Abstract
Purpose
Meniscus repair can restore meniscal function that transfers the axial compressive force to circumferential tensile strain. However, few reports have investigated the relationship between concurrent meniscus repair with acute anterior cruciate ligament (ACL) reconstruction and postoperative meniscal position. This study aimed to evaluate medial meniscal size and clinical results in patients who underwent ACL reconstruction and concomitant all-inside medial meniscus repair.
Methods
Twenty patients underwent ACL reconstruction and concurrent medial meniscus repair of a peripheral longitudinal tear using the FasT-Fix meniscal repair device. Medial tibial plateau length (MTPL) and width (MTPW) were determined by radiographic images. We evaluated the Lysholm score, anteroposterior instability, meniscal healing and magnetic resonance imaging (MRI)-based medial meniscal length (MML) and width (MMW). Correlations between MRI-based meniscal size, radiographic measurement and height were investigated.
Results
All patients showed complete healing of the repaired meniscus in arthroscopic evaluation. However, one patient needed a subsequent meniscus repair during the follow-up period. Lysholm score and anteroposterior instability improved significantly. A better correlation was observed between MMW and MTPW than between MML and MTPL. Concurrent all-inside medial meniscus repair with ACL reconstruction significantly increased MML percentage (%MML) (100 MML/MTPL) but did not affect MMW percentage (%MMW) (100 MMW/MTPW).
Conclusions
Concurrent all-inside medial meniscus repair with ACL reconstruction had satisfactory clinical results. %MML was increased by concurrent medial meniscus repair without affecting %MMW. Our results suggest that medial meniscus repair associated with ACL reconstruction may restore meniscal function by adjusting the anteroposterior length of the torn medial meniscus.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Meniscal sizing is important in evaluating meniscal damage, extrusion, movement and tibial plateau coverage by the meniscus [1, 2]. Pre-operative size matching of the meniscus is also critical for successful meniscal allograft transplantation [3]. Meniscal sizing is currently determined by measuring a combination of outer meniscal margins obtained by magnetic resonance imaging (MRI) and radiographic bony landmarks [4]. However, the literature includes reports on sizing inaccuracy resulting from difficulty in differentiating meniscal margins, radiographic errors in magnification and incorrect identification of bony landmarks [4, 5]. Furthermore, the transverse, sagittal and coronal planes of the knee on MRI often vary with each patient and MRI scan. No standard protocol has been established for comparing pre-operative and postoperative meniscal sizes in the same patient. Therefore, we invented a simple MRI-based meniscal sizing technique without using an additional image analysis workstation.
Peripheral longitudinal tears of the medial meniscus are commonly seen with acute anterior cruciate ligament (ACL) injuries. This type of tear is asymptomatic, and many of these tears could heal on their own without repair [6]. However, the conservative treatment of peripheral stable meniscus tears is less effective for the medial than for the lateral meniscus [7]. Several authors report that repair of peripheral medial meniscus tears decreases the risk of postoperative knee pain and subsequent arthroscopic salvation in ACL-reconstructed knees [7, 8]. In addition, medial meniscus tears are often associated with chronic ACL insufficiency and can be degenerative or nondegenerative, depending on the severity of instability. Typical tears in the posterior third of the medial meniscus can extend with additional giving-way episodes and eventually become “bucket-handle” tears [9, 10]. Based on these reports, we performed concurrent meniscus repair with ACL reconstruction to achieve complete healing of stable longitudinal tears of the medial meniscus. However, MRI examination and clinical assessment are not reliable to determine meniscal healing, and second-look arthroscopy is the most dependable method [11]. Thus, we arthroscopically evaluated the healing status of the repaired medial meniscus in ACL-reconstructed knees.
Repaired or healed meniscus can restore meniscus-to-femoral condyle congruity and its biomechanical function that transfers the axial compressive force to the circumferential tensile strain in the knee joint. However, few studies have investigated the relationship between concurrent meniscus repair with ACL reconstruction and postoperative meniscal position. All-inside repair for lateral meniscus root tear improves posterior meniscal extrusion on the MRI sagittal plane but does not significantly reduce radial meniscal displacement on the coronal plane in ACL-reconstructed knees [12]. We hypothesised that sutured repair of the longitudinal medial meniscus tear on the posterior segment might affect medial meniscal length (MML) and width (MMW). In this study, we investigated pre-operative and postoperative MRI-based medial meniscal size in patients who underwent ACL reconstruction and concomitant medial meniscus repair.
