Abstract
Purpose
Is it rational to recommend surgical reconstruction of the torn anterior cruciate ligament to every patient? Is conservative management still a valid option?
Method
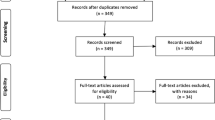
Through a literature review, we looked for the arguments from each side and checked their validity.
Results
Unfortunately results of most studies cannot be compared because of the following reasons not exhaustively cited: studied populations differed with respect to age, sex, professional and sports activity level, lesions associated with ACL rupture, patient recruitment methods, time from injury to treatment and different therapeutic modalities. Furthermore, various methods were used to evaluate the clinical and radiological results and there was no consensus of their interpretation. Some authors assumed that the incidence of further meniscus lesions could probably be reduced if the torn ACL was surgically reconstructed. But, we have no evidence to believe that this would be due to the surgical repair rather than to a decrease of involvement in strenuous activities. At present it is not demonstrated that ACL-plasty can prevent osteoarthritis. Numerous factors could explain evolution to arthrosis whatever the treatment for the ACL-ruptured knee. Studies comparing surgical and conservative treatments confirm that ACL reconstruction is not the pre-requisite for returning to sporting activities. More recent and scientifically well-designed studies demonstrate that conservative treatment could give satisfactory results for many patients. They suggest some methods to help them choose the best treatment.
Conclusion
At present there are no evidence-based arguments to recommend a systematic surgical reconstruction to any patient who tore his ACL. Knee stability can be improved not only by surgery but also by neuromuscular rehabilitation. Whatever the treatment, fully normal knee kinematics are not restored. While the patients wish to go back to their sport and want everything possible done to prolong their ability to perform these activities, they should be informed that the risk of further knee lesions and osteoarthritis remains high, whatever the treatment, surgical or conservative.
Level of evidence
Systematic review of Level I, II, III and IV studies, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thirty-five years ago, it was stated that a rupture of the anterior cruciate ligament was ‘the beginning of the end’ of the knee [105].
In 1983, Noyes et al. [76] wrote ‘A dilemma still exists concerning the proper treatment of a knee with a deficient anterior cruciate ligament, largely because of a lack of knowledge of the extent of the functional disability caused by such an injury.’
In 1987, Kannus and Järvinen [47] began their report published in the Journal of Bone and Joint Surgery by the following sentence: ‘Controversy still exists concerning the proper treatment of a knee with a ruptured anterior cruciate ligament.’ They suggested some explanations. The first one as to why the controversy exists is the heterogeneity of the initial injury in the patients whose cases have been studied. So, the populations may have differed with respect to sports activity, degree of injury, lesions associated with the injured ACL. Susceptibility bias arises when comparing the results of therapy for groups that are prognostically dissimilar. This could be avoided by randomly allocating to the same population either a conservative or a surgical treatment.
A quarter century later such a study still does not exist. Moreover, a discussion about the proper treatment after an ACL rupture could seem obsolete as it is illustrated by the imbalance between the number of reports on operative treatment compared with those on non-operative treatment.
Numerous studies concerning ACL functional anatomy and technical progress progressively induced modifications of the recommended surgical treatments from extra-articular ACL substitution to intra-articular reconstructive procedures of one single or double or triple bundles of the ACL. More and more studies recommend earlier surgical reconstruction after ACL injury in order to prevent further meniscal damage and to decrease the risk of degenerative arthritis [14, 19, 30, 34, 46, 49, 55, 79, 103]. Are these assertions well demonstrated or still speculative?
On the other hand, a few studies demonstrated that good functional results could be obtained by conservative measures in the majority of subjects with unilateral unreconstructed ACL injury.
The purpose of this paper is to critically review the literature regarding scientific support for different treatment algorithms after an ACL injury. This information could help physicians to choose the best treatment for each patient.
ACL rupture could induce degenerative changes in the knee joint
Several studies [13, 47, 66, 74, 76, 95], most of them published before 2000, revealed an increasing [76] or greater frequency [13, 47, 66, 74, 95] of abnormal radiographs over time, between 24 [13] and 86% [74] of cases 5–34 years after the injury causing ACL rupture left untreated. But, some of these retrospective studies concerned only patients with ACL tear who sought treatment for relief of their symptoms [76, 95]. This selection bias induced an overestimation of the incidence of symptomatic arthrosis after untreated ACL rupture. Others contacted patients who had undergone initially either a medial or a bi-compartmental meniscectomy and who also had an ACL rupture. The prevalence of radiographic arthrosis was between 77 and 86% of the patients and was seven times greater than in the contralateral normal knee at a mean follow-up of 27 years (20–34 years) [74, 75]. It is not a surprise that after such a long follow-up the incidence of arthrosis was so high in knees where not only the ACL was absent but also one or both menisci were excised. It was well demonstrated that 14 years after an ACL tear whatever the treatment, conservative or surgical, subjects with a meniscus tear associated with an ACL rupture had a higher prevalence of radiographic osteoarthritis than those with an isolated ACL rupture, 59% versus 31% [108]. When the selection criteria to recall the patients was an initial ACL rupture left untreated associated or not with other lesions, the incidence of radiographs demonstrating some joint space narrowing was present in 24% of the patients after a mean follow-up of 8.5 years (5–12 years) [13] or 31% after 15 years [66].
These small samples cannot illustrate the true natural history of the ACL-deficient knee. This could only be characterised by a well-designed randomised clinical trial that does not exist. Nevertheless, it is evident that an ACL rupture can induce degenerative changes over time, although we do not know the risk. Because of this, we are not able to give undeniable information to our patients.
After ACL reconstruction, the incidence of abnormal radiographs varied between 10 and 71% of the patients followed for 7 to more than 15 years [40] on average and a minimum of 5 years [15, 19, 22, 26, 35, 37, 40, 45, 46, 50, 56–58, 88, 90, 93, 94, 100, 111]. By comparing these results with those of series where the ruptured ACL was left untreated, could we conclude that radiographic abnormalities were less frequent after a surgical treatment? For different reasons, already well explained by Kannus and Järvinen [47], it is not scientifically valid to compare results between studies published at different historical periods. Moreover, various radiographic techniques and definitions of arthrosis were used, inducing detection bias and thus reliable comparisons between these studies are impossible. Firstly, radiographs were taken with the patients sometimes standing and sometimes lying on the table with the knee in extension or 20–45° flexed. Secondly, radiographs were evaluated according to criteria of Ahlbäck, Fairbank, Kellgren and Lawrence or IKDC form. Thirdly, the interpretation of these criteria to evoke a diagnosis of arthrosis was different from one study to another which used ‘adapted’ classifications [82] or scales developed by the authors but unpublished [47]. Finally, the great differences of arthrosis frequency between all these studies could be explained by susceptibility bias due to the studied populations who might have differed with respect to age, sex, participation in sports activity, accompanying meniscal injury, patient recruitment methods and time from injury to inclusion in the study.
At present we cannot assume that the incidence of arthrosis radiographically illustrated by some degree of space narrowing is less frequent in ACL-reconstructed than in ACL-unreconstructed knees. This statement was confirmed by a systematic review of studies on the prevalence of knee osteoarthritis more than 10 years after ACL injury [77]. In the same way, no one study led us to suggest that ACL reconstruction would be able to prevent the progressive deterioration of the knee. No one study was designed to give a clear answer to this question despite the recommendations already formulated in 1994 by Lohmander and Roos who encouraged prospective, controlled, randomised and masked studies that could aim to evaluate the utility of ligament reconstruction to prevent post-traumatic osteoarthritis [60].
