Abstract
Purpose
Favourable long-term results after total knee arthroplasty (TKA) require appropriate soft tissue balance. However, the relationships between long-term results after TKA surgery and mediolateral laxities at extension and at 90° flexion remain unknown. This study therefore quantitatively assessed ligament balance at extension and at 90° knee flexion at least 10 years after primary TKA, as well as clarifying the relationships between long-term outcomes and mediolateral laxities.
Methods
This study included 49 knees (19 CR type and 30 PS type) of 33 patients followed up for at least 10 years after TKA at our hospital. Plain radiographs were obtained with about 150 N of varus or valgus stress using a Telos arthrometer at extension. At 90° flexion, epicondylar views were obtained under a 1.5-kg load and with about 10 kg of varus or valgus stress.
Results
Lateral laxity of about 5° was observed in both extension and flexion, with total laxities of varus and valgus stress each less than 10°. Postoperative clinical outcomes were good, with significant improvements in extension angle, femorotibial angle, and KSS, and no loosening in any knee.
Conclusions
Good long-term results of TKA can be obtained with a lateral laxity of about 5°, equivalent to that of healthy knees.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Favourable long-term results of total knee arthroplasty (TKA) require the achievement of an appropriate soft tissue balance. Soft tissue balance may be achieved by equalizing the joint gaps at extension and at 90° flexion and by making each joint gap rectangular [3]. Various surgical techniques and tensor/balancer devices have been developed to achieve gap and ligament balance from extension to deep flexion [11, 12]. However, making the joint gaps at extension and at 90° flexion completely rectangular is difficult [8, 9]. Since healthy knees have physiological lateral laxity [13, 19], mild lateral laxity may be acceptable after TKA. To determine the extent of lateral laxity allowable, it is necessary to compare ligament balance at extension and at 90° flexion and to evaluate clinical outcomes after TKA. Ligament balance at extension after TKA has been assessed manipulatively or using the Telos arthrometer. For example, assessment of ligament balance in extension in 77 patients 5–9 years after TKA showed that mediolateral laxity within about 4° produced favourable clinical outcomes, with no clinical complications and a good range of motion [4]. However, the relationships between long-term outcomes after TKA surgery and mediolateral laxities at extension and at 90° flexion remain unknown.
This study hypothesized that patients with mild lateral laxities at extension and at 90° flexion after TKA have good long-term clinical outcomes. This study therefore evaluated the relationships between mediolateral laxity and long-term outcomes at least 10 years after TKA, with ligament balance at extension assessed using a Telos arthrometer and ligament balance at 90° flexion assessed using the trans-epicondylar view [5, 18].
Materials and methods
This study included 49 knees in 33 patients followed up for a minimum of 10 years after TKA at our hospital. The 33 patients consisted of 1 man and 32 women, of median age 81 years (range 67–95 years) and a mean follow-up period of 12 years, 8 months (range 10 years, 0 months–19 years, 8 months). TKA was performed using a cruciate-retaining design (CR type) in 19 knees (mean follow-up, 14 years, 5 months) and a posterior-stabilizing design (PS type) in 30 knees (mean follow-up, 11 years, 3 months) (Table 1). Two knees had valgus deformities and 47 had varus deformities. The underlying disease was osteoarthritis in 45 knees and spontaneous osteonecrosis of the medial femoral condyle in 4 knees; knees with infection and autoimmune disease were excluded.
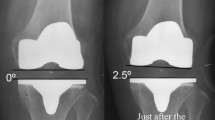
Plain radiographs were obtained with about 150 N of varus or valgus stress added using a Telos arthrometer (Fa Telos, Medizinisch-Technische, Griesheim, Germany) at knee extension. At 90° flexion, an epicondylar view was obtained under a 1.5-kg load and with about 10 kg of varus or valgus stress by manipulation [5, 18] (Figs. 1, 2). The post-operative condylar twist angle (CTA), defined as the angle formed by the femoral posterior condylar axis and the clinical trans-epicondylar axis (CEA), was measured, and femoral rotational alignment was assessed. Varus and valgus laxities were assessed by measuring on film the angle formed by the tangential lines on the femoral condyles and the tibial plateau.
