Abstract
Introduction
It remains controversial whether coronal laxity after total knee arthroplasty (TKA) is a critical factor in determining clinical outcomes such as knee range of motion (ROM). The purpose of this study was to evaluate the correlation between postoperative ROM and coronal laxity, which was defined as the angular motion from the neutral, unloaded position to the loaded position, in patients with medial knee osteoarthritis undergoing TKA.
Materials and methods
Preoperative and 1-year postoperative coronal laxity were assessed using radiographs by applying a force of 150 N with an arthrometer. A consecutive series of 204 knees was examined. A knee was defined as clinically “balanced” when the difference between medial and lateral laxity was 3° or less. Active ROM was measured using a goniometer. Values were expressed as median values.
Results
The ROM was 105° preoperatively and 110° postoperatively, with the correlation being weak (r = 0.372, p < 0.001) between the periods. The total laxity also revealed a weak correlation (r = 0.270, p < 0.001) between the periods. Preoperative laxity was significantly larger (4° vs. 3°) on the medial side (p < 0.001) and postoperative laxity was larger (4° vs. 3°) laterally (p = 0.001). There was no significant correlation between postoperative ROM and laxity pre- and postoperatively. Additionally, there were no differences in ROM between the balanced and unbalanced groups in the pre- and postoperative periods.
Conclusions
This study indicated that mediolateral coronal laxity in patients with an osteoarthritic knee did not correlate with knee ROM after TKA when 3°–4° of laxity in the medial and lateral orientations was maintained.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee range of motion (ROM) after total knee arthroplasty (TKA) is one of the main variables used to objectively evaluate clinical outcomes [1, 2]. In addition, because knee ROM has been reported to affect patient satisfaction after TKA [3, 4], many surgeons [5,6,7,8,9] have cited the importance of factors influencing ROM after TKA.
Stability after TKA is known to be an important driver of patient-specific outcomes after reconstruction, and is associated with medial and lateral coronal laxity [10,11,12]. Adequately balancing the soft tissues may be one of the key factors in achieving a successful TKA [13, 14]. In fact, coronal laxity during surgery [15,16,17] and after surgery [18, 19] was reported to be an important factor affecting ROM after TKA. Some have reported that postoperative ROM is affected by lateral laxity [15, 18], and others have shown that it is affected by balanced laxity [16, 17, 20]. Lateral laxity and well-balanced laxity may affect the physiological kinematics of the native knee that contribute to improved postoperative knee flexion angle. However, there have been no reports, to the authors’ knowledge, that have evaluated the correlation between ROM and coronal laxity before and after TKA.
Therefore, the purpose of this study was to clarify the effects of coronal laxity and balance on knee ROM before and after TKA.
Materials and methods
This prospective, quasi-randomized study was performed at our clinic between July 2008 and November 2016. Informed consent, which included a description of the protocol and potential arthrometer-related complications, was obtained from all patients. Ethical approval for this study was obtained. The LCS® Total Knee System (DePuy, Warsaw, IN, USA) was used in all patients (197 patients; 204 knees), with either a posterior cruciate ligament (PCL)-retaining (CR) design (82 patients; 82 knees) or a PCL-substituting (PS) design (115 patients; 122 knees). In all patients, the preoperative diagnosis was medial osteoarthritis (OA) of the knee. All TKAs were unilateral procedures performed under general anesthesia; all patients with bilateral disease were scheduled to undergo staged bilateral TKA. The LCS system has a spherical surface between the femoral component and the tibial insert in both designs, which allows varus–valgus motion without loss of congruent contact [21].
Each patient chose which knee would undergo the first TKA. The timing of the second TKA was determined based on the patient’s self-reported ability to tolerate the additional pain and limited activities of daily living during the postoperative period. Initially, the order in which the implant designs were used was quasi-randomized; patients with even medical record numbers received the CR implant first, while those with odd medical record numbers received the PS implant first. Unexpectedly, the PCL-retaining design was discontinued by the manufacturer at the end of January 2013, and the TKA procedures were performed using only the substituting design after that time.
