Abstract
Purpose
In clinical cardiac 82Rb PET, globally impaired coronary flow reserve (CFR) is a relevant marker for predicting short-term cardiovascular events. However, there are limited data on the impact of different software and methods for estimation of myocardial blood flow (MBF) and CFR. Our objective was to compare quantitative results obtained from previously validated software tools.
Methods
We retrospectively analyzed cardiac 82Rb PET/CT data from 25 subjects (group 1, 62 ± 11 years) with low-to-intermediate probability of coronary artery disease (CAD) and 26 patients (group 2, 57 ± 10 years; P = 0.07) with known CAD. Resting and vasodilator-stress MBF and CFR were derived using three software applications: (1) Corridor4DM (4DM) based on factor analysis (FA) and kinetic modeling, (2) 4DM based on region-of-interest (ROI) and kinetic modeling, (3) MunichHeart (MH), which uses a simplified ROI-based retention model approach, and (4) FlowQuant (FQ) based on ROI and compartmental modeling with constant distribution volume.
Results
Resting and stress MBF values (in milliliters per minute per gram) derived using the different methods were significantly different: using 4DM-FA, 4DM-ROI, FQ, and MH resting MBF values were 1.47 ± 0.59, 1.16 ± 0.51, 0.91 ± 0.39, and 0.90 ± 0.44, respectively (P < 0.001), and stress MBF values were 3.05 ± 1.66, 2.26 ± 1.01, 1.90 ± 0.82, and 1.83 ± 0.81, respectively (P < 0.001). However, there were no statistically significant differences among the CFR values (2.15 ± 1.08, 2.05 ± 0.83, 2.23 ± 0.89, and 2.21 ± 0.90, respectively; P = 0.17). Regional MBF and CFR according to vascular territories showed similar results. Linear correlation coefficient for global CFR varied between 0.71 (MH vs. 4DM-ROI) and 0.90 (FQ vs. 4DM-ROI). Using a cut-off value of 2.0 for abnormal CFR, the agreement among the software programs ranged between 76 % (MH vs. FQ) and 90 % (FQ vs. 4DM-ROI). Interobserver agreement was in general excellent with all software packages.
Conclusion
Quantitative assessment of resting and stress MBF with 82Rb PET is dependent on the software and methods used, whereas CFR appears to be more comparable. Follow-up and treatment assessment should be done with the same software and method.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
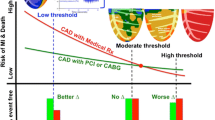
Myocardial perfusion imaging (MPI) with 82Rb chloride ECG-gated PET/CT has become an important imaging modality for the evaluation of coronary artery disease (CAD) [1–3]. As compared to conventional cardiac SPECT, it has better diagnostic quality, certainty, and accuracy [4–8]. To date, the interpretation of cardiac PET studies has relied on relative myocardial uptake and studies have been traditionally analyzed for the presence of relative regional perfusion defects, similar to cardiac SPECT [9]. However, this does not take advantage of the full potential of quantitative PET. If absolute flow is impaired globally, a comparison of the best and worst perfused regions will underestimate the severity of flow-limiting disease. This lowers the sensitivity of standard relative MPI for the detection of multivessel CAD as compared with single-vessel disease, and of diffuse disease of the microvasculature. Quantification of absolute myocardial blood flow (MBF) and coronary flow reserve (CFR) is desirable [10]. Many researchers have shown the feasibility of MBF and CFR quantification with dynamic 82Rb PET [11–16].
Evidence has accumulated supporting the prognostic value of MBF and CFR in predicting adverse cardiac outcomes [17–22]. Assessment of CFR yields independent and added prognostic information beyond relative MPI and may improve risk stratification in patients investigated for myocardial ischemia.
For the routine clinical quantification and use of MBF and CFR, robust automated quantitative tools are required. Several software packages for absolute quantification of MBF are now in existence. Each package employs different methods of segmenting the left ventricle (LV) and sampling the counts in the myocardium and blood pool to obtain time–activity curves. Only one previous study using 13N-ammonia PET has tested the variability of myocardial flow quantification among different software packages and methods [23]. However, there are no data on the impact of different software and methods for estimation of MBF and CFR using 82Rb PET.