Methods
Between July 2009 and December 2011, 23 knees in 23 patients (24 %) among 97 consecutive ACL reconstructions had a concomitant medial meniscus repair of a peripheral longitudinal tear in the posterior segment. Of those patients, 20 (87 %) underwent second-look arthroscopic evaluation of the repaired menisci and were followed up for a mean of 24 (range, 12–41) months. Second-look arthroscopy was performed postoperatively at a mean of 14 (range, six to 26) months. In all patients, MRI scans were examined before primary surgery and second-look arthroscopy. Medical records were reviewed retrospectively to examine age, sex, height, body weight, clinical findings, Lysholm score [13] and MR images. A side-to-side distance in the KT-2000 arthrometer measurement at 134 N was adopted as a parameter in the anteroposterior (AP) stability assessment. This study received the approval of our Institutional Review Board, and patients gave their informed consent for this research; eight patients were men and 12 were women, with a mean age of 19 (range, 15–38) years. All injuries were sustained during sports activities. Mean timing of ACL reconstruction was six (range, one to 36) months after injury. Patient demographics are shown in Table 1.
Surgical procedure, postoperative care and second-look arthroscopy
Peripheral longitudinal tears of the medial meniscus included partial- or full-thickness, simple longitudinal tears ≥1 cm in length located in the outer one third of the posterior segment. Medial meniscus longitudinal tear was measured by an arthroscopic probing, and mean tear length was 1.4 (range, 1.0–2.5) cm. Minor degenerative changes of the medial meniscus posterior segments were observed in five patients. Medial meniscus repairs were performed using the FasT-Fix or Ultra-FasT-Fix all-inside meniscal repair system (Smith & Nephew, Andover, MA, USA). Vertical sutures were placed across the tear of the medial meniscus (mean, 1.9; range, 1–4). Lateral meniscus tears were observed in eight knees [40 %: partial meniscectomy, two; meniscus repair by the FasT-Fix alone, four; inside-out repair with no. 2–0 Wayolax (Matsuda Medical Instrument, Tokyo, Japan) alone, one; repair with the FasT-Fix and Wayolax, one], as shown in Table 1. Small chondral injuries were not treated. ACL reconstruction was performed with either a hamstring tendon autograft [semitendinosus and gracilis muscle (STG), two bundles, 18 knees] or a bone-patellar tendon-bone autograft (BTB: single bundle, two knees). In cases in which STG autografts were used, fixation was achieved using an Endobutton or an Endobutton CL (Smith & Nephew) on the femoral side. BTB grafts were fixed by an Endobutton on the femoral side. Graft fixation on the tibial side was performed using a Double Spike Plate and a screw (Meria, Aichi, Japan). Postoperative rehabilitation protocols were similar in all patients. All patients began knee-motion exercise and partial weight bearing at two weeks postoperatively. Full weight bearing was allowed at one month, and running was allowed after five months. Return to competitive sports was allowed at eight months. Meniscal healing status was assessed by second-look arthroscopy and was performed in patients who wanted plates and screws removed. Plates, screw heads and knots sometimes induced pain in the lower leg in a specific sitting position with maximal knee flexion on a floor. In our hospital, patients who underwent ACL reconstruction usually wished to have these implants removed rather that recommendation by us. The repaired meniscus was confirmed as completely healed if all of the following criteria were met: (1) smooth surface of previously repaired sites on the tibial and femoral sides determined by overall observation; (2) no cleft detected at the repaired sites by probing; (3) good stability for the repaired sites determined by pulling with a probe [11]. Otherwise, we diagnosed the repaired meniscus as incompletely healed or unhealed.