One surgeon performed all of the TKAs using a standardized technique, including the necessary soft tissue release for proper balance; the surgical technique and rehabilitation protocol were described in detail in a previous report [22]. In all knees, the femoral components were fixed without cement and the tibial components were fixed with cement. Proper intraoperative mediolateral coronal stability was confirmed manually, although it was not quantified intraoperatively. Contraindications for surgery included revision arthroplasties, previous tibial osteotomies, and the presence of rheumatoid arthritis. The clinical characteristics of the patients are summarized in Table 1.
Laxity evaluations
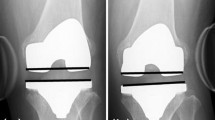
The laxity of the medial and lateral sides was measured with a Telos arthrometer (Fa Telos; Medizinisch-Technische Gerätebau GmbH, Sulzbach, Germany) with the patient lying supine on a table. For the medial/lateral stress test, a force of 150 N was applied just above the joint on the lateral or medial femoral condyle. To measure the medial and lateral angles, the femoral boundary used was the distal convex margin of the condyles. The tibial boundary was the outer margin of the condyles. The neutral, unloaded position was defined as the baseline. Based on the criteria of Siston et al. [14] and Ishii et al. [24], we defined a knee as clinically “balanced” when the difference between the medial and lateral laxity was 3° or less. The laxity was assessed preoperatively (Fig. 1) and at 12 months postoperatively (Fig. 2), which provided sufficient time to predict laxity following TKA, because coronal laxity in either type of knee prosthesis has been shown to not change significantly between 1 year and a minimum of 5 years after surgery [12].
Preoperative measurement of medial (a) and lateral laxity (c) with a Telos arthrometer while applying a force of 150 N (a 75-year-old female). b The neutral position without being loaded (the baseline). To measure the medial and lateral angles, the femoral boundary used was the distal convex margin of the condyles using a white dotted line. The tibial boundary was the outer margin of the condyles (tibial plateau line) using a white dotted line. Medial and lateral laxities of 4°, respectively, were observed from the baseline, although maximum values were 1° on the medial and 7° on the lateral side
Measurement of medial (a) and lateral (c) laxity with a Telos arthrometer while applying a force of 150 N, and b the neutral position without being loaded (the baseline) of the same patient in Fig. 1 at 1 year postoperatively. Medial and lateral laxities of 4°, respectively, were observed from the baseline
Reproducibility
An experienced technician (K.T.) performed all tests. To measure the test–retest reliability, the intraclass correlation coefficients and 95% confidence intervals (95% CI) were calculated for the three angles in the maximum medial, neutral, and maximum lateral positions. Each value was measured twice in 20 specimens.
Concerning test–retest reliability, the intraclass correlation coefficient (95% CI) was 0.971 (0.928–0.988) for the maximum medial position, 0.935 (0.843–0.974) for the neutral, and 0.962 (0.900–0.985) for the maximum lateral position. The standard error of the measurement (maximum error) was 0.354 (0.474) for the maximum medial position, 0.525 (0.736) for the neutral, and 0.412 (0.534) for the maximum lateral position.
ROM evaluations
An experienced physical therapist (TS) measured active maximum knee flexion and extension using a standard hand-held goniometer with 38-cm-long arms while the patient was supine in non-weight-bearing conditions. The lateral femoral condyle was used as the landmark to center the goniometer, with the stationary arm directed toward the greater trochanter and the movable arm directed toward the lateral malleolus. The amount of knee flexion was measured and recorded to the nearest 5°. Finally, the ROM was calculated as the range between the extension and flexion angles. The flexion angle was assessed preoperatively and at 12 months postoperatively, which provided sufficient time to predict ROM following TKA [8, 25, 26].