Radiographic classifications
In 1963, Ahlbäck observed knee radiographs with pathologic bone remodelling at the medial femorotibial articulation even though the distance between the articular joint surfaces was normal indicating articular cartilage of normal thickness [4]. He realised that these pathologic signs were observed on radiographs obtained under non-weight-bearing conditions as was generally done in most departments of diagnostic radiology at this time. Since this publication, it had been recommended to obtain radiograms under weight-bearing conditions with the knee in extension following the technique used by Ahlbäck. At present, weight-bearing anteroposterior radiographs with the knee in slight flexion are considered as the gold standard to diagnose arthrosis precociously [18]. In his publication, Ahlbäck did not propose any radiographic staging of arthrosis. Nevertheless, Ahlbäck classification criteria were described in recent publications in order to classify knee arthrosis in six stages, from 0 to V where stage 0 indicates no radiographic sign of arthrosis and stage I indicates a narrowing of the joint space of at least 50% of the space width in the other compartment or in the homologous compartment of the other knee [31]. It is a little different from the criteria explained in the study of Lidén et al. [58] where stage I is characterised by a narrowing less than 50%. But these subtle differences could not lead to different estimations of arthrosis incidence since it was decided that radiographic arthrosis was found present or absent when there was a joint space narrowing or not, whatever its amount.
Fairbank studied the pre-operative and post-operative radiographs in one hundred and seven cases, 3 months to 14 years after meniscectomy [25]. He described three types of radiographic changes: the formation of an anteroposterior ridge from the margin of the femoral condyle, flattening of the marginal half of the femoral articular surface and narrowing of the joint space. He noted that the femoral ridge may be seen even before operation and that no correlation was found between clinical and radiographic findings. With observations of arthrograms he demonstrated that the ridge consists solely of bone and that the articular cartilage is still present. He concluded that meniscectomy interferes with the mechanics of the joint and that it seems likely that narrowing of the joint space will predispose to early degenerative changes. But he did not present any type of classification. Nevertheless, for example, in their study, Cohen et al. [15] analysed the radiographs following the criteria of Fairbank and classified them into 4 grades: grade 0 (normal), 1 (mild changes), 2 (moderate changes) and 3 (severe changes) without any other information. They considered that arthrosis was present from the radiographic grade of 1. For others, osteoarthritis was classified according to Ahlbäck and Fairbank on a composite scale from grade 0 to grade III where in grade I there are some osteophytes and remodelling of the condyle but no joint space narrowing and in grade II joint space was reduced up to 50% [66].
The publication of Kellgren and Lawrence presented the radiological assessment of osteoarthrosis in eight groups of joints: distal interphalangeal, metacarpophalangeal, first carpo-metacarpal, wrist, cervical spine, lumbar spine, hip and knee. Osteoarthrosis was divided into five grades: none (0), doubtful (1), minimal (2), moderate (3) and severe (4) [48]. On the illustrations of knee radiographs, we can observe that the one illustrating a grade 1 of osteoarthrosis demonstrates some flattening of the condyle, minimal osteophytes of the joint margins and of the tibial spines but no joint space narrowing. The radiograph of a grade 2 reveals more developed osteophytes and a minimal joint space narrowing indicating in the opinion of the authors that osteoarthrosis is definitely present though of minimal severity. The radiograph used to illustrate a grade 3 arthrosis demonstrates a joint space narrowing equal or greater than 50% of the space width observed on the grade 1 radiograph and in grade 4, there is an obliteration of the joint space.
It must be remembered that a diagnosis of arthrosis can only be evoked when articular cartilage is damaged. Consequently it could induce a joint space narrowing which has to be present to evoke knee osteoarthritis following some authors [19, 37, 50, 56, 57, 74, 75, 108]. This definition of osteoarthritis corresponds to Kellgren and Lawrence osteoarthritis grade 2 as specified by von Porat et al. [108]. But in some studies they used an ‘adapted’ grading system where radiographs demonstrating osteophytes without joint space narrowing were considered as Kellgren and Lawrence grade 2 rather than grade 1 [82]. This definition, different from the original description of the authors, could lead to an overestimation of arthrosis frequency.
In order to prevent the detection bias induced by the different methods of evaluation of arthrosis, it could be better to consider three types of radiographs: normal and abnormal with or without joint space narrowing as presented in IKDC form published in June 1993 [36]. Following the recommendations of the IKDC form authors, radiographs should be taken in a standing position with the knee in 30° of flexion. But because of tibial slope angles varying between the subjects, the radiologic beam should be aligned parallel with the tibial plateaus. This was well demonstrated by Buckland–Wright et al. who recommended radiography of each knee in the standing position and flexed until the tibial plateau was horizontal relative to the floor, parallel to the central X-ray beam and perpendicular to the radiographic film. They reported that the degree of flexion ranged between 179 and 160° depending on the tibial slope angle which varies between individuals [10]. Following the IKDC form, radiographs are rated nearly normal (grade B) if there are minimal changes: osteophytes, slight sclerosis or flattening of the condyle but the joint space is wider than 4 mm. Arthrosis will be evoked only when some joint space narrowing is present.
It can be concluded that the discrepancies between all these classifications and their interpretation could explain the great variability of arthrosis frequency calculated in the different series as was also concluded in a recent systematic review of literature [77]. Arthrosis is always less frequent in the publications using Ahlbäck [22] or IKDC form definitions [37, 56, 90] than in those using Fairbank’s criteria [15, 111] where some remodelling of the condyle or osteophytes even without space joint narrowing were considered as signs of arthrosis while others considered these features as ‘typical post-meniscectomy changes, but not arthritis’ [75]. This was well illustrated in the study of Lidén et al. [58] where degenerative changes indicating arthrosis were identified in 23 or 74% of the patients according to Ahlbäck or Fairbank criteria, respectively.
Could ACL reconstruction prevent osteoarthritis?
Studies comparing surgically reconstructed ACL knees with ACL-deficient knees conservatively treated could be better to give a more definite answer.
The first comparative study was that of Dale Daniel and co-workers who reported on average 64 months after an injury which ruptured the ACL higher incidence of arthrosis in ACL-reconstructed knees than in un-operated ACL-deficient knee, even if the menisci were intact and while the activity level was not different between the groups at last follow-up or review [17]. Rather than indicating that ACL reconstruction induced arthrosis, this study suggested that ACL reconstruction did not prevent arthrosis. Nevertheless, some reconstruction procedures used in this study are not recommended at present. Indeed, the difference between both knees of anterior tibial displacement at manual maximum force measured by KT-1000 arthrometer was less than 3 mm in only 30% of the reconstructed knees versus 16% of the unreconstructed. However, this higher incidence of arthrosis in patients surgically treated was also reported in a more recent study from the same hospital where ACL was reconstructed with a BPTB autograft [27]. Early reconstructed patients had higher rates of degenerative changes on radiographs than did unreconstructed patients but Tegner scores were significantly lower in conservatively treated patients. This resulted from non-randomisation of treatments. Early ACL reconstruction, defined as within 3 months of injury, was recommended to those patients participating in Level I or II jumping or cutting sports more than 50 h per year and where KT-1000 arthrometer manual maximum injured-normal difference was at least 5 mm. Conservative treatment was recommended to patients where the KT-1000 arthrometer difference was inferior to 5 mm except if they participated more than 200 h per year in jumping or cutting sports. The two cohorts of patients were therefore different not only in activity level but also concerning the amount of post-traumatic laxity which was greater in the surgically treated patients.
Different samples of the Swedish soccer players who ruptured their ACL in 1986 were evaluated at 7 [85], 12 [61] and 14-year follow-up [108]. Sixty per cent of the players had undergone reconstructive surgery of the ACL and the others were conservatively treated. Radiographs demonstrating some joint space narrowing were observed in 51% of the female players reviewed after 12 years and in 41% of the male players reviewed after 14 years. These percentages were calculated in relation to all the subjects of the series and no differences were seen between surgically and conservatively treated patients with regard to not only radiographic arthrosis but also prevalence of symptoms or sports activity level. Seven years after the index injury, 32% were still participating in organised soccer compared to 7.8% at the 14-year follow-up. One reason evoked by the authors was that as the subjects got older they had families and had less time for soccer [108].
