Abstract
Introduction
Patellofemoral complications are one major concern after total knee arthroplasty (TKA). Anterior knee pain is one of these complications and to a high percentage responsible for unsatisfied patients after TKA. Malrotation of the femoral component can contribute to retropatellar peak pressure and consequently to anterior knee pain.
Materials and methods
Eight fresh frozen cadavers were tested in a force-controlled knee rig after TKA during isokinetic flexing of the knee from 20° to 120° under constant load. By tilting the trochlea in the material of the created femoral component replicas, a rotation of the femoral component by 3° internal, 0° (neutral), 3° and 6° external rotation to transepicondylar line was simulated without changing flexion or extension gap. Retropatellar pressure distribution was measured during flexion and extension of the knee while quadriceps muscles and hamstring forces were applied.
Results
Maximum peak pressure for internal rotation of the trochlea was 7.32 ± 2.31 MPa, in neutral position the pressure reduced slightly to 7.31 ± 2.12 MPa and during further external rotation of trochlea rotation a decrease from 3° with 7.18 ± 2.14 MPa to 6° with 6.22 ± 1.83 MPa was observed (p < 0.01). There was a tendency of lower quadriceps force with increasing external rotation of the trochlea (p = 0.08).
Conclusions
The implantation of the femoral component by 3° internal trochlea rotation to transepicondylar line resulted in a highly significant increase of the mean maximal retropatellar pressure compared to 6° external rotation of the trochlea of the femoral component (p < 0.01). A higher retropatellar pressure might lead to anterior knee pain after TKA. We recommend an external rotation of the femoral component between 3° and 6° to anatomical transepicondylar line to reduce the maximal retropatellar pressure, but only if adequate soft tissue balancing and stable knee kinematics are provided.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is an effective solution for osteoarthritis of the knee, although up to 19 % of primary TKA patients are unsatisfied postoperatively [1]. 12 % of peripatellar complications after TKA without retropatellar resurfacing is described [2]; however, revision rates and postoperative outcome are similar compared to resurfaced patella [3, 4]. Anterior knee pain is one of the major concerns after TKA; patients are suffering by peripatellar, burning pain with higher flexion grades, walking stairs and raising from a chair [5].
Excessive postoperative retropatellar pressure is supposed to provoke postoperative patella problems [6–9]. In vitro studies with human specimens are a successful method to investigate retropatellar pressure distribution [8, 10], and were also used for this study.
The trochlea of the femoral component is mainly involved in terms of patella tracking and patella pressure after TKA [11, 12] and external femoral component rotation can reproduce natural kinematics of the patella and reduce retropatellar pressure [13, 10, 14]. Clinical analysis also showed that internal rotation of the femoral component is correlated with anterior knee pain [15–17]. However, Miller et al. [18] showed in their study the best results regarding patella tracking and forces in neutral position of the femoral component to transepicondylar axis (TEA).
Hence, there is no standard recommendation of the amount of rotation of the femoral component in TKA to reduce retropatellar pressure during movement of the knee. We, therefore, evaluated retropatellar pressure distribution with 3° internal, 0° (neutral), 3° and 6° external rotation of the trochlea of the femoral component by aligning it to the anatomical transepicondylar axis in a special knee rig under force-controlled muscle load in a range of motion of 20°–120°. In addition, a comparison of the rapid prototype replicas and the standard prostheses made of cobalt–chromium alloy were examined to verify differences between the both materials for this in vitro knee rig study.
Materials and methods
Prostheses
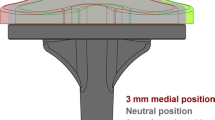
The study was performed with a posterior cruciate retraining prosthesis system with a fixed bearing UHMWPE-inlay (Aesculap, Tuttlingen, Germany, Columbus CR). Based on the CAD-data of the femoral components were modified on a personal computer by tilting the trochlea of the femoral component by 3° internal, 0° (neutral) and 3° and 6° external rotation (Catia V5R19; Dassault Systems; France). The condyles and all other geometries remained unmodified (Fig. 1). Afterwards the manufacturer used the CAD-models for producing the femoral components from size two to six with a professional 3D-printer (Object Eden 350, Rehovot Israel). Components were printed in thin layers of a liquid polymer, which immediately polymerized under UV-light. The prostheses were then polished under water with fine-grained abrasive paper up to a grain size of 1,000. The tibial components as well as PE inlays remained unchanged, the original materials were used.
Thus, it was possible to use the same bone cuts with different femoral components for an exclusive investigation of retropatellar pressure after TKA without influencing tibiofemoral compartments of the knee.
