Abstract
There are occasional marked discordances in BMD T-scores at the lumbar spine (LS) and femoral neck (FN). We investigated whether such discordances could contribute independently to fracture prediction using FRAX. We studied 21,158 women, average age 63 years, from 10 prospective cohorts with baseline FRAX variables as well as FN and LS BMD. Incident fractures were collected by self-report and/or radiographic reports. Extended Poisson regression examined the relationship between differences in LS and FN T-scores (ΔLS–FN) and fracture risk, adjusted for age, time since baseline and other factors including FRAX 10-year probability for major osteoporotic fracture calculated using FN BMD. To examine the effect of an adjustment for ΔLS–FN on reclassification, women were separated into risk categories by their FRAX major fracture probability. High risk was classified using two approaches: being above the National Osteoporosis Guideline Group intervention threshold or, separately, being in the highest third of each cohort. The absolute ΔLS–FN was greater than 2 SD for 2.5 % of women and between 1 and 2 SD for 21 %. ΔLS–FN was associated with a significant risk of fracture adjusted for baseline FRAX (HR per SD change = 1.09; 95 % CI = 1.04–1.15). In reclassification analyses, only 2.3–3.2 % of the women moved to a higher or lower risk category when using FRAX with ΔLS–FN compared with FN-derived FRAX alone. Adjustment of estimated fracture risk for a large LS/FN discrepancy (>2SD) impacts to a large extent on only a relatively small number of individuals. More moderate (1–2SD) discordances in FN and LS T-scores have a small impact on FRAX probabilities. This might still improve clinical decision-making, particularly in women with probabilities close to an intervention threshold.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
FRAX® calculates 10-year fracture probability from readily obtainable clinical risk factors (CRFs) in men and women (http://www.shef.ac.uk/FRAX) [1–3]. The fracture risk calculation can be enhanced by the optional entry of bone mineral density (BMD) measured at the femoral neck (FN), the only skeletal region of interest currently validated for use with FRAX [1]. The principal reason for the inclusion of FN BMD into FRAX was its wide availability in the development cohorts; lumbar spine (LS) BMD was available in only about half the number of individuals compared to femoral neck BMD, with peripheral BMD available in even fewer. FN BMD also has the advantage that for any given age and BMD, the fracture risk is approximately the same in men and women so that the T-score used in FRAX is derived from a single reference standard (i.e. the NHANES III database for female Caucasians aged 20–29 years) [4, 5]. Additionally, FN BMD is associated with a higher gradient of risk for hip fracture than BMD measurements at other sites, with similar or better prediction of major fractures when appropriate adjustment is made to the units of BMD [6, 7]. Notwithstanding, measurements of BMD at sites other than the FN provide significant information on fracture risk [4, 6, 7].
In clinical practice, LS BMD is frequently measured by dual-energy X-ray absorptiometry (DXA) at the same visit as FN BMD. Indeed, LS BMD is incorporated into several clinical guidelines and is the preferred measurement site for monitoring treatment [8–10]. Although the combination of these two skeletal sites does not improve the general predictive ability (sensitivity/specificity) for future fractures, there are situations when a large discordance in the T-score at the two sites in a given individual may enhance the accuracy for risk characterisation [11–13]. In a recent analysis of a large referral cohort, there was approximately a 10 % change in fracture probability for each unit of T-score discordance, and the authors proposed that the clinician may “Increase/decrease FRAX estimate for a major fracture by one-tenth for each rounded T-score difference between the lumbar spine and femoral neck” [14]. We wished to determine the impact of a T-score discordance in independent population-based cohorts and to examine the impact of the discordance on reclassification of patients across risk thresholds.
Materials and Methods
We studied women in whom FRAX variables and BMD at both the FN and LS were recorded at baseline with subsequent follow-up fracture data from 10 prospective population-based cohorts from North America, Europe, Asia and Australia as follows:
Women’s Health Initiative (WHI) Study
The study comprises three overlapping randomised controlled studies and an observational study in post-menopausal women aged 50–79 years [15, 16]. Women on HRT or other bone-active medications were excluded from the analysis. Bone mineral density measurements at the FN and LS were measured using the Hologic QDR2000. Incident hip fractures were documented from medical records and adjudicated at a central facility, while non-hip fractures were locally adjudicated. For this analysis, BMD, FRAX estimation and validated fracture follow-up were available for 4,039 women.