In this study, we compared three software packages based on methodologies that have been tested and validated for the quantitative analysis of MBF and CFR with 82Rb myocardial perfusion PET: MunichHeart, Corridor4DM (4DM), and FlowQuant.
Materials and methods
Study group
Cardiac PET/CT image datasets from 51 patients referred for MPI with 82Rb PET at the Johns Hopkins Hospital for the evaluation of ischemic heart disease were included in this study. These were divided into two groups: group 1 comprised 25 subjects (8 men and 17 women, age 62 ± 11 years) with a low-to-intermediate probability (and no known history) of CAD, and group 2 comprised 26 patients with known obstructive CAD (14 men and 12 women, age 57 ± 10 years) with a previous history of percutaneous or surgical coronary revascularization.
PET/CT protocol
All imaging was performed on a 64-slice Discovery Rx VCT PET/CT scanner (GE Medical Systems, Waukesha, WI). Individuals were positioned using a scout scan, and a low-dose CT scan (120 kV, 50–100 mA) for attenuation correction of PET data was acquired during shallow breathing. Using a large intravenous line, 1,480–1,850 MBq (40–50 mCi) of 82Rb (CardioGen-82; Bracco Diagnostics) was infused at 50 mL/min over 30 s, and a list-mode 2-D PET scan was acquired for 8 min. Vasodilator stress with infusion of dipyridamole (0.56 mg/kg, 4 min) was then started after the rest acquisition, and a second dose of 1,480–1,850 MBq (40–50 mCi) of 82Rb was injected, starting 4 min after the end of the dipyridamole infusion, followed by acquisition of an 8-min list-mode PET scan. Subsequently, rest and stress PET data were aligned with the CT scan, and attenuation correction was performed [24]. The list-mode data were used to reconstruct dynamic images (32 frames for 8 min: 20 × 6 s, 5 × 12 s, 4 × 30 s, and 3 × 60 s). The images were filtered with a Butterworth filter with a cut-off at 20.1 mm. The pixel size was 3.27 mm.
Myocardial blood flow analysis
The three software tools were used to quantify global and regional MBF values in milliliters per minute per gram for all 51 PET/CT rest/stress studies. CFR, as the ratio of global stress to resting MBF, was determined in all 51 subjects. LV contours and the input function region were obtained automatically with minimal operator intervention in 4DM (INVIA, Ann Arbor, Michigan) and FlowQuant (University of Ottawa, Canada) and semiautomatically with MunichHeart (Munich, Germany). Each dataset was analyzed independently by two different expert operators for each software program, who were blind to the results of the other observer.
MunichHeart analysis
Quantification using the custom software MunichHeart has been previously validated at our institution [15, 17, 25]. Myocardial activity in the last frame of the dynamic dataset is volumetrically sampled using regions of interest (ROI) and polar maps of the LV are generated. Segments are applied to the whole dynamic series to obtain myocardial time–activity curves. Arterial input function is calculated by a small cuboidal ROI in the center of the LV cavity defined in short-axis planes. MBF is then quantified using a simplified retention approach. Myocardial activity concentration between minutes 4 and 8 is normalized to the area under the arterial input function in the first 120 s based on the assumption that myocardial tracer retention is stable during this interval. The resulting index is corrected for partial volume losses, spill-over and nonlinear extraction of 82Rb. LV (global) MBF (milliliters per minute per gram of myocardial tissue) is obtained at peak stress and rest and the ratio of peak stress flow to rest flow is used to obtain global CFR.
