Abstract
Purpose
Although continuous improvements have been made, there is still a considerable amount of unsatisfied patients after total knee arthroplasty (TKA). A main reason for this high percentage is anterior knee pain, which is supposed to be provoked by post-operative increased retropatellar peak pressure. Since rotational malalignment of the implant is believed to contribute to post-operative pain, the aim of this study was to examine the influence of tibial component rotation on knee kinematics and retropatellar pressure.
Methods
Eight fresh-frozen knee specimens were tested in a weight-bearing knee rig after fixed-bearing TKA under a loaded squat from 20° to 120° of flexion. To examine tibial components with different rotations, special inlays with 3° internal rotation and 3° external rotation were produced and retropatellar pressure distribution was measured with a pressure-sensitive film. The kinematics of the patella and the femorotibial joint were recorded with an ultrasonic-based motion analysis system.
Results
Retropatellar peak pressure decreased significantly from 3° internal rotation to neutral position and 3° external rotation of the tibial component (8.5 ± 2.3 vs. 8.2 ± 2.4 vs. 7.8 ± 2.5 MPa). Regarding knee kinematics femorotibial rotation and anterior–posterior translation, patella rotation and tilt were altered significantly, but relative changes remained minimal.
Conclusion
Changing tibial rotation revealed a high in vitro influence on retropatellar peak pressure. We recommend the rotational alignment of the tibial component to the medial third of the tibial tuberosity or even more externally beyond that point to avoid anterior knee pain after TKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since decades, total knee arthroplasty (TKA) is the surgical therapy of choice for advanced-stage knee osteoarthritis [2, 6]. Although continuous improvements concerning surgical technique, implant design and materials have been made, there are still up to 18 % of unsatisfied patients after TKA [11, 28, 41]. Besides the patient expectations, the extent of information given to the patient, preoperative functional status and extra-articular causes, there are also several surgical factors of influence for the outcome of TKA [1, 29]. In addition to instability, polyethylene (PE) wear and aseptic loosening, anterior knee pain is the main surgical reason for post-operative pain [38, 40]. The incidence of peripatellar complications after TKA is up to 12 % [7]. Post-operative increase in the retropatellar pressure is supposed to provoke post-operative patella problems [12, 20, 37].
PE wear, loosening and instability are influenced by altered knee kinematics after TKA [24, 42]. Rotational malalignment of the implant is suspected to contribute to post-operative pain, excessive PE wear, loosening, instability and patellar maltracking as well as increased retropatellar pressure [9, 18, 22, 35]; especially, internal rotational error of the tibial component often comes along with especially anterior pain after TKA [27].
In vitro studies with cadaver knee specimens are a well-known method to analyse altered knee kinematics after TKA and implications on retropatellar pressure distribution [4, 10, 16, 39, 42]. There are studies confirming the positive effects of external rotation of the femoral component in terms of reducing retropatellar peak pressure and reproducing more natural kinematics of the patella [25, 36], but there is not much literature concerning the influence of tibial rotation on the kinematics of the patella [3, 26].
In terms of the rotation of the tibial component, it is believed that the best position may be achieved orientating the rotation to the medial border or the medial third of the tibial tuberosity [19, 23]. Even though there are several clinical studies suggesting a better outcome with the tibial component placed at medial part of the tibial tuberosity or even rotated externally beyond that point, there is a lack of cadaver studies examining the exact influence of the tibial component rotation on retropatellar pressure and kinematics in TKA. Therefore, the aim of this study was to evaluate the influence of tibial component rotation on retropatellar pressure and kinematics of the TKA using cadaver specimens mounted on a special knee rig. Tibial component rotation was simulated with a particular technique with specially produced inlays by the manufacturer to allow analysing even small amounts of component rotation in between the same specimen. Since increased retropatellar pressure is supposed to provoke anterior knee pain, the results of this study can give guidance of tibial component alignment intraoperatively.
