Abstract
Purpose
Anteroposterior (AP) joint translation is an important indicator of good clinical outcome following total knee arthroplasty (TKA). This study evaluated the in vivo relationship between changes in the degree of voluntary soft tissue tension and flexion angle versus simultaneous AP translation after TKA.
Methods
A posterior cruciate ligament (PCL)-retaining meniscal-bearing design was investigated in 20 knees of 20 patients. AP translation was measured at 30° and 75° flexion with the KT-2000 arthrometer while patients were anesthetized and non-anesthetized.
Results
The mean translations at 30° and 75° were 10.5 and 10.4 mm, respectively, in non-anesthetized patients and 13.8 and 12.7 mm, respectively, in patients under anesthesia. AP translation showed a significant positive correlation with soft tissue tension (p < 0.001), but not with flexion angle (p = 0.366). No interaction was observed between soft tissue tension and the flexion angle in terms of AP translation (p = 0.431).
Conclusion
Surgeons should recognize that AP translation is greater in anesthetized patients than in non-anesthetized patients, regardless of the flexion angle, with no significant correlation between flexion angle and translation, regardless of the level of consciousness. Because conformity between the tibial insert and femoral component decreases with flexion, whereas the opposing effects of supporting structures, such as muscles, ligaments, and capsules, increases, proper soft tissue tension, particularly retention of a functional PCL, could have an important role in determining AP translation in the current prosthesis design.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
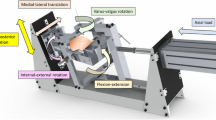
The low contact stress (LCS) posterior cruciate ligament (PCL)-retaining meniscal-bearing (MB) knee prosthesis (DePuy Orthopaedics, Warsaw, IN, USA) incorporates separate medial and lateral mobile polyethylene bearings, which slide independently in circularly arced keyways running anterior-to-posterior in the metal tibial component. This design allows unrestrained anteroposterior (AP) translation and axial rotation of the femur relative to the tibia, limited only by the periarticular tissues. In addition, the LCS femoral component has an anatomical articulating surface, and the radii of curvature decrease posteriorly. The femoral and tibial LCS components are fully conforming in the sagittal plane from full extension to 30° flexion and less conforming for greater flexion due to the decreasing radii of curvature of the posterior femoral condyles. One of the major goals of the mobile-bearing knee design is to promote load sharing through the relative translation of the tibial and femoral components [1]. Therefore, soft tissue involvement should generally be encouraged to decrease the dependence on intrinsic constraints afforded by the condylar geometry. Theoretically, soft tissue conditions play much more important roles in the mobile-bearing knee than in fixed-bearing prostheses [1]. Even in fixed-bearing prostheses, a common cause of early revision of total knee arthroplasty (TKA) was related to instability [2, 3]. Special care must be taken during the soft tissue part of the procedure to avoid early revision due to instability [2]. Moreover, Morberg et al. [4] reported the importance of a functional PCL in limiting excessive AP translation in AP-gliding rotating platform TKA.
Relationships between AP knee translation after TKA and clinical results have been examined in vitro [5], theoretically [6, 7], and in vivo [6–15]. Approximately 5–10 mm is the preferred value for TKA [6–15]; thus, understanding knee joint translations after TKA is of critical importance. However, most previous analyses have focused primarily on the effect of implant variability on the geometry [6, 7, 15, 16] or function [11, 13, 16, 17] of the PCL over time. Because patients perform more than one type of activity of daily living, the interplay of soft tissue function under different flexion angles and tensions is crucial in providing a better understanding of AP translation in mobile-bearing knee arthroplasty.
Thus, the current study was undertaken to measure the stability of the LCS meniscal-bearing total knee in anesthetized and non-anesthetized patients in terms of AP translation, as instability is a common reason for TKA revision [2, 3]. The study hypothesis was that AP translation would be smaller in non-anesthetized patients and larger with increasing flexion.
