Abstract
Summary
Change in total hip bone mineral density (BMD) provides a robust indication of anti-fracture effect during treatment monitoring in routine clinical practice, whereas spine BMD change is not independently associated with fracture risk.
Purpose
The role of monitoring bone mineral density (BMD) as an indicator of an anti-fracture effect is controversial. Discordance between the spine and hip BMD is common and creates uncertainty in clinical practice.
Methods
Using a population-based BMD Registry for the Province of Manitoba, Canada, we compared change in the spine and hip BMD as an indicator of treatment-related fracture risk reduction. The study cohort included 6093 women age > 40 years initiating osteoporosis treatment with two consecutive dual-energy X-ray absorptiometry (DXA) scans (mean interval 4.7 years). We computed change in the spine, total hip, and femur neck BMD between the first and second DXA scans as categorical (categorized as stable, detectable decrease, or detectable increase) and continuous measures. We modeled time to first incident fracture, ascertained from health services data, using Cox regression adjusted for baseline fracture probability.
Results
During a mean follow-up of 12.1 years, 995 women developed incident major osteoporotic fractures (MOF) including 246 with hip fractures and 301 with clinical vertebral fractures. Women with a detectable decrease in total hip BMD compared with stable BMD experienced an increase in MOF (adjusted hazard ratio [aHR] 1.46, 95% confidence interval [CI] 1.25–1.70) while those with a detectable increase in total hip BMD experienced a decrease in MOF (aHR 0.71, 95% CI 0.61–0.83), and these results were not attenuated when adjusted for change in spine BMD. Similar results were seen for hip and clinical vertebral fracture outcomes, when BMD change was assessed as a continuous measure, and when femur neck BMD monitoring was used instead of total hip BMD monitoring.
Conclusions
Treatment-related increases in total hip BMD are associated with lower MOF, hip, and clinical vertebral fracture risk compared with stable BMD, while BMD decreases are associated with higher fracture risk. In contrast, spine BMD change is not independently associated with fracture risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis-related fractures are common and have a significant societal impact in terms of human and economic costs [1]. Dual-energy X-ray absorptiometry (DXA) is widely used to measure bone mineral density (BMD) for the purposes of osteoporosis diagnosis and fracture risk assessment [2, 3]. Treatment is often initiated on the basis of low BMD, either used alone or in conjunction with other clinical risk factors [4,5,6]. In appropriately selected women, approved treatments can reduce fracture risk in primary and secondary prevention settings [7,8,9].
Although BMD monitoring during the initial 3–5 years of treatment is recommended by some clinical practice guidelines [5, 10], the role of repeat BMD testing during pharmacotherapy remains controversial [11,12,13]. Group-level clinical trial data suggests that larger BMD increases are associated with greater fracture risk reduction [14, 15]. A meta-regression of published trials found that greater improvements in total hip, femoral neck, and lumbar spine BMD were strongly associated with greater reductions in vertebral fractures; greater improvements in total hip and femoral neck (but not lumbar spine) BMD were strongly associated with greater reductions in hip fractures [16]. In a clinical registry-based analysis, treatment-related increases in total hip BMD were associated with reduced fracture risk compared with stable BMD, and decreases in total hip BMD were associated with greater risk for fractures [17].
Technical challenges in BMD monitoring among individuals include measurement error (typically 3–5%) [2, 18]. An additional source of confusion regards the optimal site for BMD monitoring. Discordance between the spine and hip BMD T-scores is not infrequent in routine clinical practice [19, 20], and discordance also commonly arises in observed BMD change at various measurement sites [21].
The current study was performed to compare BMD monitoring at the hip versus the lumbar spine in women initiating anti-osteoporosis drug therapy in the routine clinical practice setting. We used population-based registries from the Province of Manitoba, Canada, to assess whether anti-fracture effects were more strongly associated with change in hip BMD or change in lumbar spine BMD.
