Abstract
Purpose
Radiological evaluation of femoroacetabular impingement is based on single-plane parameters such as the alpha angle or the center edge angle, or complex software reconstruction. A new simple classification for cam and pincer morphologies, based on a two-plane radiological evaluation, is presented in this study. The determination of the intraobserver and interobserver reliability of this new classification is the purpose of this study.
Methods
We retrospectively reviewed the three-view hip study in patient undergoing hip arthroscopy for FAI syndrome between October 2015 and April 2016. Any case having protrusio acetabuli, coxa profunda or which has undergone previous osteotomic surgery was excluded. Five observers used our proposed classification to identify three different stages for the cam and pincer morphologies. Inter- and intraobserver agreement of classification was determined using average pairwise Cohen’s kappa coefficient.
Results
The interobserver agreement for the pincer and cam morphologies was excellent. For the pincer morphology classification, the average Kappa agreement was 0.838 (range 0.764–0.944). For the cam morphology, the average pairwise Cohen’s kappa coefficient was 0.846 (range 0.734–0.929). The intraobserver agreement was excellent as well. The average percent pairwise agreement was 0.870 and 0.845 for pincer and cam type, respectively.
Conclusions
The new classification system shows excellent levels of inter- and intraobserver agreement for both deformities. This classification is demonstrated to be a useful tool in planning hip arthroscopy. Further studies are needed to correlate the classification itself with specific intraoperative findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Femoroacetabular impingement (FAI) is increasingly recognized as an important cause of hip pain in young adults, as well as a leading cause of early osteoarthritis of the hip [1, 2]. Hip arthroscopy has emerged as a promising modality in the treatment for FAI syndrome [3].
Current quantification and classification of FAI syndrome are based on femoral sphericity and acetabular coverage measurements (like the alpha angle and the center edge angle of Wiberg). However, such classifications do not reflect the extent of the impingement nor the severity of the deformity [4].
The development of new parameters such as the omega zone [5] although combining the femoral and acetabular morphology requires measurements that need dedicated software and, in any case, does not provide a description or a staging of the severity of the deformities.
Another classification proposed by Ipach et al. [6, 7] describes the correlation between the severity of the cam morphology and osteoarthritis, using femoral sphericity measurements with poor reliability results. A classification should allow the injury’s identification by means of a simple algorithm based on easily recognizable and consistent imaging and clinical characteristics. In addition, it should provide a concise and descriptive terminology, information regarding the severity of the injury and guidance as to the choice of treatment and should serve as a useful tool for further studies.
A proper classification method for cam and pincer morphologies is necessary to grade the pathology and give indications for the correct surgery. A usable classification needs to be as simple as possible, reproducible and comparable between surgeons and between images taken at different services.
For all those reasons, our classification was based on standard radiographic imaging and evaluates the extent of the femoral and acetabular bony deformities, providing three stages of increasing severity either for the cam or for the pincer morphologies.
The determination of intra- and interobserver reliability for our new proposed classification system was pursued in the present study. The hypothesis of the current study was that a classification system based on a two-plane radiographic examination would result in moderate-to-substantial interobserver and intraobserver reliability of femoral and acetabular morphology.
Methods
The three-view pelvic and hip study in patient undergoing hip arthroscopy for FAI syndrome, by the same senior surgeon, between October 2015 and April 2016 was retrospectively reviewed to obtain a patient population. Radiographs were screened until 60 cases were obtained. We excluded any case having protrusio acetabuli, coxa profunda or having undergone previous osteotomic surgery. This study was performed according to the principles described in the 1964 Helsinki declaration and its later amendments.
Five observers (three orthopedic residents, one orthopedic surgeon and one senior surgeon) evaluated the data and received two anonymously labeled computer disk containing anonymized images for each hip. The observers were classified according to the above-described classification. Repeated evaluations performed at 4 weeks from the first analysis were used for intraobserver reliability, while only the initial evaluation was used for interobserver reliability for the study endpoint. A total of 300 classification forms, for each evaluation, were therefore completed and submitted to statistical analysis.
