Abstract
The continued high utilization of rest-stress single-photon emission computed tomographic (SPECT) myocardial perfusion imaging (MPI) is supported by its known clinical benefits, established reimbursement, and wide availability of cameras and radiopharmaceuticals. However, traditional rest-stress SPECT protocols tend to be lengthy and inefficient, and the prevalence of equivocal studies continues to be a problem. The use of stress-only SPECT protocols in selected patients, and a new generation of ultrafast SPECT cameras have led to improved image quality, reduced dosimetry and shorter, more efficient MPI protocols. The utilization of positron emission tomographic (PET) MPI has been accelerated by the availability of radiopharmaceuticals that can be generated on-site, and by the availability of more PET cameras. Emerging evidence consistently demonstrates that PET provides improved image quality, greater interpretive certainty, higher diagnostic accuracy, lower patient dosimetry, and shorter imaging protocols as compared to SPECT. Importantly, PET imaging allows assessment of left ventricular function at peak-stress, and evaluation of microvascular function through the measurement of absolute myocardial blood flow at rest and at peak-stress. Wider utilization of PET MPI is hindered by a high cost of entry, high on-going costs, and an immature reimbursement structure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Evolution of Myocardial Perfusion Imaging (MPI)
Radionuclide MPI is most commonly performed with a rest-stress protocol using a dual-detector Anger camera. A large body of evidence supporting the accuracy of this protocol for diagnosing coronary artery disease (CAD), for short-term risk stratification, and for triaging patient management decisions has led to its high utilization. However, the rest-stress protocol is temporally inefficient, expensive, and may expose some patients to more radiation than is necessary to assess the adequacy of myocardial perfusion. In response, the field is moving away from a one-test/one-protocol paradigm to selective testing that more carefully balances patient costs, benefits, and risks (mainly radiation exposure) required to answer the clinical questions. New single-photon emission computed tomographic (SPECT) hardware and software have been introduced that permit lower radionuclide doses, and both stress-only SPECT and myocardial perfusion PET are increasingly being used for selected patients. As such, there has been an evolution in thinking from performing the same test on all patients to a more individualized approach.
Radionuclide MPI performs best when it is used to assess patients with an intermediate (between 20% and 80%) pre-test likelihood for significant CAD. However, this large group is not as homogeneous as the term implies. It includes patients who are clinically straightforward and others who are complex due to the clinical question or the various cardiac and non-cardiac co-morbidities present. In order to refer patients for the most appropriate MPI test, it is useful to consider 3 relatively easily differentiated categories based on clinical complexity:
-
(1)
Patients with no history of CAD, who have a normal or only mildly abnormal resting ECG, who are able to exercise to a diagnostic level, and who have an intermediate-risk Duke Treadmill score, are likely to have a normal scan. Such patients are ideal candidates for stress-only SPECT imaging, optimally with low-dose radionuclide injection and with attenuation correction.
-
(2)
Patients with prior myocardial infarction and/or coronary intervention but who can still complete a diagnostic exercise stress test are more challenging. These patients are more likely to have an abnormal stress perfusion pattern. To differentiate stress-induced defects from scarred myocardium, it is most appropriate to conduct a rest/stress SPECT study.
-
(3)
The most complicated and highest-risk patients are those who require pharmacologic stress (often because of their size or other co-morbidities). These patients are also likely to have perfusion abnormalities, and are excellent candidates for PET MPI.