Statistical analyses
All values were expressed as medians (and 25th–75th percentiles). Continuous variables were compared using the Wilcoxon’s rank-sum test, Wilcoxon’s signed-rank test, and Kruskal–Wallis test. Discrete variables were compared using the Chi-square and Fisher’s exact test. Spearman’s rank correlation coefficient was used to test the relationship between variables. The strength of the correlation of the rank coefficients was defined as: strong = 0.70–1.0, moderate = 0.40–0.69, or weak = 0.20–0.39. Multivariable logistic regression analysis with the stepwise variable selection method was performed to identify factors associated with improvement in postoperative ROM. In all tests, a p value less than 0.05 was considered as significant. All statistical analyses were performed using IBM SPSS Statistics ver. 23 (IBM Japan, Tokyo, Japan).
Results
The ROM was 105° [90°, 120°] preoperatively and 110° [95°, 120°] at 1 year postoperatively, with a weak correlation (r = 0.372, p < 0.001) between the periods. The total laxity also revealed a weak correlation (r = 0.270, p < 0.001) between the periods (Table 2). In addition, the difference between pre- and postoperative ROM (dROM; 0 [− 10, 15]) showed a significant moderate negative correlation with preoperative ROM (R = − 0.637, p < 0.001) and a moderate positive correlation with postoperative ROM (R = 0.414, p < 0.001). Finally, preoperative laxity was significantly larger (4° [3°, 5°] vs. 3° [2°, 4°]) on the medial side (p < 0.001) and postoperative laxity was larger (4° [3°, 5°] vs. 3° [2°, 4°]) on the lateral side (p = 0.001) (Table 2).
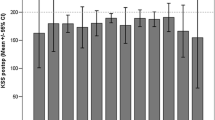
There was no significant correlation between postoperative ROM and the pre- and postoperative laxity values (medial, lateral, and total) (Table 3; Fig. 3a–c).
Despite differences in the pattern of the ROM changes before and after TKA, which indicated that one group had a maintained or improved ROM and the other had a deteriorated ROM, no significant differences were found in medial, lateral, and total coronal laxity between them (Table 4). Multivariate analysis (multiple logistic regression analysis) was performed simultaneously, which recognized the dependent variable as the improvement in postoperative ROM compared with preoperative ROM, but there was no significant independent variable in this series.
Regarding the correlation between the balance in coronal laxity and ROM, we first compared whether the characteristics of laxity on the medial–lateral side after TKA (with either one being larger than the other) had an effect on postoperative ROM. In accordance with patients’ conditions, they were stratified into three groups: lateral < medial, 60 knees, 110 [100, 120]; lateral = medial, 27 knees, 110 [90, 115]; and lateral > medial, 117 knees, 105 [93, 120]. No significant difference in ROM was observed among the three groups (p = 0.073).
When a difference of 3° or less in coronal laxity was defined as “balanced”, approximately 90% (183/204) of patients had a balanced knee preoperatively, and 80% (168/204) were balanced postoperatively. Additionally, there were no differences in ROM between the balanced and unbalanced groups in either the pre- or postoperative period (preoperative; p = 0.384, postoperative; p = 0.157) (Table 5).
Finally, patients were divided into four groups according to the patterns of the changes in the balance conditions from before to after TKA: (1) balanced to balanced, 148 knees; (2) balanced to unbalanced, 35 knees; (3) unbalanced to balanced, 20 knees; and (4) unbalanced to unbalanced, 1 knee. The Kruskal–Wallis test was used to evaluate whether there were differences in the postoperative ROM among these groups. The groups had ROMs of 110° [95°, 120°], 115° [103°, 120°], 100° [94°, 110°], and 130°, respectively, and there were no significant differences among the groups (p = 0.091).
Discussion
The most important finding of this study was that the mediolateral laxities did not correlate with postoperative ROM. Simultaneously, there was no correlation between postoperative ROM and changes in mediolateral laxity. However, our results were obtained in patients whose TKAs were generally well balanced, with ranges of coronal laxity generally in the ideal range, as described by previous studies [10,11,12]. Our results should not be considered to mean that coronal laxity, or stability more generally, is unimportant. To the contrary, proper stability and balance of TKAs is important to ROM and function, since TKAs in this study were categorized as clinically successful.
We first evaluated the correlation between laxity and ROM in the CR and PS designs simultaneously. However, Table 1 shows that both designs had comparable clinical outcomes in terms of the HSS score and pre- and postoperative ROM. Additionally, there were no differences between groups with regard to coronal laxity before and after surgery. Therefore, it was statistically reasonable to evaluate the two designs simultaneously in this study.