Materials and methods
After describing the study protocol and potential arthrometer-related complications, informed consent was obtained from all patients. We also received institutional review board approval. Twenty knees of 20 patients with bilateral osteoarthritic knees were analyzed. All patients were scheduled to undergo staged bilateral TKA and initially received LCS™ prostheses (PCL-retaining MB design; DePuy Orthopaedics) between July 1998 and January 2011. The design of this prosthesis allows unrestrained AP translation and axial rotation of the femur relative to the tibia. In this system, full contact occurs between the femoral component and tibial insert from 0° to 30°; the geometry of the prosthesis involves a progressive posterior reduction in the radius of curvature of the femoral condyle and a decrease in the conformity with flexion between the tibial and femoral components (Fig. 1) [18]. Thus, 30° is characterized by high conformity and 75° by low conformity between the femoral component and tibial insert (Fig. 2).
Articulating surface segments (from Pappas [18])
All initial TKA procedures were judged to be clinically successful (Hospital for Special Surgery scores >90) [19] with no clinical ligamentous instability or pain at the time of the second TKA. All surgeries were performed by an experienced surgeon (Y.I.) using a standardized technique, including the necessary soft tissue release for proper balance. Ligament-balancing techniques, including the necessary soft tissue release, were used and confirmed with spacer blocks to ensure a balanced knee with equal flexion and extension gaps. Proper intraoperative AP and coronal stability were confirmed manually, although not quantified intraoperatively. In all knees, the femoral components were fixed without cement, and the tibial components were fixed with cement. The indication for patients’ inclusion in this study was primary osteoarthritis. Contraindications included revision arthroplasty, previous tibial osteotomy, and rheumatoid arthritis. The clinical characteristics of the patients are summarized in Table 1 [20].
AP translation was measured using a KT-2000 arthrometer (MEDmetric, San Diego, CA, USA) following a standard protocol at 30° and 75° flexion, which was confirmed with a goniometer. An anterior force of 133 N and a posterior force of 89 N were applied to the initial TKA side while the patients were under anesthesia for the second TKA, and again after they had regained consciousness and were not anesthetized. The initial TKA side was measured under anesthesia during the second TKA surgery. The average interval between initial and final TKA measurements was 22 (range 5–104) months. We measured the initial side in non-anesthetized patients within the first week following the second surgery. Using the KT-2000 arthrometer, all patients were observed to relax their quadriceps. To minimize interobserver variation, an experienced physical therapist (T.S.) performed all tests. Three measurements were made and subjected to statistical analysis; intrasubjective errors were <1 mm.
Statistical analysis
All AP translation values are reported as means ± standard deviations. The effects of consciousness level and flexion angle on AP translation values were analyzed using a linear mixed-effects model for triplicate repeated measures, with consciousness level and flexion angle serving as fixed effects and subject as a random effect. The level of significance was set at p < 0.05. Statistical analyses were performed using the SPSS software (version 19; IBM Japan Inc., Tokyo, Japan).
Results
The mean AP translations at 30° and 75° were 10.5 ± 4.6 mm and 10.4 ± 4.5 mm, respectively, in non-anesthetized patients and 13.8 ± 5.4 mm and 12.7 ± 5.2 mm, respectively, in anesthetized patients (Table 2; Fig. 3). AP joint translation was significantly associated with consciousness level (p < 0.001), but not flexion angle (p = 0.366). No interaction was observed between soft tissue tension and the flexion angle in terms of AP translation (p = 0.431; Table 3).
Three measurements of mean total displacement (TD) in a 68-year-old female made while conscious (a 30° of knee flexion; b 75° of knee flexion) and while under anesthesia (c 30° of knee flexion; d 75° of knee flexion). a TD, 12.1 mm, b TD, 11.2 mm, c TD, 13.6 mm, d TD, 14.3 mm. X-axis: total displacement (mm), Y-axis: +, anterior force 133 N, −posterior force 89 N
Discussion
This study had two main findings. First, the range of AP translation was significantly larger in anesthetized than in non-anesthetized patients, regardless of flexion angle. Second, AP joint translation showed no positive correlation with flexion angle, regardless of voluntary soft tissue tension. Thus, the degree of conformity between components did not affect AP translation in the current prosthesis design.