Other factors assessed included pre- and post-operative joint ranges of motion, femorotibial angle (FTA), Knee Society Score (KSS), postoperative implant looseness, CTA, varus and valgus laxities during extension and 90° flexion stress and the between-implant inclination angle at 90° flexion under a 1.5-kg load. Implant loosening was assessed by the presence of a surrounding radiolucent line and/or subsidence. Lateral laxity was defined as positive. Between-implant inclination angle was measured twice by one observer at different times to determine intraobserver reliability, and blindly and independently by three observers to determine interobserver reliability (Table 2). This study was approved by the Institutional Review Board in Kyoto Prefectural University of Medicine (approval number: ERB-C-221).
Statistical analysis
All data were analysed using the R statistical software package. Data were compared by one-way analysis of variance, with p < 0.05 defined as statistically significant. Intraclass correlation coefficients (ICCs) were calculated with two-way random model using SPSS (version 21.0 for Windows; IBM, Chicago, IL).
Results
Pre- and post-operatively, the average extension angles were −9° ± 9° and 1° ± 3°, respectively (p < 0.01), while the average flexion angles were 117° ± 18° and 114° ± 12°, respectively (n.s.). Mean FTA was significantly lower (p < 0.01), while mean KSS was significantly higher (p < 0.01), after than before TKA (Table 3). None of the knees showed evidence of implant looseness, such as a surrounding radiolucent line or subsidence. The average joint laxities at extension were 5° ± 3° (range 0°–11°) in varus and 3° ± 2° (range 0°–7°) in valgus. At 90° flexion, the average joint laxities were 6° ± 4° (range 0°–20°) in varus and 4° ± 3° (range 0°–9°) in valgus, with laxities being about 2° higher at varus than at valgus at both the extended position (p < 0.01) and 90° flexion (p = 0.013). The total laxity of varus and valgus stress was stable, with means of 7° ± 3° (range 1°–16°) at extension and 10° ± 5° (range 0°–21°) at 90° flexion (p = 0.016). A comparison of CR- and PS-type knees showed that both had similar varus–valgus laxities in extension (p < 0.01 each). At 90° flexion, the CR type tended to have varus laxity (p = 0.056), but there was no significant varus–valgus difference observed with the PS type (n.s.). Mean laxity at a flexed, 1.5-kg load position was 2° ± 3° (range −4° to 20°), with mild lateral laxity (<5°) observed in 45 (92 %) of the 49 knees. The mean CTA was 3° ± 2° (range 0°–20°), with no readily apparent failure of the femoral rotation position observed.
Discussion
The most important finding of the present study was that lateral laxities of about 5° at both extension and 90° flexion were acceptable at long-term follow-up after TKA surgery.
Factors that affect the long-term results of TKA include soft tissue balance and the position of implant installation. Excessive instability resulting from poor soft tissue balance causes wearing of the polyethylene and breakage of the implant [6, 20]. Therefore, an appropriate soft tissue balance is important for obtaining favourable long-term results. Soft tissue balance includes the balance at extension and at 90° flexion. It has been recommended that adjustments be made to equalize balances at extension and at 90° flexion and that the joint gaps be rectangular [3]. However, only 7.7 % of knees were found to have perfectly rectangular gaps [2], and even experienced surgeons find it difficult to equalize the extension and 90° flexion balances and to make the joint gaps rectangular. Although favourable long-term outcomes of TKA have been reported, the relationships between these outcomes and mediolateral laxities at extension and at 90° flexion remain unknown. This study was therefore designed to evaluate these relationships a minimum of 10 years after TKA.