Methods
Patient population
The study population consisted of all women age 40 years and older not receiving osteoporosis therapy at baseline who subsequently initiated anti-osteoporosis therapy and had repeat BMD testing > 1 year later. Using linkage to the province-wide retail pharmacy network [22], we identified women without significant systemic estrogen use or other anti-osteoporosis medication use in the year prior to baseline BMD testing (defined as < 3 months pharmacy dispensed bisphosphonate, calcitonin, systemic estrogen product, raloxifene, or teriparatide) who subsequently received therapy in the year following BMD testing. We excluded women without a full year of coverage data prior to the baseline BMD or a full year of coverage after the baseline BMD, without health care coverage, and with missing BMD measurements at baseline or follow-up for the total hip, femur neck, or lumbar spine. All baseline scans were performed between April 1, 1999, and December 31, 2014, with follow-up scans to March 31, 2016.
In the Canadian Province of Manitoba (population 1.3 million in 2017), health services are provided to virtually all residents through a public healthcare system. DXA testing has been managed as an integrated program since 1997; criteria for baseline testing include screening at age 65 years for women and in younger women with additional risk factors [23]. Consistent with national guidelines, the program’s recommended interval for initial follow-up is 3 years for most patients, 1 year in those on systemic glucocorticoid therapy or aromatase inhibitors, and at least 5 years if previously reported as low risk [18]. The program maintains a database of all DXA results that can be linked with other population-based computerized health databases through an anonymous personal identifier. The DXA database has completeness and accuracy in excess of 99% [24]. The study was approved by the Health Research Ethics Board for the University of Manitoba.
Bone mineral density measurements
Lumbar spine and hip DXA scans were performed and analyzed in accordance with the manufacturer recommendations. Our in-house scheduling software automatically schedules patients on the same scanner as was used for the baseline examination. Femoral neck and total hip T-scores (number of SDs above or below young adult mean BMD) were calculated from NHANES III white female reference values [25]; lumbar spine (L1–4) T-scores were based upon the manufacturer white female reference values. The program’s quality assurance is under strict supervision by a medical physicist [23]. The six cross-calibrated instruments used for this study (3 Prodigy and 3 iDXA, GE/Lunar Healthcare, Madison, WI) exhibited stable long-term performance (coefficient of variation < 0.5%). All reporting physicians and supervising technologists are required to maintain DXA certification with the International Society for Clinical Densitometry (ISCD).
The absolute BMD difference between the two DXA tests (in g/cm2) was compared with 95% least significant change (LSC) values for assessment of change using accepted methods, where LSC is the least amount of BMD change that can be considered statistically significant [18, 26, 27]. BMD measurement error for the Manitoba BMD program used for computing the LSC is derived from more than 400 DXA scan pairs (most performed on different days but within 28 days by different technologists). Our LSC procedure requires every DXA technologist in Manitoba to participate in the precision assessment, initially following major equipment change and also as an ongoing activity (10 per technologist per year). This ensures that the LSC is current and reflects the full spectrum of DXA technologist skill and experience. We have previously reported that this approach (rather than same-day repositioning with the same technologist) is more representative of measurement error encountered during clinical monitoring [28]. From these scan pairs, we obtained the following 95% LSC values which are within acceptable ranges [17]: total hip, 0.03 g/cm2; lumbar spine, 0.05 g/cm2; femoral neck, 0.055 g/cm2. An observed absolute difference less than these values would be considered to be within the range of measurement error (designated stable) whereas an increase or decrease equal to or exceeding these values is outside the range of measurement error (designated detectable increase or decrease in BMD, respectively).
Baseline fracture probability calculations
Ten-year probability of a major osteoporotic fracture risk was calculated using the World Health Organization fracture risk assessment tool, Canadian version (FRAX® Desktop Multi-Patient Entry, version 3.7) [29, 30]. Briefly, age, body mass index (BMI), femoral neck BMD, and other data required for calculating fracture probability with FRAX were assessed through a combination of measurements (height and weight), information collected directly from subjects at the time of DXA scanning, hospital discharge abstracts (diagnoses and procedures coded using the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] prior to 2004 and International Classification of Diseases, Tenth Revision, Canadian Enhancements [ICD-10-CA] thereafter), and physician billing claims (coded using ICD-9-CM) as previously described [31]. The Canadian FRAX tool was calibrated using nationwide hip fracture data. Predictions agree closely with observed fracture risk in our population [32, 33].