Our study has four main limitations. First, the sample was relatively small. The study was performed in a group of 20 patients undergoing bilateral TKA using the KT-2000 arthrometer. The measurement methodology is well established and has been used in many previous studies to evaluate significant differences [9–11]. Second, the intervals between AP translation measurements ranged from 5 to 104 months, which may have affected the results. However, some studies [13, 16, 17] have reported no significant change in AP translation over a mid-term postoperative period in patients undergoing joint replacement with prostheses employing the PCL-retaining design with no clinical complaint. Third, AP translation was measured only in the absence of an axial load because of the characteristics of the arthrometer used. Assessments of translation under load-bearing conditions may provide a better understanding of the factors influencing clinical performance during activity. Fourth, because this study analyzed AP translation of the mobile-bearing inserts and the femoral component and inserts simultaneously, detection of each translation separately was difficult. The strengths of this study include the treatment of all patients by a single experienced surgeon using the same instrumentation. Furthermore, all participants were active, with no restriction in activities of daily living.
With regard to the effect of flexion angle on the muscle reaction around the knee joint, 15–20° was adopted in an attempt to minimize the influence of hamstring reactions during anterior translation [7, 21]. However, because most previous studies evaluated AP joint translation only in conscious patients [6–17], the effects of changes in voluntary soft tissue tension may not have been eliminated. The current study simultaneously evaluated the in vivo relationship between the degree of voluntary soft tissue tension and flexion angle after TKA versus AP translation and clarified the interaction between these two variables.
The effect of anesthesia tends to exclude the contributions of voluntary soft tissue tension on AP knee joint translation. In this study, in vivo AP joint translation was significantly associated with voluntary soft tissue tension (p < 0.001), regardless of flexion angle; the range of AP translation was significantly larger in anesthetized than in non-anesthetized patients, regardless of the difference in conformity between components in the current prosthesis design. If the translation values obtained while patients were under anesthesia can be regarded as almost equivalent to intraoperative values (i.e., exclusion of the contribution of voluntary soft tissue tension in structures such as muscles, ligaments, and capsules, although capsulorrhaphy was not performed), the results of this study indicate that intraoperative translation is greater than translation measured in non-anesthetized patients. Thus, surgeons should be aware that intraoperative AP translation is greater than the translation defined as optimal under non-anesthetized conditions, regardless of flexion angle, in the current prosthesis design.
Moreover, this study showed that AP joint translation was not significantly associated with flexion angle, regardless of the opposing effects of supporting structures, such as muscles, ligaments, and capsules. The geometry of the prosthesis involves a decrease in conformity between the tibial insert and femoral components with flexion, whereas muscular defense [21] and tension of the retaining PCL [22] increase with flexion. As a result, the muscular defense and PCL may accelerate AP translation, while the geometry may decelerate this translation, at 30° flexion; on the other hand, the converse may be true at 75° flexion. Therefore, the reverse roles of factors such as conformity and soft tissue tension at each angle may have no significant effect on AP translation. In addition, this situation may demonstrate the importance of well-functioning soft tissue conditions in the mobile-bearing knee [1].
Lower conformity, such as 75° flexion with soft tissue dysfunction including the PCL, might induce non-physiological AP translation in the current prosthesis design. In a radiographic analysis of this prosthesis design, Hartford et al. [23] found decreased range of motion and clinical scores in knees that did not reproduce normal rollback due to functional insufficiency of the PCL. Therefore, we should consistently define the proper AP translation values for the current PCL-retaining TKA design as approximately 10 mm while conscious and 13 mm while under anesthesia, although these values may not apply to cruciate-sacrificing or cruciate-substituting TKA designs. In addition, surgeons should pay careful attention to changes in the conformity of the femoral and tibial components with flexion, especially in current prostheses compared with those with a single-radius femoral component design.
In conclusion, voluntary soft tissue tension had a greater effect than flexion angle on AP translation in MB prostheses. Well-functioning soft tissues, including the PCL, might allow for the substitution of less conforming geometry with flexion to control AP translation. These findings could support the importance of soft tissue conditions with the current prosthesis design [1]. To fully understand function after knee replacement, clinical performance, and implant durability, the characterization of AP translation across the spectrum of voluntary soft tissue tensions and flexion angles that are important for patient functioning is crucial.
