Abstract
Objective
To assess diagnostic accuracy and agreement among radiologists in detecting femoroplasty on pre- and post-arthroscopic comparison frog lateral and anteroposterior (AP) pelvic radiographs after treatment of femoroacetabular impingement (FAI) syndrome.
Materials and methods
In this retrospective, cross-sectional study, 86 patients underwent hip arthroscopy (52 with and 34 without femoroplasty) for treatment of FAI syndrome. Three radiologists blinded to clinical data and chronological order of the pre- and post-arthroscopic comparison radiographs independently examined AP pelvis and frog lateral radiographs to detect femoroplasty changes. Statistical analysis outputs included diagnostic accuracy parameters and inter- and intra-observer agreement.
Results
Identification of femoroplasty in the frog lateral projection has mean sensitivity 70%, specificity 82%, inter-observer agreement κ 0.74–0.76 and intra-observer agreement κ 0.72–0.85. Using the AP pelvis projection to detect femoroplasty has mean sensitivity 32%, specificity 71%, inter-observer agreement κ 0.47–0.65, and intra-observer agreement κ, 0.56–0.84.
Conclusions
Radiologists are only moderately sensitive, though more specific, in femoroplasty detection in the frog lateral projection. The AP pelvis projection yields lower sensitivity and specificity. Both projections have moderate inter- and intra-observer agreement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Femoroacetabular impingement (FAI) syndrome of the hip is a “motion-related clinical triad of symptoms, clinical signs and imaging findings” [1]. Symptoms arise when altered bony morphology leads to abnormal bony contact of the femoral neck against the anterior acetabular rim [2]. Repetitive abutment of these bony structures leads to labral and cartilage damage [2].
The number of arthroscopies performed on patients with FAI syndrome has been rising because of increasing awareness [1], improved techniques for reshaping the bony morphology [3], and promising short-to-mid-term symptomatic relief after arthroscopic intervention [4]. After femoroplasty, radiography is the preferred initial exam not only to detect complications such as fracture but to assess residual deformity, a predictor of clinical response [5, 6]. There are many studies on pre-operative evaluation of the abnormal morphology of the femoral neck, but relatively few on post-operative evaluation of femoroplasty [5, 6]. Moreover, studies on femoroplasty have been conducted in orthopedic or clinical contexts where the emphasis is on obtaining measurements to document the extent of bone correction; it is unclear if femoroplasty can consistently be detected in a radiology context, i.e., where there is no a priori knowledge of femoroplasty and detection is based on visual comparison, not measurements. We also do not know which radiographic projection or combination of projections is best for detecting femoroplasty. This evidence has important clinical implications on managing imaging outcomes because radiography has been recommended as the initial post-operative test [1]. Moreover, characterizing the accuracy of the imaging test can help surgeons and patients understand why failure to detect simply reflects the limitation of the test rather than an interpretive error.
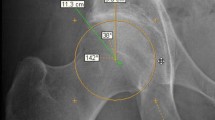
The two types of altered bony configuration in FAI syndrome are the cam and pincer morphologies. Cam morphology is characterized by a bony prominence or lack of offset in the anterior femoral neck [1, 7]. Pincer morphology is characterized by over coverage of the acetabular rim [1]. These morphologies may occur in combination. Open or arthroscopic correction involves either reshaping the profile of the anterior femoral neck (or femoroplasty) or trimming the acetabular over coverage (or acetabuloplasty). The alpha angle is the most commonly used measurement to quantify the cam morphology in the pre- [1, 7] and post-operative [8, 9] settings. Our goal was to assess diagnostic accuracy and agreement among radiologists in detecting femoroplasty when comparing anonymized pre- and post-arthroscopic frog lateral and AP pelvic radiographs after treatment of FAI syndrome.
Methods
Study design
This retrospective, cross-sectional, single-center diagnostic accuracy and agreement study was designed and conducted according to Standards for Reporting of Diagnostic Accuracy (STARD) and the Guidelines for Reporting Reliability and Agreement Studies (GRRAS) [10, 11]. Our institutional review board approved this study with a waiver of informed consent.