Corridor4DM analysis
The quantitative dynamic analysis software 4DM is based on a methodology that has been previously validated [13, 14, 19]. The software uses generalized factor analysis (FA) of dynamic sequences (GFADS). The time–activity curves globally and in each vascular and 17-segment polar map sections are modeled as a combination of three contributions: the contribution from myocardial tissue, modeled with compartment analysis, and contributions from right ventricular (RV) and LV blood pools, modeled as fractions of measured LV and RV input functions. LV and RV input functions are obtained automatically as the LV and RV factors estimated for the whole factor image. The user input consists of choosing the parameters of the kinetic model, here done according to the procedure described by Yoshida et al. [12]. MBF is obtained by fitting the 82Rb time–activity curves to a two-compartment kinetic model. The main parameters of the model are the kinetic transport constants K1 (milliliters per minute per gram) and k2 (1/min), which denote the extraction (forward) and egress (backward) rates of transport between the metabolically trapped space (myocardium) and the freely diffusible space (blood pool), respectively. To estimate MBF from measures of K1, the extraction fraction reported previously for an open-chest procedure in dogs by Yoshida et al. is used [12]. The result is a parametric 17-segment polar map. We also used a second option of determining MBF with the 4DM based on ROI methodology and the one-tissue compartment kinetic modeling according to the procedure described by Lortie et al. [16].
FlowQuant analysis
FlowQuant (University of Ottawa, Canada) has been previously validated [21, 26] for MBF quantification with 82Rb PET. The rest–stress workflow starts with automatic processing of the rest scan, followed by a nearly identical process for the stress scan, and ending with the stress–rest flow reserve analysis. Uptake images are generated by averaging the last five time frames (4 min) to maintain high myocardium-to-blood pool contrast and reduce image noise. The uptake images are automatically processed to detect the location, orientation, and size of the LV myocardium. Three blood ROIs are placed automatically in the LV cavity, base, and left atrium. In the myocardium, a time–activity curve is generated for 576 sample points (36 × 16 rings). The uptake rate of 82Rb, K1 (milliliters per minute per gram), is quantified using a one-tissue compartment constant distribution volume model in both rest and stress states. The distribution volume is set to a scan-specific constant value determined by fitting the unconstrained model to the region of highest uptake in the polar map. K1 is related to flow (MBF in milliliters per minute per gram) through an extraction model based on 13N-ammonia MBF measured in humans by Lortie et al. [16].
Quantitative regional analysis
Each software package provides default options for regional analysis of the myocardial flow polar map. As such, ROIs were applied to each flow polar map to obtain quantitative flow data in the coronary artery distributions: left anterior descending (LAD), left circumflex (LCX) and right coronary artery (RCA).
Statistical analysis
Statistical analysis was performed using SPSS, version 20.0 (IBM, Chicago, IL), and MedCalc, version 12.3 (MedCalc Software, Mariakerke, Belgium). Continuous variables are presented as means ± SD. A repeated-measures ANOVA with a Greenhouse-Geisser correction was performed with post-hoc tests using Bonferroni correction. For characterization of interobserver variability, Pearson correlation coefficients were calculated. The intraclass correlation coefficients (ICC) were also computed. A P value of less than 0.05 was considered statistically significant.
Results
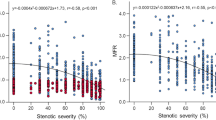
Results for mean rest and stress global MBF along with CFR values using the three different software packages employed in this study are summarized in Figs. 1, 2 and 3. MBF for both stress and rest scans were significantly higher with 4DM than with the other two programs (P < 0.001). No significant differences in CFR quantification among the three methods were found (P = 0.17). No significant difference in MBF quantification in rest or stress images was noted between MunichHeart and FlowQuant (P = 0.1) as summarized in Fig. 1. The same statistical trend in differences in MBF and CFR quantification was noted between the three software packages when the analysis was applied separately to the patient subgroups considering prior history or no history of CAD (Figs. 2 and 3).
To compare the CFR results from all four methods at the individual patient level, Fig. 4 shows linear fits and Bland–Altman plots for pairs of CFR values calculated using all four methods (six comparisons). Linear correlation coefficients varied between 0.71 (MunichHeart vs. 4DM-ROI) and 0.90 (FlowQuant vs. 4DM-ROI).
