Abstract
Until recently, PET was regarded as a luxurious way of performing myocardial perfusion scintigraphy, with excellent image quality and diagnostic capabilities that hardly justified the additional cost and procedural effort. Quantitative perfusion PET was considered a major improvement over standard qualitative imaging, because it allows the measurement of parameters not otherwise available, but for many years its use was confined to academic and research settings. In recent years, however, several factors have contributed to the renewal of interest in quantitative perfusion PET, which has become a much more readily accessible technique due to progress in hardware and the availability of dedicated and user-friendly platforms and programs. In spite of this evolution and of the growing evidence that quantitative perfusion PET can play a role in the clinical setting, there are not yet clear indications for its clinical use. Therefore, the Cardiovascular Committee of the European Association of Nuclear Medicine, starting from the experience of its members, decided to examine the current literature on quantitative perfusion PET to (1) evaluate the rationale for its clinical use, (2) identify the main methodological requirements, (3) identify the remaining technical difficulties, (4) define the most reliable interpretation criteria, and finally (5) tentatively delineate currently acceptable and possibly appropriate clinical indications. The present position paper must be considered as a starting point aiming to promote a wider use of quantitative perfusion PET and to encourage the conception and execution of the studies needed to definitely establish its role in clinical practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Clinical interest in myocardial perfusion PET has increased over the years. The widespread implementation of PET scanners for oncological indications has refuelled interest in cardiac indications. In addition there is a large body of evidence that shows the clinical value of PET-derived quantitative measurements such as myocardial blood flow (MBF) and coronary flow reserve (CFR). The aim of this narrative review was to define better the role of quantitative myocardial perfusion PET in current clinical practice, and to make suggestions for its correct execution, interpretation and reporting.
Historical perspective
In the history of PET applications, cardiology and neurology preceded oncology for clinical implementation. As early as the late 1980s the use of perfusion and metabolic PET, the latter performed with 18F-FDG, was the most established modality for the detection of viable hibernating myocardium [1]. At that time perfusion PET was regarded as an expensive but more accurate alternative to SPECT. Moreover, it had the advantages of reliable attenuation correction and of short acquisition protocols [2]. However, while PET in oncology grew exponentially, the use of myocardial perfusion PET remained confined to a few centres, mostly because of the need for a radiopharmaceutical department with an on-site cyclotron for radiopharmaceutical production (13N-ammonia, 15O-water and 11C-acetate) and for the very high cost of 82Rb generators. In practice and in terms of reimbursement, the well-shown advantage of higher diagnostic accuracy was not large enough to justify the effort (and expense) needed to transfer routine cardiac imaging from SPECT to PET [3].
In recent years, however, various factors, including the widespread availability of PET scanners, more frequently combined with an on-site cyclotron, the increased availability of 82Rb generators, and the expectations aroused by the development of 18F-labelled perfusion tracers, which would obviate the need for an on-site cyclotron, have renewed interest in PET in cardiology [4]. This renewed interest is supported by a large body of evidence demonstrating the advantages of performing MBF quantification, which supports its specific role mainly in complex heart diseases, for example multivessel coronary artery disease (CAD) [5].
Advantages of quantitative over qualitative PET perfusion imaging in the clinical setting
Diagnosis of coronary artery disease
PET perfusion imaging has now reached the level of evidence for class Ia recommendation in the noninvasive work-up of CAD in patients with intermediate pretest probability [6, 7]. In this context, the contribution of quantitative cardiac perfusion PET is to help define the total ischaemic burden. This is mainly relevant in identifying patients with balanced three-vessel CAD, which could be missed using relative tracer uptake only, as done with myocardial perfusion SPECT and qualitative PET imaging [8]. There are abundant data indicating that the haemodynamic relevance of an isolated coronary stenosis is not easily predictable and that there is a wide variability in perfusion abnormalities for any given stenosis pattern depending, for example, on variations in the microvascular bed [9, 10]. Various studies have demonstrated that quantitative perfusion PET provides significant added value in the evaluation of multivessel CAD [11–15]. Usually in this setting the most apparent perfusion defect can be attributed to the “culprit” lesion. Conversely, quantitative evaluation allows correct identification of any perfusion abnormalities in the remaining coronary perfusion territories [16–18] (Fig. 1).
Myocardial perfusion PET with 13N-ammonia in a patient with severe CAD who had already undergone multiple revascularization procedures, with worsening effort angina and positive stress testing. The stress (dipyridamole) and rest images (from top to bottom: short axis, vertical long axis and horizontal long axis), and the stress (top right) and rest (middle right) polar maps show an almost normal resting perfusion with apical thinning and a limited mild perfusion defect involving the apex and the distal inferior wall. The results of perfusion quantification show normal resting MBF, but decreased maximal hyperaemic MBF in most ventricular segments, with a corresponding abnormal CFR (<2) in all three coronary artery territories. On coronary angiography, the right coronary artery was found to be suboccluded, the left anterior descending artery had a 60 % stenosis and the left circumflex artery had an 80 % stenosis
By using previously identified stress MBF and CFR thresholds, Johnson et al. have been able to construct a model that offers a high diagnostic reliability for the objective assessment of CAD burden in an individual patient [16]. The possible coexistence of CAD and coronary microvascular dysfunction (CMD) must be taken into account, and this may limit the specificity of quantitative PET for multivessel epicardial lesions as compared to a pure morphological reference standard [7, 15, 17, 18] (Fig. 2). On the other hand, the persistence of an abnormal CFR after coronary revascularization implies an unfavourable outcome, demonstrating the prognostic role of CMD in patients with CAD [19]. In addition, the presence of CMD is also one of the reasons for the frequent disagreement between the intracoronary derived CFR and fractional flow reserve (FFR) [17]. In contrast, additional signs on PET, such as transient left ventricular dilation or a decrease in left ventricular ejection fraction after stress, may help differentiate between three-vessel CAD and diffuse CMD [20].
Myocardial perfusion PET with 13N-ammonia in a patient with a history of previous radiotherapy and chemotherapy for lymphoma with mediastinal involvement, now reporting effort dyspnoea. Same image disposition as in Fig. 1. There is apparently normal perfusion both under stress and at rest. The results of perfusion quantification show normal resting MBF, but severely and diffusely decreased maximal hyperaemic MBF (<1.3 mL/min/g), with a corresponding severely abnormal CFR (<1.5) in all three coronary artery territories. Coronary CT angiography was then performed to differentiate between extensive CAD and CMD, and showed severe three-vessel disease
Quantitative perfusion PET has been used to detect preclinical CAD and to classify the degree of response to risk factor correction, for instance through life-style changes or drug therapy. Many of these studies have focused on the demonstration of endothelium-related abnormalities in MBF and CFR elicited by means of the cold pressor test (CPT) [21]. In theory, the detection of an anomalous response to either the CPT or to maximal pharmacological vasodilation, which is the standard stress modality for PET studies, could play a role in guiding primary prevention of CAD [18, 22]. The list of conditions in which abnormal quantitative PET findings have been demonstrated is very long [21]. Because perfusion abnormalities precede other signs of atherosclerosis, the demonstration of an effective reduction in the level of risk factors by means of life-style changes and/or therapeutic intervention could be of major value, but large-scale clinical studies are still lacking [21]. Quantitative perfusion PET has been demonstrated to be advantageous for the following clinical indications:
-
1.
Atherosclerotic cardiac disease including CAD
-
(a)
Detection of preclinical disease
-
(b)
Definition of the total ischaemic burden
-
(c)
Detection of balanced three-vessel CAD
-
(d)
Prognostic stratification
-
(a)
-
2.
Non-atherosclerotic cardiac diseases
-
(a)
Detection of coronary microvascular dysfunction
-
Hypertrophic cardiomyopathy
-
Fabry-Anderson disease
-
Amyloidosis
-
-
(b)
Prognostic stratification
-
Dilated cardiomyopathy
-
Hypertrophic cardiomyopathy
-
-
(a)
Prognosis
Using the traditional visual (semiquantitative) interpretation, PET has been found to be superior to SPECT for establishing the prognosis, even in patients with a normal perfusion pattern on 201Tl and 99mTc-sestamibi scans [23, 24]. ECG gating of the PET acquisition further improves the prognostic capabilities of PET imaging [25]. MBF and CFR measured during the CPT have been shown to have prognostic implications [26]. More importantly, it has been convincingly demonstrated that MBF and CFR assessed during maximal pharmacological vasodilation have remarkable prognostic relevance [27–35]. Quantitative PET is also able to evaluate the relationship between CFR and left ventricular ejection fraction after myocardial infarction [36]. Most recently, two studies have shown that the adverse prognostic value of an impaired CFR is independent of the angiographic extent and severity of CAD [37, 38]. Therefore the physiological consequences of coronary stenoses, and not just their anatomical features, should be the considered in patient management and in therapeutic decision-making [17]. Unfortunately, no prospective trials demonstrating the real value of a (quantitative) PET-guided revascularization strategy have yet been performed and published.
