Abstract
Purpose
Anterior cruciate ligament (ACL) reconstruction can reduce the risk of developing osteoarthritic knees. The goals of ACL reconstruction are to restore knee stability and reduce post-traumatic meniscal tears and cartilage degradation. A chronic ACL insufficiency frequently results in medial meniscus (MM) injury at the posterior segment. How ACL reconstruction can reduce the deformation of the MM posterior segment remains unclear. In this study, we evaluated the form of the MM posterior segment and anterior tibial translation before and after ACL reconstruction using open magnetic resonance imaging (MRI).
Methods
Seventeen patients who underwent ACL reconstructions without MM injuries were included in this study. MM deformation was evaluated using open MRI before surgery and 3 months after surgery. We measured medial meniscal length (MML), medial meniscal height (MMH), medial meniscal posterior body width (MPBW), MM–femoral condyle contact width (M-FCW) and posterior tibiofemoral distance (PTFD) at knee flexion angles of 10° and 90°.
Results
There were no significant pre- and postoperative differences during a flexion angle of 10°. At a flexion angle of 90°, MML decreased from 43.7 ± 4.5 to 41.4 ± 4.5 mm (P < 0.001), MMH from 7.5 ± 1.4 to 6.9 ± 1.4 mm (P = 0.006), MPBW from 13.1 ± 2.0 to 12.2 ± 1.9 mm (P < 0.001) and M-FCW from 10.0 ± 1.5 to 8.5 ± 1.5 mm (P < 0.001) after ACL reconstruction. The PTFD increased from 2.1 ± 2.8 to 2.7 ± 2.4 mm after ACL reconstruction (P = 0.015).
Conclusions
ACL reconstruction affects the contact pattern between the MM posterior segment and medial femoral condyle and can reduce the deformation of the MM posterior segment in the knee-flexed position by reducing abnormal anterior tibial translation. It possibly prevents secondary injury to the MM posterior segment and cartilage that progresses to knee osteoarthritis.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In conservative treatment of anterior cruciate ligament (ACL) injuries, a high risk of meniscal injury or cartilage damage that progresses to knee osteoarthritis (OA) exists [1]. Long-term progression of knee OA still occurs even with ACL reconstruction [11]. However, studies have reported that patients who have undergone ACL reconstruction have a predominantly lower risk of developing OA than those who received conservative therapy for a knee with ACL failure [10, 15, 19]. This could be due to the increased injury in the medial meniscus (MM) in knees with chronic ACL failure [8]. Moreover, the MM surgery rate is reportedly six times higher in patients who undergo ACL reconstruction ≥ 12 months after an ACL injury [24], and a history of MM surgery associated with ACL reconstruction is a strong predictive factor for knee OA [12].
The ACL is a major source of resistance during the anterior drawer at all flexion angles and during internal rotation at flexion angles < 35° [20], while the MM is an important secondary stabilizer for anterior tibial translation [2, 13, 17, 23]. Abnormal anterior tibial translation moves the meniscal posterior segments posteriorly relative to the tibial surface [4], which is thought to be the mechanism involved in the increased incidence of MM tears observed in knees with chronic ACL injury [2]. ACL reconstruction seems necessary to prevent secondary MM injury. One magnetic resonance imaging (MRI) study by Narazaki et al. [18] reported that with 10° of knee flexion, the anteroposterior length and radial extrusion of the MM increased after ACL reconstruction; however, just how ACL reconstruction reduces MM injury remains unclear. In a previous radiograph study, ACL reconstruction suppressed abnormal anterior tibial translation [9]. The same was true for studies using cadaveric knees [14]. Therefore, it is suggested that ACL reconstruction can prevent sequential injury of the MM posterior segment during ACL insufficiency [8].