Patients
The study cohort consisted of a convenient sample of 113 consecutive patients with hip FAI syndrome who underwent hip arthroscopy between January 1, 2013 and July 31, 2015. All surgery was performed by one orthopedic surgeon in a single academic center. All patients met the required triad of positive signs for FAI syndrome (motion-related groin pain relieved by lidocaine injection), symptoms (a positive impingement provocation test, i.e., pain with flexion, adduction, internal rotation test) and imaging findings that are detailed below. The diagnosis was confirmed during arthroscopy.
Inclusion and exclusion criteria
Participants had both pre- and post-operative radiographs such as frog lateral, AP pelvis, or Dunn view, with radiographs obtained in the two years before and after hip arthroscopy. The post-op radiography was routinely obtained at our institution prior to start of weight bearing to exclude complications such as fractures [12], document residual deformity [13], and serve as a baseline to monitor potential late-term (beyond 2 years after arthroscopy) regrowth of cam morphology [14]. We accepted images acquired at other institutions. Cases were excluded if the pre- and post-surgical projections of the hip did not match, commonly for images acquired at outside institutions. Eligible cases were stratified into two cohorts: femoroplasty and nonfemoroplasty (Fig. 1).
Radiography
Radiographs were obtained using a digital radiographic system (DigitalDiagnost System, version 2.1; Philips Medical Systems, Hamburg, Germany). The AP pelvis projection was obtained with both hips in 15° of internal rotation. The frog lateral projection was obtained with imaged hip abducted 45°.
Test method
Reference standard
Surgical reports of each diagnostic arthroscopy were reviewed from the electronic medical record (EPIC; Verona, WI) and served as the reference standard for presence or absence of femoroplasty.
Arthroscopy
During arthroscopy, all patients had one or more of the following procedures:
-
Femoroplasty. Femoroplasty is reshaping of the cam morphology by trimming of the femoral head. The extent of reshaping or bony resection is monitored by dynamic intra-operative fluoroscopy [15], with no more than 30% of bone resection at femoral neck to reduce risk of fracture [12].
-
Acetabuloplasty. Acetabuloplasty is reshaping of the pincer morphology by trimming of the acetabular rim. The amount of trimmed acetabular rim is very small, < 4 mm wide in published reports [16, 17] and ≤2 mm at our institution.
-
Labral repair. The damaged labrum are repaired or reconstructed.
-
Chondroplasty. Cartilage damaged is addressed by smoothing and trimming any degenerative and unstable cartilage.
-
Other. Intra-articular body or os acetabuli removal, synovectomy, psoas release.
Femoroplasty group
This group had femoroplasty and in many cases additional procedures from the list above. Cam morphology in the femoroplasty group was confirmed by:
-
1.
Direct visualization and intra-operative fluoroscopy (Table 1) [15]
-
2.
An angle of >55° on any imaging plane or modality (MR or radiography)
Nonfemoroplasty (control) group
This group underwent arthroscopic surgery for FAI syndrome and completed one of more of the arthroscopic procedures listed above with the exception of femoroplasty. This group of patients did not undergo femoroplasty because of absence of cam morphology and served as the control (Table 1).
Image review
Two board-certified musculoskeletal radiologists (MSK1, MSK2) with 5 and over 20 years of experience, respectively and one board-certified general radiologist (GEN1) with over 20 years of experience independently evaluated radiographic images using Barco MDCG 3221 3-megapixel monitors (Kortrijk, Belgium) with Philips iSite PACS v3.6 software (Philips Healthcare, Best, Netherlands).
Review process
Pre- and post-surgical image pairs were shown to readers at all times. The image pairs were displayed in random hanging order, with all identifiers and time stamps removed so that reviewers were blinded to the chronology of the pair. Frog lateral and AP pelvis projections were reviewed in separate sessions so that each diagnosis was made in a single projection. This enabled us to assess the relative diagnostic value of each projection. The AP pelvis displayed both hips and the frog lateral displayed the surgical hip alone. Reviewers were informed only that arthroscopy had been performed on one hip during the interval between the paired images. At time 1, all observers completed a first read-through of the AP pelvis and frog lateral cases. One month later (time 2), only two observers (MSK2 and GEN1) completed a second read-through of the cases. MSK1 did not complete the second read-through because of job change, but the absence of the second read-through of this reviewer did not affect statistical analysis. Cases were reordered in the second read-through to minimize recall bias. Reviewers did not measure the alpha angle. In addition to femoroplasty, other observations were also recorded. These included intra-articular body or os acetabuli removal and a radiolucency in the femoral head neck junction representing bone loss at femoroplasty site.