Other cardiac diseases
Another major contribution of quantitative myocardial PET is to allow CMD detection in various conditions beyond CAD (listed in section Diagnosis of coronary artery disease). The main application of CMD assessment is in patients with cardiomyopathies, mainly hypertrophic cardiomyopathy (HCM). Here, CMD is responsible for the frequently reported anginal symptoms and has been demonstrated to be a powerful prognostic factor [39–42]. In patients with dilated cardiomyopathy, the severity of CMD similarly plays a prognostic role [43]. In a recent study, the adverse prognostic value of an abnormal CFR has been confirmed in patients with dilated cardiomyopathy independently of its origin, ischaemic or non-ischaemic [44]. Also in patients with Fabry-Anderson disease, CMD is frequently encountered and implies more severe heart involvement [45]. Lately, CMD has been found in patients with cardiac amyloidosis, explaining the symptoms of effort angina and dyspnoea in these patients [46].
Technical requirements and clinical protocols
Quantitative myocardial perfusion PET requires the highest technical standard. In this section the issues that are specific to quantitative studies are emphasized.
PET scanner
In PET the current state-of-the-art is a PET/CT scanner with three-dimensional (3-D) acquisition capabilities. Quantitative perfusion PET needs a dynamic acquisition starting with injection of the radiopharmaceutical. The high amounts of radioactivity can cause difficulties to older bismuth germanate (BSO) scanners. Here, either improved electronics or two-dimensional (2-D) imaging (septa in) should be performed in order to avoid the unwanted increase in randoms and scattered events together with dead-time related problems [47]. For the last difficulty, it is also possible to slow the rising time of the input curve and the related sampling frequency without impairing the quality of the quantitative assessment [48]. Indeed, the use of older devices, including 2-D scanners with line source attenuation correction, is still regarded as acceptable for cardiac studies, but, in quantitative PET, might have a major effect on MBF measurements [49].
Because of the limited thickness of the ventricular wall, high spatial resolution is required, and thus the use of iterative and resolution recovery algorithms, which is nowadays the standard for most PET scanners, appears most reasonable. However, various problems specifically related to the use of iterative methods, resolution recovery algorithms and time-of-flight (TOF) correction in the setting of quantitative PET have been reported [50–56]. For instance, three recent studies showed differences ranging from 5 % to almost 20 % in rest and stress MBF when 3-D ordered subsets expectation maximization (OSEM) and TOF plus point spread function modelling reconstructions were compared [57–59]. On the other hand, TOF has been shown to significantly improve image quality and intraobserver and interobserver reproducibility of 13N-ammonia PET [59]. Further studies are warranted to define the real impact of these factors on the clinical reliability of PET measurements.
Radiopharmaceuticals
15O-Water
A diffusible, inert tracer such as 15O-water is ideal for perfusion quantification, and indeed, because of the lack of persistent uptake in the myocardium and very short half-life (125 s), it can exclusively be used for measurement of MBF [60, 61]. Although the use of factor analysis allows identification of the heart and definition of volumes of interest (VOI) without the need for an additional blood pool scan, no true morphological images are available and gated PET studies are highly demanding [18, 62]. Apart from the high extraction fraction, the other main advantage of 15O-water in the clinical setting is the ability to perform a tight time schedule and the effectiveness of MBF quantification, as demonstrated by a wide experience in a few selected centres, mainly in combination with coronary CT angiography (CCTA) by means of hybrid imaging [63] (Fig. 3; Table 1).
Fused 15O-water PET and coronary CT angiography in a 47-year-old man with multiple risk factors, atypical left hand pain during exertion and ischaemic ECG changes. CT reconstructions show significant stenoses in the left anterior descending and left circumflex arteries. The right coronary artery shows no stenosis. Stress myocardial perfusion is reduced (blue) in the areas supplied by the left anterior descending and left circumflex arteries. Image courtesy of Prof. J. Knuuti, MD, PhD, Turku, Finland
13N-Ammonia
13N-Ammonia also requires an on-site cyclotron, but its production is easier than that of 15O-water. Because of its longer half-life (9.96 min), the time schedule for a complete rest–stress study is slightly longer than with 15O-water [60]. Owing to the good myocardial uptake, high-quality images can be obtained and gated PET is feasible with good results, although the delay in the acquisition with respect to stress is slightly longer than with 82Rb [18, 60, 64]. The extraction fraction is quite high (80 % at rest) and even though a limited roll-off phenomenon at high MBF might theoretically affect the analysis, several published studies have demonstrated the feasibility and reliability of MBF quantification using 13N-ammonia [65–68] (Table 1).
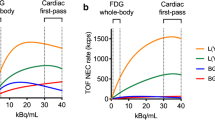
82Rubidium
The main advantage of 82Rb is that it is a generator-produced tracer with an established clinical track record [18, 60, 64]. Image quality is lower than with 13N-ammonia due the wide positron range [60]. Because of the lower extraction fraction (65 % at rest) and the ensuing roll-off phenomenon, 82Rb is not ideal for MBF quantification [18, 60]. Nevertheless, quite reliable methods have been developed to use this tracer for MBF quantification [69–71]. However, the reproducibility of MBF measurements appears lower than those with 15O-water and 13N-ammonia [18]. Additional specific problems of quantitative PET must be kept in mind, such as infusion rate capabilities of the generator, their changes related to the generator’s life time, dose balance to avoid saturation and dead-time losses during the dynamic phase without impairing the quality of later frames [64, 72–74]. Moreover, 82Rb is the only radionuclide used for perfusion PET for which the presence of prompt gammas have some relevance, with possible increases in dead-time, particularly in 3-D imaging [75]. Prompt gamma correction can improve qualitative 82Rb perfusion PET, but its importance in quantitative PET has not been established [76] (Table 1).
Examination procedure
Generally, the acquisition of a quantitative PET study does not greatly differ from that of a standard qualitative cardiac PET scan.
Patient preparation
The patient should abstain from caffeine-containing food and drinks for at least 12 h and should have fasted overnight or for at least 6 h. Washout of cardioeffective drugs should be considered in selected cases, according to the study indications and the advice of the referring cardiologist. Theophylline-containing medications must be stopped at least 48 h before the scan.
Rest and stress study
Using the currently available PET perfusion tracers the entire study (rest and stress) can be completed during one single session, with the standard approach to perform the rest study first [64]. However, various data suggest that stress MBF could be effective for ruling out CAD without the need for CFR assessment and thus for resting MBF, so the execution of stress-only scans could be considered, at least in selected patients [12, 77, 78]. The main drawback of this approach is the required immediate processing of the stress study in order to decide on the subsequent strategy. The time needed for this could interfere with patient throughput, and this delay could be longer if quantitative measurements are obtained. In the future, the use of 18F-flurpiridaz or other fluorinated compounds, which require a longer interval between the two studies, might make the stress-first (and possibly stress-only) approach much more reasonable [60].
To quantify MBF various framing schemes (i.e. number and duration) have been proposed for the dynamic acquisition. Predefined frames are now less frequently used, whilst postprocessing of list-mode acquisitions is most likely the best choice [64, 78]. Ultimately, the number and duration of frames should be based on the software and model that will be used for MBF quantification. By definition, in case of quantitative perfusion PET, the patient must be injected inside the scanner and thus pharmacological testing with coronary vasodilators is probably the only appropriate option. The only type of stress that mimics some kind of physical stimulation is the CPT, which has been reported to cause endothelium-dependent MBF activation [27]. However, despite several interesting reports of its value, the CPT is not yet widely used in clinical routine.
Traditionally, as with SPECT MPI, dipyridamole and adenosine are clinically the most used pharmacological stressors for quantitative perfusion PET. Most recently, the use of regadenoson has been reported for PET imaging, where it offers particular advantages of improved applicability and practicability, mainly with regard to the time line of application, compared to the two “traditional” stressors [79–81]. However, the delay in radiopharmaceutical injection after administration of regadenoson could affect the degree of hyperaemia achievable, although the clinical consequences of these differences are uncertain [82, 83].
Combination with ECG-gated PET
The acquisition of ECG-gated PET images with 15O-water PET is technically very challenging and only very limited data are available yet on this subject. Most likely extrapolation of these data to clinical practice will take some time. However, acquisition of gated PET images with the other perfusion tracers is readily available. In order to combine the dynamic study needed for MBF and the gated acquisition, it is better to perform a list-mode acquisition. The data can later be properly rebinned to obtain the two datasets. Alternatively, in the case of 13N-ammonia the dynamic acquisition can be followed by a second gated acquisition. With 82Rb, due to its very short half-life, this option might require a second tracer injection [64]. The reliability of gated PET measurements as compared to measurements with other established modalities and the role of functional changes between the rest and stress studies for diagnosis and prognosis have been convincingly demonstrated [20, 84].