In their study of ACL injuries suffered by players in the three upper divisions of the Norwegian handball team during two seasons of competition, the authors were able to review 79 patients on average 7 years after their injury [70]. The treatment was conservative and the ACL was not reconstructed in 22 cases. Out of the 57 players in the operative group, 47 (82%) had a bone-patellar tendon-bone (BPTB) graft reconstruction, in 8 the ligament was sutured (14%) and the procedure performed in 2 players (4%) was unknown. Meniscal or cartilage associated lesions were not mentioned in this study. Although laxity was somewhat greater in the conservatively treated group, return to the same level of sports was significantly more frequent in the conservatively treated patients, 82% versus 58% of the surgically treated patients. But, the incidence of knee arthrosis defined as grade C or D in the IKDC classification was not different between the two groups, 42 and 46% in the operated and the conservatively treated group, respectively. Furthermore, there was no correlation between arthrosis and pain scores.
Fink et al. [26] in 2001 presented the long-term outcome of early reconstructed ACL with a BPTB graft compared to conservatively treated ACL-ruptured knee patients. There was no significant difference for additional injuries, extent of anterior laxity or sports participation prior to injury between the two groups. The incidence of radiographs demonstrating some joint space narrowing was 48 and 50% of the cases in the non-operative and operative groups, respectively after a mean follow-up of 11 years. But the initial treatment, surgical ACL reconstruction or not, was chosen by the patients. This introduced susceptibility bias by comparing the results of therapy for groups that could be prognostically dissimilar. While there was no difference of the level of sports participation between the two groups before ACL rupture, the level of sports participation was significantly lower in the non-operative group at last follow-up. The authors concluded that ACL reconstruction can provide long-term patient satisfaction and continued sports participation. The degree of arthrosis increased over time in both the operative and non-operative groups. This study could not conclude that ACL reconstruction had a beneficial effect on further degeneration of the knee. A significant correlation between participation in high-risk pivoting sports such as soccer or basketball and osteoarthritic changes was also found for the non-operative group.
A more recent study reported the results of 109 patients with an isolated ACL rupture and without any meniscal or cartilage associated lesion [50]. The choice of treatment was based on agreement between the surgeon and the patient independent of the sport activity level. The incidence of radiographs demonstrating some joint space narrowing was significantly higher in the ACL reconstructed with a BPTB graft (n = 60) than in the conservatively treated group (n = 49), 45% versus 24%. The mean follow-up time was 11.1 years (7.5–16.3 years). They concluded that the risk of developing osteoarthritis after ACL rupture was significantly greater after ACL reconstruction than after a conservative procedure, while no difference between the two groups could be proven with regard to loss of sports activity.
At present the theory that ACL-plasty is valuable as a means of preventing degeneration of the joint is not confirmed by the published data reviewed by Øiestad et al. [77]. Despite these data, some authors find it appropriate to publish an Editorial where they state that ‘prompt operative intervention reduces long-term osteoarthritis after ACL tear’ [84]. These opposite opinions and persistent controversy are the reflection of the divergent results in published studies, in the majority of which the level of evidence is III or IV or sometimes V, such as the Editorial cited before [84]. Furthermore, in two recent systematic reviews of randomised controlled trials on choice of graft type and surgical technique, or aspects of rehabilitation after ACL injuries, the authors discovered several weaknesses in the study design that could cast doubt on the conclusions [5, 91]. This emphasises the need for further high-quality studies, especially with long-term follow-up [91].
Furthermore, these studies demonstrated that return to sports activities did not depend on the treatment, surgical or conservative. ACL reconstruction is not the pre-requisite nor gives guarantee for participating in sports activities. In an Editorial, Reider [83] noted that even the surgical patients did not return to the same functional levels as before the injury. But, we could not tell from the available information how often this result was due to persistent symptoms, reduced performance, fear of reinjury or a change in athletic opportunities. It was effectively demonstrated that patients who did not return to their pre-injury activity level had more fear of re-injury [54]. In a study where 65% of the patients returned to the same level of sports after an ACL reconstruction, it was revealed that an important factor influencing return to previous sports activity was the psychological profile [33]. This was also very different in patients choosing a reconstructive surgery when compared to those treated conservatively [101]. In the same way, patients choosing ACL reconstruction rather than conservative treatment had higher pre-injury activity level [100]. Although treatment randomisation would be the only way to give a definite answer to the superiority of one or another treatment, all these observations could indicate that randomisation cannot be accepted by the patients who believe that they get enough information, often from internet, to make the right choice.
Multiple etiological factors of post-traumatic osteoarthritis
Numerous factors could explain evolution to osteoarthritis whatever the treatment for the ACL-ruptured knee. These were exhaustively discussed in the literature analysis done by Lohmander et al. [62].
A persistent and evolving disturbance in cytokine and keratinsulfate profiles was observed in patients’ ACL-deficient knees compared with subjects’ uninjured knees [12]. Arthrosis could be induced by these biochemical alterations that perhaps cannot be corrected by ACL reconstruction.
The lesions associated with ACL rupture, not only those concerning the menisci, but also those affecting the capsule or the cartilage were underestimated. A biomechanical study on cadaver knees demonstrated that significant damage occurred to the articular cartilage and underlying subchondral bone during rupture of the ACL. They concluded that the type and extent of these tissue injuries were a function of the mechanism of ACL rupture [67]. The risk of osteochondral damage is especially present if the mechanism of injury involves a high compression loading component, such as during a jump landing [67].
Marrow signal changes detected only by MRI were frequently observed at time of ACL rupture [16]. They are the signs of subchondral lesions that induced changes in the overlying cartilage in some patients who had evidence of cartilage thinning adjacent to the site of osteochondral lesion demonstrated by MRI 6 years after initial injury and ACL hamstring autograft reconstruction [24]. By reviewing the scientific literature on the natural history of bone bruises after acute knee injury, Nakamae et al. [71] concluded that the results of numerous clinical and experimental studies supported the suggestion that severe bone bruise is a precursor of early degenerative changes.
At a second-look arthroscopy, 15 months on average after an ACL reconstruction by a double bundle of semitendinosus graft, a significant worsening of the status of articular cartilage was observed in all compartments except the lateral femoral condyle independently of residual laxity or of a meniscal lesion [6]. Although it has been well established that articular cartilage, once damaged, has very little response to healing, another study, 6–52 months following ACL reconstruction observed, at second-look arthroscopy, a significant recovery of untreated chondral lesions on both the medial and lateral femoral condyles, but no recovery at the tibial plateaus [72]. The great majority of the cartilage lesions were partial thickness injuries graded I and II by using the Outerbridge classification [78]. The prevalence and severity of concomitant articular cartilage injuries among acute ACL tears are not precisely known. Brophy et al. reviewed five articles, four of them published before 1995, suggesting that the incidence of articular cartilage injury in acute ACL tears was between 16 and 46% [9]. This wide range of incidence could be explained by differences of inclusion criteria between the studies. Furthermore, the grade or location of these cartilage injuries were often not specified. Nevertheless, when present, these cartilage lesions could induce evolution to osteoarthritis even if ACL had been reconstructed.
In a minimum 10-year follow-up study after arthroscopic ACL reconstruction using a bone-patellar tendon-bone autograft, it was demonstrated that arthrosis was correlated with body mass index and age of the patient at time of injury [56].
The activity level was often less rigorously evaluated though it was clearly demonstrated that heavy physical activity is an important risk factor for the development of arthrosis in uninjured knees especially among obese individuals [65]. In the same way, it was reported that weight-bearing sports activity in ex-elite athlete women was associated with a 2–3 fold increased risk of radiologic osteoarthritis in hips and knees in comparison with a control group of the general population [99].