Definition for positive identification of femoroplasty
Femoroplasty was correctly identified on the anonymized pre- and post-operative image pair (Figs. 2, and 3) when either
-
1.
The osseous prominence at head-neck junction was reduced or resected or
-
2.
The bony profile at head-neck junction was modified so an off set is restored
and
-
3.
The image with findings (1) or (2) was on the anonymized post-operative radiograph only and
-
4.
For the AP projection, positive identification was on the surgical hip.
a– d 43-year-old woman with left hip impingement symptoms with pre- and post-femoroplasty images in AP pelvis ( a, b) and frog lateral ( c, d) projections. The patient underwent arthroscopic femoroplasty, acetabuloplasty and labral debridement. All readers detected both the cam morphology (arrow) and femoroplasty (arrow head). The acetabuloplasty was imperceptible. This represents a true positive case for both projections
a– d 15-year-old girl with insidious onset of right hip pain and FAI syndrome with pre- and post-femoroplasty radiographs in AP pelvis ( a, b) and frog lateral ( c, d) projections. The patient underwent arthroscopic femoroplasty, labral debridement, psoas release, and synovectomy. Femoroplasty was detected only on the frog lateral projection ( d) by all reviewers. This represents a false negative case for the AP pelvis projection. Also noted was the slight variation in the rotation of the hip between the pre- and post-arthroscopy frog lateral view. Since the image remained diagnostic, this frog lateral set was not excluded
Statistical analysis
Statistical analyses were performed in SAS version 9.4. The diagnostic accuracy of readers in identifying femoroplasty was assessed with sensitivity, specificity, positive predictive value, and negative predictive value with 95% confidence intervals. Inter- and intra-rater agreement were assessed using simple Cohen’s kappa (κ). Interpretation of the κ value followed Landis et al. [18]: a κ of 0.00–0.20 was considered slight agreement, 0.21–0.40 fair agreement, 41–0.60 moderate agreement, 0.61–0.80 substantial agreement, and 81–1.00 almost perfect agreement.
Results
Patients
After application of inclusion and exclusion criteria, the study group consisted of 86 patients, of whom 52 had femoroplasty and 34 did not undergo femoroplasty. The latter group served as control. The demographics and surgical history of these two groups were tabulated (Table 1). Some patients had multiple concurrent procedures during arthroscopy such as labral repair, acetabuloplasty, chondroplasty, intra-articular body and os acetabuli removal, synovectomy, and psoas release. The femoroplasty group was younger, predominantly male, and more likely to undergo concurrent acetabuloplasty. Fourteen patients had an additional Dunn view as part of their pre- and post-surgical imaging evaluation. Due to the insufficient number of Dunn projections among eligible cases, this projection was removed from the analysis.
Test results
Accuracy of femoroplasty identification using anonymized pre- and post-arthroscopic comparison radiographic pair, blinded to both identity and chronology is summarized in Table 2. Sensitivity of identification of femoroplasty in the frog lateral projection ranged from 58–83% (mean 70%) compared to AP pelvis projections with 29–42% (mean 32%). Specificity was higher than sensitivity in both projections, i.e., 79–88% (mean 82%) with frog lateral and 56–79% (mean 71%) with AP pelvis projection. The general radiologist was less sensitive and specific in the AP pelvis projection than the MSK radiologists but demonstrated similar accuracy in the frog lateral projection.
Inter- and intra-observer agreement of readers in identifying femoroplasty is reported in Table 3. Inter-observer agreement in identifying femoroplasty changes was substantial in the frog lateral (κ 0.74–0.76) and moderate in the AP pelvis projection (κ 0.47–0.65). Intra-observer agreement was substantial to almost perfect in the frog lateral (κ 0.72–0.85) and moderate to almost perfect in the AP pelvis (κ 0.56–0.84). The following findings were also noted during the review:
-
Resection of os acetabuli. Os acetabuli was resected in two patients in the no-femoroplasty group and was observed inconsistently by reviewers.
-
A radiolucency in the femoral-head neck junction at resection site (Fig. 4). This lucency represented bone loss related to resection during femoroplasty and was noted in 14% (12) of AP and 18% (13) frog lateral projections.