This testing paradigm based on patient characteristics and complexity of clinical situation (Table 1) complies well with current professional society Statements and Guidelines.1-4
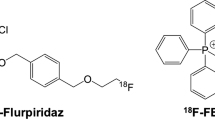
Recommendations for Reducing Radiation Exposure
It has been estimated that approximately 20% of the annual collective radiation dose received by the United States population from diagnostic procedures comes from radionuclide MPI.5 The predominant theory regarding radiation exposure is that it should be kept at the lowest amount possible because, according to the linear no-threshold concept, even the low levels associated with diagnostic testing can accumulate over a person’s lifetime and result in a higher likelihood of developing a malignancy. One recent publication estimated that as many as 7,400 additional lifetime cancers may occur based on myocardial perfusion testing frequencies observed in the US in 2008.6 In an attempt to organize the clinician’s process for selecting the most appropriate nuclear stress-imaging test, the American Society of Nuclear Cardiology released an Information Statement that considered the risk-benefit ratio of the perfusion tests currently available.3 This statement placed particular emphasis on the appropriateness of using any radionuclide imaging test, and then on selection between the various radionuclide imaging options based on their relative dosimetry. The statement proposed that if there was a suitable diagnostic test that did not expose the patient to radiation, such a test should be considered, especially for younger patients. If a radionuclide perfusion study was indicated and appropriate for a given patient, then PET perfusion imaging was suggested as a first-line option (if available). This statement is based on the lower dosimetry of nitrogen-13 (13N)-labeled ammonia and rubidium-82 (82Rb) compared to a rest/stress Tc-99m SPECT study.7,8 When PET is not available, specific SPECT protocols were suggested, favoring new instrumentation and stress-only protocols when possible (Figure 1).3
Proposed algorithm issued by ASNC for maximal reduction in patient radiation exposure. Reproduced from Springer and Cerqueira et al,3 Figure 1, Copyright 2010 Journal of Nuclear Cardiology with kind permission from Springer Science + Business Media B.V.
Stress-Only Imaging
There is now considerable data to support stress-only SPECT imaging with attenuation correction in selected patients. Duvall et al9 followed patients for up to 5 years who had a normal stress-only or a normal rest-stress SPECT study. Survival rates in both the groups were similarly very high (99.3% stress-only vs 99.2% rest-stress), suggesting that deleting rest image acquisition in this population had no adverse effect on outcomes. Likewise, Chang et al10 showed that a normal stress-only scan was associated with the same outcomes over 8 years of follow-up as did a normal rest/stress SPECT scan in men and women, in diabetics and in non-diabetics, in patients with or without prior CAD history, and in patients with a low-risk, or even an intermediate-risk, Duke Treadmill Score.
A novel approach to stress-only SPECT imaging utilizes newly introduced, highly sensitive camera systems with multiple cadmium zinc telluride detectors. As compared to Anger cameras, these systems provide high-quality images with good count statistics despite shorter acquisition times or smaller amounts of radioactive tracer. A count-rich stress image can be acquired with Tc-99m doses as low as 1-4 mCi, depending on patient size. If the stress image is abnormal, a follow-up rest dose of approximately 3 times the stress dose can be administered, and rest imaging can be completed on the same day. For lower-risk patients who can exercise, a stress-only SPECT protocol provides patients and busy clinical practices the benefits of reduced dosimetry and shorter procedures.
The advantages and disadvantages of SPECT compared to PET for radionuclide myocardial perfusion for those patients who require a full rest/stress protocol are summarized below.
Advantages and Disadvantages of Rest/Stress SPECT MPI
The many advantages of rest/stress SPECT imaging that account for its continued high utilization in busy clinical practices are summarized in Table 2. Its diagnostic accuracy, value in risk stratification, and utility in guiding patient management are well established. It is widely available, and its indications are familiar to referring physicians. Providers have access to published protocols including those for acquisition, processing, quality control, and reporting. New approaches such as stress-only imaging and PET may be perceived as professionally challenging for many providers whose formal training did not include these recent advances.
The disadvantages of traditional rest/stress SPECT are also summarized in Table 2. The typical protocol is inefficient, often taking 3 to 5 hours to complete. This limits a practice’s ability to control costs or to align costs with declining reimbursements. The supply of Tc-99m has become unreliable; some providers could not purchase any Tc-99m-labeled radiopharmaceuticals for several weeks during 2010. Unacceptably high rates of equivocal study results continue to be problematic issues for SPECT, especially when attenuation correction is not available. Finally, the correct identification of multivessel coronary disease is suboptimally low.
There have been several exciting advances in SPECT hardware and software that can now provide faster acquisitions, lower dosimetry, and improved image quality. However, these advances are expensive and are being introduced at a time of declining reimbursements and utilization. More rigorous adherence to Appropriate Use Criteria,4 now a requirement for lab accreditation, has had an impact on the volume of radionuclide perfusion imaging tests performed. Furthermore, many SPECT requisitions now need preauthorization from a radiology benefits management company that is usually incentivized to reduce the number of studies conducted, and that often uses criteria different from those published in the Appropriate Use Criteria.
