciate ligament reconstruction. Orthop Traumatol Surg Res [in press]
Shaffer B, Kennedy S, Klimkiewicz J, Yao L (2000) Preoperative sizing of meniscal allografts in meniscus transplantation. Am J Sports Med 28:524–533
McDermott ID, Sharifi F, Bull AM, Gupte CM, Thomas RW, Amis AA (2004) An anatomical study of meniscal allograft sizing. Knee Surg Sports Traumatol Arthrosc 12:130–135
Ikuma H, Abe N, Uchida Y, Furumatsu T, Fujiwara K, Nishida K, Ozaki T (2008) Novel magnetic resonance imaging evaluation for valgus instability of the knee caused by medial collateral ligament injury. Acta Med Okayama 62:185–191
Sakata K, Furumatsu T, Abe N, Miyazawa S, Sakoma Y, Ozaki T (2013) Histological analysis of failed cartilage repair after marrow stimulation for the treatment of large cartilage defect in medial compartmental osteoarthritis of the knee. Acta Med Okayama 67:65–74
Sakata K, Furumatsu T, Miyazawa S, Okada Y, Fujii M, Ozaki T (2013) Comparison between normal and loose fragment chondrocytes in proliferation and redifferentiation potential. Int Orthop 37:159–165
Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonté F, Beaudoin G, Bloch DA, Choquette D, Haraoui B, Altman RD, Hochberg M, Meyer JM, Cline GA, Pelletier JP (2005) Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis 64:556–563
Lee DH, Lee BS, Kim JM, Yang KS, Cha EJ, Park JH, Bin SI (2011) Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 19:222–229
Wenger A, Englund M, Wirth W, Hudelmaier M, Kwoh K, Eckstein F; OAI Investigators (2012) Relationship of 3D meniscal morphology and position with knee pain in subjects with knee osteoarthritis: a pilot study. Eur Radiol 22:211–220
Petersen W, Forkel P, Feucht MJ, Zantop T, Imhoff AB, Brucker PU (2014) Posterior root tear of the medial and lateral meniscus. Arch Orthop Trauma Surg 134:237–255
Mills PM, Wang Y, Cicuttini FM, Stoffel K, Stachowiak GW, Podsiadlo P, Lloyd DG (2008) Tibio-femoral cartilage defects 3–5 years following arthroscopic partial medial meniscectomy. Osteoarthritis Cartilage 16:1526–1531
Vrancken AC, Buma P, van Tienen TG (2013) Synthetic meniscus replacement: a review. Int Orthop 37:291–299
Inoue M, McGurk-Burleson E, Hollis JM, Woo SL (1987) Treatment of the medial collateral ligament injury. I: The importance of anterior cruciate ligament on the varus-valgus knee laxity. Am J Sports Med 15:15–21
Matsumoto H, Suda Y, Otani T, Niki Y, Seedhom BB, Fujikawa K (2001) Roles of the anterior cruciate ligament and the medial collateral ligament in preventing valgus instability. J Orthop Sci 6:28–32
Richmond JC, Lubowitz JH, Poehling GG (2011) Prompt operative intervention reduces long-term osteoarthritis after knee anterior cruciate ligament tear. Arthroscopy 27:149–152
Matsuo T, Mae T, Shino K, Kita K, Tachibana Y, Sugamoto K, Yoshikawa H, Nakata K (2014) Tibiofemoral relationship following anatomic triple-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 22:2128–2135
Dunn WR, Lyman S, Lincoln AE, Amoroso PJ, Wickiewicz T, Marx RG (2004) The effect of anterior cruciate ligament reconstruction on the risk of knee reinjury. Am J Sports Med 32:1906–1914
Magnussen RA, Mansour AA, Carey JL, Spindler KP (2009) Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg 22:347–357
Pujol N, Beaufils P (2009) Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc 17:396–401
Acknowledgments
We are grateful to Prof. Nobuhiro Abe (Kawasaki Medical School, Okayama, Japan) for his support. This work was supported by Grants from the Japan Society for the Promotion of Science (No. 24791546).
Conflict of interest
The authors have no conflicts of interest concerning this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Narazaki, S., Furumatsu, T., Tanaka, T. et al. Postoperative change in the length and extrusion of the medial meniscus after anterior cruciate ligament reconstruction. International Orthopaedics (SICOT) 39, 2481–2487 (2015). https://doi.org/10.1007/s00264-015-2704-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2704-z