Abstract
Summary
Denosumab discontinuation results in accelerated bone remodeling, decreased bone mineral density (BMD), and an increased risk of multiple vertebral fractures. Bisphosphonates are at least partially effective at inhibiting these consequences but there have been no randomized clinical trials assessing the efficacy of alternative antiresorptives.
Purpose
The aim of this study was to evaluate the comparative efficacy of alendronate and the SERM, raloxifene, in preventing the post-denosumab high-turnover bone loss.
Methods
We conducted an open-label randomized controlled trial in which 51 postmenopausal women at increased risk of fracture were randomized with equal probability to receive 12-months of denosumab 60-mg 6-monthly followed by 12-months of either alendronate 70-mg weekly or raloxifene 60-mg daily. Serum bone remodeling markers were measured at 0,6,12,15,18, and 24 and areal BMD of the distal radius, spine, and hip were measured at 0,12,18 and 24 months.
Results
After denosumab discontinuation, serum markers of bone remodeling remained suppressed when followed by alendronate, but gradually increased to baseline when followed by raloxifene. In the denosumab-to-alendronate group, denosumab-induced BMD gains were maintained at all sites whereas in the denosumab-to-raloxifene group, BMD decreased at the spine by 2.0% (95% CI -3.2 to -0.8, P = 0.003) and at the total hip by 1.2% (-2.1 to -0.4%, P = 0.008), but remained stable at the femoral neck and distal radius and above the original baseline at all sites. The decreases in spine and total hip BMD in the denosumab-to-raloxifene group (but not the femoral neck or distal radius) were significant when compared to the denosumab-to-alendronate group.
Conclusions
These results suggest that after one year of denosumab, one year of alendronate is better able to maintain the inhibition of bone remodeling and BMD gains than raloxifene.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Denosumab, a fully human monoclonal antibody that binds to and inhibits the receptor activator of nuclear factor kappa-B ligand (RANKL), is a widely used osteoporosis medication that increases bone mineral density (BMD), improves bone microarchitecture, and significantly reduces the risk of vertebral, hip, and non-vertebral fracture [1,2,3,4].
Denosumab acts by blocking the binding of RANKL to its receptor on pre-osteoclasts and osteoclasts, the final common pathway leading to osteoclast activation and bone resorption [5, 6]. It produces almost complete and sustained suppression of bone remodeling to a greater degree than both intravenous and oral bisphosphonates [7, 8]. In iliac crest bone biopsy specimens taken from postmenopausal women with osteoporosis who had been taking denosumab for 24–36 months, there was an 80% reduction in eroded surface and complete absence of osteoclasts in more than 50% of the specimens [8]. Discontinuation of denosumab, however, results in a rapid reversal of its antiresorptive effects, a transitory overshoot of serum bone remodeling markers to above the pre-treatment baseline, and a progressive decrease in BMD [9,10,11,12,13]. This reversal of the skeletal benefits achieved with denosumab appears to be lost even after a very short duration (12 months) of treatment with denosumab [14]. Of greater concern, post hoc analyses of the large phase 3 randomized controlled trial of denosumab (FREEDOM) reported that when denosumab is discontinued, there is an immediate loss in vertebral anti-fracture efficacy as well as a significant increase in the incidence of patients experiencing multiple vertebral fractures versus those originally assigned to placebo [15,16,17].
Given the above findings, determining the ideal sequence of therapy after denosumab is crucial. Clinical trials that have evaluated the efficacy of follow-up therapy with oral and parenteral bisphosphonates to maintain denosumab-induced BMD gains have reported preservation of BMD for at least 12 months after patients have transitioned from short-term denosumab to either oral alendronate or intravenous zoledronate [18,19,20,21]. However, in trials where patients have received a longer duration of denosumab (> 3 years), follow-up therapy with bisphosphonates have not been as effective in maintaining denosumab-induced BMD gains [22,23,24,25]. For patients who are unwilling or unable to tolerate bisphosphonate therapy, there have been no prospective trials assessing the efficacy of alternative antiresorptive drugs, such as selective estrogen receptor antagonists (SERMs). The aim of this study was to determine the comparative efficacy of the oral bisphosphonate, alendronate, and the SERM, raloxifene, when used in sequence with short-term denosumab. Specifically, we hypothesized that in postmenopausal women with osteoporosis who received denosumab for one year, alendronate would more effectively inhibit bone remodeling and maintain denosumab-induced gains in BMD compared to raloxifene.