In this study, MM morphology and tibial position before and after ACL reconstruction were assessed using sagittal open MRI without weighting, at 10° and 90° of knee joint flexion. Furthermore, the influence of ACL reconstruction on the MM posterior segment was investigated. We hypothesized that ACL reconstruction affects the form of the MM and anterior tibial translation in ACL-injured knees. We also hypothesized that in knees with an ACL injury, abnormal anterior tibial translation results in excessive stress on the posterior segment of the MM during knee joint flexion and that ACL reconstruction affects the contact pattern between the MM posterior segment and medial femoral condyle. This is because ACL reconstruction can reduce the deformation of the MM posterior segment by decreasing abnormal anterior tibial translation. Here the relationship between MM posterior segment and anterior tibial translation before and after ACL reconstruction was reported using open MRI.
Materials and methods
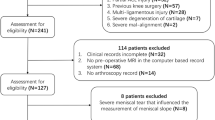
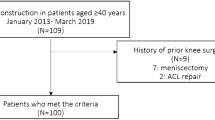
Between 2014 and 2016, 18 knees of 18 consecutive patients who underwent primary ACL reconstructions with intact MM were included in the study. In the final analysis, pre- and postoperative MRI scans of 17 knees (94%) were evaluated. One knee was excluded because of the lack of appropriate MRI scans. The patients (ten men and seven women) had a median age of 22 years (range 14–42 years). The median time from injury to preoperative MRI was 2 weeks (range 1–4 weeks). The median time at which the ACL reconstruction was performed was 3 months (range 1–5) after injury. Postoperative MRI was performed at a median of 3 months (range 3–4 months). Medical records were reviewed retrospectively to examine age, sex, height, body weight, Lysholm score [26], Tegner activity scale score [26] and MRI findings. Patient demographics are shown in Table 1.
Surgical procedure and postoperative care
Routine arthroscopic evaluation was performed prior to ACL reconstruction. No tears, instability and degenerative changes in the MM were observed during the surgery of any knees. All ACL reconstructions were performed using a hamstring tendon autograft (semitendinosus and/or gracilis muscles, anatomic double-bundle reconstruction). Femoral and tibial bone tunnels were created within the ACL footprints as previously described [5, 6, 25]. Graft fixation on the femoral side was achieved using an Endobutton CL (Smith & Nephew, Andover, MA, USA) and ACL TightRope (Arthrex, Naples, FL, USA). Graft fixation on the tibial side was performed using a double-spike plate and a screw (Meira, Aichi, Japan). An initial force of 30 and 20 N was applied to the graft for the anteromedial bundle and posterolateral bundle, respectively, at 10° of knee flexion. Postoperative rehabilitation protocols were similar for all patients. All patients began knee motion exercises and partial weight-bearing at 2 weeks postoperatively. Postoperatively, full weight-bearing and running were permitted at 1 and 5 months, respectively. Return to competitive sports was permitted at 8 months [6].
MRI measurement
MRI was performed using the Oasis 1.2 T (Hitachi Medical, Chiba, Japan) with a coil under the 10° and 90° knee-flexed position in a non-weight-bearing condition. Standard sequences of the Oasis included a sagittal proton density-weighted sequence (repetition time [TR]/echo time [TE], 1718/12) using a driven equilibrium pulse with a 90° flip angle and coronal T2-weighted multi-echo sequence (TR/TE, 4600/84) with a 90° flip angle. The slice thickness was 4 mm with a 0-mm gap. The field of view was 16 cm with an acquisition matrix size of 320 (phase) × 416 (frequency).