Specimens
Eight fresh frozen knee specimens (age range between 38 and 68 years, 3 female, 5 male, height: 176 ± 5 mm; weight: 75 ± 11 kg) were prepared preserving soft tissues surrounding the knee joint. Specimens with serious valgus or varus deformity (≥10°) were excluded from the study. The osteoarthritis was between 0° and 2° Kellgren and Lawrence Score [19]. Fibula head was fixed to tibia with a standard 4.5 diameter screw. Metallic finger traps were connected to the tendons (Bühler-Instrumente Medizintechnik GmbH, Tuttlingen, Germany), augmented with suture material (FibreWire, Arthrex, Munich, Germany). The femoral and tibial bones were embedded into a metallic pot both fixed with epoxy casting resin (Rencast FC53, Huntsman, Basel, Switzerland).
Shaping of the patella was performed by removing existing osteophytes on the patella circumference and the patella remained unresurfaced. As a next step, pressure-sensitive film (K-Scan 4000, Tekscan Inc., Boston, USA) was attached to the retropatellar surface by subcutaneous 1.0 suture material. For stable suturing and to avoid shear forces, a 0.1 mm Teflon tape was glued on the sensor before. The sensor was conditioned and calibrated with a two-point calibration using a material testing machine (Z010, Zwick, Ulm, Germany).
Biomechanical test setup
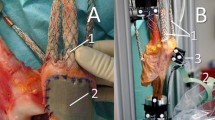
The prepared knee specimens were fixed on a six degree of freedom (DOF) knee rig which simulated a loaded squat from 20° to 120° of flexion and extension back to 20° with a velocity of 3°/s [20]. One linear drive (Driveset M150, Systec GmbH, Muenster, Germany) controlled the “hip-assembly” position related to the “ankle assembly” (Fig. 2). In both assemblies, angle sensors (8820 Burster, Gernsbach, Germany) were included to measure the flexion angle of the knee joint.
The simulation of the quadriceps muscle was performed by a second drive (Driveset M180, Systec GmbH, Muenster, Germany), while the actual quadriceps force was measured with a force sensor (8417-6002 Burster, Gernsbach, Germany) near to the tendon. In addition, lateral vastus and medial vastus muscle, as well as hamstrings (semitendinosus and biceps femoris muscle) were simulated with 2 kg weights. The ground reaction force was measured by a six DOF force moment sensor (FN 7325-31 FGP Sensors, Cedex, France) under the ankle assembly.
The flexion/extension drive and the quadriceps drive were controlled by a personal computer with the help of a self-programmed LabVIEW code (Version 8.6, National Instruments, Austin, Texas, USA) using Real-Time and PID-Control Packages, while a constant ground reaction force of 50 N was applied to the specimen.
Test procedure
We implanted TKA through a medial subvastus approach in tibia first technique. In coronal plane, the tibial resection was perpendicular to the bone axis in neutral rotation using an intramedullary rod. Soft tissue balancing was performed using a gauge instrument. An intramedullary rod aligned the femoral component with a 4°–6° valgus relative to the femoral axis. The femoral component was implanted in a neutral rotation. The neutral position was defined according to the anatomical transepicondylar axis of the femur. A K-wire was drilled through the anatomical transepicondylar axis and additionally, the Whiteside line was marked with an electronic cauter to identify femoral axis properly [21]. Afterwards, the femoral bone cuts were performed according to the defined neutral rotation of the femoral component and TKA was implanted.
A 10 mm polyethylene inlay was used in every TKA including 3° of posterior slope in the inlay design. All knees were operated by the author A.S., who is in his eighth post-graduate year and a specialist for orthopedic and trauma surgery. All knees were operated under assistance of author A.F., who is the senior attending surgeon of knee and hip arthroplasty in our department.
The evaluation after TKA was performed in 0° (neutral) rotation of the rapid prototyped femoral component. Afterwards, the femoral components with 3° internal and 3° and 6° external rotation of the trochlea were implanted and retropatellar pressure distribution was dynamically measured incrementally. The prostheses made of cobalt–chromium alloy were also tested to compare differences between the different materials in neutral position.
All specimens were x-rayed anterior–posterior, sagittal and sunrise view by fluoroscopy before implantation to evaluate the grade of osteoarthritis and patella alignment and after TKA to control the correct implantation of the prostheses.
Statistics
All results were presented in mean and standard deviation (SD). Mixed effects models were applied by utilizing random intercept per specimen to compare different trochlear rotations (SPSS 21; IBM). Flexion angle and trochlear rotation were assumed as fixed factors. Separate models were created for flexion (=0) and extension (=1). p < 0.05 represents statistical differences.
Results
Trochlear rotation had significant effect on the mean retropatellar peak pressure after TKA (p < 0.01). The regression coefficients showed a high retropatellar pressure at 3° internal rotation and on the other hand, a continuous reduction of retropatellar pressure from neutral to 6° external rotation (see Table 1). The highest peak pressure reduction was measured in high flexion angles. Therefore, the maximum peak pressure for internal rotation of the trochlea was 7.32 ± 2.31 MPa. In neutral position, the pressure reduced minimally to 7.31 ± 2.12 MPa and during further external rotation of the trochlea a decrease from 3° with 7.18 ± 2.14 MPa to 6° with 6.22 ± 1.83 MPa was observed (p < 0.01) (Fig. 3).