Methods
Study design and participants
The Comparison of Alendronate or Raloxifene following Denosumab (CARD) study was a 24-month randomized, two-arm, open label study conducted at Massachusetts General Hospital, an academic hospital in Boston, Massachusetts.
From November 2018 to January 2020, women aged 45 years and older were recruited via targeted commercial mailings and referrals from an endocrine osteoporosis clinic. Eligible women were postmenopausal (defined as more than 36 months since last spontaneous menses or > 36 months since hysterectomy with bilateral oophorectomy plus serum FSH > 40 units / liter) and at increased risk of fracture defined as having at least one of the following three criteria: (i) spine or hip T-score <—2.5 SD; (ii) personal history of spine or hip fracture; or (iii) high fracture risk consistent with National Osteoporosis Foundation guidelines (spine or hip T-score between -1.0 and—2.5 SD and a 10-year hip fracture probability ≥ 3% or a 10-year major osteoporosis-related fracture probability ≥ 20% based on the US-adapted fracture risk model, FRAX®). Hip fractures had to have occurred more than 12 months prior to enrollment. Women were excluded if they had current use or use in the past 12 months of oral bisphosphonates, teriparatide, abaloparatide or denosumab. Additionally, study participants were excluded if they had known congenital or acquired bone disease other than osteoporosis, a history of malignancy or radiation therapy, significant cardiopulmonary disease, major psychiatric disease, major alcohol and substance use, or any other condition that the investigator deemed may preclude the participant from participating safely or completing the protocol procedures.
The study protocol was approved by the Mass General Brigham Institutional Review Board and is registered with ClinicalTrials.gov, number NCT03623633. All study participants had to provide written informed consent before enrollment in the study.
Randomization and masking
Eligible participants were stratified by previous bisphosphonate use (previous use or none) and then randomly assigned within each stratum to one of the two treatment groups by computer-generated cards in a 1:1 ratio. Outcome assessors and the laboratory performing the laboratory tests were blinded to group assignment.
Study procedures
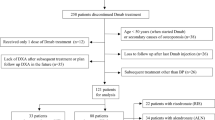
Study participants were randomized to receive denosumab 60-mg subcutaneously every 6 months for 12-months followed by 12-months of either alendronate 70-mg weekly or raloxifene 60-mg daily (Fig. 1). Adherence to alendronate and raloxifene were assessed by self-reported diary which was reviewed at each study visit. Average adherence rates were 98.7% for alendronate and 98.3% for raloxifene. All participants who reported a dietary intake of less than 1200 mg of calcium daily were given calcium supplementation (600 mg elemental calcium) to achieve an intake of 1200 mg of calcium daily. All participants received 400 IU of vitamin D. Study visits were conducted at 0, 6, 12, 15, 18, and 24 months. Blood collection was performed at each visit and bone density measurements by dual energy x-ray absorptiometry (DXA) were performed at 0, 12, 18, and 24 months. Vertebral Fracture Assessment (VFA) by DXA was completed at months 12 and 24. A semiquantitative method was used to determine the incidence of vertebral fractures between 12 and 24 months.
Trial Schema of the 24-month open label randomized controlled trial. At baseline, all participants were randomized with equal probability to receive denosumab 60-mg at 0 and 6 months, followed by either alendronate 70-mg weekly or raloxifene 60-mg daily for 12-months. Serum bone turnover markers (CTX and PINP) were measured at each time point; bone mineral density was measured by DXA at the lumbar spine, hip, and distal one-third of the radius shaft at 0,12,18, and 24 months; VFA was conducted at 12 and 24 months
Fasting morning blood samples were collected and stored at -70 °C. Measurements of serum bone remodeling markers, serum cross-linked C-telopeptide of type I collagen (CTX) and procollagen N-propeptide of type I collagen (PINP), were conducted as a batch analysis at the conclusion of the study by electrochemiluminescence (iSYS, Immunodiagnostic Systems, Scottsdale, AZ, USA). The inter- and intra-assay coefficients of variation (CVs) were 6.0% and 3.2% for CTX and 5.0% and 2.9% for PINP.