The agreement in the classification of patients among the three software packages was evaluated using a CFR cut-off value of 2.0, which is often reported as the value of CFR that separates normal from abnormal values. This has added prognostic value as shown by many groups using 82Rb or 13N-ammonia cardiac PET. Good agreement was reported and varied between 76 % and 90 % (Table 1).
Interobserver agreement in the estimation of CFR was excellent with all three software packages (Fig. 5). MunichHeart, which requires operator input for the manual orientation and short-axis sectioning of the LV, was found to have slightly higher interobserver variability than the other two software packages (R = 0.94 for MunichHeart, compared to 0.99 for 4DM-ROI, 4DM-FA, and FlowQuant), which are nearly fully automated. Correspondingly, the ICC for the degree of absolute agreement was 0.997 for FlowQuant, 4DM-FA and 4DM-ROI. Interobserver ICC was 0.970 for MunichHeart. Figure 5 shows correlation and Bland-Altman plots for the two observers for all four methods.
Mean rest and stress regional MBF and CFR values in relation to vascular territories (LAD, LCX, and RCA) using the different software packages are shown in Figs. 6, 7 and 8. Similar trends to those shown by the global blood flow values were seen for each vascular region with statistically significant differences in rest and stress MBF values, but similar CFR values. The ICCs among the software packages were 0.93 – 0.95 for regional CFR, 0.82 for regional stress MBF, and 0.86 – 0.87 for regional rest MBF.
Discussion
The main findings of this study were as follows: (1) absolute MBF values, both at rest and under pharmacological stress, determined using 4DM were significantly higher than those determined using FlowQuant and MunichHeart, particularly when using the GFADS method. In contrast, CFR values (the ratio of stress/rest MBF) were more similar among the different software packages/methods, (2) CFR values determined using FlowQuant and 4DM-ROI showed the best correlation and those determined using MunichHeart and 4DM-ROI the lowest correlation, (3) the binary agreement between the three software packages when considering a CFR cut-off value of 2.0 was highest between FlowQuant and 4DM-ROI, and lowest between MunichHeart and FlowQuant, and (4) interobserver reproducibility was excellent with FlowQuant and 4DM and very good with MunichHeart.
To compute absolute flow, several corrections must be made to the data including correcting the myocardial activity for partial volume losses and for spillover from blood-pool activity to the myocardium, correction of blood-pool activity or arterial input for myocardial to blood-pool spillover, and correcting both myocardial and blood-pool activity for random coincidences, physical decay and dead-time losses. Reliable tools for the fully automated computation of global and regional blood flow are necessary. Recently, several software packages for absolute MBF quantification have been developed and are being commercialized. This has the potential to make absolute myocardial flow measurements more available in clinical practice and not restricted to academic centers.
In this study, we quantitatively compared and evaluated three such software packages, which had been previously tested and validated. 4DM and FlowQuant are fully automated, and MunichHeart is semiautomated and relies on operator delineation and orientation of the LV. All three software programs are comprehensive packages and allow the user to choose different methodologies and kinetic modeling for MBF quantification. We restricted our comparisons to the default methods recommended by the developers, which are unique to each package. Many researchers have shown the feasibility of determining MBF and CFR with dynamic 82Rb PET [11–16]. This tracer does not require an on-site cyclotron for synthesis and thus it is more available for clinical cardiac PET in the community and has a higher potential for widespread clinical use than 13N-ammonia.
Notwithstanding the different methodologies of the three software applications for finding and segmenting the myocardium and blood pool automatically by 4DM and FlowQuant and semiautomatically by MunichHeart, and different ways of calculating the input and myocardial time–activity curves, no statistically significant differences were found between FlowQuant and MunichHeart in the quantitative determination of global MBF under rest and pharmacological stress conditions. However, statistically significant differences were found between MBF values calculated by 4DM (either 4DM-FA [12] or 4DM-ROI [16], default methods for the application) and FlowQuant and MunichHeart. Interestingly, no significant differences were found among the three packages in the estimation of global CFR, except for a trend for lower values using 4DM-ROI.