Meniscal lesions and osteoarthritis
Clinical studies where the ACL was intact reported an incidence of 30 [8] to maximum 71% [87] of radiographs demonstrating some degree of space narrowing after total [74] or partial meniscectomy [8] after a minimum follow-up of 5 years [8] and after 21 years [87] or more than 30 years [74]. The incidence of radiographic osteoarthritis was 3–7 times higher than in the contralateral normal knee more than 30 or 25 years, respectively after meniscectomy [74]. By using a control group without previous knee injury or surgery rather than the contralateral knee, the incidence of radiological changes, representing definite tibiofemoral osteoarthritis was seven times greater in the studied than in the control group [86]. The great variability of osteoarthritis incidence between the different studies could be explained by the duration of follow-up, the procedures performed or the diversity of patients studied. Without preoperative radiographs, some studies did not know the incidence of pre-existing arthritic changes [8, 74]. Despite this high percentage of radiological changes, there was no significant correlation between these and the subjective symptoms or functional outcome and subsequent surgical treatments for osteoarthritis were rare [74]. This weak correlation between symptoms and radiographic findings of osteoarthritis was also mentioned in the study of Roos et al. [87]. They found that only patients with the more significant radiographic changes had substantially more pain and more functional impairment than those without any radiological changes.
While numerous studies confirmed that any alteration of the meniscus anatomy could by itself induce radiographic degenerative signs, it was also reported that a successful meniscal repair in intact-ACL knees could not eradicate the risk of secondary radiographic remodelling in 100% of the cases [64]. This could be another demonstration that post-traumatic osteoarthritis is multifactorial in origin.
We conclude that radiographic osteoarthritis, even in intact-ACL knees, is frequently present more than 20 years after a meniscectomy, 3–7 times more frequent than in the contralateral uninjured knee. This could explain why meniscal injury was the most frequently reported risk factor for development of knee osteoarthritis in the studies where the ACL had been injured and yet reconstructed [77].
Timing of ACL reconstruction and prevention of meniscal lesions
As many authors observed that the incidence of meniscal lesions and subsequent meniscectomy [14, 30, 46, 49, 57, 63, 79, 102, 103] or the incidence of cartilage damage [14, 63, 102] as well as the incidence of radiographic degenerative changes [46] were greater in patients operated on later after the index injury, some of them recommended the earliest ACL reconstruction possible [14, 30, 46, 49, 79, 103]. The validity of their recommendations would be confirmed by the studies [19, 34, 55] reporting that early ACL reconstruction after the initial injury is associated with better results than late reconstruction. Conversely in a systematic review of the literature, no difference in clinical outcome was found between patients who underwent ACL reconstruction early, within a mean of 3 weeks post-injury, or delayed, a minimum of 6 weeks post-injury [97]. A randomised trial of treatment of acute ACL tears compared early ACL reconstruction plus structural rehabilitation and early rehabilitation with the option of delayed reconstruction [29]. At the 2-year follow-up, there was no difference between the patient-reported outcomes of the two groups. With the use of the delayed reconstruction strategy, ACL reconstruction was avoided in 61% of the subjects without adversely affecting outcomes. This latest study could confirm the hypothesis, already formulated by Holmes [39], that rather than the earliness of the treatment, the differences between the results could also be explained by the inclusion in the early ACL reconstruction group of patients who would have had a successful evolution with a conservative treatment whereas the group of late ACL reconstruction concerned only patients unsatisfied by the conservative treatment. Better results could also be explained by the lower frequency of meniscal tears in the early reconstructed study groups. It was found 10–15 years after an ACL reconstruction, that meniscectomy was associated with poorer results on objective tests [15, 111] or with significant increase in degenerative changes [37] and that after 7 years the most severe osteoarthritic changes were seen with meniscectomy [46]. It was also reported that after 24.5 years on average (range: 21–28 years) following ACL reconstruction, 61% of the patients with a healthy medial meniscus versus 31% of those having undergone total medial meniscectomy had satisfactory IKDC grade A or B radiographs [81]. Conversely, no differences were found between patients with an ACL tear, isolated or with accompanying injuries, 5–9 years after an ACL reconstruction with a bone-patellar tendon-bone autograft but tibiofemoral osteoarthritis was rare [45].
Evidence is that the results of ACL reconstruction were the poorest in the most injured knees. Therefore, better results could be obtained in the series dealing with acutely reconstructed knees and therefore most likely less injured [38]. Does it mean that ACL would have to be reconstructed systematically in any knees of any subjects? Some surgeons justify this attitude by their fundamental beliefs that with ACL reconstruction the menisci could be preserved and that further articular cartilage damage could be avoided with the result that knee osteoarthritis will be less frequent. At present, as previously noted, no published data confirmed that ACL-plasty could prevent osteoarthritis. But may we state that ACL reconstruction could preserve the integrity of the menisci?
A study of Dunn et al. [23] demonstrated that the risk of further meniscal injuries after an ACL rupture was higher when ACL was not reconstructed. It was a retrospective study of 6,576 active-duty army personnel who had been hospitalised for at least an arthroscopy demonstrating an ACL injury from 1990 to 1996. By analysing the ICD-9-CM diagnostic codes (International Classification of Diseases, 9th Revision, Clinical Modification), they found that 3,795 (58%) underwent ACL reconstruction and 2,781 (42%) did not. They reported that the risk of a subsequent meniscal re-operation was two times higher when the ACL was not reconstructed without indicating the percentages of patients. They also observed that a later ACL reconstruction was done in 27% of the initially unreconstructed ACL patients and also in 6% of the patients in the reconstructed ACL group. Unfortunately, this retrospective follow-up study using administrative databases has limitations: subjects with ACL injury but not hospitalised were not included. The initial hospitalisation did not necessarily indicate the initial time of ACL injury. The diagnostic codes do not include a laterality indicator. This could introduce bias into the study if the contralateral re-injuries were not equally distributed between the two groups. It did not give any information about the activity level or the functional outcome. And finally, at the last follow-up, on average 36 months, with a range of 0.2–107 months, this study could not know if the status of the menisci was different in the two groups and did not give any information about arthrosis incidence.
Frobell et al. suggested another explanation for this higher risk of subsequent meniscal operation when ACL was not reconstructed. In their randomised trial, they mentioned that small meniscal tears diagnosed by MRI immediately after injury were managed more aggressively in the subjects in whom the ACL was reconstructed early and were more likely to be left untreated in the subjects assigned to rehabilitation plus optional delayed ACL reconstruction. This difference of initial management could explain the greater frequency of meniscal surgery during follow-up in the latter group [29].
A reduction of the frequency of further meniscal damage or surgery after ACL reconstruction was also stated in some studies [56, 57, 81]. But it could not be explained only by ACL reconstruction and could also result from a decrease of involvement in strenuous and pivoting sports. In a population with less strenuous sporting activities followed for 2–12 years after an ACL tear treated conservatively, only 5.4% needed ACL surgery and 3.5% required secondary meniscus surgery [13].
At present we do not have any incontestable argument to recommend a systematic surgical reconstruction to any patient who tore his ACL to prevent further meniscus lesions and subsequent degeneration of the joint.
Conservative management after ACL rupture
Some studies [11, 13, 32, 51] confirmed that a conservative treatment remains an option and could give satisfactory results.
Casteleyn and Handelberg [13] reviewed 109 out of 132 patients coming from a general population less interested in sporting activities, at a mean of 8.5 years (range: 5–12 years) after an ACL rupture treated conservatively. The overall IKDC evaluations put 73% of the patients in grades A or B.
In a more recent study, one hundred patients with an acute ACL injury were observed for 15 years [51]. After arthroscopy, they underwent a rehabilitation programme. They were advised to modify their activity level especially by avoiding contact sports. Patients with recurrent giving-way episodes and/or secondary meniscal injuries requiring fixation were excluded. The majority of these excluded cases underwent ACL reconstruction. Sixty-seven % of the initial patients never underwent ACL reconstruction. Among them 60% had the same or higher activity level as before injury at the 3-year follow-up and 31% (n = 21) had a lower activity level which was a decrease of one level in 38% of them. The remaining 9% represent missing or unknown data. The decline in activity level of patients engaged in contact sports at the time of injury affected their subjective quality of life more than patients involved in non-contact sports.