Areal bone mineral density (BMD) of the posterior-anterior lumbar spine (PA spine), total hip, femoral neck, and distal one-third of the radius shaft was measured by DXA using a Hologic densitometer (Hologic, Marlborough, MA). Vertebra with obvious deformities or focal sclerosis were excluded from all analyses (1 woman in each group). Based on our center’s precision study, our short-term precision coefficient of variation (CV) for in vivo reproducibility is 0.54% for PA spine, 0.74% for total hip, 1.29% for femoral neck, and 3.17% for distal one-third radius, corresponding to a least significant change (LSC) of 0.014 g/cm2, 0.018 g/cm2, 0.025 g/cm2, and 0.020 g/cm2, respectively.
Adverse events including bone fractures were documented at each visit. Any serious adverse event that occurred during the study was reviewed by an independent data and safety monitoring board.
Outcomes
The outcome measures for this study were the between group differences in serum biochemical markers of bone remodeling (primary) as well as between group differences in DXA-derived spine and hip areal bone mineral density.
Statistical analysis
With a sample size of 20 participants per group, the study was powered to detect a between-group difference of 20% in serum CTX between month 12 (6-months after the final denosumab injection) and month 18, based on a standard deviation of 22%, and with 80% power at a significance level of 5%. Statistical analysis of the time-specific treatment effects (0–24 months, 12–18 months, and 12–24 months) of the denosumab-to-alendronate group compared to the denosumab-to-raloxifene group were assessed by analysis of variance (ANOVA) based on a modified intention to treat principle, where all participants who completed at least one visit after month 12 (cessation of denosumab and randomization to alendronate or raloxifene) were included in the analysis set. A p value of 0·05 or less was considered to indicate statistical significance. Data are presented as mean (SD) for endpoints with a normal distribution and as median (IQR) for endpoints without a normal distribution. For illustration purposes, changes in bone density parameters are shown as percent change (95% confidence interval, CI) from baseline. Statistical analysis was done with SAS (version 9.2).
Role of the funding source
The funders had no role in the study design, data collection, analyses, nor interpretation of the study results, nor in the writing of this manuscript.
Results
Fifty-one women enrolled in the study and were randomly allocated, in a 1:1 ratio, to receive 12 months of either alendronate 70-mg weekly (n = 26) or raloxifene 60-mg daily (n = 25) after 12 months of denosumab treatment. Of the 51 women who enrolled in the study, 48 women (94%) completed at least one study visit after month 12 and were included in the primary analysis. The demographic and baseline characteristics of the study participants are presented in Table 1. Study participants had an average age of 65.8 (5.2) years, 92% were white, 39% had a prevalent fragility fracture after the age of 45 years, and 33% had previously been treated with an oral bisphosphonate. Clinical characteristics were similar between groups apart from BMD at the femoral neck, which was significantly higher in the denosumab-to-raloxifene group (Fig. 2).
Changes in serum bone remodeling markers, CTX and PINP, are shown in Fig. 3. Treatment with denosumab decreased levels of CTX and PINP to a similar extent in both groups, and levels remained suppressed at all measured timepoints during the 12-month treatment period. After the transition, CTX and PINP levels remained suppressed at all time points in the denosumab-to-alendronate group. In the denosumab-to-raloxifene group, both CTX and PINP levels gradually increased and returned to baseline levels over 6 to 12 months. There was no overshoot in bone remodeling markers observed in either group.