Materials and methods
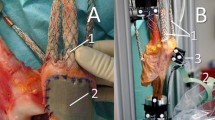
Eight fresh-frozen human knee specimens [age 58.9 ± 11.7 years (range 47–82); 3 female, 5 male; height: 176.9 ± 5.9 cm; weight: 81.5 ± 10.6 kg] were used for the experiments. Knees with serious valgus or varus deformity (≥10°) were excluded. The specimens were resected 20 cm proximal and 15 cm distal to the joint line. The soft tissue surrounding the knee joint (including capsule, ligaments and tendons) was preserved. Afterwards, the fibula head was fixed to the proximal tibia using a 4.5-mm screw, and metallic finger traps (Bühler-Instrumente Medizintechnik GmbH, Tuttlingen, Germany, Fig. 1) were connected to the tendons and fixation augmented using suture material (FibreWire, Arthrex, Munich, Germany) [35]. At the end, the tibia and the femur were embedded into metallic pots with epoxy casting resin (Rencast FC53, Huntsman, Basel, Switzerland).
For the evaluation of the degree of osteoarthritis and to exclude knees with serious deformities, X-rays in anterior–posterior, sagittal and sunrise view were taken before implantation. The same X-rays were taken after TKA to ensure the correct implantation of the prostheses.
Implantation
For this in vitro study, a fixed-bearing, cruciate-retaining TKA (Columbus CR Aesculap, Tuttlingen, Germany) was chosen. Columbus knee system is a knee system which is on the market since 2003 with approximately 185,000 implantations and currently still used for total knee replacement [14]. The femoral component is a multi-radius design with a relatively small dorsal femoral radius. The short posterior condyles enable high flexion up to 140°. The trochlea of the femoral component has a valgus direction of 7°, with an elevated antero-lateral femoral design to prevent patella luxation. The implantation was performed by the first author A.S. under supervision of the senior author A.F. using a subvastus approach to the knee and a tibia first technique for ligament balancing. According to the study of Lützner et al. [23], all tibial components were aligned to the medial third of the tibial tuberosity. In advance, the tibial tuberosity was divided into three parts, and the borders were marked with a surgical pen.
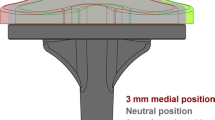
To achieve different rotations of the tibial component, different inlays using the CAD-data of the prosthesis and CAD-Software (Catia V5 R19, Dassault Systems, France) were constructed. Additional to the regular inlay (defined as neutral position), two variations with 3° of internal and external rotation were produced out of PE by the manufacturer (Fig. 2). This way, the articular surface of the inlays remained unchanged. With these variations, it was possible to examine the influence of different tibial rotations by only changing the inlays.
Biomechanical test setup
For the measurement of the retropatellar pressure distribution, the patella remained unresurfaced; only existing osteophytes on the circumference were removed. A pressure-sensitive film (K-Scan 4000, Tekscan Inc., Boston, USA) was sutured to the retropatellar surface using subcutaneous 1.0 suture material. To stabilise the attachment and to avoid shear forces, a 0.125-mm Teflon tape (PTFE-tape) was glued on the sensor before suturing. The sensor film has a total number of 572 sensels (62 sensels per cm2) with a maximum pressure of 1,500 PSI (~10 MPa). For calibration of the sensor, a two-point load, as recommended by the manufacturer, was applied using a material testing machine (Z010, Zwick, Ulm, Germany). The patella ridge was landmarked on the sensor film for orientation and the following pressure distribution analysis.
The specimens were mounted on a 6° of freedom (DOF) knee rig [35, 36]. For the measurements, a loaded squat from 20° to 120° of flexion and back to 20° of extension was induced with a constant velocity of 3°/s by a linear drive (Driveset M150, Systec GmbH, Muenster, Germany). The position of the knee and the axial femorotibial rotation was measured by two angle sensors (8820 Burster, Gernsbach, Germany) in the upper “hip assembly” and the lower “ankle assembly”. The quadriceps muscle force was simulated by another linear drive (Driveset M180, Systec GmbH, Muenster, Germany) and measured by a force sensor (8417-6002 Burster, Gernsbach, Germany) installed near the tendon. We restored the quadriceps muscle vectors anatomically: the rectus muscle was orientated to the femur shaft, vastus lateralis to the greater, vastus medialis to the lesser trochanter. Further muscles (medial vastus, lateral vastus, semitendinosus and biceps femoris muscle) were simulated using for each a 2-kg weight. In this constellation, the ground reaction force was measured under the “ankle assembly” by a six DOF force moment sensor (FN 7325-31 FGP Sensors, Cedex, France).