Canadian Multicentre Osteoporosis Study (CaMOS)
This is an on-going prospective age-stratified cohort documenting risk factors and the incidence of fractures in a random sample of 9,424 men and women aged 25 years or more selected by telephone listings [17]. Family history of fracture captured any fracture, not just hip fracture. BMD was measured by DXA at the FN and LS by Hologic QDR or Lunar DPX equipment. Machines were cross-calibrated using the same European Spine Phantom. For this analysis, BMD, FRAX and validated fracture follow-up data were available for 4,871 women.
Osteoporosis and Ultrasound Study (OPUS)
OPUS comprises five age-stratified population-based female cohorts drawn from different European centres (Sheffield and Aberdeen (UK), Berlin and Kiel (Germany), and Paris (France)) [18, 19]. Participants completed a questionnaire at baseline and BMD was measured by DXA using the Hologic QDR 4500 (Kiel, Paris and Sheffield) or the Lunar Expert (Aberdeen and Berlin). Baseline estimates for BMD at both skeletal sites and FRAX estimates were available in 2,176 women. Incident fractures were documented from hospital, general practitioner or individual imaging databases.
Rochester Cohorts
These comprised two random population samples stratified by decade of age, one followed for up to 20 years and the other for 8 years [20, 21]. Current smoking was captured as ever use of smoking. Data on rheumatoid arthritis and alcohol intake were absent and set to “No” in the analysis of FRAX. BMD of the right femoral neck was measured by dual photon absorptiometry in the first cohort (cross-calibrated to DXA) and by DXA (Hologic QDR 2000) in the second group. Fractures were ascertained by periodic interview combined with review of the in-patient and outpatient medical records of all local care providers. For this analysis, BMD, FRAX probabilities and validated fracture follow-up were available for 487 women.
Dubbo Osteoporosis Epidemiology Study (DOES)
This is a population-based study with multiple assessments of skeletal status in men and women aged 60 years or more from Dubbo, Australia [22, 23]. A family history of osteoporosis was used instead of a parental history of hip fracture. Baseline measurements included BMD at the FN and LS assessed using DXA (GE-Lunar DPX and Prodigy). Fractures were identified through radiologists’ reports. For this analysis, BMD, FRAX and validated fracture follow-up were available for 1,221 women.
Adult Health Study (AHS)
The AHS was established in 1958 and documents the late health effects of radiation exposure among atomic bomb survivors in Hiroshima and Nagasaki, originally comprising about 15,000 survivors and 5,000 controls. Data on family history, rheumatoid arthritis and alcohol intake were not captured and set to “no” in FRAX calculations. BMD was measured at the both skeletal sites by DXA in 1994 (Hologic QDR 2000) [24, 25]. For this analysis, BMD, FRAX and validated fracture follow-up were available for 1,318 women.
European Vertebral Osteoporosis Study/European Prospective Osteoporosis Study (EVOS/EPOS)
These two linked studies comprised age- and sex-stratified random samples from multiple centres in 19 European countries [26–28]. Alcohol intake was entered as “yes” in FRAX, where the intake was documented as at least 5 days per week. BMD was measured at 13 centres by DXA at the FN and LS using pencil beam machines that were cross-calibrated using the European Spine Phantom. For this analysis, BMD, FRAX and validated fracture follow-up were available for 1,550 women.
Osteoporosis Risk Factor and Prevention Study (OSTPRE)
In a sub-study of this study [29], a prospective population sample of women aged 47–56 years who were residents of Kuopio province in 1989, 3,222 women underwent bone densitometry by DXA using the Lunar DPX. Incident fractures were captured by questionnaire on a yearly basis, but only validated fractures reviewed from medical records or X-rays were included in the analysis. For this analysis, BMD, FRAX and validated fracture follow-up were available for 2,711 women.