Preoperative ROM is currently regarded as the principal factor predicting postoperative ROM [5, 8, 9]. Our study also indicated that patients with good knee ROM preoperatively tended to obtain a good postoperative ROM, despite the weak correlation between the periods. Total laxity also showed a weak correlation between before and after TKA. We speculate that the reason that total laxity postoperatively was determined by the more lax side preoperatively was to obtain a balanced knee during surgery. As a result, patients with larger laxity preoperatively may tend to have a larger laxity postoperatively. Siston et al. also [14] observed no difference between the total arc of varus–valgus motion before and after primary TKA in extension and flexion.
Mediolateral coronal laxity has been reported to be asymmetric even in the native knee [24, 27]. Medial knee OA also showed asymmetric coronal laxity. Preoperative laxity was significantly larger on the medial side and postoperative laxity was larger on the lateral side. We speculate that a larger laxity may be mainly induced not by the changes in the properties of soft tissues but by those of the hard tissues such as the femoral and tibial cartilage or bone. Considering that tibiofemoral angle (TFA) in the native knee was reported to be 178° [24], a TFA of 181° in this series might not be a severe enough varus deformity to intrinsically change the properties of the medial and lateral soft tissue structures. Thus, the larger preoperative laxity in the medial soft tissues may have occurred due to the femur and tibia moving closer to one another as a result of decreased cartilage height or bony attrition. However, the larger postoperative laxity in lateral soft tissue tension may have also occurred due to the femur and tibia moving closer to one another due to correction in alignment from the varus to valgus knee. Bellemans et al. [28] may support our speculations. They reported that none of the intrinsic shortening of the medial collateral structures or stretching of the lateral soft tissues occurs when the preoperative deformity is not severe (e.g., when it does not exceed 10°), although they evaluated the varus deformity with the mechanical axis of the femur and tibia.
Various factors have been shown to be involved in knee ROM after TKA, including preoperative flexion angle [5, 6, 8], preoperative alignment [6, 8], implant design [9, 29], posterior tibial slope [7, 30], anterior movement of the femur [30, 31], surgical technique [8, 19], and rehabilitation protocol [32, 33]. Although proper soft tissue balance was reported to be one of the most important factors for postoperative function and implant durability in TKA [10,11,12,13], the current study indicated that, when the laxity was maintained at approximately 3° or 4° on the medial and lateral sides and 7° in total, the coronal laxity was not correlated with postoperative ROM.
With regard to the changes in ROM from before to after TKA, a couple of papers [9, 26] reported that patients with limited ROM preoperatively demonstrated an improvement in ROM postoperatively, whereas patients with a large preoperative ROM tended to lose motion. The results of our study had a similar pattern. Therefore, preventing the deterioration of postoperative ROM in patients with good ROM preoperatively could be one of the strategies for obtaining good clinical outcomes as well as for improving postoperative ROM in those with limited ROM preoperatively.
Finally, the laxity on the medial and lateral sides has little effect on postoperative ROM. In addition, no significant difference was observed between the different changing patterns of coronal balance between before and after surgery. Based on these results, it seems reasonable to conclude that the balance in coronal laxity does not correlate with the postoperative ROM after TKA.
There were several limitations of this study. First, the results may not be generalizable to all patients with knee arthroplasties, because participants in this study were patients with medial OA knee who had generally well-balanced knees with few outliers in either ROM or coronal laxity after surgery. Second, the laxity was evaluated only in knee extension owing to the characteristics of the arthrometer used. We are aware of the importance of evaluating laxity over the entire range of knee flexion to confirm proper tension in the coronal plane [34]. However, considering that both medial and lateral laxity in both designs showed about 4° laxity in extension and 3° in 75° of flexion using this arthrometer [20], the different flexion angles in these designs may have less of a clinical impact on coronal laxity. In addition, this study focused on the coronal laxity, so we did not take sagittal laxity into account. Third, the data from knees with medial OA may not be generalizable to patients with lateral OA, because medial and lateral OA have unique characteristics [35].