Hybrid imaging
Because of the widespread availability of PET combined with fully diagnostic CT scanners, it is also reasonable to consider the possibility of hybrid imaging for quantitative PET. With regard to the combination of diagnostic CT and cardiac PET, either for coronary calcium scoring or for CCTA, there are no specific technical problems related to the choice of performing quantitative PET. Indeed, there are some very interesting reports on the reliability of such a hybrid solution in the case of 15O-water PET [63]. This approach, however, requires a state-of-the-art CT scanner with at least 64 slices, increases the radiation burden and prolongs the PET/CT scanner occupation time [64]. On the other hand, off-line image fusion may be an interesting alternative. The combination of qualitative myocardial perfusion and CCTA has been suggested for optimal identification of the vascular territories in the individual patient, but most recently the true diagnostic impact of this procedure has been questioned [85, 86]. On the other hand, most interesting results have been reported using the combination of CCTA with MBF parametric images, which have so far mainly been developed for 15O-water, so that the real effect on perfusion of each obstruction can be assessed. Nevertheless, the possibility of obtaining these parametric images has recently also been demonstrated for 13N-ammonia (Fig. 4) [63, 87].
Off-line fusion of 13NH3 PET and coronary CT angiography in the patient described in Fig. 2. In the left panel the standard stress 13NH3 uptake image shows a limited perfusion defect in the distal left anterior descending artery territory in spite of multiple obstructions in both the left anterior descending and the left circumflex arteries (arrows). However, as shown in the right panel, using parametric 13NH3 MBF images, a severe diffuse reduction in maximal MBF is demonstrated in almost the whole anterolateral wall (orange-yellow maximum of the image scale, set to 1.5 mL/min/g)
Sources of error
Attenuation correction
Attenuation correction itself can cause artefacts if not properly performed, and therefore the possibility of differences between emission images acquired during normal breathing and CT should be taken into account [73, 88–90]. The possibility of minor misalignment should always be considered even in the absence of overt patient motion. Whilst CT provides a “frozen” image of a specific phase of breathing, PET data are acquired during the full cycle of normal respiratory motion [73]. The evaluation of minor differences between CT and PET images can be particularly challenging in dynamic studies, because of the poor quality of PET images.
Patient motion
Ensuring that the patient is in the most comfortable position possible during cardiac PET should avoid motion affecting the acquisition, particularly because the patient should have arms above the head during the acquisition. Patient motion, particularly irregular breathing, may affect the frame sequence from which the time–activity curves will be extracted. The patient should therefore be requested to breathe normally and not to speak during the few minutes of the dynamic phase. Respiratory gating is desirable and respiratory correction from dynamic data has recently been reported, but this is so far not yet routinely implemented in cardiac studies [91, 92]. It is thus important to have the option to correct the position of abnormal frame(s) before proceeding with MBF measurements [73].
Cardiac contraction
As already mentioned, gating of dynamic sequences is currently not possible. Moreover, the possible adverse influence on the noise ratio of reducing the counts of every single time-frame by splitting it according to the cardiac cycle should be considered. However, myocardial contraction remains a major limitation in optimizing the spatial resolution of cardiac studies [93].
Image processing and MBF measurement
Image reconstruction
Because high resolution is needed, in general the most advanced reconstruction methods are desirable. The main issues related to the relationship between the reconstruction procedure and the subsequent MBF quantification are dealt with above. A thorough examination of many of these problems with the main focus on 82Rb has recently been published [49]. In the clinical practice of quantitative PET, these issues must be kept in mind in order to choose the best possible compromise given the characteristics of the scanner used.
Processing software
PET scanner vendors are becoming aware of the potential importance of cardiac PET. As a consequence, dedicated processing packages are now available, sometimes associated with additional costs [94]. Some of these packages include the same capabilities as SPECT cameras, with qualitative perfusion analysis, possibly offering comparison with a normal database, and gated image quantification, including ventricular volumes and ejection fractions. Other packages, however, already consider the possibility of performing MBF measurements [94]. Alternatively, various platforms are available for off-line processing of dynamic studies, usually exported as DICOM files [94].
Image preparation
Before processing, some programs allow correction for patient motion affecting the frame sequence. These platforms and the programs already implemented in the scanner software usually allow reorientation of the heart along its axes, and identification of the right and left ventricular VOIs and the myocardial VOI from which the tracer time-activity curves will be extracted. With most programs an automatic procedure is available, with some degree of operator interaction to correct for reorientation and VOI definition mistakes.
Compartmental models
There are different approaches to MBF quantification, mainly based on compartmental models of tracer kinetics [95]. They are generally based on the fitting of the time–activity curves to derive the parameters for the input function and for the myocardial tracer uptake. These parameters will afterwards be included in the equation of the selected model to derive the kinetic parameter that best depicts MBF. Various correction factors are usually considered, for example for activity spill-over from blood into the myocardium, as well as for partial volume effect and system resolution [96–98].
Several studies have demonstrated a high intraobserver and interobserver reproducibility of quantitative PET [99–108]. Other studies have compared the reliability of the different models used for quantification of MBF, and have shown different degrees of agreement, and that there are methodological inequalities that must be taken into account if the results from different laboratories have to be compared [95, 109–117]. In general, however, the reproducibility of MBF calculated using the same model but different platforms is good-to-excellent [112, 114, 115, 117]. Moreover, CFR is often more reliable for comparisons because, as the ratio between stress and rest MBF, it is less affected by possible differences between platforms [116, 118]. Most importantly, there is a wide consensus that PET measurements are quite robust and compare well with other quantitative parameters in terms of test–retest variability [17].
Interpretation and reporting of results
Which parameters should be considered?
The parameters that can be derived from quantitative PET are resting and maximal MBF and their ratio, usually identified as CFR or MBF reserve. These parameters are generally calculated for the whole left ventricular myocardium and usually for the coronary territories and/or the ventricular walls. In studies performed with 15O-water, anatomical images are not available, but can be derived from MBF parametric images. Conversely, both 13N-ammonia and 82Rb allow direct visual evaluation of perfusion images and their qualitative assessment [119]. A semiautomatic procedure based on comparison with a normal database can sometimes be used [120]. Additionally, gated PET can be analysed by means of various programs, mostly those already extensively employed for gated SPECT [20, 31, 84].
Which criteria should be applied?
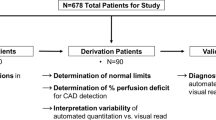
In the literature a wide array of criteria have been proposed for classifying quantitative perfusion PET results as normal or abnormal. The tracer used is the main variable. Furthermore, in order to obtain a correct CFR value, it is important to correct the baseline MBF for the resting rate pressure product, which can sometimes be abnormally high, for instance in anxious subjects [121]. With 15O-water previous studies have shown that a CFR threshold of 2.5 is the most effective for identifying patients with CAD defined as lumen narrowing of >50 % on coronary angiography plus FFR <0.8 [63, 104]. However, more recent studies have suggested that stress MBF can be as effective as CFR for detecting CAD (and possibly more effective), with the potential advantage with high values of making the resting study unnecessary [77, 122]. In a large study to identify the best possible thresholds, a stress MBF cut-off of 2.3 mL/min/g had a diagnostic accuracy of 86 % at the per-patient level and 85 % at the per-vessel level, and in the same population a CFR cut-off of 2.5 had a diagnostic accuracy of 78 % at the per-patient level and 81 % at the per-vessel level [77]. Moreover, MBF parametric images produced with 15O-water have been used to examine the possibility of assessing the difference in MBF between the endocardial and epicardial layers [123]. The transmural perfusion gradient has not so far been shown to add significantly to the diagnostic performance of quantitative PET [124]. However, this particular approach could become of increasing importance in other conditions in which MBF is impaired because of CMD, in particular HCM [87, 125].
For 13N-ammonia, the first proposed thresholds were 1.52 mL/min/g for stress MBF and 2.74 for CFR, with a slight superiority of the latter for detecting a significant coronary stenosis [126]. Later, different thresholds were proposed (1.85 mL/min/g for stress MBF and 2 for CFR), but in this study, stress MBF appeared more effective than CFR [12]. The CFR threshold of 2 was later confirmed in another study [13]. A lower threshold of 1.44 has also been proposed for CFR, but this was based on a different approach to MBF quantification using a graphic method [109, 127].
Surprisingly, for the most used perfusion tracer, 82Rb, the thresholds are less well defined. Anagnostopoulos et al. suggested 1.7 for CFR and 1.4 mL/min/g for stress MBF as possible thresholds for differentiating patients with >50 % stenosis on coronary angiography [128]. More recently, in a very large patient population, Johnson et al. identified a similar threshold for CFR (1.74), but a very low stress MBF threshold (0.91 mL/min/g) for identifying patients with ischaemia as defined by typical angina or diagnostic electrocardiographic changes during dipyridamole infusion [16].