The two linear drives were controlled by a self-programmed LabVIEW code (Version 8.6, National Instruments, Austin, Texas, USA) on a personal computer using Real-Time and PID-Control Packages to achieve a constant ground reaction force of 50 N.
For recording of knee kinematics, an ultrasonic-based 3-dimensional motion analysis system (Zebris CMS 20, Isny, Germany) was used. Three miniature transmitters each were attached to the femur, the patella and the tibia (Fig. 1), providing the determination of the rotation and translation of the femur, the patella and the tibia with an accuracy of 0.1° and 0.1 mm. For the kinematics of the patella, the definitions of Bull et al. [8] (flexion, rotation, tilt and shift) were used (Fig. 3). Sufficient measurement reliability for kinematics and retropatellar pressure was assured by test–retest analysis; accuracy of the measurement system has been described in a former study [35]. This study was approved by the ethical committee of University of Munich (LMU).
Statistical analysis
Results for absolute values were presented in mean ± standard deviation. To compare different tibial rotations, the measured parameters were modelled using mixed-effect model with random intercept per knee specimen. Fixed effects were included in the model by the cosine of the flexion angle (FA in radian), the squared cosine of the FA, the cubed cosine of the FA, the different tibial rotations (external/neutral/internal) as well as flexion/extension of the knee. For this model, the results were displayed as regression coefficient with 95 % confidence interval. Analyses were performed using SPSS software (SPSS release 21.0, IBM, New York, USA). p < 0.05 was considered statistically significant.
Results
According to mixed-effect model, alteration of the rotation of the tibial component had a significant influence on the mean retropatellar peak pressure after TKA (Table 1). In neutral position, the retropatellar peak pressure was 8.2 ± 2.4 MPa. 3° of internal tibial rotation led to a clear increase in retropatellar peak pressure (8.5 ± 2.3 MPa), while 3° external rotation revealed a pronounced decrease in pressure (7.8 ± 2.5 MPa) (p < 0.01). Regarding the pressure distribution, the peak pressure was located at the medial part of the patella ridge (Fig. 4). The highest peak pressure differences were measured in high flexion angles (>80°). Quadriceps muscle force and ground reaction force did not alter significantly (Table 1).
Regarding the influence on the kinematic of the patella, there was a significant difference in patella rotation [rotation at 120° of flexion: neutral (3.1° ± 7.2°), internal (3.3° ± 7.2°), external (3.0° ± 7.2°) (p = 0.04) and patella tilt; tilt at 120° of flexion: neutral (4.1° ± 8.3°); internal (4.0° ± 8.3°); external (4.3° ± 8.4°) (p = 0.02)]. The changes in patella flexion and patella shift were not significant (Table 1).
Different rotations of the tibial component not only had an influence on the patella, there was also a significant alteration on the kinematics of the femorotibial joint (Table 1). 3° internal rotation of the tibial component led to a higher posterior translation of the femur. The opposite effect was seen using the inlay with 3° external rotation. Posterior translation of the femur at 120° of flexion was in neutral rotation −5.0 ± 3.9 mm, in internal rotation −5.6 ± 5.1 mm, in external rotation −4.9 ± 4.6 mm (p < 0.01).
Discussion
The most important finding of the present study was a significant influence of the rotation of the tibial component on retropatellar peak pressure. Looking at the pressure distribution, especially the peak pressure, on the medial part of the patella ridge was reduced by external rotation of the tibial component. This in vitro tendency might support clinical studies revealing less anterior knee pain after TKA with external rotation of the tibial component [23, 27]. Even though the mixed-effect model revealed a significant difference with alteration of only 3°, there is no threshold for the amount of reduction of retropatellar peak pressure and an effect on clinical symptoms like anterior knee pain. There are no standard guidelines for the rotational placement of the tibia component in TKA [19, 23, 32], and in clinical situations, malrotations of the tibial component are often much higher [13, 23]. Even if there would be a uniform ideal rotational position, it is hardly possible to place the tibial component within a range of 3° with conventional or patient-specific instrumentation or even computer-assisted surgery [15, 30, 33].
Even though there were significant differences regarding the regression coefficients of patella tilt and patella rotation between internal and external rotation of the tibial component, the influence on patella kinematics was rather marginal. The relatively small alteration of the patella rotation and patella tilt might not have a clinical impact. The alterations of the patella flexion and patella shift were even smaller and not significant.