An evaluation of physiological laxity in healthy knees using varus–valgus stress images found that both extension and flexion had about 3° of lateral laxity [ 13 ], with healthy knees also reported to have mild lateral laxity. An assessment of extended-position balance and range of motion 1 year after TKA in 80 patients reported significant improvements in range of motion in patients with a <2° varus–valgus difference, when compared with patients with a ≥2° varus–valgus difference, as well as in patients with a total varus–valgus laxity of 6°–10°, when compared with patients with a total varus–valgus laxity <6° or >10° [7]. An assessment of 77 patients 5–9 years after TKA reported that mediolateral laxity within about 4° produced favourable clinical outcomes at extension [4]. Taken together, these findings showed that good soft tissue balance was associated with favourable postoperative clinical outcomes and range of motion. However, the effects of good soft tissue balance on long-term results had not been determined. This study showed a mean lateral laxity at extension of about 5°, a 2° varus–valgus difference and a total varus–valgus laxity of 7°. Postoperative results showed favourable clinical outcomes, with significant improvements in extension range of motion, FTA, and KSS, and no looseness in any of the knees. Taken together, these findings indicate that good soft tissue balance is related to favourable long-term clinical outcomes.
Various methods have been developed to measure knees in flexion. The epicondylar view consists of plain radiograph with the knee in 90° flexion; this method also allows for imaging at a flexed position under conditions of varus–valgus stress [5]. This method has been reported to correlate with intraoperative measurements using a tensor/balancer device [10], but this correlation has not been determined in patients undergoing long-term follow-up after TKA. Installation of the femoral component at a significantly internally rotated position into knees showing lateral instability in flexion yielded poor clinical outcomes, including pain [14]. Based on the recommendation that the femoral component be approximately 3° internal to the CEA [5], none of the knees evaluated in this study showed a readily apparent poor femoral rotational alignment (mean 3° ± 2°), with the position of installation having little impact on ligament balance. Moreover, lateral laxity of about 5° was observed at 90° of flexion, and the total varus–valgus laxity was less than 10° for both flexion and extension. One report found no evidence of lift-off at about 5° of laxity [3]. Mild lateral laxity after TKA surgery was reported necessary for the reproducibility of the medial pivot pattern in flexion [1], consistent with results showing that healthy knees in a flexed position had about 5° of physiological lateral laxity and a varus–valgus total of about 10° [19]. Thus, mild lateral laxity, equivalent to that of healthy knees, should yield favourable long-term results after TKA.
Although several recently developed tensor/balancer devices [9] were found to enhance appropriate soft tissue balance during surgery, perfect matches of soft tissue balances remain difficult. Use of offset-type tensor to assess 135 knees, 90 CR type and 45 PS type, that underwent osteotomy using the gap technique, and 120 patients, 20 with CR type and 100 with PS type, that underwent osteotomy using the measured-resection technique, found that a rectangular form could be acquired in only 66.7 % of the CR type and 44.4 % of the PS type using the gap technique and in only 50.0 and 28.0 %, respectively, using the measured resection technique [8]. The results presented here also showed a 2° varus–valgus difference in the between-implant inclination angle for both extension and 90° flexion and that it was difficult to adjust to a rectangular form.
In the flexed position, CR-type knees showed lateral laxity, whereas PS-type knees did not show a significant difference in varus–valgus. PCL interruption has been reported to increase medial laxity in a flexed position [15] and may have resulted in lower lateral laxity when using PS-type knees. These findings indicate that PS-type knees in particular require strict adjustments of soft tissue balance to prevent medial laxity in a flexed position. The mild lateral laxity allowable in extension and 90° flexion is clinically relevant.
This study had several limitations, include the small numbers of patients and knees and the lack of assessment of midflexion instability. In addition, comparisons were made using different models. Also the results were skewed towards patients who performed well after TKA, as this study only assessed patients followed up for a minimum 10 years who did not undergo revisions during this time period. Moreover, changes in lateral laxity over time have not been assessed. Although one study reported that mean lateral laxity in an extended position, from immediately after TKA surgery until 1 year later, was reduced by about 4° [16], another found that varus–valgus laxity increased over time after TKA [21], and a third observed no readily apparent changes over time [17]. These reports assessed short-term progression after surgery, indicating a need for studies assessing long-term results.
Conclusion
Favourable long-term clinical outcomes were observed in patients who underwent TKA, with soft tissue balance being stable in both extended and flexed positions and a mild lateral opening observed. None of the knees included experienced looseness of implants or poor rotational installation. These results suggest that lateral laxity of about 5° is acceptable at long-term follow-up after TKA surgery.