No data on the clinical reliability of 18F-flurpiridaz for MBF quantification have been published as this tracer has not yet been clinically approved. However, the feasibility of quantitative perfusion imaging with this radiotracer has been demonstrated [129].
Indications for PET perfusion imaging
So far there are no specific guidelines for the use of quantitative PET. The current guidelines of ACC/AHA/ASNC for the use of radionuclide imaging suggest the use of PET as an alternative to SPECT, without mentioning the role of quantitative PET [6]. Even in guidelines on advanced imaging, the specific role of quantitative PET is only mentioned in passing [130]. Similarly, the more recent appropriateness guidelines suggest equality between PET and SPECT in the context of (qualitative) MPI [131]. The Japanese guidelines on cardiac nuclear medicine mention the value of quantitative PET for assessing the severity of ischaemia and CMD, and for detecting preclinical disease and determining treatment effects [132]. In Europe, the possible role of PET, but not specifically of quantitative PET, has been explored more recently in the setting of hybrid imaging [133, 134], and finally considered specifically for risk stratification in stable coronary disease [135]. Similarly, PET is broadly reported as an alternative to other noninvasive techniques in the European guidelines on coronary revascularization [136].
Therefore any attempt to present clinical indications for quantitative perfusion PET remains somehow arbitrary and is open to criticism. Nevertheless, given the accumulated evidence of the added value of MBF and CFR over standard visual evaluation of PET images, it seems reasonable to define some specific clinical scenarios in which the use of quantitative PET appears most valuable. In addition, the use of PET is associated with a lower radiation burden than other diagnostic modalities such as SPECT and CCTA, and fulfils the current necessity for dose reduction [4, 137–143]. Thus, independently of quantification, myocardial PET perfusion is preferred in younger patients, and especially women.
Diagnosis, assessment and prognostication of CAD
For diagnostic purposes, MPI is in general indicated only in patents with intermediate pretest probability of CAD. In this scenario, however, particularly when there are reasons to suspect multivessel disease, the use of quantitative PET would be advantageous. Quantitative PET can be used to establish the diagnosis and simultaneously define the total ischaemic burden, thereby better stratifying patients for coronary revascularization [7, 17].
The practical usefulness of the detection of abnormalities in MBF as a sign of preclinical atherosclerosis in patients with low pretest probability has not yet been demonstrated. More realistically, the use of quantitative PET could be considered in the increasing number of patients in whom the results of CCTA, or even those of intracoronary angiography (ICA), are inconclusive because of the presence of intermediate lesions or of other signs suggestive of atherosclerosis [7, 144, 145]. Similarly, in patients without significant coronary lesions but with anginal symptoms, the use of quantitative PET would be reasonable to evaluate the haemodynamic consequences of minimal obstructions or to make a diagnosis of CMD [146]. Patients with known anomalous coronary artery anatomy, fistulas or bridging, especially patients with chest pain, are a particular group eligible for quantitative myocardial perfusion PET [147, 148].
Although in general imaging for risk-stratifying patients is underutilized, the excellent prognostic value of quantitative perfusion PET-derived parameters make it an ideal tool for this purpose.
Use of quantitative PET in other heart diseases
A completely normal quantitative perfusion PET scan would reasonably exclude the presence of haemodynamically significant CAD in patients with anginal chest pain but with possible non-atherosclerotic heart disease. Much more importantly, there is enough evidence to emphasize the importance of an accurate assessment of MBF for identifying the presence of CMD in patients with cardiomyopathies, in particular HCM [41]. Less certain, but undoubtedly promising, is the use of quantitative PET for the assessment of therapeutic responses in these patients [18, 149].
Quantitative PET in comparison with other imaging modalities
The general advantages of PET as compared to SPECT have already been mentioned, and MBF quantification is one of the most important. However, the new gamma cameras with cadmium-zinc-telluride (CZT) technology could potentially be used in quantitative assessment even with single-photon tracers, although there is as yet no definitive demonstration of their reliability [150]. The differences between the physiological approach to CAD as compared to the anatomical one based on CCTA or ICA have also been described [17]. The measurement of FFR during ICA can certainly improve the evaluation of the haemodynamic significance of any single obstruction, but there remain important differences between this approach and CFR calculation [17]. There have also been attempts to add flow measurement capabilities to CCTA, but they are still in the developmental phase, and have the additional problems of the radiation burden and contrast medium-related concerns [151]. Possibly more promising, because no ionizing radiation is used, is the measurement of MBF by means of magnetic resonance imaging (MRI) [152]. Good correlations between MRI PET measurements have been reported [127]. However, the possible concerns about paramagnetic contrast media and the contraindications to MRI in cardiac patients with implanted devices must be taken into account [153]. Finally, the availability of dedicated MRI scanners with appropriate software and adequately trained personnel is relatively limited.
Future perspectives
Together with further improvements in PET technology such as solid-state scanners, improved gating capabilities and implementation of advanced reconstruction algorithms, the imminent availability of the 18F-labelled tracer 18F-flurpiridaz is the most exciting development in quantitative perfusion PET [60]. However, this anticipated advance should not prevent the use of quantitative PET wherever possible. In particular, in centres that have already made the great investment necessary for changing to 82Rb PET for a large part of their MPI routine should consider performing MBF quantification in at least all patients with the indications listed above. Similarly, all groups with an on-site cyclotron, particularly if some initial experience with 13N-ammonia qualitative PET is available, should also be encouraged to perform quantitative PET. Because of its more demanding methodology it is less likely that new centres will consider performing 15O-water studies.
In recent years, radiopharmaceutical production systems that deliver a single patient dose of a few PET radioisotopes and biomarkers have been developed. Due to their small footprint and self-shielding, these “baby cyclotron” systems offer the advantage of being easily incorporated into an existing clinical setting, just close to, for example, a PET scanner. At present, the only featured target is 18O, thus leading to a unique 18O(p,n)18F nuclear reaction, and the production cycle of a single dose of 18F takes no less than 35 min. Because of the limited beam current (<5 μA), and the suboptimal peak proton energy (7.5 MeV), the 9.96 min decay half-life of 13N would make the 16O(p,α)13N reaction practically unfeasible. The only exception to this rule seems to be a 13N-only dedicated superconducting mini-cyclotron system (Ionetix ION-12sc). However, because of the declared technical characteristics (as low as 10 μA beam current and 12 MeV peak proton energy, while the major reaction efficiency for 13N production is at 8 MeV), and the absence of scientific papers demonstrating its capabilities, there are major doubts as to the reliability of such a system.
In such a scenario of augmented awareness of the merits of quantitative perfusion PET and of increasing confidence in its feasibility, the effective introduction of an 18F-labelled radiopharmaceutical would permit quantitative PET imaging to be performed in all patients in whom this technology could have major clinical benefit. In turn this would probably further encourage the vendors to implement the platforms and programs needed for MBF measurement, making their use much easier for the clinician. An increasing number of patients could be studied with exercise qualitative PET, a modality so far never utilized and in which the impossibility of MBF quantification could be at least partly compensated for by the more physiological stimulation of the coronary reserve. However, what still remains to be accomplished is the planning and execution of dedicated trials that would finally define the clinical role of quantitative perfusion PET as a specific imaging modality.
References
Tillisch J, Brunken R, Marshall R, Schwaiger M, Mandelkern M, Phelps M, et al. Reversibility of cardiac wall-motion abnormalities predicted by positron tomography. N Engl J Med. 1986;314:884–8.
Stewart RE, Schwaiger M, Molina E, Popma J, Gacioch GM, Kalus M, et al. Comparison of rubidium-82 positron emission tomography and thallium-201 SPECT imaging for detection of coronary artery disease. Am J Cardiol. 1991;67:1303–10.
Bateman TM. Advantages and disadvantages of PET and SPECT in a busy clinical practice. J Nucl Cardiol. 2012;19:S3–11.
Beanlands R, Heller GV. Proceedings of the ASNC Cardiac PET Summit, 12 May 2014, Baltimore, MD: 1: the value of PET: integrating cardiovascular PET into the care continuum. J Nucl Cardiol. 2015;22:557–62.
Bateman TM, Lance Gould K, Di Carli MF. Proceedings of the Cardiac PET Summit, 12 May 2014, Baltimore, MD: 3: quantification of myocardial blood flow. J Nucl Cardiol. 2015;22:571–8.
Klocke FJ, Baird MG, Lorell BH, Bateman TM, Messer JV, Berman DS, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging – executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging). Circulation. 2003;108:1404–18.
Cremer P, Hachamovitch R, Tamarappoo B. Clinical decision making with myocardial perfusion imaging in patients with known or suspected coronary artery disease. Semin Nucl Med. 2014;44:320–9.
Beller GA. Underestimation of coronary artery disease with SPECT perfusion imaging. J Nucl Cardiol. 2008;15:151–3.