-
Acetabuloplasty change. The surgeon at our institution was conservative in surgical technique at the acetabulum and removed less than 2 mm of the acetabular rim during arthroscopy. No reviewer observed changes in the acetabulum when acetabuloplasty was performed.
a– b 37-year-old male with chronic right hip pain and FAI syndrome refractive to conservative treatment underwent femoroplasty with pre- ( a) and post-femoroplasty ( b) AP pelvis radiographs. An ill-defined radiolucency surrounded by a segment of indistinct cortex (arrow) on the post-operative image ( b) reflected bone loss as result of femoroplasty. This lucency was noted in 14% (12) of AP and 18% (13) frog lateral projections in this cohort
Discussion
Post-femoroplasty radiographs are routinely performed [8, 9] not only to detect complications such as fractures [12] and delayed regrowth of cam morphology but also to assess completeness of bone correction, an important predictor of clinical outcome [5, 6]. This study evaluates radiologists’ ability to detect femoroplasty by comparing anonymized pre- and post-arthroscopy image pairs, blinded to identity and chronology. We found sensitivities of 70 and 32% for the frog lateral and AP pelvis projections respectively. Specificities were higher than sensitivities (82% for frog lateral, 71% for AP pelvis). The frog lateral projection had higher inter-observer agreement (κ 0.74–0.76) than the AP pelvis (κ 0.56–0.84). Of note, we are the first to report a focus of radiolucency representing bone loss at site of femoroplasty.
If bone reshaping site is expected to correspond to cam morphology location, our finding that the AP projection performs poorly is not surprising. The reason is that the AP projection captures the superior or 12 o’clock position, where the cam morphology is less frequent, low sensitivity is expected, (Table 4) [15, 19,20,21,22]. Similarly, sensitivity of the frog lateral projection is also anticipated to be low because it captures the 3 o’clock region, also a less frequent location for cam morphology (Table 4). The 70% sensitivity of the frog lateral, however, exceeds expectation. Our data raise the possibility that the distributions of femoroplasty site may not match those of cam morphology. In other words, the imaging plane that frequently captures the cam morphology may not be the same as that of bone resection. One reason for this disparity could be the imprecision of surgical technique; a comparison of open to arthroscopic femoroplasty on cadaveric specimens noted that the arthroscopic technique tended to underestimate the length of bone resection and placed the resection more posterior than planned [23]. Adding variability is the wide distribution of the maximal cam morphology (Table 4), which could be anterosuperior [21], lateral [15] or anterolateral [22]. These data are important because larger cam morphology lends to easier detection of its resection. As a result, the site of bone reshaping is less predictable.
If the site of bone reshaping is variable, one strategy to improve detection is to canvass the anterior neck from 12 to 3 o’clock with combined radiographic projections (Table 4)—e.g., one may combine frog lateral (3 o’clock), false profile (2–3 o’clock), Dunn (1–2 o’clock), and AP (12 o’clock) projections to cover most of the anterior femoral neck (Table 4) [15, 20, 24, 25]. This concept has been tested in detection of cam morphology; Hellman et al. combined 90° Dunn, false profile, and AP pelvis projections and reported sensitivity and specificity of 86% and 75% respectively [24]. Meyer et al. studied six radiographic projections to assess femoral head/neck asphericity and concluded that a combination AP pelvis and cross-table view in internal rotation minimized false negatives [26]. Nepple et al. evaluated four projections (AP pelvis, 45° Dunn, frog lateral, and cross-table lateral) individually and in combination [20]. The highest sensitivity (90%) was from combining all four projections, although this improvement was not without cost, as specificity dropped to 9% [20]. We can apply the same strategy for femoroplasty detection, but more studies are needed to find the combination of projections that yields the best balance of sensitivity and specificity.