Median value of serum bone remodeling markers, CTX (A) and PINP (B). Error bars show 95% CI. CTX = cross linked C-telopeptide of type I collagen; PINP = procollagen N-propeptide of type I collagen. *P < 0.001 for between-group comparison from month 0. #P < 0.05 for between-group comparison from month 12
Longitudinal changes in BMD at the PA spine, hip, and distal one-third of the radius shaft are shown in Fig. 4. Twelve months of denosumab increased BMD at the PA spine, total hip and femoral neck similarly in both groups. Conversely, BMD at the distal one-third of the radius shaft decreased in both groups. After the transition, denosumab-induced gains in BMD were maintained over 12 months at all measured sites in the denosumab-to-alendronate group. In the denosumab-to-raloxifene group, however, BMD decreased at the PA spine by 2.0% (95% CI -3.2 to -0.8, P = 0.003 for 12–24 month within group comparison) and at the total hip by 1.2% (95% CI -2.1 to -0.4%, P = 0.008 for 12–24 month within group comparison) but was maintained at the femoral neck and distal one-third of the radius shaft. From 12 to 24 months, the mean differences in BMD change in the denosumab-to-alendronate group compared to the denosumab-to-raloxifene group were 2.9% (95% CI 1.4 to 4.5%, P < 0.001) at the PA spine; 1.2% (95% CI 0.2 to 2.3%, P = 0.02) at the total hip; 0.6% (95% CI—1.8 to 3.0%, P = 0.6) at the femoral neck, and 0.3% (95% CI – 1.1 to 1.7%, P = 0.6) at the distal one-third of the radius shaft. In both groups, BMD remained above the pre-treatment baseline (0 months) at the PA spine and hip sites. Given the significant between group difference in femoral neck BMD at baseline, femoral neck outcomes were also re-analyzed after adjustment for baseline femoral neck BMD and showed similar results (data not shown).
Mean percentage change in areal bone mineral density (aBMD) of the lumbar spine (A), distal one-third of the radius shaft (B), total hip (C), and femoral neck (D). Error bars show 95% CI. *P < 0.05, **P = 0.07, ***P = 0.09 for between-group comparison from month 0. #P < 0.05 for between-group comparison from month 12
An exploratory analysis of the percent of participants who had > 3% BMD loss at the PA spine, total hip, and femoral neck was calculated for all participants who completed baseline, month 12, and month 24 study visits. A 3% threshold was predetermined based on the widely accepted least significant change in DXA BMD measurements, which assumes a DXA precision error of 1% [26]. From 12 to 24 months, the number of participants with > 3% loss of BMD at the PA spine was 1 (4%) in the denosumab-to-alendronate group versus 6 (29%) in the denosumab-to-raloxifene group, P = 0.04. The number of participants with > 3% loss at the total hip was 0 in the denosumab-to-alendronate group compared to 5 (23%) in the denosumab-to-raloxifene group, P = 0.02. The number of participants with > 3% loss at the femoral neck was 1 (4%) in the denosumab-to-alendronate group compared to 5 (23%) in the denosumab-to-raloxifene group, P = 0.08.
The incidence rate of treatment related non-serious adverse events was 19 events in 12 women in the denosumab-to-alendronate group and 21 events in 15 women in the denosumab-to-raloxifene group (Table 2). All cases of constipation (n = 5) and gastro-esophageal reflux disease (n = 4) were reported in the denosumab-to-alendronate group, and all cases of hot flashes were reported in the denosumab-to-raloxifene group (n = 6). Serious adverse events, unrelated to the treatment intervention, occurred in 2 participants in the denosumab-to-alendronate group (one woman had diverticulitis with a bowel perforation and the other had palpitations and dyspnea associated with a known mitral valve prolapse) and 1 participant in the denosumab-to-raloxifene group (death after a motor vehicle accident). Between 0 to 12 months (denosumab phase), 2 participants in the denosumab-to-alendronate group had a humerus fracture and 1 participant in the denosumab-to-raloxifene group had simultaneous fractures of the femoral condyle and lateral tibial plateau. Between 12 to 24 months (transition phase), no clinical fractures were reported in either group. Study participants had a vertebral fracture assessment (VFA) at 12 and 24 months. Only 1 participant in the denosumab-to-alendronate group had a new thoracic (T9) fracture assessed by VFA performed at 24 months. Formal comparisons of safety and fracture events between the denosumab-to-alendronate and denosumab-to-raloxifene groups are not possible because of the limited sample size.
Discussion
In this study, we report that in postmenopausal women with osteoporosis who discontinued denosumab after 12 months, alendronate was better able to suppress bone remodeling and maintain the denosumab-induced gains in BMD compared to raloxifene.