Measurements of the MM and tibial position were performed using a simple MRI-based meniscal sizing technique on the sagittal and coronal views at knee flexion angles of 10° and 90° (Figs. 1a, b, 2a, b) [7]. Details of the meniscal sizing are shown in Figs. 1 and 2. The axial views were taken parallel to the medial tibial plateau. A posterior condylar (PC) line was drawn intersecting the most posterior edge of the femoral condyles on the axial image. The sagittal views were created vertical to the PC line. The measurement plane was a sagittal plane with the longest medial meniscal length (MML). Measurements at 90° of knee joint flexion were also performed using the same procedure. However, in consideration of the internal rotation of the tibia in the flexion position, the measurement plane was rotated 3 degrees internally from the PC line. In addition, in order to improve accuracy, the medial edge of the MM in the sagittal plane was determined as a reference in all cases. Furthermore, the number of slices every 4 mm of the measurement surface was the same before and after the surgery. The distance from the anterior to the posterior margin of the MM on the sagittal image was the MML (Figs. 1c, 2c). The medial meniscal height (MMH) was the distance from the bottom to the top of the MM posterior segment (Figs. 1c, 2c). The longest MML view was measured. The width of the inferior surface of the meniscus at its posterior segment was the medial meniscal posterior body width (MPBW) (Figs. 1c, 2c). The MM–femoral condyle contact width (M-FCW) was the distance from the inner edge of the MM posterior segment to the portion of contact between the upper surface of the MM posterior segment and the femoral condyle (Figs. 1c, 2c). The distance from the perpendicular line of the tibial posterior edge to the back of the femoral posterior condyle edge was the posterior tibiofemoral distance (PTFD) (Figs. 1c, 2c). To validate the measurements, four orthopaedic surgeons (HI, MF, YK and TO), who were blinded to the study aims, retrospectively reviewed the radiographic images and MRI scans. To determine intra- and interobserver repeatability, the intraclass correlation coefficient (ICC) was calculated based on two-way, random, single measures with absolute agreement. All measurements demonstrated high precision with ICCs for both intra- and interobserver reliability levels of 0.92 or more. All parameters of the ACL-deficient (preoperative) and ACL-reconstructed (postoperative) knees were compared. The Lysholm score and Tegner activity scale score were used in the clinical evaluation.
This study was approved by Institutional Review Board of Okayama University Graduate School (1857), and the patients provided their informed consent.
Statistical analysis
Pre- and postoperative meniscal measurements were evaluated using the paired t test. Clinical value was evaluated using the Wilcoxon signed-rank test. Power and statistical analyses were performed using EZR-WIN software. Data are presented as the mean ± standard deviation. Significance was set at P < 0.05. Sample size was estimated for a minimal statistical power of 80% (α = 0.05). All sample size and power calculations were completed using EZR-WIN software. Required sample size for the MPBW at 90° of knee flexion was 18.
Results
Clinical evaluations
ACL reconstruction improved knee-associated symptoms. Physical signs, such as knee joint swelling, joint-line tenderness or locking, were not observed during the final follow-up evaluation. Satisfactory clinical outcomes were noted postoperatively at a mean of 9 months (range 3–12 months). The mean Lysholm score was 88.9 (range 77–95) before ACL reconstruction, which improved to 97.7 (range 93–100) at the final follow-up examination (P = 0.004). No significant difference was observed in the median Tegner activity scale score.
MRI-based measurement of the MM
Flexion angle of 10°
The MML decreased from 42.8 ± 3.7 to 42.5 ± 3.8 mm after ACL reconstruction (n.s.; Table 2). The MMH decreased from 5.7 ± 0.7 to 5.5 ± 0.7 mm (n.s.), the MPBW from 14.1 ± 2.0 to 13.9 ± 1.8 mm (n.s.), the M-FCW from 10.9 ± 2.0 to 10.2 ± 1.6 mm (n.s.) and the %M-FCW (M-FCW/MPBW × 100) from 78.0 ± 9.3 to 73.9 ± 10.4%, postoperatively (n.s.). The PTFD changed from 3.7 ± 2.4 to 3.7 ± 1.4 mm (n.s.). No significant differences were found.
Flexion angle of 90°
The MML decreased from 43.7 ± 4.5 to 41.4 ± 4.5 mm after ACL reconstruction (P < 0.001; Table 3). The MMH decreased from 7.5 ± 1.4 to 6.9 ± 1.4 mm (P = 0.006), the MPBW from 13.1 ± 2.0 to 12.2 ± 1.9 mm (P < 0.001), the M-FCW from 10.0 ± 1.5 to 8.5 ± 1.5 mm (P < 0.001) and the %M-FCW (M-FCW/MPBW × 100) from 76.9 ± 8.7 to 69.5 ± 8.1%, postoperatively (P < 0.001). The PTFD increased from 2.1 ± 2.8 to 2.7 ± 2.4 mm (P = 0.015). The differences were significant for all parameters.