In conclusion, the preoperative coronal laxity was balanced in 90% of patients with advanced medial OA of the knee, and in 80% of patients after surgery. Clinically, an evaluation using stress radiographs may be useful to obtain information on whether TKA patients have a balanced or unbalanced knee with regard to coronal laxity pre- and postoperatively. This study indicated that mediolateral coronal laxity did not correlate with knee ROM after TKA when 3°–4° laxity in the medial and lateral orientations was maintained.
References
Alicea J (2001) Scoring systems and their validation for the arthritic knee. In: Insall JN, Scott WN (eds) Surgery of the knee, vol 2, 3rd edn. Churchill Livingstone, New York, pp 1507–1515
Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN (2012) The new knee society knee scoring system. Clin Orthop Relat Res 470:3–19
Matsuda S, Kawahara S, Okazaki K, Tashiro Y, Iwamoto Y (2013) Postoperative alignment and ROM affect patient satisfaction after TKA. Clin Orthop Relat Res 471:127–133
Padua R, Ceccarelli E, Bondì R, Campi A, Padua L (2007) Range of motion correlates with patient perception of TKA outcome. Clin Orthop Relat Res 460:174–177
Gatha NM, Clarke HD, Fuchs R, Scruderi GR, Insall JN (2004) Factors affecting postoperative range of motion after total knee arthroplasty. J Knee Surg 17:196–202
Kawamura H, Bourne RB (2001) Factors affecting range of flexion after total knee arthroplasty. J Orthop Sci 6:248–252
Malviya A, Lingard EA, Weir DJ, Deehan DJ (2009) Predicting range of movement after knee replacement: the importance of posterior condylar offset and tibial slope. Knee Surg Sports Traumatol Arthrosc 17:491–498
Ritter MA, Harty LD, Davis KE, Meding JB, Keating EM (2003) Predicting range of motion after total knee arthroplasty. J Bone Jt Surg Am 85:1278–1285
Schurman DJ, Rojer DE (2005) Total knee arthroplasty: range of motion across five systems. Clin Orthop Relat Res 430:132–137
Ishii Y, Matsuda Y, Ishii R, Sakata S, Omori G (2003) Coronal laxity in extension in vivo after total knee arthroplasty. J Orthop Sci 8:538–542
Matsuda Y, Ishii Y (2004) In vivo laxity of low contact stress mobile- bearing prostheses. Clin Orthop Relat Res 419:138–143
Takeda M, Ishii Y, Noguchi H, Matsuda Y, Sato J (2012) Changes in varus-valgus laxity after total knee arthroplasty with a minimum five-year follow-up. Knee Surg Sports Traumatol Arthrosc 20:1984–1989
Mihalko WM, Saleh KJ, Krackow KA, Whiteside LA (2009) Soft-tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg 17:766–774
Siston RA, Goodman SB, Delp SL, Giori NJ (2007) Coronal plane stability before and after total knee arthroplasty. Clin Orthop Relat Res 463:43–49
Nakano N, Matsumoto T, Muratsu H, Takayama K, Kuroda R, Kurosaka M (2016) Postoperative knee flexion angle is affected by lateral laxity in cruciate-retaining total knee arthroplasty. J Arthroplasty 31:401–405
Tsukeoka T, Tsuneizumi Y, Yoshino K (2017) The rectangular flexion gap is associated with an increased knee flexion angle in a cruciate-sacrificing rotating platform mobile-bearing total knee arthroplasty. J Orthop Sci 22:313–317
Watanabe T, Muneta T, Sekiya I, Banks SA (2015) Intraoperative joint gaps and mediolateral balance affect postoperative knee kinematics in posterior-stabilized total knee arthroplasty. Knee 22:527–534
Kobayashi T, Suzuki M, Sasho T, Nakagawa K, Tsuneizumi Y, Takahashi K (2012) Lateral laxity in flexion increases the postoperative flexion angle in cruciate-retaining total knee arthroplasty. J Arthroplasty 27:260–265