Discontinuation of denosumab, after 2 years of treatment, results in a transitory overshoot in serum bone remodeling markers to above pre-treatment baseline levels and an accompanying decrease in BMD [9]. The underlying molecular and cellular mechanisms responsible for this overshoot are not fully defined though reports from preclinical studies suggests that an increase in the osteoclast precursor pool [27], an increase in the RANKL:OPG ratio [28], and a decrease in the number of osteocytes and osteoblasts in the initial phase after denosumab discontinuation [29] may all play a role. The benefits observed with alendronate over raloxifene in our study are likely due to the greater suppression of bone remodeling achieved with alendronate compared to raloxifene [30, 31]. In our study, alendronate was able to maintain suppression of bone remodeling similar to what was achieved during treatment with denosumab. Raloxifene, however, was not able to maintain the same degree of bone remodeling suppression, and within 3 months of transitioning from denosumab to raloxifene, there was a significant increase in both CTX and PINP, with levels gradually increasing to baseline at 24 months. There was no overshoot in bone remodeling markers observed during treatment with raloxifene. However, as there was no placebo group in our study, it is not known whether the overshoot in bone remodeling occurs after 12 months of treatment with denosumab (as has been described with denosumab cessation after 24 months of treatment) [9]. This observation is in contrast to reports from two recently published retrospective studies, where raloxifene did not prevent the overshoot in bone remodeling in postmenopausal women with osteoporosis who transitioned to raloxifene 60-mg daily after an average of 12–18 months of denosumab [32, 33]. The reasons for this discrepancy are unclear but could be due to slightly different durations of denosumab treatment (women in these studies had up to 5 doses of denosumab whereas women in our study received 2 doses). In addition, given the retrospective nature of these studies, there may be confounding variables that have not been accounted for.
As expected, 12 months of denosumab resulted in BMD increases at the PA spine and hip. These gains in BMD are comparable to those reported in the landmark FREEDOM trial in postmenopausal women with osteoporosis who received denosumab 60-mg 6-monthly [4]. After the transition, consistent with the observed changes in serum bone remodeling markers, denosumab-induced BMD increases at the PA spine and total hip were better maintained in those who transitioned to alendronate compared to those who transitioned to raloxifene. At the end of the 24-month study period, PA spine and total hip BMD were significantly increased in the denosumab-to-alendronate group compared to the denosumab-to-raloxifene group. Overall BMD at the femoral neck and distal one-third of the radius shaft were similarly maintained in both groups, though there was a wide variation among individuals. Some of this variation is likely due to greater measurement error at the femoral neck and radius sites. Importantly, in both groups, after the transition from denosumab to either alendronate or raloxifene, BMD remained above the pre-treatment baseline at all sites. Our study results are similar to previously published reports from studies that have evaluated the efficacy of alendronate or raloxifene in maintaining BMD after cessation of denosumab. For example, in the multi-center Denosumab Adherence Preference Satisfaction (DAPS) study of 126 postmenopausal women [20], BMD gains at the spine and hip after 12 months of denosumab were maintained in the 115 women who transitioned to alendronate for 12 months. In a retrospective study of 66 postmenopausal women in Korea [33], after 1:1 propensity score matching, bone density loss at the lumbar spine was attenuated in those who transitioned from denosumab (1–4 doses) to raloxifene compared to those who did not receive any sequential treatment (2.8% versus 5.8%, P = 0.01), whereas BMD loss at the total hip did not differ between the two groups (1.4% versus 1.4%, P = 1.0) [33].
The ability of raloxifene to partially maintain BMD gains may be clinically significant. Many patients are unable to tolerate oral bisphosphonates, mainly due to upper gastrointestinal adverse effects such as nausea, dyspepsia, abdominal pain, and gastritis [34,35,36]. Intravenous bisphosphonates are also associated with an acute phase reaction (fever, headache, myalgia, and arthralgia) in approximately one-third of patients receiving their first infusion of zoledronic acid, though this incidence declines progressively with subsequent infusions [37]. Moreover, even in those without an absolute contraindication to bisphosphonate therapy, many patients often refuse to take these medications due to concerns of rare but serious side effects such as atypical femoral fractures and osteonecrosis of the jaw [38, 39]. It should be noted, however, that raloxifene may not be a suitable alternative for everyone, as there are off-target effects, such as an increased risk of venous thromboembolic events and hot flashes, that need to be considered when assessing the suitability of this drug for patients [40, 41]. In addition, raloxifene has been shown to reduce vertebral fracture risk but not non-vertebral fracture risk and may not be suitable for patients at high risk of non-vertebral fractures who discontinue denosumab [40].