At both 10° and 90° of knee flexion, the upper surface of the MM posterior segment was in contact with the medial posterior condyle of the femur preoperatively (Fig. 3a, b). At 10° of knee flexion, anterior tibial translation was unchanged after ACL reconstruction; similarly, not much change was observed in the morphology of the MM posterior segment (Fig. 3c). At 90° of knee flexion, however, ACL reconstruction reduced anterior tibial translation of the ACL-deficient knees. The PTFD was also reduced, and the compressed shape of the MM posterior segment showed improvement (Fig. 3d).
Medial meniscal position on MRI. A 19-year-old woman with Judo-induced ACL injury. Preoperative sagittal images of the MM at knee flexion angles of 10° (a) and 90° (b). Postoperative sagittal images of the MM at knee flexion angles of 10° (c) and 90° (d). Inlets denote enlarged images of the MM posterior segment (b, d); dashed lines, posterior margins of the tibia; double-headed arrows, PTFD
Discussion
The most important finding of the present study was that ACL reconstruction improved the anterior shifting of the tibia at 90° of knee flexion, suggesting the possibility that stress on the MM posterior segment was reduced. In knees with ACL failure, anterior tibial translation reportedly causes secondary injury to the posterior segment of the MM [2]. Thompson et al. and Yao et al. reported that movement of the meniscus backward during knee flexion is the least in the MM posterior segment [27, 29]. Moreover, compared with the extended position, in the deep flexion position of the knee joint, the contact area of the femoral tibial joint is reduced by 75% and the contact percentage between the meniscus and the femoral condyle is increased [29]. Allen et al. [2] reported that when a 134 N anterior load was applied to ACL-deficient knees, the resultant force on the MM increased by 52% in the full extension position and 197% at 60° flexion compared with healthy knees. Hence, the meniscus plays a vital role in load transmission in a flexed position and the MM posterior segment is more susceptible to injury in knees with chronic ACL failure. In this study, the MM posterior segment morphology and anterior tibial translation position before and after ACL reconstruction showed no significant difference at 10° of knee flexion. On the other hand, at 90° of knee flexion, a more anterior position of the tibia, a greater surface area of contact between the MM posterior segment and the femoral condyle was observed, as well as a larger MM posterior segment before ACL reconstruction. These results show that in knees with ACL failure, the MM posterior segment is compressed to the medial femoral posterior condyle and shows posterior shifting due to abnormal anterior tibial translation at 90° of knee flexion, which in turn leads to the MM stretching in the posterior and superoinferior direction (Fig. 4a). A greater area of contact between the MM and the femoral condyle would reduce the contact pressure in the meniscus. However, we consider that an excessive contact pressure in the MM posterior segment at 90° of knee flexion may not be fully released by an increase in contact area between the MM and the femoral condyle in the ACL-deficient knee.
Schematic illustrations of the MM posterior segment at 90° of knee flexion. a The ACL-deficient knee. The MM posterior segment compresses to the medial femoral condyle. Excessive anterior translation force to the tibia (red arrows). b The ACL-reconstructed knee. The ACL reconstruction restores the positional relationship between the femur and tibia, and the compressed shape of the MM posterior segment is improved. Dashed lines denote the posterior tibial margins
Meniscus-to-femoral condyle congruity is essential for the development of circumferential hoop stresses and meniscal function. Abnormalities in the position of the MM and its coverage, such as a meniscal root tear, substantial meniscal extrusion and meniscectomy-related meniscal defects, can alter knee joint congruity and are associated with the progression of tibiofemoral OA and cartilage degradation [3, 16, 22]. Thompson et al. [27] studied the anteroposterior translation of the anterior and posterior segments of the medial and lateral menisci captured with 1.5T MRI at 0° to 90° of flexion in five knees from fresh cadavers without weighting. They reported that the anterior and posterior segments of the MM had 7.0 and 3.2 mm of posterior shifting, respectively. Vedi et al. [28] used 0.5 T open MRI to study the dynamics of the anterior and posterior segments of the medial and lateral menisci in 16 footballers and reported that the anterior segment and posterior segments had 5.4 and 3.8 mm of posterior shifting, respectively, in a non-weighted position. In our study, the MML before ACL reconstruction increased by 0.9 mm, and after ACL reconstruction, it decreased by 1.1 mm from 10° to 90° of knee flexion. Thus, ACL reconstruction reduces deformation of the MM posterior segment and normalizes flexion-related MML changes by suppressing abnormal anterior tibial translation (Fig. 4a, b). Moreover, the morphology of the MM posterior segment in the flexion position of knees with ACL failure suggests increased contact pressure between the femoral condyle and the MM posterior segment, which may result in MM injury secondary to chronic ACL failure. On the other hand, it is considered that ACL reconstruction surgically removes excessive stress on the posterior segment of MM in knee-flexed position, thereby maintaining the structure and function of the MM and reducing the risk of developing knee OA. Surgeons should know that ACL reconstruction should not only improve knee instability, but also be a necessary treatment to protect MM.