Measurement of bony landmarks and medial meniscal sizes
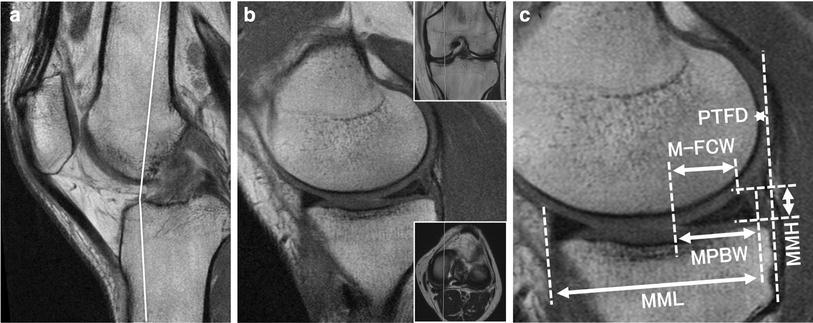
Medial tibial plateau length (MTPL) was measured from the maximum AP dimension of the medial plateau in a radiographic lateral view [14, 15]. Anteroposterior radiography was used to measure medial tibial plateau width (MTPW) by obtaining the distance from the medial margin of the tibial plateau to the peak of the medial intercondylar eminence [14, 15]. Imaging evaluation was performed using an Achieva 1.5 T (Philips, Amsterdam, The Netherlands) or an EXCELART Vantage Powered by Atlas 1.5 T (Toshiba Medical Systems, Tochigi, Japan) with a coil. Mean time from injury to pre-operative MRI was three (range, one to 12) weeks, and mean time from meniscal repair to postoperative MRI was six (range, one to 12) months. Standard sequences of the Achieva included sagittal [repetition time (TR)/echo time (TE) 742/18], coronal (TR/TE 637/18) and axial (TR/TE 499/18) T2-weighted fast-field echo with a 20° flip angle (FA). Standard sequences of the Vantage included sagittal and coronal proton-density fast-spin-echo (TR/TE 2,300/18), and axial T2-weighted fat suppression (TR/TE 3,500/60) with a 90° FA. Slice thickness was 3 mm with a 0.6-mm gap. Field of view (FOV) was 16 (or 17) cm with an acquisition matrix size of 205 × 256 (or 200 × 368) [16–18]. Two orthopaedic surgeons performed the MRI evaluation, and all images were reviewed retrospectively. Measurements of medial meniscal sizes (MML and MMW) were performed using a simple MRI-based meniscal sizing technique in transverse, sagittal and coronal views. Details of meniscal sizing are shown in Fig. 1. In brief, a reference (Ref) line was created vertical to the posterior condylar line on the transverse image with the medial meniscus. AP edges of the medial meniscus were determined by the Ref line and sagittal and coronal views on the transverse image. Distance from the anterior to the posterior point on the Ref line was measured as MML (Fig. 1). MMW, from the outer border of the medial meniscus to the medial edge of the medial intercondylar eminence, was measured parallel to the articular surface of the tibia on the coronal image that crossed the center of the MML. The percentage of the MML to each MTPL was calculated as %MML and %MMW was determined by the percentage of the MMW to each MTPW. The following correlations were examined:
-
(i)
Height and MTPL
-
(ii)
Height and pre-operative MML
-
(iii)
Height and postoperative MML
-
(iv)
Pre-operative MML and MTPL
-
(v)
Postoperative MML and MTPL
-
(vi)
Height and MTPW
-
(vii)
Height and pre-operative MMW
-
(viii)
Height and postoperative MMW
-
(ix)
Pre-operative MMW and MTPW
-
(x)
Postoperative MMW and MTPW
Pre-operative and postoperative MML and MMW were compared. In addition, preoperative and postoperative %MML and %MMW were compared.
Magnetic resonance image (MRI) showing transverse, sagittal, and coronal views from which medial meniscal length (MML) was measured. a A posterior condylar (PC) line was drawn intersecting the most posterior edge of the femoral condyles on the transverse image. b A reference (Ref) line (white dotted line) was created vertical to the PC line at the centre of the medial meniscal width (MMW) on the transverse image with the medial meniscus. The anterior edge of the medial meniscus was determined by the Ref line and c sagittal and d coronal views on the transverse image. An appropriate anterior margin of the medial meniscus was fixed on the Ref line according to the nearest point created by sagittal–coronal crossing lines. The posterior edge of the medial meniscus was similarly determined on the Ref line by the e sagittal and f coronal images. The distance from the anterior to the posterior point (double-headed arrow) was measured on the Ref line and used as MML. Note that, as usual, the sagittal and coronal planes are not completely parallel to the Ref and PC lines, respectively
Statistical analysis
Linear regression analysis was used to assess correlations among indicated values. A good correlation is represented by R 2 ≥ 0.65, fair correlation by R 2 ≥ 0.50, and poor correlation by R 2 ≤ 0.50. The Mann–Whitney U test was used to study the effects of variables with two categories. Data are presented as the mean ± standard deviation (SD). Significance was set at P < 0.05.