Fractures outcomes
Manitoba Health records were assessed for the presence of incident non-traumatic hip, clinical vertebral, forearm, and humerus fracture diagnostic codes (collectively designated “major osteoporotic” fractures) using previously validated algorithms [34, 35]. Fractures that were not associated with trauma codes were assessed through a combination of hospital discharge abstracts and physician billing claims. We required that hip and forearm fractures codes be associated with site-specific fracture reduction, fixation, or casting codes to enhance specificity for an acute fracture event. To minimize potential misclassification of prior incident fractures, we conservatively required that there be no hospitalization or physician visit(s) with the same fracture type in the 6 months preceding an incident fracture diagnosis.
Statistical analysis
Statistical analyses were performed with Statistica (Version 13.0, StatSoft Inc., Tulsa, OK). Descriptive statistics for demographic and baseline characteristics are presented as mean ± SD for continuous variables or number (%) for categorical variables. Student’s t tests (continuous measures) and χ2 tests (categorical measures) were used to test for between-group differences. Time to incident fracture following the first DXA scan (index date) was studied using Cox proportional hazards regression. Observations were censored for death, migration out of province, or end of follow-up (March 31, 2017). Our primary analysis examined incident MOF as the outcome of interest with BMD change as a categorical measure: stable (referent), detectable decrease, or detectable increase. Models considered total hip BMD change and lumbar spine BMD change, first separately then simultaneously. We reported hazard ratios (HRs) with 95% confidence intervals (CIs) in addition to the overall Wald score as measures of effect size. HRs were adjusted for baseline fracture probability using the FRAX score log-transformed to correct for a skewed distribution (MOF fracture probability for incident MOF or vertebral fracture, hip fracture probability for incident hip fracture). The proportional hazards assumption was confirmed by testing scaled Schoenfeld residuals versus time. We undertook a series of secondary sensitivity analyses to test the robustness of our findings. First, we examined three continuous measures of BMD change: absolute change in g/cm2, annualized change, and annualized percent change. Second, we considered hip fracture and vertebral fracture as the outcomes of interest. Third, we repeated analyses using femur neck instead of total hip as the monitoring site. Last, we repeated the categorical analyses based upon exclusion of lumbar spine levels with structural artifact by ISCD certified reporting physicians using LSC limits adjusted for the loss in spine precision due to the smaller number of available vertebrae [36].
Results
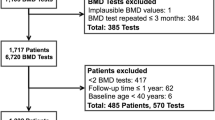
The study population selection flow chart is shown in Supplemental Fig. 1. The final study population consisted of 6093 women, with baseline characteristics summarized in Table 1. Mean age was 63.4 ± 9.8 years at baseline and the mean testing BMD interval was 4.7 ± 2.6 years. The majority (56.5%) of the women met the osteoporosis BMD T-score definition at one or more sites. Bisphosphonate therapy accounted for the majority of the treatment (70%) followed by systemic estrogen (23%), raloxifene (5%), calcitonin (2%), denosumab and teriparatide (< 1%).
Table 2 summarizes detectable BMD change according to measurement site. For total hip and lumbar spine, there was concordance in 57.2% of cases. Detectable decrease in BMD was seen in 19.8% of total hip measurements vs 10.8% of lumbar spine measurements, while a detectable increase was seen in 30.7% of total hip and 39.7% of lumbar spine cases. Both total hip and lumbar spine showed a detectable change in 49.5% of cases. In contrast, the femur neck showed detectable change in only 20.2% of cases. Overall concordance for the femur neck vs lumbar spine was 53.1%. Detectable decrease was similar for femur neck and lumbar spine (10.8%) while a detectable increase was more frequently seen for lumbar spine than femur neck (39.7 vs 9.4%).