A comparison with former in vitro studies examining the influence of tibial component rotation on patella kinematics is difficult due to different experimental set-ups [3, 26]. But in both referenced studies, the alteration of patella tilt, shift and rotation were also only marginal. Regarding external rotation of the tibial component, Anglin et al. [3] also found the tendency of a more lateral patella tilt in knee flexion compared with the position in extension.
The influence of the rotation of the tibial component on the kinematics of the femorotibial joint was also rather small. With internal rotation of the tibia, there was slightly more posterior translation of the femur, but a clinical impact of this difference is rather unlikely. The same applies for the femorotibial rotation. The difference of the mean values between 3° internal and 3° external rotation of the tibial component was statistically significant. Probably due to the low constraining force between the femur and tibial component in the used CR prosthesis, a rotation of the tibial component did not lead to a highly altered femorotibial rotation.
Comparing former in vitro studies with this experimental setup is complex, because different specimens with anatomical variability of the patella were used [35, 36]. But there seems to be a higher influence of the tibial rotation compared with the femoral rotation concerning retropatellar peak pressure. In a former study of Steinbrück et al. [36], the alteration of the femoral compartment of 3° internal rotation produced an increase in maximum retropatellar peak pressure of 0.01 MPa, and using the variant with 3° external rotation caused a decrease of 0.1 MPa compared with the neutral rotation. Compared with these data, 3° internal rotation of the tibial component led to a higher increase in the maximum retropatellar peak pressure by 0.2 MPa, as well as 3° external rotation revealed a higher decrease by 0.5 MPa. In the range of ±3° of rotation alteration, the influence on the maximum retropatellar peak pressure was five times higher for the tibial component compared with the femoral component (0.7 vs. 0.1 MPa). Only further external rotation of the femoral component by 6° caused a distinct decrease in mean retropatellar peak pressure of 1.1 MPa.
This study has a number of limitations to be considered. One limitation lies within the variety of the tibial tuberosity [17]. Especially in knees with varus deformity, the tibial tuberosity is not a reliable rotational landmark for the tibia component [5, 31]. On the other hand, Lawrie et al. [21] are certifying a good reliability of the tibial tuberosity on the flexion–extension axis. In our study, we used the tibial tuberosity for orientation since it is the main rotational landmark in clinical practice of TKA [23]. To reduce the amount of variety, specimens with serious valgus or varus deformity (≥10°) were excluded.
A challenge of all in vitro studies using cadaver specimens is the limited acquisition of samples. We tested all modifications of implantation in between one specimen, and due to paired observations, statistical significance is supported, although a higher number of specimens might have supported our results substantially. Due to technical reasons, it was only possible to produce altered inlays with 3° of internal or external rotation. In clinical situations, malrotations of the tibial component are often much higher [13, 23]. Another limitation with in a knee rig study lies within the constriction of simulation to a loaded squat. Many activities of daily living like walking, climbing stairs or rising from a chair cannot be simulated with this rig. But parts of the results may be transferred to in vivo activities.
Finally, these achieved results only apply for TKA with fixed-bearing inlays. The results cannot be transferred to TKA with mobile bearing inlays or rotation platform, because these inlays adjust independently to the rotation of the tibial component.
The results of our study highlight the importance of tibial component alignment especially in knee arthroplasty with fixed bearing. In patients with unexplained knee pain after TKA, a vast internal tibial malrotation should be radiologically excluded [27, 34].
Conclusion
A significant reduction of retropatellar pressure by rotating the tibial component externally could be confirmed by this in vitro study, while knee kinematics remained almost unchanged. Wide internal rotation of the tibial component should be avoided intraoperatively and might cause anterior knee pain according to clinical studies.