Results
Clinical and second-look arthroscopic evaluations
All 20 patients showed complete healing of the medial meniscus tear in the second-look arthroscopic evaluation. No physical signs such as knee-joint swelling, joint-line tenderness, locking or a positive McMurray test result were observed at the time of second-look arthroscopy [19]. However, one patient (5 %) had a clinical symptom of meniscus tear at 27 postoperative months. This patient had a minor degenerative change in the posterior segment of the medial meniscus at the time of ACL reconstruction. In the primary surgery, two vertical sutures were placed across a peripheral longitudinal tear (1.5 cm) with the FasT-Fix. The repaired medial meniscus had good stability on probing. Complete healing of the repaired meniscus was observed by a second-look arthroscopy at 13 months. Satisfactory clinical outcomes were obtained at 24 postoperative months. Lysholm score improved from 58 to 90. A difference in the KT-2000 measurement improved from 5 to 1 mm. A subsequent medial meniscus repair was performed using the FasT-Fix 360 (Smith & Nephew) at 30 months. Mean Lysholm score was 60.1 ± 4.7 (range, 52–68) before ACL reconstruction, and improved to 93.1 ± 3.1 (range, 88–98) at the final follow-up examination (Table 2). Mean side-to-side distance in the KT-2000 measurement was 6.1 ± 2.2 (range, 3–9) mm before ACL reconstruction and decreased to 1.2 ± 0.7 (range, 0–2) mm at the final follow-up examination (Table 2). Significant differences between pre-operative and postoperative values were observed in these items (P < 0.001, Table 2).
Correlations between the MRI-based medial meniscal size, radiographic measurement, and height
Good correlation between MTPL and height (R 2 = 0.740), poor correlation between preoperative MML and height (R 2 = 0.429) and poor correlation between postoperative MML and height (R 2 = 0.295) were found. However, good correlation was observed between pre-operative MML and MTPL (R 2 = 0.743); fair correlation was found between postoperative MML and MTPL (R 2 = 0.620). Best-fit equations for predicting each value were as follows:
-
(i)
MTPL = 38.48 height (m) − 16.95 mm
-
(ii)
Pre-operative MML = 20.44 height (m) + 8.30 mm
-
(iii)
Postoperative MML = 16.92 height (m) + 15.71 mm
-
(iv)
Pre-operative MML = 0.60 MTPL + 13.99 mm
-
(v)
Postoperative MML = 0.55 MTPL + 18.03 mm
Radiographic MTPL was more useful for predicting the MRI-based measurement of MML than the height of each patient. Meanwhile, good correlation between MTPW and height (R 2 = 0.663), poor correlation between pre-operative MMW and height (R 2 = 0.477) and good correlation between postoperative MMW and height (R 2 = 0.668) were found. In addition, good correlation was observed between pre-operative (R 2 = 0.805) and postoperative (R 2 = 0.821) MMW and MTPW. The best-fit equations for predicting each value were as follows:
-
(i)
MTPW = 30.97 height (m) − 20.62 mm
-
(ii)
Pre-operative MMW = 22.03 height (m) − 8.83 mm
-
(iii)
Postoperative MMW = 20.99 height (m) − 7.13 mm
-
(iv)
Pre-operative MMW = 0.752 MTPW + 4.57 mm
-
(v)
Postoperative MMW = 0.61 MTPW + 8.88 mm
Postoperative change in MRI-based measurement of the medial meniscus
Concurrent medial meniscus repair with ACL reconstruction slightly increased MML from 42.2 ± 2.8 to 43.6 ± 2.8 mm, but no significant difference between pre-operative and postoperative MML was noted (P = 0.072, Table 3). However, postoperative %MML (100 MML/MTPL) was significantly increased from 89.8 ± 3.7 to 92.8 ± 4.3 % by concurrent all-inside medial meniscus repair (P = 0.014, Table 3). Meanwhile, MMW and %MMW were not affected by medial meniscus repair associated with ACL reconstruction (P = 0.489 and 0.476, respectively; Table 3).
Discussion
Stable peripheral longitudinal meniscal tears with acute ACL injury can heal without tear extension in 58–69 % cases [6, 20]. However, in a systematic literature review, stable medial meniscal tears left in situ during ACL reconstructions result in the high prevalence of failures, such as residual pain and subsequent meniscus repair (or partial meniscectomy) [21]. In our study, FasT-Fix all-inside meniscus repairs showed complete healing of simple longitudinal medial meniscus tears on second-look arthroscopic evaluation in 100 % of cases. However, during the follow-up period, one patient (5 %) underwent a subsequent medial meniscus repair at 30 postoperative months. DeHaan et al. [22] report that FasT-Fix all-inside repair of unstable longitudinal medial meniscus tear showed a high failure rate (22 %) at a mean of three postoperative years, especially repairs for tears in the red–white zone of the meniscus (80 %). Taken together, a repaired meniscus may be inferior in holding various mechanical stresses in the mid to long term. Although second-look arthroscopy is the most dependable method to determine meniscal healing [11], abnormal hypersignals are present on MRI examination ten years after meniscus repair using FasT-Fix devices [23]. A follow-up study is required to determine the long-term healing status of repaired medial meniscus in ACL-reconstructed knees.