Advantages and Disadvantages of Rest/Stress PET MPI
Myocardial perfusion PET imaging offers many advantages compared to SPECT (Table 3). An aging, sedentary, and obese population presents an increasing number of patients who cannot complete a diagnostic exercise stress test, necessitating a pharmacologic stress procedure. In these patients, PET offers improved image quality, greater interpretive certainty, higher diagnostic accuracy, and high laboratory throughput efficiency.11,12 The dosimetry for a rest-stress 82Rb-PET study is less than half that of a rest-stress technetium-99m scan.7,8 Supply-chain issues for PET radiopharmaceuticals have been greatly improved by onsite radionuclide availability, and more PET cameras are now available. Exciting developments include the rapidly evolving and increasingly routine measurements of left ventricular (LV) function at peak-stress and absolute myocardial blood flow.
The current disadvantages of PET in a busy clinical practice are the high cost of entry, high ongoing costs, greater challenges for preauthorization among private payers, the lack of an accommodating national coverage determination, and a limited availability of dedicated cardiac PET cameras (Table 3).
PET Versus SPECT Image Quality and Diagnostic Certainty
The differences between the quality of SPECT and PET scans are fairly striking, and represent a significant step forward in assessing and monitoring myocardial perfusion. Figure 2 shows a SPECT scan and a PET scan acquired from the same patient on sequential days. The count density and the uniformity of tracer in different areas of the myocardium are much higher in the PET scan compared to the SPECT scan. In the SPECT study, the inferior wall cannot be assessed because of considerable scatter from subdiaphragmatic structures. There is no such interference in the PET study acquired the next day. There are normalization issues seen in the SPECT scan. In addition to the higher quality, the 82Rb-PET scan was acquired in only 3.5 minutes, compared to 12 minutes for the SPECT scan.
Figure 3 illustrates another advantage of PET in addressing a fairly common problem seen when SPECT is performed using vasodilator stress. In the upper 4 rows of SPECT images, a loop of bowel containing radionuclide appears to be overlapping the inferior wall of the heart, preventing accurate interpretation of perfusion. The bowel is still visible in the lower 4 rows of PET images, but because of the better spatial resolution of PET and the reduced influence of scattered counts, the inferior wall is distinct and is easily interpreted.
This higher quality of PET images as compared to SPECT images leads to higher interpretive certainty and greater diagnostic accuracy. In the only contemporary comparison study of the accuracy of SPECT versus PET, two-patient populations matched for age, gender, body mass index, and presence and extent of CAD were imaged using either same-day rest/stress Tc-99m SPECT or same-day rest/stress 82Rb-PET.11 The population consisted of patients who completed coronary angiography (and thus had a relatively high likelihood of an abnormal study), and patients who had a low (<5%) pre-test likelihood for CAD (and thus a low likelihood of having abnormal perfusion). Expert readers blinded to patient information interpreted the scans. They rated 96% of the PET studies as definitely normal or abnormal, and only 4% as uncertain. In contrast, only 82% of SPECT studies were considered definitely normal or abnormal, and 18% fell into the equivocal or uncertain categories (Figure 4). The diagnostic accuracy of PET versus SPECT was higher overall, and also when the results were analyzed by gender and body mass index. In addition, identification of a second or third vessel supplying an area of abnormal perfusion improved from 48% with SPECT to 71% with PET. Importantly, PET outperformed SPECT even after attenuation correction was applied to the SPECT scans.
Comparison (percents of study populations) of interpretive certainty of SPECT and PET images. Note that more PET than SPECT studies were rated as normal, and that only 4% of PET studies, but 18% of the SPECT studies fell into the uncertain categories. Reproduced from Springer and Bateman et al,11 Figure 2, Copyright 2006 Journal of Nuclear Cardiology with kind permission from Springer Science + Business Media B.V.
Improved quality of PET images was also associated with increased diagnostic certainty in a study in which 96 patients with non-definitive Tc99m-SPECT perfusion scans also underwent 82Rb-PET studies within 6 months.12 Of the 96 SPECT images, quality was rated as good in only 20%, fair in 31%, and suboptimal in 49%. In contrast, 94% of the PET images in the same patients were rated as good, only 6% were fair, and there were no suboptimal PET images (Figure 5). In this challenging population, 49% of the SPECT images were classified as diagnostically uncertain but all 96 PET images were interpretable as normal or abnormal.