References
Freeman MAR (1997) Soft tissues: a question of balance. Orthopedics 20:827–831
Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15:970–973
Insall JN (1993) Surgery of the knee, vol 26, 2nd edn. Churchill Livingstone, New York, pp 739–804
Ishi Y, Matsuda Y, Ishii R, Sakata S, Omori G (2003) Coronal laxity in extension in vivo after total knee arthroplasty. J Orthop Sci 8:538–542
Kanekasu K, Kondo M, Kadoya Y (2005) Axial radiography of the distal femur to assess rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 434:193–197
Lewis P, Rorabeck CH, Bourne RB, Devane P (1994) Posteromedial tibial polyethylene failure in total knee replacements. Clin Orthop Relat Res 299:11–17
Matsuda Y, Ishii Y, Noguchi H, Ishii R (2005) Varus–valgus balance and range of movement after total knee arthroplasty. J Bone Joint Surg 87-B:804–808
Matsumoto T, Muratsu H, Kawakami Y, Takayama K, Ishida K, Matsushita T, Akisue T, Nishida K, Kuroda R, Kurosaka M (2014) Soft-tissue balancing in total knee arthroplasty: cruciate-retaining versus posterior-stabilised, and measured-resection versus gap technique. Int Orthop 38:531–537
Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kurosaka M, Kuroda R (2009) Soft tissue balance measurement in posterior-stabilized total knee arthroplasty with a navigation system. J Arthroplasty 24:358–364
Moro-oka TA, Shiraishi H, Iwamoto Y, Banks SA (2010) Modified gap-balancing technique in total knee arthroplasty: evaluation of the post-operative coronal laxity. Knee Surg Sports Traumatol Arthrosc 18:375–380
Mullaji AB, Shetty GM (2013) Surgical technique: computer-assisted sliding medial condylar osteotomy to achieve gap balance in varus knees during TKA. Clin Orthop Relat Res 471:1484–1491
Okamoto S, Okazaki K, Mitsuyasu H, Matsuda S, Mizu-uchi H, Hamai S, Tashiro Y, Iwamoto Y (2014) Extension gap needs more than 1-mm laxity after implantation to avoid post-operative flexion contracture in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3174–3180
Okazaki K, Miura H, Matsuda S, Takeuchi N, Mawatari T, Hashizume M, Iwamoto Y (2006) Asymmetry of mediolateral laxity of the normal knee. J Orthop Sci 11:264–266
Romero J, Stähelin T, Binkert C, Pfirrmann C, Hodler J, Kessler O (2007) The clinical consequences of flexion gap asymmetry in total knee arthroplasty. J Arthroplasty 22:235–240
Saeki K, Mihalko WM, Patel V, Conway J, Naito M, Thrum H, Vandenneuker H, Whiteside LA (2001) Stability after medial collateral ligament release in total knee arthroplasty. Clin Orthop Relat Res 392:184–189
Sekiya H, Takatoku K, Takada H, Sasanuma H, Sugimoto N (2009) Postoperative lateral ligamentous laxity diminishes with time after TKA in the varus knee. Clin Orthop Relat Res 467:1582–1586
Takeda M, Ishii Y, Noguchi H, Matsuda Y, Sato J (2012) Changes in varus–valgus laxity after total knee arthroplasty over time. Knee Surg Sports Traumatol Arthosc 20:1988–1993
Tokuhara Y, Kadoya Y, Kanekasu K, Kondo M, Kobayashi A, Takaoka K (2006) Evaluation of the flexion gap by axial radiography of the distal femur. J Bone Joint Surg 88-B:1327–1330
Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K (2004) The flexion gap in normal knees. An MRI study. J Bone Joint Surg 86-B:1133–1136
Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG (1994) Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res 299:31–43
Yagishita K, Muneta T, Yamamoto H, Shinomiya K (2001) The relationship between postoperative ligament balance and preoperative varus deformity in total knee arthroplasty. Bull Hosp Jt Dis 60:23–28
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoshihara, Y., Arai, Y., Nakagawa, S. et al. Assessing coronal laxity in extension and flexion at a minimum of 10 years after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24, 2512–2516 (2016). https://doi.org/10.1007/s00167-015-3601-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3601-0