This study had several limitations. The MRI-based medial meniscal size and tibial position were evaluated at knee flexion angles of 10° and 90° under non-weight-bearing conditions with a 4-mm slice thickness. Thus, a comparison of the real function of the MM in ACL-deficient and ACL-reconstructed knees using thin slices, at various knee flexion angles, and under a loading condition is necessary. Three-dimensional reconstruction of the MM using dynamic MRI may be useful to understand postoperative MM position and morphology changes. In this study, pre- and postoperative measurements were as similar as possible, but not necessarily identical. In addition, tears of the posterior horn of the MM may be underdiagnosed by intraoperative assessments that only use an anterolateral portal during ACL reconstruction [21].
Conclusions
In conclusion, this study, using open MRI, has shown that ACL reconstruction results in a decreased anterior tibial translation at 90° knee flexion and in the deference of MM morphology. ACL reconstruction possibly reduces the load on the MM posterior segment and prevents secondary injury to the MM posterior segment by suppressing anterior tibial translation at 90° knee flexion.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- MM:
-
Medial meniscus
- MML:
-
Medial meniscal length
- MMH:
-
Medial meniscal height
- MPBW:
-
Medial meniscal posterior body width
- M-FCW:
-
Medial meniscus–femoral condyle contact width
- PTFD:
-
Posterior tibiofemoral distance
- OA:
-
Osteoarthritis
- MRI:
-
Magnetic resonance imaging
- TR:
-
Repetition time
- TE:
-
Echo time
- ICC:
-
Intraclass correlation coefficient
References
Aït Si Selmi T, Fithian D, Neyret P (2006) The evolution of osteoarthritis in 103 patients with ACL reconstruction at 17 years follow-up. Knee 13:353–358
Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL (2000) Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res 18:109–115
Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonté F, Beaudoin G, Bloch DA, Choquette D, Haraoui B, Altman RD, Hochberg M, Meyer JM, Cline GA, Pelletier JP (2005) Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis 64:556–563
Bylski-Austrow DI, Ciarelli MJ, Kayner DC, Matthews LS, Goldstein SA (1994) Displacements of the menisci under joint load: an in vitro study in human knees. J Biomech 27:421–431
Fujii M, Furumatsu T, Miyazawa S, Okada Y, Tanaka T, Ozaki T, Abe N (2015) Intercondylar notch size influences cyclops formation after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 23:1092–1099
Furumatsu T, Fujii M, Tanaka T, Miyazawa S, Ozaki T (2015) The figure-of-nine leg position for anatomic anterior cruciate ligament reconstruction. Orthop Traumatol Surg Res 101:391–393
Furumatsu T, Miyazawa S, Tanaka T, Okada Y, Fujii M, Ozaki T (2014) Postoperative change in medial meniscal length in concurrent all-inside meniscus repair with anterior cruciate ligament reconstruction. Int Orthop 38:1393–1399
Hagino T, Ochiai S, Senga S, Yamashita T, Wako M, Ando T, Haro H (2015) Meniscal tears associated with anterior cruciate ligament injury. Arch Orthop Trauma Surg 135:1701–1706
Hooper GJ (1986) Radiological assessment of anterior cruciate ligament deficiency. A new technique. J Bone Joint Surg Br 68:292–296
Kluczynski MA, Marzo JM, Bisson LJ (2013) Factors associated with meniscal tears and chondral lesions in patients undergoing anterior cruciate ligament reconstruction: a prospective study. Am J Sports Med 41:2759–2765
Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C (2008) Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med 36:1275–1282
Leiter JR, Gourlay R, McRae S, de Korompay N, MacDonald PB (2014) Long-term follow-up of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc 22:1061–1069