Image quality (percents of population) in 96 patients imaged with PET after a non-definitive SPECT study. The quality of nearly all the PET studies (94%), but only 20% of the SPECT studies, was rated as good (leftmost bars). 49% of the SPECT studies, but none of the PET studies, were rated suboptimal (rightmost bars). Reprinted from Yoshinaga et al,12 Copyright 2006, with permission from Elsevier
Clinical Information Provided by PET and SPECT
A typical rest-stress SPECT procedure takes 3 to 5 hours to complete, while a rest-stress PET study using 82Rb can be completed in 20 to 30 minutes (Figure 6). Most rest-stress SPECT protocols involve complex scheduling of radiopharmaceutical administration, application of stress, and two separate in-camera image acquisition periods. Most PET perfusion protocols follow the pattern shown in Figure 6 regardless of whether images are acquired with a dedicated PET camera or a hybrid PET/CT camera. A transmission scan (for attenuation mapping) lasting a few seconds to 2 minutes is acquired. The radiopharmaceutical is injected and a gated rest emission scan is acquired. The pharmacologic stress agent is then administered, and the procedure is repeated: a transmission scan is acquired, another dose of the radiopharmaceutical is injected, and the gated stress emission scan is acquired.
The clinical information provided by PET and SPECT myocardial perfusion studies, as typically performed, is summarized in Table 4. Both provide visual and quantitative, spatially relative perfusion at both rest and stress, and SPECT provides functional information (LV, end-systolic volume [ESV], end-diastolic volume [EDV], and ejection fraction [EF]) at rest and post-stress. But PET offers the distinct advantages of assessment of gated LV function at the peak of the stress response, as well as high-quality intrinsic attenuation correction, and the measurement of absolute global and regional myocardial blood flow at rest and at peak-stress (enabling calculation of coronary flow reserve [CFR]).
Peak-stress functional data provides prognostic information which is additive to that determined by the extent and severity of perfusion abnormality alone. In a recent study, patients who completed an 82Rb-PET perfusion scan were divided into 3 categories of perfusion defect based on summed stress scores (SSS) (0-3, 4-8, or >8) and 3 categories of peak-stress EF (>50%, 40% to 49%, or <40%). Adding peak-stress EF significantly enhanced the prognostic value of the PET scan. Annualized mortality rates for patients with lower peak-stress EFs were higher in all groups (Figure 7).13 Peak-stress myocardial function cannot be assessed with typical SPECT perfusion protocols.
Addition of peak-stress EF to myocardial perfusion provides incremental prognostic information. Annualized mortality rates in patients with peak-stress LVEF ≥ 50%, from 40% to 49%, or <40%, grouped by the severity of perfusion defect: normal perfusion (SSS = 0 to 3), moderately abnormal (SSS = 4 to 8), or severely abnormal (SSS > 8) perfusion. Reproduced from Springer and Lertsburapa et al,13 Figure 5, Copyright 2008 Journal of Nuclear Cardiology with kind permission from Springer Science + Business Media B.V.
The value of measuring CFR during PET MPI was examined in a study in which 256 patients completed a PET perfusion scan that included measurement of CFR. Patients who had either normal or abnormal PET perfusion scans were divided into groups whose coronary blood flow increased ≥2-fold (normal CFR) or increased <2-fold (abnormal CFR). The major adverse cardiac event and cardiac death rates were significantly higher in patients with abnormal CFR as early as 3 years following the PET scan, whether their PET perfusion scans were normal or abnormal (Table 5). Abnormal CFR was a strong predictor of major adverse cardiac events (MACE) and cardiac death.14 While measuring CFR with PET is not yet routine, studies to date suggest substantial promise for improving patient risk stratification.
Conclusions
At this time, rest-stress SPECT protocols continue to dominate myocardial perfusion testing, but attractive alternatives are increasingly available. These alternatives are making their way into the guidelines, but financial factors remain significant hurdles to wider availability. Stress-only SPECT protocols resulting in lower dosimetry and less time in the imaging laboratory may be appropriate for many patients. PET perfusion imaging offers indisputably better images that are characterized by higher resolution, better attenuation correction, less scatter, and better contrast. Patients are exposed to less radiation, and the PET protocols are simpler and shorter. There is consistent and growing evidence that the improved image quality seen with PET MPI leads to enhanced diagnostic certainty and accuracy. The availability of LV function measurements at peak-stress and the ability to quantitate myocardial blood flow promise to provide data that clinicians will find indispensable.