The prevalence of tibiofemoral osteoarthritis was also reported in this same cohort [73]. Only 16% of the patients developed radiographic osteoarthritis. All these patients had their knee meniscectomised. In contrast, none of the non-meniscectomised knees developed osteoarthritis.
Sixty-seven patients from this same cohort, at 15 years on average after the initial injury were evaluated and compared to a control group of uninjured subjects [1]. Their motor function was evaluated by one leg hop test. Their knee muscle strength was determined throughout a range of motion from 0 to 100° flexion and peak torque and total work in isokinetic extension and flexion were measured with a Biodex isokinetic dynamometer at an angular velocity of 90° per second. Their sensory function was evaluated by measuring the threshold for detection of passive motion when performing knee extension or flexion. All these data were compared with those of uninjured individuals. There were no differences between the two groups in hop distance and knee muscle strength. But the patients had significantly poorer kinaesthesia in both legs than the controls.
These observations were confirmed by more recent studies [2, 68]. The study of Ageberg et al. [2] is a randomised controlled trial on training and surgical reconstruction or training only. In the Norwegian study [68], the treatment was not randomly allocated but was chosen by the patients. At a one-[68] or two-year [2] follow-up examination, no differences were detected between the two groups with regard to the ability to resume pre-injury activity level, muscle strength or functional performance.
The randomised study of Frobell et al. also demonstrated that an ACL reconstruction could be avoided in 61% of the patients without compromising the results evaluated at 2 years after injury by providing initially a structured rehabilitation followed by an optional delayed ACL reconstruction instead of an early and systematic reconstruction [29]. The frequency of meniscal resections was greater in the delayed-surgery than in the early-surgery group, 70% versus 48% of the patients, respectively. These data might demonstrate following some authors that menisci may be saved by an early surgical reconstruction [84]. If probably true, at least in young active patients, it has not yet been demonstrated that early reconstruction reduced long-term osteoarthritis incidence after ACL tear.
From these results, ACL-injured subjects should be informed of the possibility of success after non-operative treatment. But informed of the somewhat lesser risk of further meniscal injuries when ACL was reconstructed early, this last therapeutic option could be the more desirable choice for some patients [7]. Can we differentiate the patients who would be satisfied by a conservative treatment from those for whom ACL reconstruction would give greater satisfaction?
Patient’s selection for conservative or surgical treatment
Different methods have been described to make this selection. Fithian et al. [27] used the surgical risk factor (SURF) algorithm of Daniel et al. [17] to prospectively classify 209 patients with acute, isolated ACL injury by surgical risk according to activity level and side-to-side laxity values. The patients with small side-to-side laxity differences and low activity levels were not significantly at risk for later ACL reconstruction or meniscus surgery. Following this algorithm, an ACL reconstruction would be recommended to all patients with high activity levels or/and great side-to-side laxity differences. However, some studies already mentioned that AP knee laxity measurements cannot differentiate compensators and non-compensators [80, 98].
A recent study of Kostogiannis et al. [52] demonstrated that a positive pivot-shift test at 3 months after injury in an awaken patient is the strongest predictor for the future need for ACL reconstruction.
It was also demonstrated that preoperative questionnaire about the functional impairment due to knee injury and its auto-evaluation by the patient could be a predictor of outcome 1 year after anterior cruciate ligament reconstruction [104].
Other studies identified a BMI greater than 30 kg/m² or smoking as factors strongly associated with lower patient-reported outcome as measured by the IKDC subjective knee form after ACL reconstruction [53].
A team from Newark, Delaware used a screening examination to classify highly active patients with and without good dynamic knee stability early after ACL rupture [41, 42]. One of the study inclusion criteria was regular participation in IKDC level I or II activities. They used simple hop tests and validated knee outcome surveys (KOS–ADLS: Knee Outcome Survey–Activities of Daily Living Scale [44]) to identify patients who have a good potential to be conservatively treated with physical therapy over a 2- to 5-week protocol [28]. These so-called ‘potential copers’ represented 42% of the initial population of ACL-injured patients. This short-term non-operative care allowed a rapid return to previous high level activities for nearly 50% of the selected patients. After this successful return to sports activities, the patients were counselled to return to their physicians for further treatment that was ACL reconstruction for 59% of them. The others chose not to undergo surgery, returned to pre-injury sports activities and were very satisfied with this choice at the latest follow-up (range: 1–10 years). This screening examination was able to identify candidates who might safely return to sports and delay the surgical management at a more convenient time or finally choose a non-operative management. They estimated that clinical tests that capture neuromuscular adaptations may be more useful in guiding individualised patient management after ACL injury than only the magnitude of knee laxity and pre-injury activity level used by the SURF algorithm [42].
We can conclude that a conservative treatment gave satisfaction to a great majority of the patients when their sporting activities did not imply competition or could be modified by avoiding contact sports. In a population with an IKDC level I or II activity before injury, it was also demonstrated that some patients could successfully return to the same sporting activities with non-operative management.
Several severity grades of ACL tear
We all know patients with an ACL rupture who do well without surgery. Indeed, it has been clearly demonstrated in cadaver studies that sectioning the ACL induces variable degrees of knee laxity in different specimens [96]. Spontaneous healing of ACL rupture conservatively treated was sometimes observed in our current practise (Fig. 1) and was already well documented by Ihara et al. [43] with the help of sequential MRI evaluations and laxity measurements on stress radiographs. This was further confirmed in a more recent communication describing normal magnetic resonance imaging of previously totally ruptured ACL, and an excellent result in 13 out of 17 patients conservatively treated [20].
These images illustrate the healing potentialities of a partially ruptured ACL. a This man aged 44 years suffered a knee sprain during an assault. At first examination, 3 months later, an ACL tear was suspected because the Lachman sign was present and a glide pivot shift was evoked. MRI confirmed the diagnosis of an acute ACL tear which was probably partial because some fibres kept a normal direction. b The patient was satisfied with a conservative treatment. At one year after initial injury, the Lachman sign was only a little increased with a hard endpoint in comparison with the other knee and the pivot shift was no more evoked. MRI demonstrated a nearly normalised aspect of the ACL. This patient could have undergone unnecessary surgery if an early ACL reconstruction was more systematically recommended
The physicians who manage patients with ACL injury have to keep in mind that spontaneous healing of torn ACL could occur. It is our duty to give the best information to our patients and to advertise them that a too soon performed ACL reconstruction cancels any chance of spontaneous healing that could also give satisfaction.
Complications after surgery
We cannot forget that ACL reconstruction remains associated with some morbidity. Some studies reported that 23 [55] to 28% [106] of the patients underwent additional surgery after ACL reconstruction during a median follow-up of 32 or a mean follow-up of 89 months, respectively. The most frequent reason for additional surgery was meniscal lesion (6.9%) [55]. More serious complications such as range of motion deficits (6.3%) or infection (0.6%) requiring a second surgical procedure were also reported [55].
Some complications may be considered as minor such as morbidity due to graft harvest or fixation devices or the development of a Cyclops lesion [21]. Others are more serious: neurologic or vascular lesions, arthrofibrosis, infections [92, 107, 109]. The incidence of the most severe complications, not readily published, is probably underestimated. In the future, a better evaluation of the complication incidence as well as of the functional outcome could be obtained from the data collected in a national registry like that established in Denmark in 2005 [59]. Technical errors occurred in 9.6% of the cases during graft harvesting, tunnel placement or graft fixation that might have no effect on the final outcome if the surgeon has the required expertise to deal with these incidents intraoperatively [3]. The incidence of graft rupture increases with time after surgery: 3% [110], 6% [89] and between 9 and 12% [22, 50, 90] at 2-, 5- and between 8- to 13-year follow-up, respectively. A contralateral ACL rupture was reported to occur in 3–24% of the surgically treated patients, depending on the length of the follow-up [22, 40, 70, 90, 110]. It is not known if this incidence is higher than this observed in a normal active population or in subjects who were conservatively treated after an ACL injury. But as that was mentioned by Salmon et al., the high percentage (34%) of patients in their series suffering a subsequent ACL injury, graft rupture or contralateral ACL rupture, might be greater than that seen in the normal population [90]. They suggested that specific motor-retraining programmes, as described by Myklebust et al. [69] should be added to the rehabilitation of ACL-reconstructed patients to reduce this risk. Finally, the increase of ACL revision reconstruction publications gives evidence that ACL reconstruction is not a 100% guaranteed successful treatment.