Aberdeen Prospective Osteoporosis Screening Study (APOSS)
5,119 women 45–54 years of age were randomly selected from a community-based register and attended a baseline visit between 1990 and 1994 [30]. All participants underwent bone densitometry of the LS and left FN by DXA using Norland scanners (Cooper Surgical, Trumbull, CT, USA). The mean time for follow-up was 9.7 years, ranging from a minimum of 7.5 years to a maximum of 12.2 years. For this analysis, BMD, FRAX and validated fracture follow-up were available for 1,154 women.
MsOS Hong Kong
This comprised a cohort of 2,000 Hong Kong Chinese women, 65 years of age or older [31]. Stratified sampling was used in order to obtain approximately one-third of the subjects in each of the following age groups: 65–69, 70–74 and ≥75 years. All eligible subjects were community-dwelling and ambulatory. Trained interviewers conducted face-to-face interviews based on a structured and validated questionnaire. BMD of the LS and FN was measured using Hologic QDR-4500W densitometers. For this analysis, BMD, FRAX estimation and validated fracture follow-up were available for 1,631 women.
Statistical Analysis
FRAX probabilities were computed using the appropriate country models for the study cohorts. Differences in scanning equipment between cohorts were accommodated by the use of cohort-specific z-scores for BMD prior to conversion to T-scores using NHANES III reference data for the femoral neck and Hologic reference data for the lumbar spine. We have been able to compare this approach to actual reported T-scores in a small sample of the cohorts that also provided original T-scores to us. The mean difference in T-score was −0.3 suggesting that our calculated T-score values were slightly lower than those produced locally by the manufacturer’s reference range. The difference between LS and FN T-scores (ΔLS–FN) was calculated by simply subtracting the FN T-score from that at the LS.
Risk for major osteoporotic fracture, including clinical vertebral fracture, hip fracture, forearm or humerus fracture, was investigated using an extended Poisson model applied to each cohort, with subsequent merging of the β-coefficients from each cohort, weighted according to the variance. The gradient of risk was estimated as the hazard ratio (HR) for a 1SD decrease in ΔLS–FN. Adjustment was made for age, time from baseline and FRAX probabilities. As LS BMD can be artefactually increased with advancing age due to disorders such as degenerative changes and aortic calcification, we also explored if the HR differed for those with higher LS than FN T-scores and those where the LS T-score was lower than that at the FN.
Finally, we examined the impact of taking account of the discordance by looking at the proportion of patients reclassified using two approaches; first, we utilised the National Osteoporosis Guideline Group (NOGG) intervention thresholds as utilised in European guidance [32, 33] and the UK [34] and secondly, given the fact that different country models were used, we also derived cohort-specific thresholds that categorised the highest third of FRAX probabilities to be “at risk” within each cohort.
Results
The analysis population comprised 21,158 women, ranging in age from 40–90 years with an average age of 63 years (SD 10 years) (Table 1). During a mean follow-up of 7.4 years, 1,844 women sustained one or more major osteoporotic fracture.
Discordance Between LS and FN T-Scores
The mean T-score was similar at the FN (−1.40, SD 1.11) and LS (−1.35, SD, 1.21) with a mean T-score offset (ΔLS–FN) of +0.05 (SD 0.89). Discordances between T-scores at the two measurement sites showed a near normal distribution (Fig. 1). Major discrepancies (>2 SD) in T-scores between the two sites were uncommon, comprising 2.5 % of all the participants. Those with major discrepancies were of similar mean age to the cohort as a whole (mean 63, 63 and 66 years for the whole cohort, those with FN lower than LS and those with FN higher than LS, respectively. Moderate discordances (between 1 and 2 SDs) were more frequent but still comprised a minority of the study population (21 %).