During mean follow-up 12.1 ± 3.6 years, 995 women sustained one or more incident MOF, 246 sustained hip fracture, and 301 sustained clinical vertebral fracture. Table 3 shows the mean change in BMD (absolute change, annualized change, and annualized percent change) according to site of fracture and site of BMD measurement. For the total hip, there was a significantly greater increase in BMD in fracture-free vs fracture women regardless of whether change was expressed as an absolute measurement, annualized per year, or annualized percent change. For the femur neck, significantly greater increase in BMD was seen for women without incident MOF or hip fracture, but not for incident vertebral fracture. In contrast, change in lumbar spine BMD was not associated with incident MOF or hip fracture, and paradoxically, women without incident vertebral fracture had a smaller (not larger) BMD increase compared with women sustaining a vertebral fracture.
Table 4 shows HRs for incident fracture adjusted for baseline fracture probability according to detectable BMD change in models that considered hip and spine measurements, first separately then simultaneously. Detectable decreases in total hip BMD and lumbar spine BMD were separately associated with increased risk for incident MOF, but when combined, only detectable decrease in total hip BMD continued to predict increase fracture risk (HR 1.46, 95% CI 1.24–1.73). A detectable increase in total hip BMD was associated with reduced risk for incident MOF (HR 0.71, 95% CI 0.61–0.83) while lumbar spine change was not (HR 0.93, 95% CI 0.81–1.06). As a monitoring site, total hip was more strongly associated with incident MOF (Wald 60.6, P < 0.001) than lumbar spine (Wald 10.9. P = 0.004) and showed minimal attenuation in the combined model (Wald 51.9, P < 0.001 vs 1.7, P = 0.428). Similar results were seen for incident hip fracture and incident vertebral fracture as the outcomes of interest. In both sets of analyses, detectable decrease in total hip BMD was associated with increased fracture risk whereas a detectable increase was associated with a reduction in fracture risk, and this was largely unaffected by simultaneous adjustment for change in lumbar spine BMD. In contrast, when adjusted for change in total hip BMD, a detectable decrease in lumbar spine BMD did not predict increased fracture risk and a detectable increase in lumbar spine did not predict reduced fracture risk. Results were broadly similar for femur neck BMD vs lumbar spine BMD monitoring (Supplemental Table 1) and after exclusion of vertebral levels with structural artifact (Supplemental Table 2). Once again, lumbar spine BMD change was not a reliable predictor of anti-fracture effects when combined with femur neck BMD change.
We also looked at BMD change as a continuous measure expressed as HR per SD. Similar to the categorical analyses, each SD increase in total hip BMD change was associated with a significant reduction in incident MOF, incident hip, and incident vertebral fracture before and after simultaneously considering change in lumbar spine BMD change (Fig. 1). In contrast, an increase in lumbar spine BMD showed only a weak trend towards incident MOF risk when tested separately and was not associated with the incident hip fracture or incident vertebral fracture. When simultaneously considering change in total hip BMD, an increase in lumbar spine BMD did not predict reduced fracture risk (paradoxically fracture risk appeared to be slightly greater). Similar results were seen for continuous analysis based upon femur neck BMD change versus lumbar spine BMD change (Supplemental Fig. 2).
Adjusted hazard ratio (HR) with 95% confidence interval (CI) for incident fracture according to continuous change in total hip and lumbar spine bone mineral density (BMD), with sites considered separately and simultaneously. Results adjusted for baseline fracture probability. a Incident major osteoporotic fracture (MOF). b Incident hip fracture. c Incident vertebral fracture
Discussion
In this large clinical cohort, we were able to look at BMD change in women initiating anti-osteoporosis therapy and relate their fracture outcomes to BMD change. There was consistent evidence that change in total hip BMD, whether assessed categorically or as a continuous measure, was associated with incident fracture outcomes. Femur neck BMD showed a similar but slightly less robust association. In contrast, lumbar spine BMD change was less strongly associated with fracture outcomes and any effect was attenuated (or reversed) by simultaneously considering hip BMD change.