References
Ali A, Sundberg M, Robertsson O, Dahlberg LE, Thorstensson CA, Redlund-Johnell I, Kristiansson I, Lindstrand A (2014) Dissatisfied patients after total knee arthroplasty: a registry study involving 114 patients with 8–13 years of followup. Acta Orthop 85(3):229–233
Anderson JG, Wixson RL, Tsai D, Stulberg SD, Chang RW (1996) Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty 11(7):831–840
Anglin C, Brimacombe JM, Hodgson AJ, Masri BA, Greidanus NV, Tonetti J, Wilson DR (2008) Determinants of patellar tracking in total knee arthroplasty. Clin Biomech (Bristol, Avon) 23(7):900–910
Arnout N, Vanlommel L, Vanlommel J, Luyckx JP, Labey L, Innocenti B, Victor J, Bellemans J (2014) Post-cam mechanics and tibiofemoral kinematics: a dynamic in vitro analysis of eight posterior-stabilized total knee designs. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3167-2
Bonnin MP, Saffarini M, Mercier PE, Laurent JR, Carrillon Y (2011) Is the anterior tibial tuberosity a reliable rotational landmark for the tibial component in total knee arthroplasty? J Arthroplasty 26(2):260–267 e1–e2
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63
Boyd AD Jr, Ewald FC, Thomas WH, Poss R, Sledge CB (1993) Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am 75(5):674–681
Bull AM, Katchburian MV, Shih YF, Amis AA (2002) Standardisation of the description of patellofemoral motion and comparison between different techniques. Knee Surg Sports Traumatol Arthrosc 10(3):184–193
Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A (2004) A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 428:180–189
Didden K, Luyckx T, Bellemans J, Labey L, Innocenti B, Vandenneucker H (2010) Anteroposterior positioning of the tibial component and its effect on the mechanics of patellofemoral contact. J Bone Joint Surg Br 92(10):1466–1470
Dunbar MJ, Robertsson O, Ryd L, Lidgren L (2001) Appropriate questionnaires for knee arthroplasty: results of a survey of 3600 patients from The Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br 83(3):339–344
Fuchs S, Skwara A, Tibesku CO, Rosenbaum D (2005) Retropatellar contact characteristics before and after total knee arthroplasty. Knee 12(1):9–12
Harman MK, Banks SA, Kirschner S, Lutzner J (2012) Prosthesis alignment affects axial rotation motion after total knee replacement: a prospective in vivo study combining computed tomography and fluoroscopic evaluations. BMC Musculoskelet Disord 13:206
Hauschild O, Muenzberg M, Knothe D, Konstantinidis L, Helwig P, Sudkamp NP, Thielemann FW (2013) Rotational limb alignment changes following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21(10):2346–2354
Hernandez-Vaquero D, Noriega-Fernandez A, Fernandez-Carreira JM, Fernandez-Simon JM, Llorens de Los Rios J (2014) Computer-assisted surgery improves rotational positioning of the femoral component but not the tibial component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(12):3127–3134
Heyse TJ, Becher C, Kron N, Ostermeier S, Hurschler C, Schofer MD, Tibesku CO, Fuchs-Winkelmann S (2010) Patellofemoral pressure after TKA in vitro: highly conforming vs. posterior stabilized inlays. Arch Orthop Trauma Surg 130(2):191–196
Howell SM, Chen J, Hull ML (2013) Variability of the location of the tibial tubercle affects the rotational alignment of the tibial component in kinematically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21(10):2288–2295
Howell SM, Hodapp EE, Vernace JV, Hull ML, Meade TD (2013) Are undesirable contact kinematics minimized after kinematically aligned total knee arthroplasty? An intersurgeon analysis of consecutive patients. Knee Surg Sports Traumatol Arthrosc 21(10):2281–2287
Kim YH, Park JW, Kim JS, Park SD (2014) The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop 38(2):379–385
Kulkarni SK, Freeman MA, Poal-Manresa JC, Asencio JI, Rodriguez JJ (2000) The patellofemoral joint in total knee arthroplasty: Is the design of the trochlea the critical factor? J Arthroplasty 15(4):424–429
Lawrie CM, Noble PC, Ismaily SK, Stal D, Incavo SJ (2011) The flexion–extension axis of the knee and its relationship to the rotational orientation of the tibial plateau. J Arthroplasty 26(6 Suppl):53–58 e1
Lutzner J, Kirschner S, Gunther KP, Harman MK (2012) Patients with no functional improvement after total knee arthroplasty show different kinematics. Int Orthop 36(9):1841–1847