Impact of Spine and Femoral Neck Discordance (ΔLS–FN) on Fracture Prediction
In multivariate models, adjusted for age, time since baseline and FN-BMD, ΔLS–FN was a significant independent predictor of major osteoporotic fracture risk (GR 1.20, 95 % CI 1.07–1.35, p < 0.001) but not of hip fracture risk (GR 1.04, 95 % CI 0.92–1.17, p > 0.30).
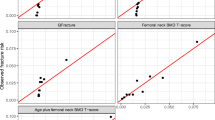
In a further multivariate model, adjusted for age, time since baseline and the 10-year probability of a major osteoporotic fracture, ΔLS–FN still remained a significant predictor of major osteoporotic fracture risk. This suggests that low BMD at the LS, relative to that at the FN, is a predictor of increased fracture risk. Each 1SD decrease in ΔLS–FN was associated with a 9 % increase in fracture risk (GR 1.09, 95 % CI 1.04–1.15) (Fig. 2).
When the study population was dichotomised into those with lower LS than FN T-scores versus those with higher LS T-scores, the gradient of risk in each group was similar in both groups (HR 1.11, 95 % CI 1.00–1.24) to that observed when the whole population was included in a single analysis (Fig. 2).
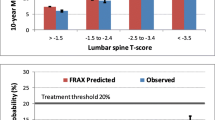
Impact of Discordance on Reclassification
In this analysis, the original FRAX probability for each individual was adjusted as follows. Where the ΔLS–FN was between −1 and +1 SDs, no adjustment was made; where ΔLS–FN was between 1 and 2 SDs, the FRAX probability was increased or decreased by 10 % in those where the LS T-score was lower or higher, respectively; for those with ΔLS–FN between 2 and 3 SDs, the FRAX probability was increased or decreased by 20 % and so on.
The outcomes of the reclassification analyses using the NOGG intervention thresholds or the cohort-specific thresholds (highest third) are shown in Tables 2 and 3, respectively. A total of 2.2 % of the women were reclassified across the NOGG thresholds with more women moving from above the threshold to below it compared to the converse movement (Table 2). A similar, small proportion (3.3 %) was reclassified using the cohort-specific thresholds, again with the majority moving from above to below the threshold (Table 3).
Discussion
The current study involving multiple international cohorts suggests that discordance between LS and FN BMD T-scores can contribute to fracture risk, independently of FRAX probabilities that incorporate FN BMD alone. The effect is small, however, with only a 9 % change in fracture risk for each 1SD difference in T-score between the two sites.
The present study has a number of limitations. We did not have access to the original scans and were unable to determine, therefore, whether vertebrae were excluded from analysis of LS BMD where there was evidence of significant confounding pathology, such as osteoarthritis, aortic calcification, facet joint arthritis or vertebral fracture. The fact that the discordant T-scores showed a near normal distribution, with an identical gradient of risk for those with higher or lower LS T-scores, suggests that this was not a significant limitation. A further limitation is the lack of consensus over an international reference standard for LS BMD. Recently, LS BMD values have also been published from NHANES III and it would be possible to re-compute our LS T-scores using these data [35]. It should be noted, however, that whilst the absolute LS T-score values may differ slightly, as long as the variance is similar this would have little or no impact on the gradient of risk analysis that examines the risk associated with a 1 SD decrease in the difference between T-scores (ΔLS–FN). The present analysis has been confined to the impact of discordance on the risk of future major osteoporotic fractures in women. Whether a similar conclusion would be reached for the hip fractures remains untested, but is unlikely given the fact that there is no incremental benefit of LS BMD over FN BMD alone for the prediction of hip fractures [36]. It is not clear if a similar result would be obtained in men. Finally, the current analysis does not take into account potential interactions between ΔLS–FN and individual variables within FRAX or its potential interaction with mortality.