References
Callaghan JJ, Insall JN, Greenwald AS, Dennis DA, Komistek RD, Murray DW, Bourne RB, Rorabeck CH, Dorr LD (2000) Mobile-bearing knee replacement. Concepts and results. J Bone Joint Surg Am 82(7):1020–1041
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M (2001) Early failures in total knee arthroplasty. Clin Orthop Relat Res 392:315–318
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM (2002) Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
Morberg P, Chapman-Sheath P, Morris P, Cain S, Walsh WR (2002) The function of the posterior cruciate ligament in an anteroposterior-gliding rotating platform total knee arthroplasty. J Arthroplasty 17(4):484–489
Matsuda S, Whiteside LA, White SE, McCarthy DS (1999) Knee stability in meniscal bearing total knee arthroplasty. J Arthroplasty 14(1):82–90
Walker PS, Ambarek MS, Morris JR, Olanlokun TK, Cobb AG (1995) Anterior-posterior stability in partially conforming condylar knee replacement. Clin Orthop Relat Res 310:87–97
Warren PJ, Olanlokun TK, Cobb AG, Walker PS, Iverson BF (1994) Laxity and function in knee replacements. A comparative study of three prosthetic designs. Clin Orthop Relat Res 305:200–208
Dejour D, Deschamps G, Garotta L, Dejour H (1999) Laxity in posterior cruciate sparing and posterior stabilized total knee prostheses. Clin Orthop Relat Res 354:182–193
Ishii Y, Matsuda Y, Ishii R, Sakata S, Omori G (2005) Sagittal laxity in vivo after total knee arthroplasty. Arch Orthop Trauma Surg 125(4):249–253
Jones DPG, Locke C, Pennington J, Theis JC (2006) The effect of sagittal laxity on function after posterior cruciate-retaining total knee arthroplasty. J Arthroplasty 21(5):719–723
Matsuda S, Miura H, Nagamine R, Urabe K, Matsunobu T, Iwamoto Y (1999) Knee stability in posterior cruciate ligament retaining total knee arthroplasty. Clin Orthop Relat Res 366:169–173
Matsuda Y, Ishii Y (2004) In vivo laxity in low contact stress knee system. Clin Orthop Relat Res 419:138–143
Mizu-uchi H, Matsuda S, Miura H, Nabeyama R, Okazaki K, Iwamoto Y (2006) Anteroposterior stability in posterior cruciate ligament-retaining total knee arthroplasty. J Arthroplasty 21(4):592–598
White SH, O’Connor JJ, Goodfellow JW (1991) Sagittal plane laxity following knee arthroplasty. J Bone Joint Surg Br 73(2):268–270
Yamakado K, Kitaoka K, Yamada H, Hashiba K, Nakamura R, Tomita K (2003) Influence of stability on range of motion after cruciate-retaining TKA. Arch Orthop Trauma Surg 123(1):1–4
Schuster AJ, von Roll AL, Pfluger D, Wyss T (2011) Anteroposterior stability after posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19(7):1113–1120
Chouteau J, Lerat JL, Testa R, Moyen B, Banks SA (2009) Sagittal laxity after posterior cruciate ligament-retaining mobile-bearing total knee arthroplasty. J Arthroplasty 24(5):710–715
Pappas MJ (2002) Engineering design of the LCS replacement. In: Hamelynck KJ, Stiehl JB (eds) LCS mobile-bearing knee arthroplasty. 25 years of worldwide experience. Springer, Berlin, pp 39–52
Alicea J (2001) Scoring systems and their validation for the arthritic knee. In: Insall JN, Scott WN (eds) Surgery of the knee, vol 2. Churchill Livingstone, New York, pp 1507–1515
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Iversen BF, Sturup J, Jacobsen K, Andersen J (1989) Implications of muscular defense in testing for the anterior drawer sign in the knee: a stress radiographic investigation. Am J Sports Med 17(3):409–413
Girgis FG, Marshall JL, Al Monejem ARS (1975) The cruciate of the knee joint: anatomical, function and experimental analysis. Clin Orthop Relat Res 106:216–231
Hartford JM, Banit D, Hall K, Kaufer H (2001) Radiographic analysis of low contact stress meniscal bearing total knee replacement. J Bone Joint Surg Am 83(2):229–234
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, and patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
Ethical standard
The local institutional review board approved this study. All patients provided informed consent.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ishii, Y., Noguchi, H., Takeda, M. et al. In vivo anteroposterior translation after meniscal-bearing total knee arthroplasty: effects of soft tissue conditions and flexion angle. Eur J Orthop Surg Traumatol 24, 967–971 (2014). https://doi.org/10.1007/s00590-013-1271-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-013-1271-5