This study has some limitations. First, our study did not have an untreated or placebo-controlled group (which would have been ethically impermissible), so the effects on bone remodeling markers and BMD following cessation of denosumab after 12 months of treatment are not known. Second, as the women in our study were treated with denosumab for 12 months, the effects of alendronate and raloxifene may differ in individuals who discontinue denosumab after a longer duration of treatment. Finally, this was a relatively small study limited to serum markers of bone remodeling and BMD as endpoints. Although our sample size estimate was based on the between-group difference in CTX, our study size was 80% powered to detect a between-group difference of at least 1.4% at the total hip and 2.1% at the lumbar spine between 12 and 24 months. It is of interest that raloxifene, in addition to its antiresorptive properties, has also been reported to improve bone toughness in a cell-independent manner by increasing matrix bound water and modifying collagen nanomorphology to resist fracture [42]. Therefore, fracture risk reduction with raloxifene may not be entirely explained by its effects on BMD. Additional studies are needed to address whether the differential effects of alendronate and raloxifene observed in this study will translate into differences in fracture outcomes.
In conclusion, in postmenopausal women with osteoporosis who discontinue short-term denosumab treatment and who are unable or unwilling to transition to a bisphosphonate, raloxifene may be a suitable though likely inferior alternative. Larger and more diverse clinical trials that can adequately assess the capacity of follow-up SERM therapy to reduce the risk of multiple vertebral fractures after denosumab discontinuation would be extremely helpful to physicians as would studies in patients who have discontinued denosumab after a longer duration of treatment, which occurs more commonly in clinical practice.
Financial support for the study
This project was supported by Amgen, NIH NIAMS K24AR067847 (BZL), and NIH NCATS 1UL1TR002541-01.
Change history
09 November 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00198-023-06966-6
References
Bone HG, Wagman RB, Brandi ML et al (2017) 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol 5:513–523
Tsai JN, Uihlein AV, Burnett-Bowie SM, Neer RM, Derrico NP, Lee H, Bouxsein ML, Leder BZ (2016) Effects of Two Years of Teriparatide, Denosumab, or Both on Bone Microarchitecture and Strength (DATA-HRpQCT study). J Clin Endocrinol Metab 101:2023–2030
McClung MR, Lewiecki EM, Cohen SB et al (2006) Denosumab in postmenopausal women with low bone mineral density. N Engl J Med 354:821–831
Cummings SR, San Martin J, McClung MR et al (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Lacey DL, Timms E, Tan HL et al (1998) Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell 93:165–176
Yasuda H, Shima N, Nakagawa N et al (1998) Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci U S A 95:3597–3602
Brown JP, Prince RL, Deal C et al (2009) Comparison of the effect of denosumab and alendronate on BMD and biochemical markers of bone turnover in postmenopausal women with low bone mass: a randomized, blinded, phase 3 trial. J Bone Mineral Res 24:153–161
Reid IR, Miller PD, Brown JP et al (2010) Effects of denosumab on bone histomorphometry: the FREEDOM and STAND studies. J Bone Miner Res 25:2256–2265
Bone HG, Bolognese MA, Yuen CK, Kendler DL, Miller PD, Yang YC, Grazette L, San Martin J, Gallagher JC (2011) Effects of denosumab treatment and discontinuation on bone mineral density and bone turnover markers in postmenopausal women with low bone mass. J Clin Endocrinol Metab 96:972–980