Levy IM, Torzilli PA, Warren RF (1982) The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am 64:883–888
Lorbach O, Kieb M, Domnick C, Herbort M, Weyers I, Raschke M, Engelhardt M (2015) Biomechanical evaluation of knee kinematics after anatomic single- and anatomic double-bundle ACL reconstructions with medial meniscal repair. Knee Surg Sports Traumatol Arthrosc 23:2734–2741
Louboutin H, Debarge R, Richou J, Selmi TA, Donell ST, Neyret P, Dubrana F (2009) Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee 16:239–244
Mills PM, Wang Y, Cicuttini FM, Stoffel K, Stachowiak GW, Podsiadlo P, Lloyd DG (2008) Tibio-femoral cartilage defects 3–5 years following arthroscopic partial medial meniscectomy. Osteoarthr Cartil 16:1526–1531
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38:1591–1597
Narazaki S, Furumatsu T, Tanaka T, Fujii M, Miyazawa S, Inoue H, Shimamura Y, Saiga K, Ozaki T (2015) Postoperative change in the length and extrusion of the medial meniscus after anterior cruciate ligament reconstruction. Int Orthop 39:2481–2487
Neyret P, Donell ST, Dejour H (1993) Results of partial meniscectomy related to the state of the anterior cruciate ligament. Review at 20 to 35 years. J Bone Joint Surg Br 75:36–40
Parsons EM, Gee AO, Spiekerman C, Cavanagh PR (2015) The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med 43:669–674
Peltier A, Lording TD, Lustig S, Servien E, Maubisson L, Neyret P (2015) Posteromedial meniscal tears may be missed during anterior cruciate ligament reconstruction. Arthroscopy 31:691–698
Petersen W, Forkel P, Feucht MJ, Zantop T, Imhoff AB, Brucker PU (2014) Posterior root tear of the medial and lateral meniscus. Arch Orthop Trauma Surg 134:237–255
Seon JK, Gadikota HR, KozanekM OhLS, Gill TJ, Li G (2009) The effect of anterior cruciate ligament reconstruction on kinematics of the knee with combined anterior cruciate ligament injury and subtotal medial meniscectomy: an in vitro robotic investigation. Arthroscopy 25:123–130
Sri-Ram K, Salmon LJ, Pinczewski LA, Roe JP (2013) The incidence of secondary pathology after anterior cruciate ligament rupture in 5086 patients requiring ligament reconstruction. Bone Joint J 95:59–64
Tampere T, Van Hoof T, Cromheecke M, Van der BH, Chahla J, Verdonk P, Victor J (2017) The anterior cruciate ligament: a study on its bony and soft tissue anatomy using novel 3D CT technology. Knee Surg Sports Traumatol Arthrosc 25:236–244
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Thompson WO, Thaete FL, Fu FH, Dye SF (1991) Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med 19:210–216
Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM (1999) Meniscal movement. An in vivo study using dynamic MRI. J Bone Joint Surg Br 81:37–41
Yao J, Lancianese SL, Hovinga KR, Lee J, Lerner AL (2008) Magnetic resonance image analysis of meniscal translation and tibio-menisco-femoral contact in deep knee flexion. J Orthop Res 26:673–684
Author information
Authors and Affiliations
Contributions
HI, MF, YK and TO performed the MRI-based measurements. TF and SM performed the surgery. TF designed this study. HI and TF prepared the manuscript, tables and figures. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interests to declare.
Funding
No funding was required.
Ethical approval
Ethical approval for this study was obtained from Institutional Review Board of Okayama University Graduate School (1857).
Rights and permissions
About this article
Cite this article
Inoue, H., Furumatsu, T., Miyazawa, S. et al. Improvement in the medial meniscus posterior shift following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 26, 434–441 (2018). https://doi.org/10.1007/s00167-017-4729-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4729-x