Our finding of only moderate (30–70%) accuracy femoroplasty detection using commonly performed radiographic projections has important clinical implications, as visibility of femoroplasty on the index post-operative radiograph could influence one’s choice of subsequent imaging exams—for example, if the femoroplasty is not visible, adding other projections or supplementary CT or MRI to survey more of the anterior femoral neck might be necessary to assess the completeness of bone correction in cases of failed arthroscopy [13, 26]. In contrast, if the femoroplasty is clearly visible on the index post-operative radiographs, serial radiography using the same projections would suffice to monitor the bone resection site for complications, including potential late-term regrowth of cam morphology. Our data provide a starting point for future investigations to determine which combination of radiographic projections will produce the highest accuracy and reliability in profiling the site of femoroplasty. This is important since radiography, with its low radiation dose and cost relative to CT and/or MRI, remains the choice of initial imaging assessment [1] after treatment of FAI syndrome.
Finally, our study simulates the context of most radiology practice, where the radiologist may not have a priori knowledge of femoroplasty due to incomplete history and detection of post-operative changes is generally based on visual comparison. Our data on femoroplasty accuracy may thus help surgeons and patients understand that detection failure can simply reflect a limitation of the test itself rather than interpretive error. This is particularly relevant as the readily accessible medical record and imaging report [27] frequently serve as the starting point for patients to begin their on-line research [16]. Absent our data, the inconsistent reporting of femoroplasty change could be perceived as poor-quality care, leading to loss of confidence in the radiologist by both surgeon and patient.
Limitations
First, our findings are biased by our knowledge that arthroscopy had occurred. This information could increase the scrutiny of the reviewers for post-arthroscopic changes and subsequently affect accuracy of the test. We attempted to mitigate this bias by blinding the image pairs in both identity and chronology. Moreover, we required the reviewers to correctly identify the post-arthroscopic image where femoroplasty is detected.
Second, other post-operative findings such as resection of os acetabuli or acetabuloplasty could theoretically unblind the reader to the chronology of the comparison radiographs. Since only two patients in the nonfemoroplasty group had resection of os acetabuli and the readers inconsistently made this observation, our results are unlikely to have been significantly affected. Similarly, acetabuloplasty could potentially unmask the order of the comparison radiographs; however, the amount of carefully trimmed acetabular rim is very small, < 4 mm wide in published reports [16, 17] and ≤2 mm at our institution. Moreover, Bedi et al. reported a 3.2-mm rim reduction corresponded to a change of coronal center edge angle of 3.9° [16]. This change is small and is not noted by any of our reviewers.
Third, the amount of resected bone was not recorded. This theoretically could affect the visibility of femoroplasty; however, the amount of bone resection is substantive, with reported approximate alpha angle correction ranges from 13° [16] to 38° [15, 28]. We consider this relatively large degree of correction likely to be visible in the appropriate projection and with comparison radiographs.
In conclusion, radiologists are only moderately sensitive but are more specific in femoroplasty detection when comparing anonymized pre- and post-arthroscopic radiographs in the frog lateral projection. The AP pelvis projection yields lower sensitivity and specificity. Both projections have moderate inter- and intra-observer agreement. The higher than expected sensitivity of the frog lateral projection suggests the site of femoroplasty could be unpredictable. More studies are needed to determine whether the accuracy improves when more projections are added.
References
Griffin DR, Dickenson EJ, O’Donnell J, Agricola R, Awan T, Beck M, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50:1169–76.
Ito K, Minka MA, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect: a MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–6.
Reiman MP, Thorborg K, Hölmich P. Femoroacetabular impingement surgery is on the rise: but what is the next step? J Orthop Sport Phys Ther. 2016;46:406–8.
Steppacher SD, Anwander H, Zurmühle CA, Tannast M, Siebenrock KA. Eighty percent of patients with surgical hip dislocation for femoroacetabular impingement have a good clinical result without osteoarthritis progression at 10??Years. Clin Orthop Relat Res. 2015;473:1333–41.
de Sa D, Urquhart N, Philippon M, Ye J-E, Simunovic N, Ayeni OR. Alpha angle correction in femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22:812–21.
Sardana V, Philippon MJ, de Sa D, Bedi A, Ye L, Simunovic N, et al. Revision hip arthroscopy indications and outcomes: a systematic review. Arthroscopy. 2015;31:2047–55.
Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–60.
Hetaimish BM, Khan M, Crouch S, Simunovic N, Bedi A, Mohtadi N, et al. Consistency of reported outcomes after arthroscopic management of femoroacetabular impingement. Arthroscopy. 2013;29:780–7.