Our radiographic examination was based on the following three-view pelvic and hip study: anteroposterior view (AP) according to Siebenrock et al. [8], Dunn [9] view and Lequesne false profile [10] view.
By means of these three views, the femoral head–neck junction and the acetabular rim were evaluated at different degrees of rotation, for the presence of abnormalities and/or circumferential prominences.
Both cam and the pincer morphologies were classified in three stages of severity.
The anteroposterior and the Dunn views were used for the classification of the cam morphology. On the AP view, we drew three parallel lines, from medial to lateral, perpendicular to the neck axis. A first line “a” was drawn passing through the point of loss of sphericity of the femoral head [11], a second line “c” was drawn through the femoral neck isthmus and a third line “b” was drawn at the midpoint between line “a” and “c.”
The three stages of classification are defined as follows (Fig. 1):
-
Cam 1 deformity between line “a” and “b”;
-
Cam 2 deformity between line “b” and “c”;
-
Cam 3 deformity beyond line “c.”
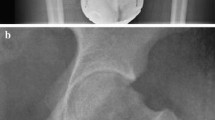
The same procedure was applied to the Dunn projection. We defined as cam 1 even all the deformities that were seen exclusively on the Dunn view, despite their extension (Fig. 2).
Cam classification. AP X-ray right hip. Line “a” is drawn passing through the point of loss of sphericity of the femoral head [11], line “c” is drawn through the femoral neck isthmus and line “b” is drawn at the midpoint between line “a” and “c”
For the classification of the pincer morphology, we relied on the lateral center edge angle of Wiberg (LCEA) modified by Ogata et al. [12] and the anterior center edge angle of Lequesne (ACAE).
Once the LCEA was identified on the AP view, we drew two other angles measuring half the LCEA, thus identifying three lines “a,” “b” and “c.”
The pincer morphology was classified as follows (Fig. 3):
-
Pincer 1 deformity between line “a” and “b”;
-
Pincer 2 deformity between line “b” and “c”;
-
Pincer 3 deformity beyond line “c.”
The measures were repeated on the false profile view using the ACE angle.
For better characterization of the pincer deformity, all the cases where the only radiological evidence was a positive crossover sign were defined as pincer 1 (Fig. 4).
We developed our classification on a radiographic study that can provide a three-dimensional analysis of the hip: the AP, false profile and Dunn view [13]. We found that a critical point in classifying cam morphology, according to our method, was the identification of the isthmus. It can simply be defined as the narrowest area of the femoral neck. Anyway, in a short femoral neck, or in the presence of a pistol grip deformity, proper identification of the isthmus can be difficult. In those cases, we therefore relied on the medial cortex of the femoral neck to identify this landmark. We outlined the isthmus drawing a line, perpendicular to the femoral neck axis, from the most lateral point on the medial cortex (Fig. 5). We found this technique ensures a more reproducible identification of the neck isthmus even in difficult cases.
The pincer morphology was analyzed in the AP and the false profile views. The AP view is either helpful to analyze the version of the acetabulum with the crossover sign, posterior wall sign and prominent ischial spine sign. We based the classification on two known and reliable parameters: the LCEA and the ACEA. We used the modified method by Ogata [12] to correctly identify the LCEA that provides real support to the femoral head, therefore better identifying the bony prominence to be removed. In the presence of os acetabuli, we decided to include it in the LCEA or ACEA when it was not completely detached from the acetabular rim. Otherwise, it was not included in the angle measurement.
The average pairwise Cohen’s kappa test and the average pairwise percent agreement were used to determine both inter- and intraobserver reliability for the classification. We used the Landis and Koch [14] guidelines to categorize the kappa value and define the strength of agreement for the classification, with values of 0.81–1.00 indicating excellent agreement, 0.61–0.80 substantial agreement, 0.41–0.60 moderate agreement, 0.21–0.40 fair agreement and 0–0.20 slight agreement.