All these unforeseen events could explain that return to the same level of sport activities which is the primary goal of ACL reconstruction was generally reported for 65% of the patients on average [33], or that the results were judged A or B with the IKDC form in only 70% of the patients and that the Tegner activity level dropped from 8 to 6 at a median of 32 months follow-up (21–117 months) [55].
Limitations
For the literature search, the online MEDLINE database was used, but a hand search of relevant journals was also undertaken to find studies related to ACL injuries and published between 1983 and 2011. Not only English but also French articles were included. Studies written in other European languages were not searched. Despite this extensive research, it could be that some studies were not discovered. Nevertheless, these could probably not change the conclusions which tell us that the few evidence-based data do not firmly discredit any kinds of treatment after ACL injuries.
As underlined by others [5, 91], positive studies indicating effectiveness of a treatment are more likely to be published. Our research did not find a lot of publications on surgical complications. Their incidence could probably be underestimated because less successful outcomes are rarely published. Therefore, we are not able to correctly measure the potential benefits and risks of all forms of treatments and particularly of surgical ones.
By reviewing not only Level I and II trials but also Level III and IV studies as well as Level V expert opinions, we artificially lower the Level of Evidence of our work although the conclusions were mainly suggested by the results of Level I or II studies.
Conclusion
This literature review demonstrates that ACL reconstruction does not reduce the incidence of further radiographic osteoarthritis nor guarantee return to sports. There is no doubt that ACL rupture can initiate degeneration of the knee joint. At present no one study has firmly demonstrated that ACL reconstruction is the right way to prevent osteoarthritis. The lesions associated with ACL rupture can be numerous following the injury mechanism and could explain an inescapable evolution to arthrosis despite ACL reconstruction. Furthermore when knee laxity has been improved by ACL-plasty, the best advice given to our patients is probably not to promote return to high-risk pivoting sports.
The patients with an ACL tear should be informed that a surgical reconstruction is not the prerequisite or the only way to return to sports activities that can be resumed also with a conservative treatment. A better selection of the patients for surgical or conservative management is possible and a systematic surgical treatment cannot be suggested only by the amount of laxity or the level of sports activity. This attitude could be beneficial for the patients. Furthermore, less surgery and consequently fewer complications would result in lower healthcare costs which are partly borne by the taxpayer. The primary goal of surgery remains the improvement of knee stability which however can also be improved by a correct neuromuscular rehabilitation in some patients.
Whatever the treatment, surgical or conservative, the patients should be informed that the risk of further knee lesions and osteoarthritis remains high especially if they resume high-risk pivoting sports.
References
Ageberg E, Pettersson A, Fridén T (2007) 15-year follow-up of neuromuscular function in patients with unilateral nonreconstructed anterior cruciate ligament injury initially treated with rehabilitation and activity modification. A longitudinal prospective study. Am J Sports Med 35:2109–2117
Ageberg E, Thomeé R, Neeter C, Silbernagel KG, Roos EM (2008) Muscle strength and functional performance in patients with ACL injury treated with training and surgical reconstruction or training only : a two to five-year follow-up. Arthritis Rheum 59:1773–1779
Almazán A, Miguel A, Odor A, Ibarra JC (2006) Intraoperative incidents and complications in primary arthroscopic anterior cruciate ligament reconstruction. Arthroscopy 22:1211–1217
Ahlbäck S (1968) Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn 277(Suppl):7–72
Andersson D, Samuelsson K, Karlsson J (2009) Treatment of anterior cruciate ligament injuries with special reference to surgical technique and rehabilitation: an assessment of randomized controlled trials. Arthroscopy 25:653–685
Asano H, Muneta T, Ikeda H, Yagishita K, Kurihara Y, Sekiya I (2004) Arthroscopic evaluation of articular cartilage after anterior cruciate ligament reconstruction: a short-term prospective study of 105 patients. Arthroscopy 20:474–481
Bernstein J (2011) Early versus delayed reconstruction of the anterior cruciate ligament. A decision analysis approach. J Bone Joint Surg 93-A:e48(1–5)
Bolano LE, Grana WA (1993) Isolated arthroscopic partial meniscectomy. Functional radiographic evaluation at five years. Am J Sports Med 21:432–437
Brophy RH, Zeltser D, Wright RW, Flanigan D (2010) Anterior cruciate ligament reconstruction and concomitant articular cartilage injury: incidence and treatment. Arthroscopy 26:112–120
Buckland-Wright JC, Macfarlane DG, Williams SA, Ward RJ (1995) Accuracy and precision of joint space width measurements in standard and macroradiographs of osteoarthritic knees. Ann Rheum Dis 54:872–880
Buss DD, Min R, Skyhar M, Galinat B, Warren RF, Wickiewicz TL (1995) Nonoperative treatment of acute anterior cruciate ligament injuries in a selected group of patients. Am J Sports Med 23:160–165
Cameron M, Buchgraber A, Passler H, Vogt M, Thonar E, Fu F, Evans CH (1997) The natural history of the anterior cruciate ligament-deficient knee. Changes in synovial fluid cytokine and keratan sulfate concentrations. Am J Sports Med 25:751–754
Casteleyn PP, Handelberg F (1996) Non-operative management of anterior cruciate ligament injuries in the general population. J Bone Joint Surg 78-B:446–451
Church S, Keating JF (2005) Reconstruction of the anterior cruciate ligament. Timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg 87-B:1639–1642
Cohen M, Tarouco Amaro J, Ejnisman B, Teixeira Carvalho R, Kodi Nakano K, Peccin MS, Teixeira R, Laurino CFS, Abdalla RJ (2007) Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy 23:629–634
Costa-Paz M, Muscolo L, Ayerza M, Makino A, Aponte-Tinao L (2001) Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy 17:445–449
Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR (1994) Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med 22:632–644
Davies AP, Calder DA, Marshall T, Glasgow MMS (1999) Plain radiography in the degenerate knee. A case for change. J Bone Joint Surg 81-B:632–635
Dejour H, Dejour D, Aït Si Selmi T (1999) Laxités antérieures chroniques du genou traitées par greffe libre de tendon rotulien avec plastie latérale extra-articulaire. 148 cas revus à plus de 10 ans. Rev Chir Orthop 85:777–789
Delin C, Silvera S, Djian P, Courroy JB, Rousseau D, Folinais D, Oudjit A, Legman P (2008) Traitement conservateur des ruptures complètes du LCA : étude prospective sur la cicatrisation dirigée du LCA avec restitution anatomique et fonctionnelle chez des patients présélectionnés par des IRM en diffusion. Expérience initiale. Abstract in French. Rev Chir Orthop 94:S293–S294
Delincé P, Krallis P, Descamps PY, Fabeck L, Hardy D (1998) Different aspects of the cyclops lesion following anterior cruciate ligament reconstruction. A multifactorial etiopathogenesis. Arthroscopy 14:869–876
Drogset JO, Grøntvedt T (2002) Anterior cruciate ligament reconstruction with and without a ligament augmentation device. Results at 8-year follow-up. Am J Sports Med 30:851–856
Dunn WR, Lyman S, Lincoln AE, Amoroso PJ, Wickiewicz T, Marx RG (2004) The effect of anterior cruciate ligament reconstruction on the risk of knee reinjury. Am J Sports Med 32:1906–1913