Our findings are in keeping with the report from the Manitoba cohort [14] that also demonstrated that discordances between FN and LS BMD T-scores can contribute to fracture risk. Bearing in mind some of the limitations of the analysis, the gradient of risk for the discordance between the two sites in the present analysis (1.09/SD) is very similar to that reported by Leslie and colleagues (1.12/SD) [14]. Indeed, we observed a gradient of risk of 1.11/SD when the analysis was restricted to those subjects where the LS T-score was lower or higher than the FN. Leslie et al. have suggested that a relatively simple adjustment (approximately 10 % per SD) for major osteoporosis fracture probability may be an appropriate clinical tool to take such discordances into account. It is, however, important to note that the number of individuals who were reclassified following adjustment was small (2.3 % and 3.3 % for the NOGG and cohort-specific thresholds). At first glance, these values seem somewhat lower than the 8.3 % reclassification reported by Leslie [14]. This reflects a slight difference in the method of utilising ΔLS–FN for the estimation of the offset; in this study, for example, we applied the same weight to ΔLS–FN between −1 and −2, whereas Leslie used rounding to the nearest integer. While this will have a small impact to decrease the reclassification in our study, it is important to recall that the analysis of reclassification in the Manitoba study used movement across two thresholds (low-, medium- and high-risk groups). This would have been approximately halved with the use of a single threshold as in the NOGG approach that we have used. The small increment in risk stratification almost certainly reflects the modest, but significant, correlations between measurements of BMD at both sites (r = 0.5–0.7) [37, 38].
In summary, major discordances between LS and FN BMD T-scores are relatively uncommon but recognition of this issue may enhance the assessment of fracture risk where they exist. Our findings in a number of international cohorts are similar to that reported from a single cohort previously. It is important to note that adjustment of FRAX for these discrepancies impacts to a large extent on only a relatively small number of individuals in the context of clinical practise, but our results do provide some guidance for physicians, particularly those that report on the output of DXA to primary care.
References
Kanis JA On behalf of the WHO Scientific Group. Assessment of osteoporosis at the primary health-care level. Technical Report. Sheffield: WHO Collaborating Centre, University of Sheffield, UK2008
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19(4):385–397
McCloskey EV, Johansson H, Oden A, Kanis JA (2009) From relative risk to absolute fracture risk calculation: the FRAX algorithm. Curr Osteoporos Rep 7(3):77–83
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ 3rd, O’Neill T, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20(7):1185–1194
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC Jr, Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8(5):468–489
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312(7041):1254–1259
Stone KL, Seeley DG, Lui LY, Cauley JA, Ensrud K, Browner WS, Nevitt MC, Cummings SR (2003) BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res 18(11):1947–1954
National Osteoporosis Foundation (2008) Clinician’s guide to prevention and treatment of osteoporosis. Washington, DC: National Osteoporosis Foundation
Papaioannou A, Morin S, Cheung AM, Atkinson S, Brown JP, Feldman S, Hanley DA, Hodsman A, Jamal SA, Kaiser SM, Kvern B, Siminoski K, Leslie WD (2010) Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ 182(17):1864–1873
Baim S, Binkley N, Bilezikian JP, Kendler DL, Hans DB, Lewiecki EM, Silverman S (2008) Official Positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD Position Development Conference. J Clin Densitom 11(1):75–91