Di Carli M, Czernin J, Hoh CK, Gerbaudo VH, Brunken RC, Huang SC, et al. Relation among stenosis severity, myocardial blood flow, and flow reserve in patients with coronary artery disease. Circulation. 1995;91:1944–51.
Gould KL. Does coronary flow trump coronary anatomy? JACC Cardiovasc Imaging. 2009;2:1009–23.
Parkash R, deKemp RA, Ruddy TD, Kitsikis A, Hart R, Beauchesne L, et al. Potential utility of rubidium 82 PET quantification in patients with 3-vessel coronary artery disease. J Nucl Cardiol. 2004;11:440–9.
Hajjiri MM, Leavitt MB, Zheng H, Spooner AE, Fischman AJ, Gewirtz H. Comparison of positron emission tomography measurement of adenosine-stimulated absolute myocardial blood flow versus relative myocardial tracer content for physiological assessment of coronary artery stenosis severity and location. JACC Cardiovasc Imaging. 2009;2:751–8.
Fiechter M, Ghadri JR, Gebhard C, Fuchs TA, Pazhenkottil AP, Nkoulou RN, et al. Diagnostic value of 13N-ammonia myocardial perfusion PET: added value of myocardial flow reserve. J Nucl Med. 2012;53:1230–4.
Ziadi MC, Dekemp RA, Williams K, Guo A, Renaud JM, Chow BJ, et al. Does quantification of myocardial flow reserve using rubidium-82 positron emission tomography facilitate detection of multivessel coronary artery disease? J Nucl Cardiol. 2012;19:670–80.
Naya M, Murthy VL, Taqueti VR, Foster CR, Klein J, Garber M, et al. Preserved coronary flow reserve effectively excludes high-risk coronary artery disease on angiography. J Nucl Med. 2014;55:248–55.
Johnson NP, Gould KL. Physiological basis for angina and ST-segment change PET-verified thresholds of quantitative stress myocardial perfusion and coronary flow reserve. JACC Cardiovasc Imaging. 2011;4:990–8.
Gould KL, Johnson NP, Bateman TM, Beanlands RS, Bengel FM, Bober R, et al. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol. 2013;62:1639–53.
Schindler TH, Quercioli A, Valenta I, Ambrosio G, Wahl RL, Dilsizian V. Quantitative assessment of myocardial blood flow – clinical and research applications. Semin Nucl Med. 2014;44:274–93.
Slart RH, Zeebregts CJ, Hillege HL, de Sutter J, Dierckx RA, van Veldhuisen DJ, et al. Myocardial perfusion reserve after a PET-driven revascularization procedure: a strong prognostic factor. J Nucl Med. 2011;52:873–9.
Dorbala S, Di Carli MF. Cardiac PET perfusion: prognosis, risk stratification, and clinical management. Semin Nucl Med. 2014;44:344–57.
Murthy VL, Di Carli MF. Non-invasive quantification of coronary vascular dysfunction for diagnosis and management of coronary artery disease. J Nucl Cardiol. 2012;19:1060–72.
Pearson TA. New tools for coronary risk assessment: what are their advantages and limitations? Circulation. 2002;105:886–92.
MacIntyre WJ, Go RT, King JL, Cook SA, Neumann DR, Saha GB, et al. Clinical outcome of cardiac patients with negative thallium-201 SPECT and positive rubidium-82 PET myocardial perfusion imaging. J Nucl Med. 1993;34:400–4.
Yoshinaga K, Chow BJ, Williams K, Chen L, deKemp RA, Garrard L, et al. What is the prognostic value of myocardial perfusion imaging using rubidium-82 positron emission tomography? J Am Coll Cardiol. 2006;48:1029–39.
Dorbala S, Hachamovitch R, Curillova Z, Thomas D, Vangala D, Kwong RY, et al. Incremental prognostic value of gated Rb-82 positron emission tomography myocardial perfusion imaging over clinical variables and rest LVEF. JACC Cardiovasc Imaging. 2009;2:846–854.
Schindler TH, Nitzsche EU, Schelbert HR, Olschewski M, Sayre J, Mix M, et al. Positron emission tomography-measured abnormal responses of myocardial blood flow to sympathetic stimulation are associated with the risk of developing cardiovascular events. J Am Coll Cardiol. 2005;45:1505–12.
Tio RA, Dabeshlim A, Siebelink HM, de Sutter J, Hillege HL, Zeebregts CJ, et al. Comparison between the prognostic value of left ventricular function and myocardial perfusion reserve in patients with ischemic heart disease. J Nucl Med. 2009;50:214–9.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography: added value of coronary flow reserve. J Am Coll Cardiol. 2009;54:150–6.
Fukushima K, Javadi MS, Higuchi T, Lautamäki R, Merrill J, Nekolla SG, et al. Prediction of short-term cardiovascular events using quantification of global myocardial flow reserve in patients referred for clinical 82Rb PET perfusion imaging. J Nucl Med. 2011;52:726–32.
Ziadi MC, deKemp RA, Williams KA, Guo A, Chow BJ, Renaud JM, et al. Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia. J Am Coll Cardiol. 2011;58:740–8.
Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Di Carli G, et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation. 2011;124:2215–24.
Murthy VL, Naya M, Foster CR, Gaber M, Hainer J, Klein J, et al. Association between coronary vascular dysfunction and cardiac mortality in patients with and without diabetes mellitus. Circulation. 2012;126:1858–68.
Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Dorbala S, et al. Coronary vascular dysfunction and prognosis in patients with chronic kidney disease. JACC Cardiovasc Imaging. 2012;5:1025–34.
Farhad H, Dunet V, Bachelard K, Allenbach G, Kaufmann PA, Prior JO. Added prognostic value of myocardial blood flow quantification in rubidium-82 positron emission tomography imaging. Eur Heart J Cardiovasc Imaging. 2013;14:1203–10.
Mc Ardle BA, Davies RA, Chen L, Small GR, Ruddy TD, Dwivedi G, et al. Prognostic value of rubidium-82 positron emission tomography in patients after heart transplant. Circ Cardiovasc Imaging. 2014;7:930–7.
Juárez-Orozco LE, Glauche J, Alexanderson E, Zeebregts CJ, Boersma HH, Glaudemans AW, et al. Myocardial perfusion reserve in spared myocardium: correlation with infarct size and left ventricular ejection fraction. Eur J Nucl Med Mol Imaging. 2013;40:1148–54.
Taqueti VR, Everett BM, Murthy VL, Gaber M, Foster CR, Hainer J, et al. Interaction of impaired coronary flow reserve and cardiomyocyte injury on adverse cardiovascular outcomes in patients without overt coronary artery disease. Circulation. 2015;131:528–35.
Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J, et al. Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation. 2015;131:19–27.
Camici P, Chiriatti G, Lorenzoni R, Bellina RC, Gistri R, Italiani G, et al. Coronary vasodilation is impaired in both hypertrophied and nonhypertrophied myocardium of patients with hypertrophic cardiomyopathy: a study with nitrogen-13 ammonia and positron emission tomography. J Am Coll Cardiol. 1991;17:879–86.
Cecchi F, Sgalambro A, Baldi M, Sotgia B, Antoniucci D, Camici PG, et al. Microvascular dysfunction, myocardial ischemia, and progression to heart failure in patients with hypertrophic cardiomyopathy. J Cardiovasc Transl Res. 2009;2:452–61.
Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med. 2003;349:1027–35.
Olivotto I, Cecchi F, Gistri R, Lorenzoni R, Chiriatti G, Girolami F, et al. Relevance of coronary microvascular flow impairment to long-term remodeling and systolic dysfunction in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2006;47:1043–8.
Neglia D, Michelassi C, Trivieri MG, Sambuceti G, Giorgetti A, Pratali L, et al. Prognostic role of myocardial blood flow impairment in idiopathic left ventricular dysfunction. Circulation. 2002;105:186–93.
Majmudar MD, Murthy VL, Shah RV, Kolli S, Mousavi N, Foster CR, et al. Quantification of coronary flow reserve in patients with ischaemic and non-ischaemic cardiomyopathy and its association with clinical outcomes. Eur Heart J Cardiovasc Imaging. 2015;16:900–9.
Tomberli B, Cecchi F, Sciagrà R, Berti V, Lisi F, Torricelli F, et al. Coronary microvascular dysfunction is an early feature of cardiac involvement in patients with Anderson-Fabry disease. Eur J Heart Fail. 2013;15:1363–73.
Dorbala S, Vangala D, Bruyere Jr J, Quarta C, Kruger J, Padera R, et al. Coronary microvascular dysfunction is related to abnormalities in myocardial structure and function in cardiac amyloidosis. JACC Heart Fail. 2014;2:358–67.
Votaw JR, White M. Comparison of 2-dimensional and 3-dimensional cardiac Rb-82 PET studies. J Nucl Med. 2001;42:701–6.