Lutzner J, Krummenauer F, Gunther KP, Kirschner S (2010) Rotational alignment of the tibial component in total knee arthroplasty is better at the medial third of tibial tuberosity than at the medial border. BMC Musculoskelet Disord 11:57
Matsuzaki T, Matsumoto T, Kubo S, Muratsu H, Matsushita T, Kawakami Y, Ishida K, Oka S, Kuroda R, Kurosaka M (2014) Tibial internal rotation is affected by lateral laxity in cruciate-retaining total knee arthroplasty: an intraoperative kinematic study using a navigation system and offset-type tensor. Knee Surg Sports Traumatol Arthrosc 22(3):615–620
Merican AM, Ghosh KM, Iranpour F, Deehan DJ, Amis AA (2011) The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19(9):1479–1487
Nagamine R, Whiteside LA, White SE, McCarthy DS (1994) Patellar tracking after total knee arthroplasty: the effect of tibial tray malrotation and articular surface configuration. Clin Orthop Relat Res 304:262–271
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 92(9):1238–1244
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Noble PC, Fuller-Lafreniere S, Meftah M, Dwyer MK (2013) Challenges in outcome measurement: discrepancies between patient and provider definitions of success. Clin Orthop Relat Res 471(11):3437–3445
Parratte S, Blanc G, Boussemart T, Ollivier M, Le Corroller T, Argenson JN (2013) Rotation in total knee arthroplasty: no difference between patient-specific and conventional instrumentation. Knee Surg Sports Traumatol Arthrosc 21(10):2213–2219
Sahin N, Atici T, Ozturk A, Ozkaya G, Ozkan Y, Avcu B (2012) Accuracy of anatomical references used for rotational alignment of tibial component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(3):565–570
Scott RD (2013) Femoral and tibial component rotation in total knee arthroplasty: methods and consequences. Bone Joint J 95-B(11 Suppl A):140–143
Silva A, Sampaio R, Pinto E (2014) Patient-specific instrumentation improves tibial component rotation in TKA. Knee Surg Sports Traumatol Arthrosc 22(3):636–642
Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ (2005) The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am 87(10):2276–2280
Steinbruck A, Schroder C, Woiczinski M, Fottner A, Muller PE, Jansson V (2013) Patellofemoral contact patterns before and after total knee arthroplasty: an in vitro measurement. Biomed Eng Online 12:58
Steinbruck A, Schroder C, Woiczinski M, Fottner A, Muller PE, Jansson V (2014) The effect of trochlea tilting on patellofemoral contact patterns after total knee arthroplasty: an in vitro study. Arch Orthop Trauma Surg 134(6):867–872
Stukenborg-Colsman C, Ostermeier S, Burmester O, Wirth CJ (2003) Dynamic in vitro measurement of retropatellar pressure after knee arthroplasty. Orthopade 32(4):319–322
van Kempen RW, Schimmel JJ, van Hellemondt GG, Vandenneucker H, Wymenga AB (2013) Reason for revision TKA predicts clinical outcome: prospective evaluation of 150 consecutive patients with 2-years followup. Clin Orthop Relat Res 471(7):2296–2302
Vandenneucker H, Labey L, Victor J, Vander Sloten J, Desloovere K, Bellemans J (2014) Patellofemoral arthroplasty influences tibiofemoral kinematics: the effect of patellar thickness. Knee Surg Sports Traumatol Arthrosc 22(10):2560–2568
Vince KG (2003) Why knees fail. J Arthroplasty 18(3 Suppl 1):39–44
Wylde V, Learmonth I, Potter A, Bettinson K, Lingard E (2008) Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br 90(9):1172–1179
Zihlmann MS, Stacoff A, Romero J, Quervain IK, Stussi E (2005) Biomechanical background and clinical observations of rotational malalignment in TKA: literature review and consequences. Clin Biomech (Bristol, Avon) 20(7):661–668
Acknowledgements
The authors thank the Dr. Auguste Schaedel-Dantscher Foundation for their financial support of this study. We thank Aesculap AG especially PD Dr. Dr. Thomas Grupp for providing CAD-Files of the TKA. Sincere thanks are given to Moritz von Holst for his help in translating our text into English and to Dr. Alexander Crispin (Institute of Biometry and Epidemiology, LMU Munich) for his statistical council.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Steinbrück, A., Schröder, C., Woiczinski, M. et al. Influence of tibial rotation in total knee arthroplasty on knee kinematics and retropatellar pressure: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24, 2395–2401 (2016). https://doi.org/10.1007/s00167-015-3503-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3503-1