Results
The average age of all patients was 38.7 ± 11.6 (range 19–66), and 36 (60%) were male. For the cam classification model, of the entire group of 300 forms analyzed, 138 (46%) reported a Cam 1; 69 (23%) a Cam 2; 48 (16%) a Cam 3; and 45 (15.00%) no Cam deformity.
When the interobserver agreement was evaluated for the classification of the cam morphology, the average pairwise Cohen’s kappa was 0.846 (range 0.734–0.929) and the average pairwise percent agreement was 89.4%. For all these factors therefore, the reliability of the classification was evaluated as excellent.
For the pincer classification model, 246 (82%) of the 300 analyzed forms reported a pincer 1; 24 (8%) a pincer 2; 15 (5%) a pincer 3; and 15 (5%) no pincer deformity.
The average pairwise Cohen’s kappa, for the evaluation of the interobserver agreement for the pincer type, was 0.838 (range 0.764–0.944), and the average pairwise percent agreement was 95.5%. Again, the reliability of the classification was evaluated as excellent.
At the second evaluation, performed 4 weeks after the first assessment, to evaluate only the intraobserver reliability, the average percent intraobserver agreement was 84.5% (range 78.3–90%) for the cam and 87% (range 83.3–93.3%) for the pincer classification.
Discussion
Classifications should be useful to clinicians in order to use a common language and correlate with prognostic patterns. In FAI syndrome, however, so many variables are used to describe the anatomy and identify the presence of the impingement, the majority of them related to head sphericity and based on single-plane radiographs. It is widely known in the literature that a classification based only on a single-plane radiograph cannot be useful [15].
There is not, actually, a proper classification for FAI syndrome that can describe both sides of the pathology. Ipach et al. [6, 7] proposed a classification only for the pistol grip deformity. It is a three-step classification based on the alpha angle and the head ratio measurements. This system describes the severity of the femoral deformity in three stages from none to moderate and strong deformity (Figs. 6, 7). The Ipach study has the limitation of a classification based only on a comparison between two observers, and it does not analyze the acetabulum at all. They reported a very low interobserver and intraobserver agreement for alpha angle and head ratio. Bouma et al. [5] proposed a new parameter based on CT scans: the omega zone that combines the alpha angle, the LCEA, acetabular and femoral version and neck-shaft angle. As a major limitation anyway, their study did not evaluate other impingement patterns but cam morphology. Arbabi et al. [16] studied virtual hip models where all morphology parameters were kept constant except alpha angle and LCEA. Collision detection algorithms demonstrated two types of penetration of the two rotating bodies, named radial and curvilinear, for cam and pincer morphologies, respectively. This method is interesting for detecting the presence of cam or pincer impingement but it has only been studied on geometrical models created with CAD software, and it is only focused on LCEA and alpha angle. Our classification has the advantage of being simpler and requiring less software processing. Chadayamurri et al. [17] demonstrated that measured values of the LCEA are consistently inflated on CT scan compared to X-ray on a wide variety of hip conditions, highlighting the need for standardization and validation of CT-based measurements. Schottel et al. [18] demonstrated how LCEA and alpha angle show excellent levels of inter- and intraobserver agreement for the measurement on plain radiographs, despite the observers’ experience. Nepple et al. [19] showed how alpha angle measurements demonstrated only moderate interobserver reliability, despite excellent intraobserver reliability.
This is the first study proposing this type of classification, where the study group concentrated on defining the border between normal and pathologic conditions. Our study has, however, some limitations. A first limitation was the absence of another comparable classification for FAI syndrome, to understand which one could have better reliability. Another limitation in the study design was the limited number of cases and observers and the lack of a clinical correlation. Finally, there was a steep but short learning curve in identifying the radiological bony landmarks that could significantly alter the results.
Our proposed classification system for FAI syndrome demonstrated excellent levels of inter- and intraobserver reliability for cam and pincer morphologies. However, this classification is dependent from the quality of the radiographic study. This classification can be considered a useful tool in assessing hip and pelvic morphology and in planning surgery. Further studies are needed to correlate the classification with specific intraoperative findings, such as labral tears or chondral lesions, and to therefore achieve a corresponding treatment algorithm.