Raylman RR, Caraher JM, Hutchins GD. Sampling requirements for dynamic cardiac PET studies using image-derived input functions. J Nucl Med. 1993;34:440–7.
Moody JB, Lee BC, Corbett JR, Ficaro EP, Murthy VL. Precision and accuracy of clinical quantification of myocardial blood flow by dynamic PET: a technical perspective. J Nucl Cardiol. 2015;22:935–51.
Chen GP, Branch KR, Alessio AM, Pham P, Tabibiazar R, Kinahan P, et al. Effect of reconstruction algorithms on myocardial blood flow measurement with 13N-ammonia PET. J Nucl Med. 2007;48:1259–65.
Van Velden FHP, Kloet RW, van Berckel BNM, Lammertsma AA, Boellaard R. Accuracy of 3-dimensional reconstruction algorithms for the high-resolution research tomograph. J Nucl Med. 2009;50:72–80.
Walker MD, Asselin M-C, Julyan PJ, Feldmann M, Talbot PS, Jones T, et al. Bias in iterative reconstruction of low-statistics PET data: benefits of a resolution model. Phys Med Biol. 2011;56:931–49.
Rahmim A, Qi J, Sossi V. Resolution modeling in PET imaging: theory, practice, benefits, and pitfalls. Med Phys. 2013;40:064301.
Tong S, Alessio AM, Thielemans K, Stearns C, Ross S, Kinahan PE. Properties and mitigation of edge artifacts in PSF-based PET reconstruction. IEEE Trans Nucl Sci. 2011;58:2264–75.
Karp JS, Surti S, Daube-Witherspoon ME, Muehllehner G. Benefit of time-of-flight in PET: experimental and clinical results. J Nucl Med. 2008;49:462–70.
Westerwoudt V, Conti M, Eriksson L. Advantages of improved time resolution for TOF PET at very low statistics. IEEE Trans Nucl Sci. 2014;61:126–33.
Presotto L, Busnardo E, Bettinardi V, Landoni C, Todeschini P, Rimoldi O, et al. Evaluation of time of flight (TOF) and point spread function (PSF) reconstructions in the quantification of myocardial blood flow with 13N ammonia and PET: Comparison among reconstructions (reprojection, OSEM), software (PMOD and CARIMAS) and operators. Nuclear Science Symposium and Medical Imaging Conference (NSS/MIC), 2012 IEEE. p. 3979–82.
Armstrong IS, Tonge CM, Arumugam P. Impact of point spread function modeling and time-of-flight on myocardial blood flow and myocardial flow reserve measurements for rubidium-82 cardiac PET. J Nucl Cardiol. 2014;21:467–74.
Tomiyama T, Ishihara K, Suda M, Kanaya K, Sakurai M, Takahashi N, et al. Impact of time-of-flight on qualitative and quantitative analyses of myocardial perfusion PET studies using 13N-ammonia. J Nucl Cardiol. 2015;22:998–1007.
Maddahi J, Packard RRS. Cardiac PET perfusion tracers: current status and future directions. Semin Nucl Med. 2014;44:333–43.
Bergmann SR, Fox KA, Rand AL, McElvany KD, Welch MJ, Markham J, et al. Quantification of regional myocardial blood flow in vivo with H215O. Circulation. 1984;70:724–33.
Hermansen F, Ashburner J, Spinks TJ, Kooner JS, Camici PG, Lammertsma AA. Generation of myocardial factor images directly from the dynamic oxygen-15-water scan without use of an oxygen-15-carbon monoxide blood-pool scan. J Nucl Med. 1998;39:1696–702.
Kajander S, Joutsiniemi E, Saraste M, Pietila M, Ukkonen H, Saraste A, et al. Cardiac positron emission tomography/computed tomography imaging accurately detects anatomically and functionally significant coronary artery disease. Circulation. 2010;122:603–13.
Di Carli MF, Dorbala S, Meserve J, El Fakhri G, Sitek A, Moore SC. Clinical myocardial perfusion PET/CT. J Nucl Med. 2007;48:783–93.
Krivokapich J, Smith GT, Huang SC, Hoffman EJ, Ratib O, Phelps ME, et al. 13N ammonia myocardial imaging at rest and with exercise in normal volunteers: quantification of absolute myocardial perfusion with dynamic positron emission tomography. Circulation. 1989;80:1328–37.
Muzik O, Beanlands RS, Hutchins GD, Manger TJ, Nguyen N, Schwaiger M. Validation of nitrogen-13-ammonia tracer kinetic model for quantification of myocardial blood flow using PET. J Nucl Med. 1993;34:83–91.
DeGrado TR, Hanson MW, Turkington TG, Delong DM, Brezinski DA, Vallée JP, et al. Estimation of myocardial blood flow for longitudinal studies with 13N-labeled ammonia and positron emission tomography. J Nucl Cardiol. 1996;3:494–507.
Hutchins GD, Schwaiger M, Rosenspire KC, Krivokapich J, Schelbert H, Kuhl DE. Noninvasive quantification of regional blood flow in the human heart using N-13 ammonia and dynamic positron emission tomographic imaging. J Am Coll Cardiol. 1990;15:1032–42.
Herrero P, Markham J, Shelton ME, Weinheimer CJ, Bergmann SR. Noninvasive quantification of regional myocardial perfusion with rubidium-82 and positron emission tomography: exploration of a mathematical model. Circulation. 1990;82:1377–86.
El Fakhri G, Sitek A, Guerin B, Kijewski MF, Di Carli MF, Moore SC. Quantitative dynamic cardiac 82Rb PET using generalized factor and compartment analyses. J Nucl Med. 2005;46:1264–71.
Lortie M, Beanlands RSB, Yoshinaga K, Klein R, DaSilva JN, deKemp RA. Quantification of myocardial blood flow with 82Rb dynamic PET imaging. Eur J Nucl Med Mol Imaging. 2007;34:1765–74.
Klein R, Adler A, Beanlands RS, deKemp RA. Precision-controlled elution of a 82Sr/82Rb generator for cardiac perfusion imaging with positron emission tomography. Phys Med Biol. 2007;52:659–73.
Klein R, Beanlands RS, deKemp RA. Quantification of myocardial blood flow and flow reserve: technical aspects. J Nucl Cardiol. 2010;17:555–70.
Tout D, Tonge C, Muthu S, Arumugam P. Assessment of a protocol for routine simultaneous myocardial blood flow measurement and standard myocardial perfusion imaging with rubidium-82 on a high count rate positron emission tomography system. Nucl Med Commun. 2012;33:1202–11.
Martin CC, Christian BT, Satter MR, Nickerson LDH, Nickles RJ. Quantitative PET with positron emitters that emit prompt gamma rays. IEEE Trans Med Imaging. 1995;14:681–7.
Esteves FP, Nye JA, Khan A, Folks RD, Halkar RK, Garcia EV, et al. Prompt-gamma compensation in Rb-82 myocardial perfusion 3D PET/CT. J Nucl Cardiol. 2010;17:247–53.
Danad I, Uusitalo V, Kero T, Saraste A, Raijmakers PG, Lammertsma AA, et al. Quantitative assessment of myocardial perfusion in the detection of significant coronary artery disease: cutoff values and diagnostic accuracy of quantitative [15O]H2O PET imaging. J Am Coll Cardiol. 2014;64:1464–75.
Schindler TH, Dilsizian V. PET-determined hyperemic myocardial blood flow: further progress to clinical application. J Am Coll Cardiol. 2014;64:1476–8.
Goudarzi B, Fukushima K, Bravo P, Merrill J, Bengel FM. Comparison of the myocardial blood flow response to regadenoson and dipyridamole: a quantitative analysis in patients referred for clinical 82Rb myocardial perfusion PET. Eur J Nucl Med Mol Imaging. 2011;38:1908–16.
Hsiao E, Ali B, Blankstein R, Skali H, Ali T, Bruyere Jr J, et al. Detection of obstructive coronary artery disease using regadenoson stress and 82Rb PET/CT myocardial perfusion imaging. J Nucl Med. 2013;54:1748–54.
Cullom SJ, Case JA, Courter SA, McGhie AI, Bateman TM. Regadenoson pharmacologic rubidium-82 PET: a comparison of quantitative perfusion and function to dipyridamole. J Nucl Cardiol. 2013;20:76–83.
Johnson NP, Gould KL. Regadenoson versus dipyridamole hyperemia for cardiac PET imaging. JACC Cardiovasc Imaging. 2015;8:438–47.
Sinusas AJ. Does a shortened hyperemia with regadenoson stress pose a concern for quantitative Rb-82 PET imaging? Optimization of regadenoson PET imaging. JACC Cardiovasc Imaging. 2015;8:448–50.
Dorbala S, Vangala D, Sampson U, Limaye A, Kwong R, Di Carli MF. Value of vasodilator left ventricular ejection fraction reserve in evaluating the magnitude of myocardium at risk and the extent of angiographic coronary artery disease: a 82Rb PET/CT study. J Nucl Med. 2007;48:349–58.