Kanis JA, Johnell O, Oden A, Johansson H, Eisman JA, Fujiwara S, Kroger H, Honkanen R, Melton LJ 3rd, O’Neill T, Reeve J, Silman A, Tenenhouse A (2006) The use of multiple sites for the diagnosis of osteoporosis. Osteoporos Int 17(4):527–534
Blake GM, Patel R, Knapp KM, Fogelman I (2003) Does the combination of two BMD measurements improve fracture discrimination? J Bone Miner Res 18(11):1955–1963
Leslie WD, Lix LM, Tsang JF, Caetano PA (2007) Single-site vs multisite bone density measurement for fracture prediction. Arch Intern Med 167(15):1641–1647
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA (2011) Spine-hip discordance and fracture risk assessment: a physician-friendly FRAX enhancement. Osteoporos Int 22(3):839–847
Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, Bonds D, Brunner R, Brzyski R, Caan B, Chlebowski R, Curb D, Gass M, Hays J, Heiss G, Hendrix S, Howard BV, Hsia J, Hubbell A, Jackson R, Johnson KC, Judd H, Kotchen JM, Kuller L, LaCroix AZ, Lane D, Langer RD, Lasser N, Lewis CE, Manson J, Margolis K, Ockene J, O’Sullivan MJ, Phillips L, Prentice RL, Ritenbaugh C, Robbins J, Rossouw JE, Sarto G, Stefanick ML, Van Horn L, Wactawski-Wende J, Wallace R, Wassertheil-Smoller S (2004) Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA 291(14):1701–1712
Hays J, Hunt JR, Hubbell FA, Anderson GL, Limacher M, Allen C, Rossouw JE (2003) The Women’s Health Initiative recruitment methods and results. Ann Epidemiol 13(9 Suppl):S18–S77
Kreiger N, Tenenhouse A, Joseph L, Mackenzie T, Poliquin S, Brown JP, Prior JC, Rittmaster RS (1999) The Canadian Multicentre Osteoporosis Study (CaMos): background, Rationale, Methods. Can J Aging 18:376–387
Gluer CC, Eastell R, Reid DM, Felsenberg D, Roux C, Barkmann R, Timm W, Blenk T, Armbrecht G, Stewart A, Clowes J, Thomasius FE, Kolta S (2004) Association of five quantitative ultrasound devices and bone densitometry with osteoporotic vertebral fractures in a population-based sample: the OPUS Study. J Bone Miner Res 19(5):782–793
Stewart A, Felsenberg D, Eastell R, Roux C, Gluer CC, Reid DM (2006) Relationship between risk factors and QUS in a European Population: the OPUS study. Bone 39(3):609–615
Melton LJ 3rd, Crowson CS, O’Fallon WM, Wahner HW, Riggs BL (2003) Relative contributions of bone density, bone turnover, and clinical risk factors to long-term fracture prediction. J Bone Miner Res 18(2):312–318
Melton LJ 3rd, Atkinson EJ, O’Connor MK, O’Fallon WM, Riggs BL (1998) Bone density and fracture risk in men. J Bone Miner Res 13(12):1915–1923
Jones G, Nguyen T, Sambrook PN, Kelly PJ, Gilbert C, Eisman JA (1994) Symptomatic fracture incidence in elderly men and women: the Dubbo Osteoporosis Epidemiology Study (DOES). Osteoporos Int 4(5):277–282
Nguyen T, Sambrook P, Kelly P, Jones G, Lord S, Freund J, Eisman J (1993) Prediction of osteoporotic fractures by postural instability and bone density. BMJ 307(6912):1111–1115
Fujiwara S, Kasagi F, Masunari N, Naito K, Suzuki G, Fukunaga M (2003) Fracture prediction from bone mineral density in Japanese men and women. J Bone Miner Res 18(8):1547–1553
Fujiwara S, Kasagi F, Yamada M, Kodama K (1997) Risk factors for hip fracture in a Japanese cohort. J Bone Miner Res 12(7):998–1004
Lunt M, Felsenberg D, Adams J, Benevolenskaya L, Cannata J, Dequeker J, Dodenhof C, Falch JA, Johnell O, Khaw KT, Masaryk P, Pols H, Poor G, Reid D, Scheidt-Nave C, Weber K, Silman AJ, Reeve J (1997) Population-based geographic variations in DXA bone density in Europe: the EVOS Study. European Vertebral Osteoporosis. Osteoporos Int 7(3):175–189
Lunt M, Felsenberg D, Reeve J, Benevolenskaya L, Cannata J, Dequeker J, Dodenhof C, Falch JA, Masaryk P, Pols HA, Poor G, Reid DM, Scheidt-Nave C, Weber K, Varlow J, Kanis JA, O’Neill TW, Silman AJ (1997) Bone density variation and its effects on risk of vertebral deformity in men and women studied in thirteen European centers: the EVOS Study. J Bone Miner Res 12(11):1883–1894