References
Ganz R, Parvizi J, Beck M et al (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. https://doi.org/10.1097/01.blo.0000096804.78689.c2
Leunig M, Ganz R (2005) Femoroacetabular impingement. A common cause of hip complaints leading to arthrosis. Unfallchirurg 108:9–10, 12–17. https://doi.org/10.1007/s00113-004-0902-z
Rühmann O (2008) Arthroscopy of the hip joint: indication, technique, results. Dtsch Ärzteblatt Int 105:559–566. https://doi.org/10.3238/arztebl.2008.0559
Pollard TCB, Villar RN, Norton MR et al (2010) Femoroacetabular impingement and classification of the cam deformity: the reference interval in normal hips. Acta Orthop 81:134–141. https://doi.org/10.3109/17453671003619011
Bouma HW, Hogervorst T, Audenaert E et al (2015) Can combining femoral and acetabular morphology parameters improve the characterization of femoroacetabular impingement? Clin Orthop Relat Res 473:1396–1403. https://doi.org/10.1007/s11999-014-4037-4
Ipach I, Mittag F, Sachsenmaier S et al (2011) A new classification for “pistol grip deformity”—correlation between the severity of the deformity and the grade of osteoarthritis of the hip. RöFo Fortschritte auf dem Gebiete der Röntgenstrahlen und der Nukl 183:365–371. https://doi.org/10.1055/s-0029-1245817
Ipach I, Arlt E-M, Mittag F et al (2011) A classification-system improves the intra- and interobserver reliability of radiographic diagnosis of “pistol-grip-deformity”. Hip Int 21:732–739. https://doi.org/10.5301/HIP.2011.8821
Siebenrock KA, Kalbermatten DF, Ganz R (2003) Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res 407:241–248
Dunn DM (1952) Anteversion of the neck of the femur; a method of measurement. J Bone Jt Surg Br 34-B:181–186
Lequesne M, de Seze (1961) False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies. Rev du Rhum des Mal ostéo-articulaires 28:643–652
Rippstein J (1955) Determination of the antetorsion of the femur neck by means of two X-ray pictures. Z Orthop Ihre Grenzgeb 86:345–360
Ogata S, Moriya H, Tsuchiya K et al (1990) Acetabular cover in congenital dislocation of the hip. J Bone Jt Surg Br 72:190–196
Goodman DA, Feighan JE, Smith AD et al (1997) Subclinical slipped capital femoral epiphysis. Relationship to osteoarthrosis of the hip. J Bone Jt Surg Am 79:1489–1497
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Meyer DC, Beck M, Ellis T et al (2006) Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res 445:181–185. https://doi.org/10.1097/01.blo.0000201168.72388.24
Arbabi E, Chegini S, Boulic R et al (2010) Penetration depth method—novel real-time strategy for evaluating femoroacetabular impingement. J Orthop Res 28:880–886. https://doi.org/10.1002/jor.21076
Chadayammuri V, Garabekyan T, Jesse M-K et al (2015) Measurement of lateral acetabular coverage: a comparison between CT and plain radiography. J Hip Preserv Surg 2:392–400. https://doi.org/10.1093/jhps/hnv063
Schottel PC, Park C, Chang A et al (2014) The role of experience level in radiographic evaluation of femoroacetabular impingement and acetabular dysplasia. J Hip Preserv Surg 1:21–26. https://doi.org/10.1093/jhps/hnu005
Nepple JJ, Martell JM, Kim Y-J et al (2014) Interobserver and intraobserver reliability of the radiographic analysis of femoroacetabular impingement and dysplasia using computer-assisted measurements. Am J Sports Med 42:2393–2401. https://doi.org/10.1177/0363546514542797
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fioruzzi, A., Acerbi, A., Jannelli, E. et al. Interobserver and intraobserver reliability of a new radiological classification for femoroacetabular impingement syndrome. Musculoskelet Surg 104, 279–284 (2020). https://doi.org/10.1007/s12306-019-00618-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-019-00618-x