Javadi MS, Lautamaki R, Merrill J, Voicu C, Epley W, McBride G, et al. Definition of vascular territories on myocardial perfusion images by integration with true coronary anatomy: a hybrid PET/CT analysis. J Nucl Med. 2010;51:198–203.
Thomassen A, Petersen H, Johansen A, Braad PE, Diederichsen AC, Mickley H, et al. Quantitative myocardial perfusion by O-15-water PET: individualized vs. standardized vascular territories. Eur Heart J Cardiovasc Imaging. 2015;16:970–6.
Sciagrà R, Passeri A, Cipollini F, Castagnoli H, Olivotto I, Burger C, et al. Validation of pixel-wise parametric mapping of myocardial blood flow with (13)NH3 PET in patients with hypertrophic cardiomyopathy. Eur J Nucl Med Mol Imaging. 2015;42:1581–8.
Gould KL, Pan T, Loghin C, Johnson NP, Guha A, Sdringola S. Frequent diagnostic errors in cardiac PET/CT due to misregistration of CT attenuation and emission PET images: a definitive analysis of causes, consequences, and corrections. J Nucl Med. 2007;48:1112–21.
Martinez-Moller A, Souvatzoglou M, Navab N, Schwaiger M, Nekolla SG. Artifacts from misaligned CT in cardiac perfusion PET/CT studies: frequency, effects, and potential solutions. J Nucl Med. 2007;48:188–93.
Lautamaki R, Brown TL, Merrill J, Bengel FM. CT-based attenuation correction in (82)Rb-myocardial perfusion PET-CT: incidence of misalignment and effect on regional tracer distribution. Eur J Nucl Med Mol Imaging. 2008;35:305–10.
Livieratos L, Rajappan K, Stegger L, Schafers K, Bailey DL, Camici PG. Respiratory gating of cardiac PET data in list-mode acquisition. Eur J Nucl Med Mol Imaging. 2006;33:584–8.
Schleyer PJ, Thielemans K, Marsden PK. Extracting a respiratory signal from raw dynamic PET data that contain tracer kinetics. Phys Med Biol. 2014;59:4345–56.
Garcia EV. Proceedings of the Cardiac PET Summit Meeting 12 May 2014: Cardiac PET and SPECT instrumentation. J Nucl Cardiol. 2015;22:563–70.
Saraste A, Kajander S, Han C, Nesterov SV, Knuuti J. PET: is myocardial flow quantification a clinical reality? J Nucl Cardiol. 2012;19:1044–59.
Choi Y, Huang SC, Hawkins RA, Kim JY, Kim BT, Hoh CK, et al. Quantification of myocardial blood flow using 13N-ammonia and PET: comparison of tracer models. J Nucl Med. 1999;40:1045–55.
Hoffman EJ, Huang SC, Plummer D, Phelps ME. Quantification in positron emission tomography: 6. Effect of nonuniform resolution. J Comput Assist Tomogr. 1982;6:987–99.
Hove JD, Gambhir SS, Kofoed KF, Freiberg J, Kelbaek H. Quantification of the regional blood flow in the interventricular septum using positron emission tomography and nitrogen-13 ammonia. Eur J Nucl Med Mol Imaging. 2003;30:109–16.
Hutchins GD, Caraher JM, Raylman RR. A region of interest strategy for minimizing resolution distortions in quantitative myocardial PET studies. J Nucl Med. 1992;33:1243–50.
Sawada S, Muzik O, Beanlands RS, Wolfe E, Hutchins GD, Schwaiger M. Interobserver and interstudy variability of myocardial blood flow and flow-reserve measurements with nitrogen 13 ammonia-labeled positron emission tomography. J Nucl Cardiol. 1995;2:413–22.
Nagamachi S, Czernin J, Kim AS, Sun KT, Böttcher M, Phelps ME, et al. Reproducibility of measurements of regional resting and hyperemic myocardial blood flow assessed with PET. J Nucl Med. 1996;37:1626–31.
Kaufmann PA, Gnecchi-Ruscone T, Yap JT, Rimoldi O, Camici PG. Assessment of the reproducibility of baseline and hyperemic myocardial blood flow measurements with 15O-labeled water and PET. J Nucl Med. 1999;40:1848–56.
Jagathesan R, Kaufmann PA, Rosen SD, Rimoldi OE, Turkeimer F, Foale R, et al. Assessment of the long-term reproducibility of baseline and dobutamine-induced myocardial blood flow in patients with stable coronary artery disease. J Nucl Med. 2005;46:212–9.
Knešaurek K, Machac J, Zhang Z. Repeatability of regional myocardial blood flow calculation in 82Rb PET imaging. BMC Med Phys. 2009;9:2.
Nesterov SV, Han C, Mäki M, Kajander S, Naum AG, Helenius H, et al. Myocardial perfusion quantification with 15O-labeled water PET: high reproducibility of the new cardiac analysis software (CarimasTM). Eur J Nucl Med Mol Imaging. 2009;36:1594–602.
El Fakhri G, Kardan A, Sitek A, Dorbala S, Abi-Hatem N, Lahoud Y, et al. Reproducibility and accuracy of quantitative myocardial blood flow assessment with 82Rb PET: comparison with 13N-ammonia PET. J Nucl Med. 2009;50:1062–71.
Manabe O, Yoshinaga K, Katoh C, Naya M, deKemp RA, Tamaki N. Repeatability of rest and hyperemic myocardial blood flow measurements with 82Rb dynamic PET. J Nucl Med. 2009;50:68–71.
Klein R, Renaud JM, Ziadi MC, Thorn SL, Adler A, Beanlands RS, et al. Intra- and inter-operator repeatability of myocardial blood flow and myocardial flow reserve measurements using rubidium-82 PET and a highly automated analysis program. J Nucl Cardiol. 2010;17:600–16.
Efseaff M, Klein R, Ziadi MC, Beanlands RS, deKemp RA. Short-term repeatability of resting myocardial blood flow measurements using rubidium-82 PET imaging. J Nucl Cardiol. 2012;19:997–1006.
Choi Y, Huang SC, Hawkins RA, Kim JY, Kim BT, Hoh CK, et al. A simplified method for quantification of myocardial blood flow using nitrogen-13-ammonia and dynamic PET. J Nucl Med. 1993;34:488–97.
Coxson PG, Huesman RH, Borland L. Consequences of using a simplified kinetic model for dynamic PET data. J Nucl Med. 1997;38:660–7.
Slomka PJ, Alexanderson E, Jácome R, Jiménez M, Romero E, Meave A, et al. Comparison of clinical tools for measurements of regional stress and rest myocardial blood flow assessed with 13N-ammonia PET/CT. J Nucl Med. 2012;53:171–81.
deKemp RA, Declerck J, Klein R, Pan X-B, Nakazato R, Tonge C, et al. Multisoftware reproducibility study of stress and rest myocardial blood flow assessed with 3D dynamic PET/CT and a 1-tissue-compartment model of 82Rb kinetics. J Nucl Med. 2013;54:571–7.
Tahari AK, Lee A, Rajaram M, Fukushima K, Lodge MA, Lee BC, et al. Absolute myocardial flow quantification with 82Rb PET/CT: comparison of different software packages and methods. Eur J Nucl Med Mol Imaging. 2014;41:126–35.
Nesterov SV, Deshayes E, Sciagrà R, Settimo L, Declerck JM, Pan X-B, et al. Quantification of myocardial blood flow in absolute terms using 82Rb PET imaging: results of RUBY-10 study. JACC Cardiovasc Imaging. 2014;7:1119–27.
Harms HJ, Nesterov SV, Han C, Danad I, Leonora R, Raijmakers PG, et al. Comparison of clinical non-commercial tools for automated quantification of myocardial blood flow using oxygen-15-labelled water PET/CT. Eur Heart J Cardiovasc Imaging. 2014;15:431–41.
Sunderland JJ, Pan X-B, Declerck J, Menda Y. Dependency of cardiac rubidium-82 imaging quantitative measures on age, gender, vascular territory, and software in a cardiovascular normal population. J Nucl Cardiol. 2015;22:72–84.
Dunet V, Klein R, Allenbach G, Renaud J, deKemp RA, Prior JO. Myocardial blood flow quantification by Rb-82 cardiac PET/CT: a detailed reproducibility study between two semi-automatic analysis programs. J Nucl Cardiol. 2015. doi:10.1007/s12350-015-0151-2
Bateman TM, Case JA. Variability in normal myocardial blood flow measurements: physiologic, methodologic, or protocol related? J Nucl Cardiol. 2015;22:85–8.
Sampson UK, Dorbala S, Limaye A, Kwong R, Di Carli MF. Diagnostic accuracy of rubidium-82 myocardial perfusion imaging with hybrid positron emission tomography/computed tomography in the detection of coronary artery disease. J Am Coll Cardiol. 2007;49:1052–8.