Meniscus-to-femoral condyle congruity is essential for the development of circumferential hoop stresses and meniscus function. To restore the physiological relationship between femur, meniscus and tibia, accurate positioning of the meniscus based on precise meniscal sizing is critical in meniscus repair and replacement [24]. Several variables, such as patient height and weight and radiographic measurements of the medial tibial plateau are considered good candidates for determining medial meniscal size [25]. Height has linear relationships with MRI-based measurement of MML (R 2 = 0.526) and MMW (R 2 = 0.651) [4]. Using measurements of MTPL and MTPW, actual meniscal dimensions (MML and MMW) can be predicted with a mean error of 5.0 ± 6.4 % [15]. Despite a fair correlation (R 2 = 0.544) between MMW and MTPW, a poor correlation (R 2 = 0.295) was observed in the relationship between MML and MTPL [15]. In our study, height had a poorer correlation with MML than with MMW preoperatively and postoperatively. These findings suggest that anteroposterior MML might be more varied than MMW. In addition, MML might not be predicted accurately from height, skeletal size and sex. Thus, we used %MML to evaluate the change in MML in concurrent medial meniscus repair with ACL reconstruction.
Our results demonstrate that postoperative MML slightly increased did not significantly change following concurrent meniscus repair with ACL reconstruction (Table 3). In addition, medial meniscus repair did not affect MMW and %MMW (Table 3). We consider that the FasT-Fix all-inside suturing device satisfactorily healed the peripheral longitudinal tear of the medial meniscus without inducing excessive posterior and radial shifts of the repaired medial meniscus. However, %MML was significantly increased by the all-inside medial meniscus repair concomitant with ACL reconstruction (Table 3). ACL insufficiency allows anterior translation of the tibia. Abnormal anterior tibial translation influences the anatomical relationship between the femoral condyle, meniscus and tibia [26]. Thus, an ACL-deficient knee may induce excessive posterior shift of the medial meniscus posterior segment via abnormal tibial anterior sliding. In our study, MML measured on preoperative MRI might already be elongated by the anterior tibial translation force. If so, an all-inside suturing device might excessively stabilize the posterior segment of the medial meniscus. We consider that concurrent repair of the medial meniscus tear on the posterior segment would restore medial meniscal position in ACL-reconstructed knees. However, difference in timing of postoperative MRI examination would affect the MRI-based measurement of MML and MMW. Further investigations are required to determine precise meniscal length, width and position in ACL-deficient knees that have no medial meniscus injury.
In conclusion, concurrent all-inside medial meniscus repair with ACL reconstruction resulted in complete healing of the meniscus at second-look arthroscopy and had satisfactory clinical evaluations; MRI-based MML was slightly increased, and postoperative %MML was significantly increased without affecting %MMW. Our results suggest that medial meniscus repair associated with ACL reconstruction may restore medial meniscus function by adjusting the position of the torn medial meniscus in ACL-deficient knees.