O’Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ (1996) The prevalence of vertebral deformity in european men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 11(7):1010–1018
Honkanen RJ, Honkanen K, Kroger H, Alhava E, Tuppurainen M, Saarikoski S (2000) Risk factors for perimenopausal distal forearm fracture. Osteoporos Int 11(3):265–270
Stewart A, Torgerson DJ, Reid DM (1996) Prediction of fractures in perimenopausal women: a comparison of dual energy x ray absorptiometry and broadband ultrasound attenuation. Ann Rheum Dis 55(2):140–142
Kwok AW, Gong JS, Wang YX, Leung JC, Kwok T, Griffith JF, Leung PC (2013) Prevalence and risk factors of radiographic vertebral fractures in elderly Chinese men and women: results of Mr. OS (Hong Kong) and Ms. OS (Hong Kong) studies. Osteoporos Int 24(3):877–885
Lekamwasam S, Adachi JD, Agnusdei D, Bilezikian J, Boonen S, Borgstrom F, Cooper C, Diez Perez A, Eastell R, Hofbauer LC, Kanis JA, Langdahl BL, Lesnyak O, Lorenc R, McCloskey E, Messina OD, Napoli N, Obermayer-Pietsch B, Ralston SH, Sambrook PN, Silverman S, Sosa M, Stepan J, Suppan G, Wahl DA, Compston JE (2012) A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int 23(9):2257–2276
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24(1):23–57
Compston J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, McCloskey EV, Reid DM, Selby P, Wilkins M (2009) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas 62(2):105–108
Looker AC, Melton LJ 3rd, Borrud LG, Shepherd JA (2012) Lumbar spine bone mineral density in US adults: demographic patterns and relationship with femur neck skeletal status. Osteoporos Int 23(4):1351–1360
Leslie WD, Lix LM (2011) Absolute fracture risk assessment using lumbar spine and femoral neck bone density measurements: derivation and validation of a hybrid system. J Bone Miner Res 26(3):460–467
Faulkner KG, von Stetten E, Miller P (1999) Discordance in patient classification using T-scores. J Clin Densitom 2(3):343–350
McCloskey EV, Murray SA, Miller C, Charlesworth D, Tindale W, O’Doherty DP, Bickerstaff DR, Hamdy NA, Kanis JA (1990) Broadband ultrasound attenuation in the os calcis: relationship to bone mineral at other skeletal sites. Clin Sci (Lond) 78(2):227–233
Acknowledgments
The Rochester study was supported by the National Institute of Musculoskeletal and Skin Diseases (R01 AR27065), U.S. Public Health Service. The AHS has been conducting at the Radiation Effects Research Foundation (RERF), Hiroshima and Nagasaki, Japan, which is a private, non-profit foundation funded by the Japanese Ministry of Health, Labour and Welfare (MHLW) and the U.S. Department of Energy (DOE), the latter in part through DOE Award DE-HS0000031 to the National Academy of Sciences. CaMos is currently funded by the Canadian Institutes for Health Research (CIHR), with additional support from Amgen, Merck Frosst Canada Ltd, and Eli Lilly and Company. The OSTPRE study was supported by the Academy of Finland. The Women’s Health Initiative programme is funded by the National Heart, Lung, and Blood Institute, the National Institutes of Health, and the US Department of Health and Human Services. Mr OS (Hong Kong) is also supported by National Institutes of Health funding. The Dubbo Osteoporosis Epidemiology study has been supported by the National Health and Medical Research Council of Australia and by untied educational grants from Amgen, GE-LUNAR, Lilly, Merck Sharp and Dohme, Novartis, Sanofi-Aventis and Servier.
Conflict of Interest
There are no conflicts of interest to declare.
Human and Animal Rights and Informed Consent
Participants in the cohorts included in this analysis provided informed consent at enrolment to the individual cohort studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johansson, H., Kanis, J.A., Odén, A. et al. Impact of Femoral Neck and Lumbar Spine BMD Discordances on FRAX Probabilities in Women: A Meta-analysis of International Cohorts. Calcif Tissue Int 95, 428–435 (2014). https://doi.org/10.1007/s00223-014-9911-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-014-9911-2