Santana CA, Folks RD, Garcia EV, Verdes L, Sanyal R, Hainer J, et al. Quantitative 82Rb PET/CT: development and validation of myocardial perfusion database. J Nucl Med. 2007;48:1122–8.
Czernin J, Müller P, Chan S, Brunken RC, Porenta G, Krivokapich J, et al. Influence of age and hemodynamics on myocardial blood flow and flow reserve. Circulation. 1993;88:62–9.
Danad I, Raijmakers PG, Appelman YE, Harms HJ, de Haan S, van den Oever ML, et al. Hybrid imaging using quantitative H215O PET and CT-based coronary angiography for the detection of coronary artery disease. J Nucl Med. 2013;54:55–63.
Vermeltfoort IA, Raijmakers PG, Lubberink M, Germans T, van Rossum AC, Lammertsma AA, et al. Feasibility of subendocardial and subepicardial myocardial perfusion measurements in healthy normals with (15)O-labeled water and positron emission tomography. J Nucl Cardiol. 2011;18:650–6.
Danad I, Raijmakers PG, Harms HJ, Heymans MW, van Royen N, Lubberink M, et al. Impact of anatomical and functional severity of coronary atherosclerotic plaques on the transmural perfusion gradient: a [15O]H2O PET study. Eur Heart J. 2014;35:2094–105.
Knaapen P, Germans T, Camici PG, Rimoldi OE, ten Cate FJ, ten Berg JM, et al. Determinants of coronary microvascular dysfunction in symptomatic hypertrophic cardiomyopathy. Am J Physiol Heart Circ Physiol. 2008;294:H986–93.
Muzik O, Duvernoy C, Beanlands RS, Sawada S, Dayanikli F, Wolfe Jr ER, et al. Assessment of diagnostic performance of quantitative flow measurements in normal subjects and patients with angiographically documented coronary artery disease by means of nitrogen-13 ammonia and positron emission tomography. J Am Coll Cardiol. 1998;31:534–40.
Morton G, Chiribiri A, Ishida M, Hussain ST, Schuster A, Indermuehle A, et al. Quantification of absolute myocardial perfusion in patients with coronary artery disease: comparison between cardiovascular magnetic resonance and positron emission tomography. J Am Coll Cardiol. 2012;60:1546–55.
Anagnostopoulos C, Almonacid A, El Fakhri G, Curillova Z, Sitek A, Roughton M, et al. Quantitative relationship between coronary vasodilator reserve assessed by 82Rb PET imaging and coronary artery stenosis severity. Eur J Nucl Med Mol Imaging. 2008;35:1593–601.
Packard RR, Huang SC, Dahlbom M, Czernin J, Maddahi J. Absolute quantification of myocardial blood flow in human subjects with or without myocardial ischemia using dynamic flurpiridaz F18 PET. J Nucl Med. 2014;55:1438–44.
Beanlands RS, Chow BJ, Dick A, Friedrich MG, Gulenchyn KY, Kiess M, et al. CCS/CAR/CANM/CNCS/CanSCMR joint position statement on advanced noninvasive cardiac imaging using positron emission tomography, magnetic resonance imaging and multidetector computed tomographic angiography in the diagnosis and evaluation of ischemic heart disease – executive summary. Can J Cardiol. 2007;23:107–19.
Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. Circulation. 2009;119:e561–87.
JCS Joint Working Group. Guidelines for clinical use of cardiac nuclear medicine (JCS 2010). Digest version. Circ J. 2012;76:761–7.
Le Guludec D, Lautamäki R, Knuuti J, Bax JJ, Bengel FM, European Council of Nuclear Cardiology. Present and future of clinical cardiovascular PET imaging in Europe – a position statement by the European Council of Nuclear Cardiology (ECNC). Eur J Nucl Med Mol Imaging. 2008;35:1709–24.
Flotats A, Knuuti J, Gutberlet M, Marcassa C, Bengel FM, Kaufmann PA, et al. Hybrid cardiac imaging: SPECT/CT and PET/CT. A joint position statement by the European Association of Nuclear Medicine (EANM), the European Society of Cardiac Radiology (ESCR) and the European Council of Nuclear Cardiology (ECNC). Eur J Nucl Med Mol Imaging. 2011;38:201–12.
Acampa W, Gaemperli O, Gimelli A, Knaapen P, Schindler TH, Verberne HJ, et al. Role of risk stratification by SPECT, PET, and hybrid imaging in guiding management of stable patients with ischaemic heart disease: expert panel of the EANM cardiovascular committee and EACVI. Eur Heart J Cardiovasc Imaging. 2015;16:1289–98.
Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, et al. 2014 ESC/EACTS guidelines on myocardial revascularization. EuroIntervention. 2015;10:1024–94.
Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MJ. Radiation dose to patients from cardiac diagnostic imaging. Circulation. 2007;116:1290–305.
Achenbach S, Anders K, Kalender WA. Dual-source cardiac computed tomography: image quality and dose considerations. Eur Radiol. 2008;18:1188–98.
Cerqueira MD, Allman KC, Ficaro EP, Hansen CL, Nichols KJ, Thompson RC. Recommendations for reducing radiation exposure in myocardial perfusion imaging. J Nucl Cardiol. 2010;17:709–18.
Senthamizhchelvan S, Bravo PE, Esaias C, Lodge MA, Merrill J, Hobbs RF, et al. Human biodistribution and radiation dosimetry of 82Rb. J Nucl Med. 2010;51:1592–9.
Senthamizhchelvan S, Bravo PE, Lodge MA, Merrill J, Bengel FM, Sgouros G, et al. Radiation dosimetry of 82Rb in humans under pharmacologic stress. J Nucl Med. 2011;52:485–91.
Einstein AJ. Effects of radiation exposure from cardiac imaging: how good are the data? J Am Coll Cardiol. 2012;59:553–65.
Hunter CR, Hill J, Ziadi MC, Beanlands RSB, de Kemp RA. Biodistribution and radiation dosimetry of 82Rb at rest and during peak pharmacological stress in patients referred for myocardial perfusion imaging. Eur J Nucl Med Mol Imaging. 2015;42:1032–42.
Naya M, Murthy VL, Blankstein R, Sitek A, Hainer J, Foster C, et al. Quantitative relationship between the extent and morphology of coronary atherosclerotic plaque and downstream myocardial perfusion. J Am Coll Cardiol. 2011;58:1807–16.
Liga R, Marini C, Coceani M, Filidei E, Schlueter M, Bianchi M, et al. Structural abnormalities of the coronary arterial wall in addition to luminal narrowing affect myocardial blood flow reserve. J Nucl Med. 2011;52:1704–12.
Graf S, Khorsand A, Gwechenberger M, Schütz M, Kletter K, Sochor H, et al. Typical chest pain and normal coronary angiogram: cardiac risk factor analysis versus PET for detection of microvascular disease. J Nucl Med. 2007;48:175–81.
Coceani M, Ciardetti M, Pasanisi E, Schlueter M, Palmieri C, Neglia D, et al. Surgical correction of left coronary artery origin from the right coronary artery. Ann Thorac Surg. 2013;95:e1–2.
Said SA, Nijhuis RL, Akker JW, Takechi M, Slart RH, Bos JS, et al. Unilateral and multilateral congenital coronary-pulmonary fistulas in adults: clinical presentation, diagnostic modalities, and management with a brief review of the literature. Clin Cardiol. 2014;37:536–45.
Neglia D, De Maria R, Masi S, Gallopin M, Pisani P, Pardini S, et al. Effects of long-term treatment with carvedilol on myocardial blood flow in idiopathic dilated cardiomyopathy. Heart. 2007;93:808–13.
Ben-Haim S, Murthy VL, Breault C, Allie R, Sitek A, Roth N, et al. Quantification of myocardial perfusion reserve using dynamic SPECT imaging in humans: a feasibility study. J Nucl Med. 2013;54:873–9.
Nakauchi Y, Iwanaga Y, Ikuta S, Kudo M, Kobuke K, Murakami T, et al. Quantitative myocardial perfusion analysis using multi-row detector CT in acute myocardial infarction. Heart. 2012;98:566–72.
Lee DC, Johnson NP. Quantification of absolute myocardial blood flow by magnetic resonance perfusion imaging. JACC Cardiovasc Imaging. 2009;2:761–70.
Dill T. Contraindications to magnetic resonance imaging: non-invasive imaging. Heart. 2008;94:943–8.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
None.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Sciagrà, R., Passeri, A., Bucerius, J. et al. Clinical use of quantitative cardiac perfusion PET: rationale, modalities and possible indications. Position paper of the Cardiovascular Committee of the European Association of Nuclear Medicine (EANM). Eur J Nucl Med Mol Imaging 43, 1530–1545 (2016). https://doi.org/10.1007/s00259-016-3317-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-016-3317-5