Faber KJ, Dill JR, Amendola A, Thain L, Spouge A, Fowler PJ (1999) Occult osteochondral lesions after anterior cruciate ligament rupture. Six-year magnetic resonance imaging follow-up study. Am J Sports Med 27:489–494
Fairbank TJ (1948) Knee joint changes after meniscectomy. J Bone Joint Surg 30:664–670
Fink C, Hoser C, Hackl W, Navarro RA, Benedetto KP (2001) Long-term outcome of operative or nonoperative treatment of anterior cruciate ligament rupture—Is sports activity a determining variable? Int J Sports Med 22:304–309
Fithian DC, Paxton EW, Stone ML, Luetzow WF, Csintalan RP, Phelan D, Daniel DM (2005) Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am J Sports Med 33:335–346
Fitzgerald GK, Axe MJ, Snyder-Mackler L (2000) A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc 8:76–82
Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS (2010) A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 363:331–342
Gadeyne S, Besse JL, Galand-Desme S, Lerat JL, Moyen B (2006) Lésions méniscales constatées lors de la reconstruction du ligament croisé antérieur. Siège et nature dans une série continue de 156 patients. Rev Chir Orthop 92:448–454
Galli M, De Santis V, Tafuro L (2003) Reliability of the Ahlbäck classification of knee osteoarthritis. OsteoArthr Cartil 11:580–584
Giove TP, Miller SJ, Kent BE, Sanford TL, Garrick JG (1983) Non-operative treatment of the torn anterior cruciate ligament. J Bone Joint Surg 65:184–192
Gobbi A, Francisco R (2006) Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc 14:1021–1028
Goradia VK, Grana WA (2001) A comparison of outcomes at 2 to 6 years after acute and chronic anterior cruciate ligament reconstructions using hamstring tendon grafts. Arthroscopy 17:383–392
Hart AJ, Buscombe J, Malone A, Dowd GSE (2005) Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament. A study using single-photon emission computed tomography at ten years. J Bone Joint Surg 87-B:1483–1487
Hefti F, Müller W, Jakob RP, Stäubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1:226–234
Hertel P, Behrend H, Cierpinski T, Musahl V, Widjaja G (2005) ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10 year clinical results. Knee Surg Sports Traumatol Arthrosc 13:248–255
Holmes PF, James SL, Larson RL, Singer KM, Jones DC (1991) Retrospective direct comparison of three intraarticular anterior cruciate ligament reconstructions. Am J Sports Med 19:596–600
Holmes PF (2001) Letter to the editor. Arthroscopy 17:900–901
Hui C, Salmon LJ, Kok A, Maeno S, Linklater J, Pinczewski LA (2011) Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for “isolated” anterior cruciate ligament tear. Am J Sports Med 39:89–98
Hurd WJ, Axe MJ, Snyder-Mackler L (2008) A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury. Part 1, Outcomes. Am J Sports Med 36:40–47
Hurd WJ, Axe MJ, Snyder-Mackler L (2008) A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury. Part 2, determinants of dynamic knee stability. Am J Sports Med 36:48–56
Ihara H, Miwa M, Deya K, Torisu K (1996) MRI of anterior cruciate ligament healing. J Comp Ass Tomogr 20:317–321
Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD (1998) Development of a patient-reported measure of function of the knee. J Bone Joint Surg 80-A:1132–1145
Järvelä T, Kannus P, Järvinen M (2001) Anterior cruciate ligament reconstruction in patients with or without accompanying injuries: A re-examination of subjects 5 to 9 years after reconstruction. Arthroscopy 17:818–825
Jomha NM, Borton DC, Clingeleffer AJ, Pinczewski LA (1999) Long term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res 358:188–193
Kannus P, Järvinen M (1987) Conservatively treated tears of the anterior cruciate ligament. J Bone Joint Surg 69-A:1007–1012
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kennedy J, Jackson MP, O’Kelly P, Moran R (2010) Timing of reconstruction of the anterior cruciate ligament in athletes and the incidence of secondary pathology within the knee. J Bone Joint Surg 92:362–366
Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS (2008) Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 16:442–448
Kostogiannis I, Ageberg E, Neuman P, Dahlberg L, Fridén T, Roos H (2007) Activity level and subjective knee function 15 years after anterior cruciate ligament injury. A prospective, longitudinal study of nonreconstructed patients. Am J Sports Med 35:1135–1143
Kostogiannis I, Ageberg E, Neuman P, Dahlberg LE, Fridén T, Roos H (2008) Clinically assessed knee joint laxity as a predictor for reconstruction after an anterior cruciate ligament injury. A prospective study of 100 patients treated with activity modification and rehabilitation. Am J Sports Med 36:1528–1533
Kowalchuk DA, Harner CD, Fu FH, Irrgang JJ (2009) Prediction of patient-reported outcome after single-bundle anterior cruciate ligament reconstruction. Arthroscopy 25:457–463
Kvist J, Ek A, Sporrstedt K, Good L (2005) Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 13:393–397
Laxdal G, Kartus J, Ejerhed L, Sernert N, Magnusson L, Faxén E, Karlsson J (2005) Outcome and risk factors after anterior cruciate ligament reconstruction: a follow-up study of 948 patients. Arthroscopy 21:958–964
Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C (2008) Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft. A minimum 10-year follow-up. Am J Sports Med 36:1275–1282
Lerat JL, Chotel F, Besse JL, Moyen B, Binet G, Craviari T, Brunet-Guedj E, Adeleine P, Nemoz JC (1998) Les résultats après 10 à 16 ans du traitement de la laxité chronique antérieure du genou par une reconstruction du ligament croisé antérieur avec une greffe de tendon rotulien associée à une plastie extra-articulaire externe. A propos de 138 cas. Rev Chir Orthop 84:712–727
Lidén M, Sernert N, Rostgård-Christensen L, Kartus C, Ejerhed L (2008) Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autografts: a retrospective, 7-year radiographic and clinical follow-up study. Arthroscopy 24:899–908
Lind M, Menhert F, Pedersen AB (2009) The first results from the Danish ACL reconstruction registry: epidemiologic and 2-year follow-up results from 5, 818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc 17:117–134
Lohmander LS, Roos H (1994) Knee ligament injury, surgery and osteoarthrosis. Truth or consequences ? Acta Orthop Scand 65:605–609
Lohmander LS, Östenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50:3145–3152
Lohmander LS, Englund M, Dahl LL, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries. Osteoarthritis. Am J Sports Med 35:1756–1769
Maffulli N, Binfield PM, King JB (2003) Articular cartilage lesions in the symptomatic anterior cruciate ligament-deficient knee. Arthroscopy 19:685–690
Majewski M, Stoll R, Widmer H, Müller W, Friederich NF (2006) Midterm and long-term results after arthroscopic suture repair of isolated, longitudinal, vertical meniscal tears in stable knees. Am J Sports Med 34:1072–1076
McAlindon TE, Wilson PWF, Aliabadi P, Weissman B, Felson DT (1999) Level of physical activity and the risk of radiographic and symptomatic knee osteoarthritis in the elderly: the Framingham study. Am J Med 106:151–157
Meunier A, Odensten M, Good L (2007) Long-term results after primary repair or non-surgical treatment of anterior cruciate ligament rupture: a randomized study with a 15-year follow-up. Scand J Med Sci Sports 17:230–237
Meyer EG, Baumer TG, Slade JM, Smith WE, Haut RC (2008) Tibiofemoral contact pressures and osteochondral microtrauma during anterior cruciate ligament rupture due to excessive compressive loading and internal torque of the human knee. Am J Sports Med 36:1966–1977
Moksnes H, Risberg MA (2009) Performance-based functional evaluation of non-operative and operative treatment after anterior cruciate ligament injury. Scand J Med Sci Sports 19:345–355
Myklebust G, Engebretsen L, Hoff Braekken I, Skjølberg A, Olsen O-E, Bahr R (2003) Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med 13:71–78
Myklebust G, Holm I, Mæhlum S, Engebretsen L, Bahr R (2003) Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury. A follow-up study. Am J Sports Med 31:981–989