Our results may at first appear paradoxical, since lumbar spine BMD shows a larger increase than hip BMD in individuals initiating treatment. However, this is offset by a lower test precision and by measurement error (e.g., degenerative spondylosis) that can produce an increase in BMD unrelated to treatment [36, 37]. Indeed, the placebo arms of many clinical trials demonstrate an increase in spine BMD while hip BMD decreases [16]. Finally, vertebral fractures in the lumbar spine could falsely elevated spine BMD despite best efforts to exclude these from the region of interest.
Our study supports the individual-level meta-analysis of clinical trial data from Bouxsein et al. [16]. In this pooled analysis of multiple clinical trials, change in hip BMD was more strongly associated with hip fracture outcomes than lumbar spine BMD. Conversely, the latter found that change in lumbar spine BMD was more strongly associated with vertebral fracture outcomes than hip BMD, though the two sites were not assessed simultaneously. The weaker performance of lumbar spine BMD change in our study may reflect a higher prevalence of degenerative and structural artifact in a clinical population compared with women included in clinical trials.
Strengths of our study include broad inclusion criteria, which are representative of women treated in routine clinical practice, and access to a DXA registry with rigorous data collection and linkage to administrative healthcare databases [24]. Our results are therefore likely to be of greater applicability to clinical practice than prospective research cohorts [38] or clinical trials [13]. We also acknowledge several limitations. Firstly, the threat of “confounding by indication” exists in all observational studies; however, the fact that all women in this study initiated treatment mitigates this concern to a great degree. In addition, women with strong contraindications to therapy or with primary non-adherence (i.e., not filling an initial prescription) were excluded from our study, but this also reflects a common clinical reality. Secondly, a limitation is in the lack of standardization in the BMD testing interval. Whereas a fixed testing interval would be seen in a clinical trial or a research cohort, in clinical practice, it is not possible to strictly enforce this. However, alternative measures of change (annualized) did not alter our findings suggesting that this is not an important limitation. Unfortunately, our study cannot provide specific guidance on the optimal testing interval where a relatively short testing interval is often recommended (e.g., 1–2 years after initiating therapy) [5, 10]. Thirdly, a limitation is that we did not consider change in clinical management that might occur based upon the results from the second BMD measurement. It is possible that when confronted with a detectable decrease in BMD, this might improve patient adherence or lead to a change in therapy. Alternatively, individuals with a detectable increase in BMD might be considered for a “drug holiday.” Either action would be expected to bias our results towards the null, and therefore, our findings are likely to be conservative. Fourthly, our study population was predominantly treated with bisphosphonates, and whether similar results would be seen for anabolic agents is uncertain. Finally, our study does not address the question of whether monitoring is useful in terms of guiding appropriate changes in therapy that ultimately lead to better fracture outcomes.
In conclusion, treatment-related increases in total hip BMD are associated with lower MOF, hip, and clinical vertebral fracture risk compared with stable BMD, while BMD decreases are associated with higher fracture risk. In contrast, spine BMD change is not independently associated with fracture risk. These findings may help to inform clinical management regarding BMD monitoring in women initiating anti-osteoporosis therapy. If monitoring is performed, the total hip site provides a better indicator of an anti-fracture effect than the lumbar spine.