Matsuda Y, Ishii Y, Noguchi H, Ishii R (2005) Varus-valgus balance affects the range of movement after total knee arthroplasty. J Bone Jt Surg Br 87:804–808
Matsuda Y, Ishii Y, Noguchi H, Ishii R (2005) Effect of flexion angle on coronal laxity in patients with mobile-bearing total knee arthroplasty prostheses. J Orthop Sci 10:37–41
Pappas MJ (2002) Engineering design of the LCS replacement. In: Hamelynck KJ, Stiehl JB (eds) LCS mobile bearing knee arthroplasty: a 25 years worldwide review. Springer, Berlin, pp 39–52
Ishii Y, Noguchi H, Takeda M, Sato J, Toyabe S (2011) Prediction of range of motion 2 years after mobile-bearing total knee arthroplasty: PCL-retaining versus PCL-sacrificing. Knee Surg Sports Traumatol Arthrosc 19:2002–2008
Kellgren JH, Lawrence JS (1957) Radiographical assessment of osteoarthritis. Ann Rheum Dis 16:494–502
Ishii Y, Noguchi H, Sato J, Ishii H, Todoroki K, Toyabe SI (2018) Medial and lateral laxity in knees with advanced medial osteoarthritis. Osteoarthr Cartil 26:666–670
Chaudhary R, Beaupré LA, Johnston DWC (2003) Knee range of motion during the first two years after use of posterior cruciate-stabilizing or posterior cruciate-retaining total knee prostheses—a randomized clinical trial. J Bone Jt Surg Am 90:2579–2586
Parsley BS, Engh GA, Dwyer KA (1992) Preoperative flexion. Does it influence postoperative flexion after posterior-cruciate-retaining total knee arthroplasty? Clin Orthop Relat Res 275:204–210
Deep K (2014) Collateral ligament laxity in knees: what is normal? Clin Orthop Relat Res 472:3426–3431
Bellemans J, Vandenneucker H, Vanlauwe J, Victor J (2010) The influence of coronal plane deformity on mediolateral ligament status: an observational study in varus knees. Knee Surg Sports Traumatol Arthrosc 18:152–156
Dennis DA, Komistek RD, Stiehl JB, Walker SA, Dennis KN (1998) Range of motion after total knee arthroplasty: the effect of implant design and weight-bearing conditions. J Arthroplasty 13:748–752
Massion P, Gournay A (2006) Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthroplasty 21:889–896
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemance A (2002) Fluoroscopic analysis of the kinematics deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Jt Surg Br 84:50–53
Mauerhan DR, Mokris JG, Ly A, Kiebzak GM (1998) Relationship between length of stay and manipulation rate after total knee arthroplasty. J Arthroplasty 13:896–900
Ranawat CS, Ranawat AS, Mehta A (2003) Total knee arthroplasty rehabilitation protocol. What makes the difference? J Arthroplasty 18(1 Suppl):27–30
Hino K, Kutsuna T, Watamori K, Kiyomatsu H, Ishimaru Y, Takeba J, Watanabe S, Shiraishi Y, Miura H (2017) Varus-valgus stability at 90° flexion correlates with the stability at midflexion range more widely than that at 0° extension in posterior-stabilized total knee arthroplasty. Arch Orthop Trauma Surg 137:1429–1434
Muraki S, Akune T, En-Yo Y, Yoshida M, Suzuki T, Yoshida H, Ishibashi H, Tokimura F, Yamamoto S, Tanaka S, Nakamura K, Kawaguchi H, Oka H, Yoshimura N (2015) Joint space narrowing, body mass index, and knee pain: the ROAD study (OAC1839R1). Osteoarthr Cartil 23:874–881
Acknowledgements
We thank Koji Todoroki RT and Tetsuya Sakurai PT for their contributions in gathering the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ishii, Y., Noguchi, H., Sato, J. et al. Mediolateral coronal laxity does not correlate with knee range of motion after total knee arthroplasty. Arch Orthop Trauma Surg 139, 851–858 (2019). https://doi.org/10.1007/s00402-019-03161-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03161-3