Nakamae A, Engebretsen L, Bahr R, Krosshaug T, Ochi M (2006) Natural history of bone bruises after acute knee injury: clinical outcome and histopathological findings. Knee Surg Sports Traumatol Arthrosc 14:1252–1258
Nakamura N, Horibe S, Toritsuka Y, Mitsuoka T, Natsu-Ume T, Yoneda K, Hamada M, Tanaka Y, Boorman RS, Yoshikawa H, Shino K (2008) The location-specific healing response of damaged articular cartilage after ACL reconstruction: short-term follow-up. Knee Surg Sports Traumatol Arthrosc 16:843–848
Neuman P, Englund M, Kostogiannis I, Friden T, Roos H, Dahlberg LE (2008) Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury. A prospective cohort study. Am J Sports Med 36:1717–1725
Neyret P, Donell ST, Dejour H (1993) Results of partial meniscectomy related to the state of the anterior cruciate ligament. Review at 20 to 35 years. J Bone Joint Surg 75-B:36–40
Neyret P, Donell ST, Dejour D, Dejour H (1993) Partial meniscectomy and anterior cruciate ligament rupture in soccer players. A study with a minimum 20-year followup. Am J Sports Med 21:455–460
Noyes FR, Mooar PA, Matthews DS, Butler DL (1983) The symptomatic anterior cruciate-deficient knee. Part I: the long-term functional disability in athletically active individuals. J Bone Joint Surg 65-A:154–162
Øiestad BE, Engebretsen L, Storheim K, Risberg MA (2009) Knee osteoarthritis after anterior cruciate ligament injury. Am J Sports Med 37:1434–1443
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg 43:752–757
Papastergiou SG, Koukoulias NE, Mikalef P, Ziogas E, Voulgaropoulos H (2007) Meniscal tears in the ACL-deficient knee: correlation between meniscal tears and the timing of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 15:1438–1444
Patel RR, Hurwitz DE, Bush-Joseph CA, Bach BR Jr, Andriacchi TP (2003) Comparison of clinical and dynamic knee function in patients with anterior cruciate ligament deficiency. Am J Sports Med 31:68–74
Pernin J, Verdonk P, Aït Si Selmi T, Massin P, Neyret P (2010) Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med 38:1094–1102
Petersson IF, Boegård T, Saxne T, Silman AJ, Svensson B (1997) Radiographic osteoarthritis of the knee classified by the Ahlbäck and Kellgren & Lawrence systems for the tibiofemoral joint in people aged 35–54 years with chronic knee pain. Ann Rheum Dis 56:493–496
Reider B (2005) Understanding the anterior cruciate ligament. Rhythm and algorithm. Am J Sports Med 33:333–334
Richmond JC, Lubowitz JH, Poehling GG (2011) Prompt operative intervention reduces long-term osteoarthritis after knee anterior cruciate ligament tear. Arthroscopy 27:149–152
Roos H, Ornell M, Gärdsell P, Lohmander LS, Linstrand A (1995) Soccer after anterior cruciate ligament injury–an incompatible combination ? A national survey of incidence and risk factors and a 7-year follow-up of 310 players. Acta Orthop Scand 66:107–112
Roos H, Laurén M, Adalberth T, Roos EM, Jonsson K, Lohmander LS (1998) Knee osteoarthritis after meniscectomy. Prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum 41:687–693
Roos EM, Östenberg A, Roos H, Ekdahl C, Lohmander LS (2001) Long-term outcome of meniscectomy: symptoms, function, and performance tests in patients with or without radiographic osteoarthritis compared to matched controls. Osteoarthr Cartil 9:316–324
Ruiz AL, Kelly M, Nutton RW (2002) Arthroscopic ACL reconstruction: a 5–9 year follow-up. Knee 9:197–200
Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K (2005) Incidence and risk factors for graft rupture and controlateral rupture after anterior cruciate ligament reconstruction. Arthroscopy 21:948–957
Salmon LJ, Russell VJ, Refshauge K, Kader D, Connolly C, Linklater J, Pinczewski LA (2006) Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft. Minimum 13-year review. Am J Sports Med 34:721–732
Samuelsson K, Andersson D, Karlsson J (2009) Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy 25:1139–1174
Schulz AP, Götze S, Schmidt HGK, Jürgens C, Faschingbauer M (2007) Septic arthritis of the knee after anterior cruciate ligament surgery. A stage-adapted treatment regimen. Am J Sports Med 35:1064–1069
Seon JK, Song EK, Park SJ (2006) Osteoarthritis after anterior cruciate ligament reconstruction using a patellar tendon autograft. Int Orthop 30:94–98
Shelbourne KD, Gray T (2000) Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery: five to fifteen-year evaluation. Am J Sports Med 28:446–452
Sherman MF, Warren RF, Marshall JL, Savatsky GJ (1988) A clinical and radiographical analysis of 127 anterior cruciate insufficient knees. Clin Orthop Relat Res 227:229–237
Shoemaker SC, Daniel DM (1990) The limits of knee motion. In vitro studies. In: Daniel D, Akeson W, O’Connor J (eds) Knee ligaments, 1st edn. Raven Press, New-York, pp 153–161
Smith TO, Davies L, Hing CB (2010) Early versus delayed surgery for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 18:304–311
Snyder-Mackler L, Fitzgerald GK, Bartolozzi AR III, Ciccotti MG (1997) The relationship between passive joint laxity and functional outcome after anterior cruciate ligament injury. Am J Sports Med 25:191–195
Spector TD, Harris PA, Hart DJ, Cicuttini FM, Nandra D, Etherington J, Wolman RL, Doyle DV (1996) Risk of osteoarthritis associated with long-term weight-bearing sports. Arthritis Rheum 39:988–995
Sutherland AG, Cooper K, Alexander LA, Nicol M, Smith FW, Scotland TR (2010) The long-term functional and radiological outcome after open reconstruction of the anterior cruciate ligament. J Bone Joint Surg 92-B:1096–1099
Swirtun LR, Eriksson K, Renström P (2006) Who chooses anterior cruciate ligament reconstruction and why? A 2-year prospective study. Scand J Med Sci Sports 16:441–446
Tandogan RN, Taşer O, Kayaalp A, Taşkiran E, Pinar H, Alparslan B, Alturfan A (2004) Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Taumatol Arthrosc 12:262–270
Tayton E, Verma R, Higgins B, Gosal H (2009) A correlation of time with meniscal tears in anterior cruciate ligament deficiency: stratifying the risk of surgical delay. Knee Surg Sports Tramatol Arthrosc 17:30–34
Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J (2008) Self-efficacy of knee function as a pre-operative predictor of outcome one year after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 16:118–127
Torg JS, Conrad W, Kalen V (1976) Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med 4:84–93
Van Dijck RAHE, Saris DB, Willems JW, Fievez AWFM (2008) Additional surgery after anterior cruciate ligament reconstruction: can we improve technical aspects of the initial procedure? Arthroscopy 24:88–95
Van Tongel A, Stuyck J, Bellemans J, Vandenneucker H (2007) Septic arthritis after arthroscopic anterior cruciate ligament reconstruction. A retrospective analysis of incidence, management and outcome. Am J Sports Med 35:1059–1063
von Porat A, Roos EM, Roos H (2004) High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis 63:269–273
Wang C, Ao Y, Wang J, Hu Y, Cui G, Yu J (2009) Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: a retrospective analysis of incidence, presentation, treatment, and cause. Arthroscopy 25:243–249
Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, Marx RG, McCarty EC, Parker RD, Wolcott M, Wolf BR, Spindler KP (2007) Risk of tearing the intact anterior cruciate ligament in the controlateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction. A prospective MOON cohort study. Am J Sports Med 35:1131–1134
Wu WH, Hackett T, Richmond JC (2002) Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction. A long-term prospective study. Am J Sports Med 30:845–850
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Delincé, P., Ghafil, D. Anterior cruciate ligament tears: conservative or surgical treatment? A critical review of the literature. Knee Surg Sports Traumatol Arthrosc 20, 48–61 (2012). https://doi.org/10.1007/s00167-011-1614-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1614-x