Previous studies have shown that a CFR cut-off value of 2.0 separates lower from higher risk individuals for cardiovascular events and therefore warrants prognostic consideration [17–22]. In this regard, agreement between the three software packages when considering a CFR cut-off value of 2.0 was good but not excellent. The software agreement varied between 76 % and 90 %, being highest between FlowQuant and 4DM-ROI. Similarly, global CFR values showed better correlations between FlowQuant and 4DM-ROI and lesser associations between MunichHeart and 4DM.
These discrepancies were likely due to many factors. Different methodologies for segmenting the myocardium and blood pool and different ways of calculating the input and myocardial time–activity curves may play a role. In this regard, both FlowQuant and 4DM-ROI use a similar LV segmentation (ROI-based) and one-tissue compartment kinetic modeling [16], which likely explain the better correlation between these two packages. On the contrary, MunichHeart and 4DM-FA, which use different LV segmentation (ROI vs. FA) and kinetic modeling (retention vs. compartment) methods, yielded lesser correlations. 4DM uses the concept of FA and is unique to this program [13, 14, 27]. The time–activity curve in each 17-segment polar map section is modeled as a combination of myocardial tissue, modeled with compartment analysis, and contributions from RV and LV blood pools, and modeled as fractions of measured LV and RV input functions. The spillover is modeled differently in these packages and may lead to differences in quantification of the MBF. Furthermore, it has been recently shown that spatially filtering the data affects the flow values from the 4DM-FA algorithm. In particular, a lower filter cut-off frequency increases the flow values because the peak activity in the whole image is decreased by smoothing which affects the scaling of the time–activity curves [28]. For the 4DM-FA algorithm, minimal filtering is recommended to improve the MBF estimates [28] and further provide lower standard error than that of ROI methods [29]. Mean CFR values were relatively constant due to similar changes in both stress and rest MBFs.
Not unexpectedly, the interobserver reproducibility showed better results for the fully automated programs 4DM and FlowQuant over MunichHeart, which is semiautomated, but automation may not always yield accurate results. In cases of strong subdiaphragmatic radiotracer uptake and scatter, automatic recognition of the myocardium may not work and observer intervention may be needed. Fortunately, optional operator intervention is available in FlowQuant and 4DM.
This study had several limitations. A gold standard by which to evaluate the accuracy of MBF measurements is lacking. A large animal study comparing myocardial flow determined using 82Rb using different kinetic models and microspheres would be ideal, but would also be limited by anatomical and pathophysiological differences between animals and humans. An alternative would be to include human studies comparing the use of 82Rb with 15O-water. Our goal, however, was to compare and analyze the results from the clinical implementation of outcome-validated kinetic modeling software tools, using the same scanner and reconstruction protocol in the same patient population. In this work, we studied only 82Rb MBF.
A recent study by Slomka et al. compared three software programs for 13 N-ammonia (QPET, syngo MBF, and PMOD) and found excellent correlation between packages [23]. The reason for greater discrepancies in this work may be attributable to fundamentally different tracer kinetic modeling approaches and the need for extraction correction of K1 values in order to estimate MBF values. 82Rb extraction is MBF-dependent and highly nonlinear. Model-specific extraction functions have previously been demonstrated and can serve to correct for biases in MBF resulting from the image acquisition, reconstruction, and analysis processes [30, 31].
One needs to be aware of these limitations when using 82Rb and that numbers cannot be extrapolated from one software to another, especially the absolute flow values. Similarly, further discrepancies in reference values between facilities may be possible due to differences in scanner type, and reconstruction and dynamic protocols applied. Finally, we are aware that the sample size in our study was relatively small, yet the myocardial flow differences seen among the various software packages were maintained between patients with low-intermediate probability of CAD (higher flow parameters) and those with known CAD (lower flow values), implying that our results are likely reliable across a wide range of myocardial flow values.