References
Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM (1999) Meniscal movement. An in-vivo study using dynamic MRI. J Bone Joint Surg Br 81:37–41
Bloecker K, Guermazi A, Wirth W et al (2013) Tibial coverage, meniscus position, size and damage in knees discordant for joint space narrowing - data from the Osteoarthritis Initiative. Osteoarthritis Cartilage 21:419–427
Alhalki MM, Hull ML, Howell SM (2000) Contact mechanics of the medial tibial plateau after implantation of a medial meniscal allograft. A human cadaveric study. Am J Sports Med 28:370–376
Stone KR, Freyer A, Turek T, Walgenbach AW, Wadhwa S, Crues J (2007) Meniscal sizing based on gender, height, and weight. Arthroscopy 23:503–508
Haut TL, Hull ML, Howell SM (2000) Use of roentgenography and magnetic resonance imaging to predict meniscal geometry determined with a three-dimensional coordinate digitizing system. J Orthop Res 18:228–237
Ihara H, Miwa M, Takayanagi K, Nakayama A (1994) Acute torn meniscus combined with acute cruciate ligament injury. Second look arthroscopy after 3-month conservative treatment. Clin Orthop Relat Res 307:146–154
Pujol N, Beaufils P (2009) Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc 17:396–401
Beaufils P, Hulet C, Dhénain M, Nizard R, Nourissat G, Pujol N (2009) Clinical practice guidelines for the management of meniscal lesions and isolated lesions of the anterior cruciate ligament of the knee in adults. Orthop Traumatol Surg Res 95:437–442
Shelbourne KD, Rask BP (2001) The sequelae of salvaged nondegenerative peripheral vertical medial meniscus tears with anterior cruciate ligament reconstruction. Arthroscopy 17:270–274
Feng H, Hong L, Geng XS, Zhang H, Wang XS, Jiang XY (2008) Second-look arthroscopic evaluation of bucket-handle meniscus tear repairs with anterior cruciate ligament reconstruction: 67 consecutive cases. Arthroscopy 24:1358–1366
Miao Y, Yu JK, Ao YF, Zheng ZZ, Gong X, Leung KK (2011) Diagnostic values of 3 methods for evaluating meniscal healing status after meniscal repair: comparison among second-look arthroscopy, clinical assessment, and magnetic resonance imaging. Am J Sports Med 39:735–742
Ahn JH, Lee YS, Yoo JC, Chang MJ, Park SJ, Pae YR (2010) Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy 26:67–75
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154
Shaffer B, Kennedy S, Klimkiewicz J, Yao L (2000) Preoperative sizing of meniscal allografts in meniscus transplantation. Am J Sports Med 28:524–533
McDermott ID, Sharifi F, Bull AM, Gupte CM, Thomas RW, Amis AA (2004) An anatomical study of meniscal allograft sizing. Knee Surg Sports Traumatol Arthrosc 12:130–135
Ikuma H, Abe N, Uchida Y, Furumatsu T, Fujiwara K, Nishida K, Ozaki T (2008) Novel magnetic resonance imaging evaluation for valgus instability of the knee caused by medial collateral ligament injury. Acta Med Okayama 62:185–191
Sakata K, Furumatsu T, Abe N, Miyazawa S, Sakoma Y, Ozaki T (2013) Histological analysis of failed cartilage repair after marrow stimulation for the treatment of large cartilage defect in medial compartmental osteoarthritis of the knee. Acta Med Okayama 67:65–74
Sakata K, Furumatsu T, Miyazawa S, Okada Y, Fujii M, Ozaki T (2013) Comparison between normal and loose fragment chondrocytes in proliferation and redifferentiation potential. Int Orthop 37:159–165
Barrett GR, Field MH, Treacy SH, Ruff CG (1998) Clinical results of meniscus repair in patients 40 years and older. Arthroscopy 14:824–829
Weiss CB, Lundberg M, Hamberg P, DeHaven KE, Gillquist J (1989) Non-operative treatment of meniscal tears. J Bone Joint Surg Am 71:811–822
Magnussen RA, Mansour AA, Carey JL, Spindler KP (2009) Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg 22:347–357
DeHaan A, Rubinstein RA Jr, Baldwin JL (2009) Evaluation of success of a meniscus repair device for vertical unstable medial meniscus tears in ACL-reconstructed knees. Orthopedics 32(4)
Pujol N, Tardy N, Boisrenoult P, Beaufils P (2013) Magnetic Resonance Imaging is not suitable for interpretation of meniscal status ten years after arthroscopic repair. Int Orthop [Epub ahead of print]
Vrancken AC, Buma P, van Tienen TG (2013) Synthetic meniscus replacement: a review. Int Orthop 37:291–299
Kim YM, Joo YB, Cha SM, Hwang JM (2012) Role of the mechanical axis of lower limb and body weight in the horizontal tear and root ligament tear of the posterior horn of the medial meniscus. Int Orthop 36:1849–1855
Bylski-Austrow DI, Ciarelli MJ, Kayner DC, Matthews LS, Goldstein SA (1994) Displacements of the menisci under joint load: an in vitro study in human knees. J Biomech 27:421–431
Acknowledgments
We are grateful to Prof. Nobuhiro Abe for his support. This work was supported by grants from the Japan Society for the Promotion of Science (No. 24791546).
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Furumatsu, T., Miyazawa, S., Tanaka, T. et al. Postoperative change in medial meniscal length in concurrent all-inside meniscus repair with anterior cruciate ligament reconstruction. International Orthopaedics (SICOT) 38, 1393–1399 (2014). https://doi.org/10.1007/s00264-013-2238-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2238-1