Miller PD, Bolognese MA, Lewiecki EM, McClung MR, Ding B, Austin M, Liu Y, San Martin J, Amg Bone Loss Study G (2008) Effect of denosumab on bone density and turnover in postmenopausal women with low bone mass after long-term continued, discontinued, and restarting of therapy: a randomized blinded phase 2 clinical trial. Bone 43:222–229
McClung MR, Wagman RB, Miller PD, Wang A, Lewiecki EM (2017) Observations following discontinuation of long-term denosumab therapy. Osteoporos Int 28:1723–1732
Zanchetta MB, Boailchuk J, Massari F, Silveira F, Bogado C, Zanchetta JR (2018) Significant bone loss after stopping long-term denosumab treatment: a post FREEDOM study. Osteoporos Int 29:41–47
Brown JP, Dempster DW, Ding B, Dent-Acosta R, San Martin J, Grauer A, Wagman RB, Zanchetta J (2011) Bone remodeling in postmenopausal women who discontinued denosumab treatment: off-treatment biopsy study. J Bone Miner Res 26:2737–2744
Seeman E ZR, Zanchetta JR, Hanley DA, Wang A, Libanti C, Wagman RB (2017) Bone microarchitecture after discontinuation of denosumab in postmenopausal women with low bone mass. J Bone Miner Res 31:Supplement 1
Brown JP, Roux C, Torring O et al (2013) Discontinuation of denosumab and associated fracture incidence: analysis from the Fracture Reduction Evaluation of Denosumab in Osteoporosis Every 6 Months (FREEDOM) trial. J Bone Miner Res 28:746–752
Cummings SR, Ferrari S, Eastell R et al (2018) Vertebral Fractures After Discontinuation of Denosumab: A Post Hoc Analysis of the Randomized Placebo-Controlled FREEDOM Trial and Its Extension. J Bone Miner Res 33:190–198
Cosman F, Huang S, McDermott M, Cummings SR (2022) Multiple Vertebral Fractures After Denosumab Discontinuation: FREEDOM and FREEDOM Extension Trials Additional Post Hoc Analyses. J Bone Miner Res 37:2112–2120
Anastasilakis AD, Papapoulos SE, Polyzos SA, Appelman-Dijkstra NM, Makras P (2019) Zoledronate for the Prevention of Bone Loss in Women Discontinuing Denosumab Treatment. A Prospective 2-Year Clinical Trial. J Bone Miner Res 34:2220–2228
Makras P, Papapoulos SE, Polyzos SA, Appelman-Dijkstra NM, Anastasilakis AD (2020) The three-year effect of a single zoledronate infusion on bone mineral density and bone turnover markers following denosumab discontinuation in women with postmenopausal osteoporosis. Bone 138:115478
Kendler D, Chines A, Clark P, Ebeling PR, McClung M, Rhee Y, Huang S, Stad RK (2020) Bone mineral density after transitioning from denosumab to alendronate. J Clin Endocrinol Metab 105(3):e255–e264
Ramchand SK, David NL, Lee H, Eastell R, Tsai JN, Leder BZ (2021) Efficacy of Zoledronic Acid in Maintaining Areal and Volumetric Bone Density After Combined Denosumab and Teriparatide Administration: DATA-HD Study Extension. J Bone Miner Res 36:921–930
Horne AM, Mihov B, Reid IR (2019) Effect of Zoledronate on Bone Loss After Romosozumab/Denosumab: 2-Year Follow-up. Calcif Tissue Int 105:107–108
Reid IR, Horne AM, Mihov B, Gamble GD (2017) Bone Loss After Denosumab: Only Partial Protection with Zoledronate. Calcif Tissue Int 101:371–374
Everts-Graber J, Reichenbach S, Ziswiler HR, Studer U, Lehmann T (2020) A Single Infusion of Zoledronate in Postmenopausal Women Following Denosumab Discontinuation Results in Partial Conservation of Bone Mass Gains. J Bone Miner Res 35:1207–1215
Solling AS, Harslof T, Langdahl B (2021) Treatment With Zoledronate Subsequent to Denosumab in Osteoporosis: A 2-Year Randomized Study. J Bone Miner Res 36:1245–1254
Bonnick SL, Johnston CC Jr, Kleerekoper M, Lindsay R, Miller P, Sherwood L, Siris E (2001) Importance of precision in bone density measurements. J Clin Densitom 4:105–110
McDonald MM, Khoo WH, Ng PY et al (2021) Osteoclasts recycle via osteomorphs during RANKL-stimulated bone resorption. Cell 184:1940