Conclusion
Quantification of resting and stress MBF is dependent on the software and methods used. CFR, on the other hand, appears to be more comparable. The threshold value for abnormal CFR is software-dependent. A normal reference range should be sought and fixed for each application separately. As a consequence, follow-up and treatment assessment should be done with the same software and methods.
References
Machac J. Cardiac positron emission tomography imaging. Elsevier; 2005. p. 17–36.
Bengel FM, Higuchi T, Javadi MS, Lautamäki R. Cardiac positron emission tomography. J Am Coll Cardiol. 2009;54:1–15.
Di Carli MF, Hachamovitch R. New technology for noninvasive evaluation of coronary artery disease. Circulation. 2007;115:1464–80.
Bateman TM, Heller GV, McGhie AI, Friedman JD, Case JA, Bryngelson JR, et al. Diagnostic accuracy of rest/stress ECG-gated Rb-82 myocardial perfusion PET: comparison with ECG-gated Tc-99m sestamibi SPECT. J Nucl Cardiol. 2006;13:24–33.
Sampson UK, Dorbala S, Limaye A, Kwong R, Di Carli MF. Diagnostic accuracy of rubidium-82 myocardial perfusion imaging with hybrid positron emission tomography/computed tomography in the detection of coronary artery disease. J Am Coll Cardiol. 2007;49:1052–8.
Lertsburapa K, Ahlberg AW, Bateman TM, Katten D, Volker L, Cullom SJ, et al. Independent and incremental prognostic value of left ventricular ejection fraction determined by stress gated rubidium 82 PET imaging in patients with known or suspected coronary artery disease. J Nucl Cardiol. 2008;15:745–53.
Yoshinaga K, Chow BJW, Williams K, Chen L, deKemp RA, Garrard L, et al. What is the prognostic value of myocardial perfusion imaging using rubidium-82 positron emission tomography? J Am Coll Cardiol. 2006;48:1029–39.
Flotats A, Bravo PE, Fukushima K, Chaudhry MA, Merrill J, Bengel FM. 82Rb PET myocardial perfusion imaging is superior to 99mTc-labelled agent SPECT in patients with known or suspected coronary artery disease. Eur J Nucl Med Mol Imaging. 2012;39:1233–9.
Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, et al. Single photon-emission computed tomography. J Nucl Cardiol. 2010;17:941–73.
Bengel FM. Leaving relativity behind: quantitative clinical perfusion imaging. J Am Coll Cardiol. 2011;58:749.
Herrero P, Markham J, Shelton ME, Bergmann SR. Implementation and evaluation of a two-compartment model for quantification of myocardial perfusion with rubidium-82 and positron emission tomography. Circ Res. 1992;70:496–507.
Yoshida K, Mullani N, Gould KL. Coronary flow and flow reserve by PET simplified for clinical applications using rubidium-82 or nitrogen-13-ammonia. J Nucl Med. 1996;37:1701–12.
El Fakhri G, Sitek A, Guérin B, Kijewski MF, Di Carli MF, Moore SC. Quantitative dynamic cardiac 82Rb PET using generalized factor and compartment analyses. J Nucl Med. 2005;46:1264–71.
El Fakhri G, Kardan A, Sitek A, Dorbala S, Abi-Hatem N, Lahoud Y, et al. Reproducibility and accuracy of quantitative myocardial blood flow assessment with 82Rb PET: comparison with 13N-ammonia PET. J Nucl Med. 2009;50:1062–71.
Lautamäki R, George RT, Kitagawa K, Higuchi T, Merrill J, Voicu C, et al. Rubidium-82 PET-CT for quantitative assessment of myocardial blood flow: validation in a canine model of coronary artery stenosis. Eur J Nucl Med Mol Imaging. 2009;36:576–86.
Lortie M, Beanlands RSB, Yoshinaga K, Klein R, DaSilva JN, DeKemp RA. Quantification of myocardial blood flow with 82Rb dynamic PET imaging. Eur J Nucl Med Mol Imaging. 2007;34:1765–74.