References
Klocke FJ, Baird MG, Lorell BH, Bateman TM, Messer JV, Berman DS, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging). Circulation 2003;108:1404-18.
Des Prez RD, Dahlberg ST, Einstein AJ, et al. ASNC Clinical Update. Stress-Only Myocardial Perfusion Imaging, 2009 http://www.asnc.org/imageuploads/ClinicalUpdateStressOnlyMPI2009.pdf. Accessed Jan 5, 2011.
Cerqueira MD, Allman KC, Ficaro EP, Hansen CL, Nichols KJ, Thompson RC, et al. Recommendations for reducing radiation exposure in myocardial perfusion imaging. J Nucl Cardiol 2010;17:709-18.
Hendel RC, Berman DS, DiCarli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging. J Am Coll Cardiol 2009;53:2201-29.
Mettler FA, Thomadsen BR, Bhargavan M, Gilley DB, Gray JE, Lipoti JA, et al. Medical radiation exposure in the U.S. in 2006: Preliminary results. Health Phys 2008;95:502-7.
Berrington de Gonzalez A, Kim K-P, Smith-Bindman R, McAreavey D. Myocardial perfusion scans: Projected population cancer risks from current levels of use in the United States. Circulation 2010;122:2403-10.
Stabin MG. Radiopharmaceuticals for nuclear cardiology: Radiation dosimetry, uncertainties, and risk. J Nucl Med 2008;49:1555-63.
Senthamizhchelvan S, Bravo PE, Esaias C, Lodge MA, Merrill J, Hobbs RF, et al. Human biodistribution and radiation dosimetry of 82Rb. J Nucl Med 2010;51:1592-9.
Duvall WL, Wijetunga MN, Klein TM, Razzouk L, Godbold J, Croft LB, et al. The prognosis of a normal stress-only Tc-99m myocardial perfusion imaging study. J Nucl Cardiol 2010;17:370-7.
Chang SM, Nabi F, Xu J, Raza U, Mahmarian JJ. Normal stress-only versus standard stress/rest myocardial perfusion imaging: Similar patient mortality with reduced radiation exposure. J Am Coll Cardiol 2010;55:221-30.
Bateman TM, Heller GV, McGhie AI, Friedman JD, Case JA, Bryngelson JR, et al. Diagnostic accuracy of rest/stress ECG-gated Rb-82 myocardial perfusion PET: Comparison with ECG-gated Tc-99m sestamibi SPECT. J Nucl Cardiol 2006;13:24-33.
Yoshinaga K, Chow BJW, Williams K, Chen L, deKemp RA, Garrard L, et al. What is the Prognostic value of myocardial perfusion imaging using rubidium-82 positron emission tomography? J Am Coll Cardiol 2006;48:1029-39.
Lertsburapa K, Ahlberg AW, Bateman TM, Katten D, Volker L, Cullom SJ, et al. Independent and incremental prognostic value of left ventricular ejection fraction determined by stress gated rubidium-82 PET imaging in patients with known or suspected coronary artery disease. J Nucl Cardiol 2008;15:745-53.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography: Added value of coronary flow reserve. J Am Coll Cardiol 2009;54:150-6.
Disclosure
Dr Bateman reported receiving grant support from Bracco Diagnostics, Philips Healthcare, GE Healthcare, Lantheus Medical Imaging, Astellas Pharmaceuticals, CellPoint, and SpectrumDynamics. Dr Bateman reported receiving royalties from ExSPECT II, and ImagenPro/MD/Q. Dr Bateman reported stock ownership in CVIT. Dr Bateman reported to be part of the advisory board for Bracco Diagnostics, Lantheus Medical Imaging, Spectrum Dynamics, Astellas Pharmaceuticals, and GE Healthcare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bateman, T.M. Advantages and disadvantages of PET and SPECT in a busy clinical practice. J. Nucl. Cardiol. 19 (Suppl 1), 3–11 (2012). https://doi.org/10.1007/s12350-011-9490-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-011-9490-9