Fu Q, Bustamante-Gomez NC, Reyes-Pardo H et al (2023) Reduced osteoprotegrin expression by osteocytes may contribute to rebound resorption after denosumab discontinuation. J Clin Invest Insight 8(18):e167790. https://doi.org/10.1172/jci.insight.167790
Jahn-Rickert K, Wolfel EM, Jobke B, Riedel C, Hellmich M, Werner M, McDonald MM, Busse B (2020) Elevated Bone Hardness Under Denosumab Treatment, With Persisting Lower Osteocyte Viability During Discontinuation. Front Endocrinol 11:250
Johnell O, Scheele WH, Lu Y, Reginster JY, Need AG, Seeman E (2002) Additive effects of raloxifene and alendronate on bone density and biochemical markers of bone remodeling in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 87:985–992
Ott SM, Oleksik A, Lu Y, Harper K, Lips P (2002) Bone histomorphometric and biochemical marker results of a 2-year placebo-controlled trial of raloxifene in postmenopausal women. J Bone Miner Res 17:341–348
Ha J, Kim J, Jeong C, Lim Y, Kim MK, Kwon HS, Song KH, Kang MI, Baek KH (2022) Effect of follow-up raloxifene therapy after denosumab discontinuation in postmenopausal women. Osteoporos Int 33:1591–1599
Hong N, Shin S, Lee S, Kim KJ, Rhee Y (2022) Raloxifene Use After Denosumab Discontinuation Partially Attenuates Bone Loss in the Lumbar Spine in Postmenopausal Osteoporosis. Calcif Tissue Int 111:47–55
Greenspan S, Field-Munves E, Tonino R, Smith M, Petruschke R, Wang L, Yates J, de Papp AE, Palmisano J (2002) Tolerability of once-weekly alendronate in patients with osteoporosis: a randomized, double-blind, placebo-controlled study. Mayo Clin Proc 77:1044–1052
Harris ST, Watts NB, Genant HK et al (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA 282:1344–1352
Chesnut CH 3rd, Skag A, Christiansen C et al (2004) Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res 19:1241–1249
Black DM, Delmas PD, Eastell R et al (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Jha S, Wang Z, Laucis N, Bhattacharyya T (2015) Trends in Media Reports, Oral Bisphosphonate Prescriptions, and Hip Fractures 1996–2012: An Ecological Analysis. J Bone Miner Res 30:2179–2187
Black DM, Rosen CJ (2016) Postmenopausal Osteoporosis. N Engl J Med 374:2096–2097
Ettinger B, Black DM, Mitlak BH et al (1999) Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA 282:637–645
Martino S, Cauley JA, Barrett-Connor E, Powles TJ, Mershon J, Disch D, Secrest RJ, Cummings SR, Investigators C (2004) Continuing outcomes relevant to Evista: breast cancer incidence in postmenopausal osteoporotic women in a randomized trial of raloxifene. J Natl Cancer Inst 96:1751–1761
Gallant MA, Brown DM, Hammond M, Wallace JM, Du J, Deymier-Black AC, Almer JD, Stock SR, Allen MR, Burr DB (2014) Bone cell-independent benefits of raloxifene on the skeleton: a novel mechanism for improving bone material properties. Bone 61:191–200
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
JNT has a financial interest in Amgen. JNT’s interests were reviewed and are managed by MGH and Mass General Brigham in accordance with their conflict-of-interest policies. All other authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sabashini K. Ramchand and Joy N. Tsai are equal first authors.
The original online version of this article was revised: the ‘Co-first authorship’ note was missing, and should have read that Sabashini K. Ramchand and Joy N. Tsai are equal first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramchand, S.K., Tsai, J.N., Lee, H. et al. The comparison of alendronate and raloxifene after denosumab (CARD) study: A comparative efficacy trial. Osteoporos Int 35, 255–263 (2024). https://doi.org/10.1007/s00198-023-06932-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06932-2