Fukushima K, Javadi MS, Higuchi T, Lautamäki R, Merrill J, Nekolla SG, et al. Prediction of short-term cardiovascular events using quantification of global myocardial flow reserve in patients referred for clinical 82Rb PET perfusion imaging. J Nucl Med. 2011;52:726–32.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography: added value of coronary flow reserve. J Am Coll Cardiol. 2009;54:150–6.
Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Di Carli G, et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation. 2011;124:2215–24.
Tio RA, Dabeshlim A, Siebelink HMJ, De Sutter J, Hillege HL, Zeebregts CJ, et al. Comparison between the prognostic value of left ventricular function and myocardial perfusion reserve in patients with ischemic heart disease. J Nucl Med. 2009;50:214–9.
Ziadi MC, deKemp RA, Williams KA, Guo A, Chow BJW, Renaud JM, et al. Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia. J Am Coll Cardiol. 2011;58:740–8.
Fiechter M, Gebhard C, Ghadri JR, Fuchs TA, Pazhenkottil AP, Nkoulou RN, et al. Myocardial perfusion imaging with 13N-ammonia PET is a strong predictor for outcome. Int J Cardiol. 2013;167:1023–6.
Slomka PJ, Alexanderson E, Jácome R, Jiménez M, Romero E, Meave A, et al. Comparison of clinical tools for measurements of regional stress and rest myocardial blood flow assessed with 13N-ammonia PET/CT. J Nucl Med. 2012;53:171–81.
Rajaram M, Tahari AK, Lee AH, Lodge MA, Tsui B, Nekolla S, et al. Cardiac PET/CT misregistration causes significant changes in estimated myocardial blood flow. J Nucl Med. 2013;54:50–4.
Nekolla SG, Miethaner C, Nguyen N, Ziegler SI, Schwaiger M. Reproducibility of polar map generation and assessment of defect severity and extent assessment in myocardial perfusion imaging using positron emission tomography. Eur J Nucl Med Mol Imaging. 1998;25:1313–21.
Klein R, Renaud JM, Ziadi MC, Thorn SL, Adler A, Beanlands RS, et al. Intra- and inter-operator repeatability of myocardial blood flow and myocardial flow reserve measurements using rubidium-82 PET and a highly automated analysis program. J Nucl Cardiol. 2010;17:600–16.
Sitek A, Gullberg GT, Huesman RH. Correction for ambiguous solutions in factor analysis using a penalized least squares objective. IEEE Trans Med Imaging. 2002;21:216–25.
Lee B, Moody J, Sitek A, Murthy V, Di Carli M, Corbett J, et al. Effects of filtering on Rb-82 myocardial blood flow estimates. J Nucl Med. 2013;54 Suppl 2:1659.
Moody JB, Lee BC, Ficaro EF. Error estimation for dynamic PET myocardial blood flow. J Nucl Med. 2012;53 Suppl 1:323.
Klein R, Beanlands RS, deKemp RA. Quantification of myocardial blood flow and flow reserve: technical aspects. J Nucl Cardiol. 2010;17:555–70.
Klein R, Beanlands RS, Wassenaar RW, Thorn SL, Lamoureux M, DaSilva JN, et al. Kinetic model-based factor analysis of dynamic sequences for 82-rubidium cardiac positron emission tomography. Med Phys. 2010;37:3995–4010.
Acknowledgments
A.K.T. was supported by the National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health under Award Number T32EB006351.
Conflicts of interest
R.K. and R.deK. acknowledge receiving revenue shares from the sale of FlowQuant. E.F. acknowledges receiving revenue shares from the sale of Corridor4DM. B.L. acknowledges receiving financial support from INVIA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tahari, A.K., Lee, A., Rajaram, M. et al. Absolute myocardial flow quantification with 82Rb PET/CT: comparison of different software packages and methods. Eur J Nucl Med Mol Imaging 41, 126–135 (2014). https://doi.org/10.1007/s00259-013-2537-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2537-1