References
Compston JE, McClung MR, Leslie WD (2019) Osteoporosis. Lancet 393(10169):364–376
Cummings SR, Bates D, Black DM (2002) Clinical use of bone densitometry: scientific review. JAMA. 288(15):1889–1897
Force USPST (2011) Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med 154(5):356–364
Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12(1):43
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R, National Osteoporosis Foundation (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381
Kanis JA, Harvey NC, Cooper C, Johansson H, Oden A, McCloskey EV et al (2016) A systematic review of intervention thresholds based on FRAX: a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11(1):25
MacLean C, Newberry S, Maglione M, McMahon M, Ranganath V, Suttorp M, Mojica W, Timmer M, Alexander A, McNamara M, Desai SB, Zhou A, Chen S, Carter J, Tringale C, Valentine D, Johnsen B, Grossman J (2008) Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med 148(3):197–213
Murad MH, Drake MT, Mullan RJ, Mauck KF, Stuart LM, Lane MA, Abu Elnour NO, Erwin PJ, Hazem A, Puhan MA, Li T, Montori VM (2012) Clinical review. Comparative effectiveness of drug treatments to prevent fragility fractures: a systematic review and network meta-analysis. J Clin Endocrinol Metab 97(6):1871–1880
Saito T, Sterbenz JM, Malay S, Zhong L, MacEachern MP, Chung KC (2017) Effectiveness of anti-osteoporotic drugs to prevent secondary fragility fractures: systematic review and meta-analysis. Osteoporos Int 28(12):3289–3300
Papaioannou A, Morin S, Cheung AM, Atkinson S, Brown JP, Feldman S, Hanley DA, Hodsman A, Jamal SA, Kaiser SM, Kvern B, Siminoski K, Leslie WD, for the Scientific Advisory Council of Osteoporosis Canada (2010) 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 182(17):1864–1873
Compston J (2009) Monitoring osteoporosis treatment. Best Pract Res Clin Rheumatol 23(6):781–788
Bruyere O, Reginster JY (2014) Monitoring of osteoporosis therapy. Best Pract Res Clin Endocrinol Metab 28(6):835–841
Bell KJ, Hayen A, Macaskill P, Irwig L, Craig JC, Ensrud K et al (2009) Value of routine monitoring of bone mineral density after starting bisphosphonate treatment: secondary analysis of trial data. BMJ. 338:b2266
Hochberg MC, Greenspan S, Wasnich RD, Miller P, Thompson DE, Ross PD (2002) Changes in bone density and turnover explain the reductions in incidence of nonvertebral fractures that occur during treatment with antiresorptive agents. J Clin Endocrinol Metab 87(4):1586–1592
Wasnich RD, Miller PD (2000) Antifracture efficacy of antiresorptive agents are related to changes in bone density. J Clin Endocrinol Metab 85(1):231–236
Bouxsein ML, Eastell R, Lui LY, Wu LA, de Papp AE, Grauer A, Marin F, Cauley JA, Bauer DC, Black DM, for the FNIH Bone Quality Project (2019) Change in bone density and reduction in fracture risk: a meta-regression of published trials. J Bone Miner Res. https://doi.org/10.1002/jbmr.3641
Leslie WD, Majumdar SR, Morin SN, Lix LM (2016) Change in bone mineral density is an indicator of treatment-related antifracture effect in routine clinical practice: a registry-based cohort study. Ann Intern Med 165(7):465–472
Shepherd JA, Lu Y, Wilson K, Fuerst T, Genant H, Hangartner TN, Wilson C, Hans D, Leib ES (2006) Cross-calibration and minimum precision standards for dual-energy X-ray absorptiometry: the 2005 ISCD Official Positions. J Clin Densitom 9(1):31–36
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA (2011) Spine-hip discordance and fracture risk assessment: a physician-friendly FRAX enhancement. Osteoporos Int 22(3):839–847
Johansson H, Kanis JA, Oden A, Leslie WD, Fujiwara S, Gluer CC et al (2014) Impact of femoral neck and lumbar spine BMD discordances on FRAX probabilities in women: a meta-analysis of international cohorts. Calcif Tissue Int 95(5):428–435
Abrahamsen B, Stilgren LS, Hermann AP, Tofteng CL, Barenholdt O, Vestergaard P et al (2001) Discordance between changes in bone mineral density measured at different skeletal sites in perimenopausal women--implications for assessment of bone loss and response to therapy: the Danish osteoporosis prevention study. J Bone Miner Res 16(7):1212–1219