Dzaja I, Martin K, Kay J, Memon M, Duong A, Simunovic N, et al. Radiographic outcomes reporting after arthroscopic management of femoroacetabular impingement: a systematic review. Curr Rev Musculoskelet Med. 2016;9:411–7.
Kottner J, Audig L, Brorson S, Donner A, Gajewski BJ. Guidelines for reporting reliability and agreement studies (GRRAS) were proposed. J Clin Epidemiol. 2011;64:96–106.
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Paul P, Irwig L, et al. STARD 2015: an updated list of essential items for. Res Methods Reporting. 2015;5527:1–9.
Ilizaliturri VM. Complications of arthroscopic femoroacetabular impingement treatment: a review. Clin Orthop Relat Res. 2009;467:760–8.
Ross JR, Larson CM, Adeoyo O, Kelly BT, Bedi A. Residual deformity is the most common reason for revision hip arthroscopy: a three-dimensional CT study. Clin Orthop Relat Res 2014;1388–1395.
Gupta A, Redmond JM, Stake CE, Finch NA, Dunne KF, Domb BG. Does the femoral cam lesion regrow after osteoplasty for femoroacetabular impingement? Am J Sports Med. 2014;42:2149–55.
Ross JR, Bedi A, Stone RM, Sibilsky Enselman E, Leunig M, Kelly BT, et al. Intraoperative fluoroscopic imaging to treat cam deformities: correlation with 3-dimensional computed tomography. Am J Sports Med. 2014;42:1370–6.
Bedi A, Zaltz I, De La Torre K, Kelly BT. Radiographic comparison of surgical hip dislocation and hip arthroscopy for treatment of cam deformity in femoroacetabular impingement. Am J Sports Med. 2011;39(Suppl):20S–8S.
Jackson TJ, Stake CE, Trenga AP, Morgan J, Domb BG. Arthroscopic technique for treatment of femoroacetabular impingement. Arthrosc Tech. 2013;2:e55–9.
Landis JR, Koch GG. Agreement measures for categorical data. Biometrics. 1977;33:159–74.
Rakhra KS, Sheikh AM, Allen D, Beaulé PE. Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:660–5.
Nepple JJ, Martel JM, Kim YJ, Zaltz I, Clohisy JC. Do plain radiographs correlate with CT for imaging of cam-type femoroacetabular impingement? Clin Orthop Relat Res. 2012;470:3313–20.
Pfirrmann CW. A, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778–85.
Audenaert EA, Baelde N, Huysse W, Vigneron L, Pattyn C. Development of a three-dimensional detection method of cam deformities in femoroacetabular impingement. Skelet Radiol. 2011;40:921–7.
Mardones R, Lara J, Donndorff A, Barnes S, Stuart MJ, Glick J, et al. Surgical correction of “cam-type” femoroacetabular impingement: a cadaveric comparison of open versus arthroscopic debridement. Arthroscopy. 2009;25:175–82.
Hellman MD, Mascarenhas R, Gupta A, Fillingham Y, Haughom BD, Salata MJ, et al. The false-profile view may be used to identify cam morphology. Arthroscopy. 2015:1–5.
Domayer SE, Ziebarth K, Chan J, Bixby S, Mamisch TC, Kim YJ. Femoroacetabular cam-type impingement: diagnostic sensitivity and specificity of radiographic views compared to radial MRI. Eur J Radiol. 2011;80:805–10.
Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res 2006;PAP:181–5.
Hanauer DA, Preib R, Zheng K, Choi SW. Patient-initiated electronic health record amendment requests. J Am Med Inform Assoc. 2014;21:992–1000.
Stähelin L, Stähelin T, Jolles BM, Herzog RF. Arthroscopic offset restoration in femoroacetabular cam impingement: accuracy and early clinical outcome. Arthroscopy. 2008;24:51–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
This study was partially funded by Dartmouth Clinical and Translational Science Institute (NIH award number UL1TR001086 to Steffen Haider).
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Haider, S.J., Siegel, A.H., Spratt, K.F. et al. Detection of femoroplasty on pre- and post-arthroscopic comparison radiographs following treatment of femoroacetabular impingement syndrome: multi-reader accuracy and agreement study. Skeletal Radiol 47, 233–242 (2018). https://doi.org/10.1007/s00256-017-2789-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-017-2789-0