Kozyrskyj AL, Mustard CA (1998) Validation of an electronic, population-based prescription database. Ann Pharmacother 32(11):1152–1157
Leslie WD, Metge C (2003) Establishing a regional bone density program: lessons from the Manitoba experience. J Clin Densitom 6(3):275–282
Leslie WD, Caetano PA, Macwilliam LR, Finlayson GS (2005) Construction and validation of a population-based bone densitometry database. J Clin Densitom 8(1):25–30
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston Jr CC, Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8(5):468–489
Gluer CC, Blake G, Lu Y, Blunt BA, Jergas M, Genant HK (1995) Accurate assessment of precision errors: how to measure the reproducibility of bone densitometry techniques. Osteoporos Int 5(4):262–270
Gluer CC (1999) Monitoring skeletal changes by radiological techniques. J Bone Miner Res 14(11):1952–1962
Leslie WD (2008) Factors affecting short-term bone density precision assessment and the effect on patient monitoring. J Bone Miner Res 23(2):199–204
Kanis JA, Oden A, Johansson H, Borgstrom F, Strom O, McCloskey E (2009) FRAX and its applications to clinical practice. Bone. 44(5):734–743
Leslie WD, Lix LM, Langsetmo L, Berger C, Goltzman D, Hanley DA, Adachi JD, Johansson H, Oden A, McCloskey E, Kanis JA (2011) Construction of a FRAX(R) model for the assessment of fracture probability in Canada and implications for treatment. Osteoporos Int 22(3):817–827
Bisson EJ, Finlayson ML, Ekuma O, Marrie RA, Leslie WD (2019) Accuracy of FRAX(R) in people with multiple sclerosis. J Bone Miner Res. https://doi.org/10.1002/jbmr.3682
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA et al (2010) Independent clinical validation of a Canadian FRAX tool: fracture prediction and model calibration. J Bone Miner Res 25(11):2350–2358
Fraser LA, Langsetmo L, Berger C, Ioannidis G, Goltzman D, Adachi JD et al (2011) Fracture prediction and calibration of a Canadian FRAX(R) tool: a population-based report from CaMos. Osteoporos Int 22(3):829–837
Lix LM, Azimaee M, Osman BA, Caetano P, Morin S, Metge C, Goltzman D, Kreiger N, Prior J, Leslie WD (2012) Osteoporosis-related fracture case definitions for population-based administrative data. BMC Public Health 12:301
Epp R, Alhrbi M, Ward L, Leslie WD (2018) Radiological validation of fracture definitions from administrative data. J Bone Miner Res 33(Supp 1):S275
Tsang JF, Leslie WD (2007) Exclusion of focal vertebral artifacts from spine bone densitometry and fracture prediction: a comparison of expert physicians, three computer algorithms, and the minimum vertebra. J Bone Miner Res 22(6):789–798
Jones G, Nguyen T, Sambrook PN, Kelly PJ, Eisman JA (1995) A longitudinal study of the effect of spinal degenerative disease on bone density in the elderly. J Rheumatol 22(5):932–936
Gourlay ML, Fine JP, Preisser JS, May RC, Li C, Lui LY, Ransohoff DF, Cauley JA, Ensrud KE (2012) Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med 366(3):225–233
Acknowledgments
The authors acknowledge the Manitoba Centre for Health Policy (MCHP) for use of data contained in the Population Health Research Data Repository (HIPC Project Number 2016/2017-29). The results and conclusions are those of the authors, and no official endorsement by the MCHP, Manitoba Health, or other data providers is intended or should be inferred. This article has been reviewed and approved by the members of the Manitoba Bone Density Program Committee.
Grant support
Dr. Lix is supported by a Tier 1 Canada Research Chair.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Health Research Ethics Board for the University of Manitoba.
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 209 kb)
Rights and permissions
About this article
Cite this article
Leslie, W.D., Martineau, P., Bryanton, M. et al. Which is the preferred site for bone mineral density monitoring as an indicator of treatment-related anti-fracture effect in routine clinical practice? A registry-based cohort study. Osteoporos Int 30, 1445–1453 (2019). https://doi.org/10.1007/s00198-019-04975-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-04975-y