Figure 4 shows a retropatellar pressure distribution of a typical specimen with the four different trochlear rotations in a flexion angle of 110°. For the internal and neutral position the center of pressure occurred within the ridge of the patella. After external rotation of the trochlea the center of peak pressure drifted to the medial facet of the patella (see also Table 1).
After TKA, the tibial rotation altered between the specimens: three specimens showed an internal rotation between 1° and 7° with flexion, two knees rotated slightly externally between 0.3° and 1° and three specimens rotated very little between 0.15° internal and 0.15° external rotation. However, these tibial rotations remained unchanged by using the femoral components with different trochlear rotations (Table 1, row 3; p = 0.95).
There was a tendency of lower quadriceps force with increasing external rotation of the trochlea, but without statistical significance (p = 0.08). The controlled ground force also did not alter significantly (p = 0.33).
For the mentioned parameters, no statistical differences were found between the usage of rapid prototyped or standard prostheses made of cobalt–chromium (Fig. 5).
Discussion
Anterior knee pain after TKA is a relevant postoperative complication and is causing unsatisfied patients [22]. The trochlea of the femoral component is mainly involved in terms of patella tracking and patella pressure after TKA [11, 12]. Rhoads et al. [13] showed already 1993 in vitro that external femoral component rotation can reproduce natural kinematics of the patella. Anouchi et al. [14] underlined these findings in their study in the same year. Fuchs et al. [10] showed by static measurements in their rig study that external rotation can reduce retropatellar pressure. Berger et al. [15] showed in their clinical analysis that on the other hand internal rotation of the femoral component is correlated with anterior knee pain. Barrack et al. [16] underlined these results by their analysis of 102 knees. One of the latest studies concerning this issue showed that already a slight internal femoral component rotation to surgical TEA can lead to anterior knee pain after TKA [17]. However, Miller et al. [18] showed in their study the best results regarding patella tracking and forces in neutral position of the femoral component to transepicondylar axis. Hence, there is no gold standard in terms of the amount of rotation of the femoral component in TKA to reduce retropatellar pressure during movement of the knee. In the presented setting, we found a significant decrease of maximum retropatellar pressure ranging from 3° internal to 6° external rotation of the trochlea in a fixed bearing TKA system. As we simulated the rotation of the femoral component using the same bone cuts, we did not change the flexion and extension gap and soft tissue balancing was equal. Hence, retropatellar pressure distribution could be examined exclusively. On the other hand, by tilting the trochlea we did not analyze the effect on TKA kinematics by a real rotation of a femoral component, which would result in a changing flexion gap. However, a bigger lateral tibiofemoral compartment is one of the main causes to rotate the femoral component externally to provide soft tissue balancing and stable knee kinematics [10, 13]. We recommend an external rotation of the femoral component between 3° and 6° to anatomical transepicondylar line to reduce the maximal retropatellar pressure, but only if adequate soft tissue balancing and stable knee kinematics are provided.
The data suggest that rapid prototyping material may be used as an alternative to the standard prosthesis material for retropatellar pressure investigations with reduced weight bearing conditions as done in this trial. Due to our findings, however, rapid prototyped prostheses cannot be recommended for fatigue, biocompatibility, tribology and test with loads like in situ. Rapid prototyping with polymers is a cheap and simple solution with a high accuracy to get prototypes of knee prostheses for in vitro investigations.
A limitation of our study is that we tested only one particular TKA design. Consequentially, our results may not be transferred to all other implant designs. However, Columbus knee system is a product of one major manufacturer on the market and currently used for total knee replacement [23]. Our results may therefore be transferred to similar implant designs. Another limitation is that we also could not simulate daily activities like walking stairs and rising from a chair with our knee rig, but parts of our results of a loading squat might be transferrable to these activities.
Further studies must be conducted to analyze the influence of different modifications in implanting prostheses on patellofemoral contact patterns and knee kinematics.
References
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63
Boyd AD Jr, Ewald FC, Thomas WH, Poss R, Sledge CB (1993) Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am 75(5):674–681
Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L (2001) Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg Am 83-A(9):1376–1381
Robertsson O, Knutson K, Lewold S, Lidgren L (2001) The Swedish Knee Arthroplasty Register 1975-1997: an update with special emphasis on 41,223 knees operated on in 1988-1997. Acta Orthop Scand 72(5):503–513
Springorum HR, Rath B, Baier C, Lechler P, Luring C, Grifka J (2011) Patellofemoral pain after total knee arthroplasty: clinical pathway and review of the literature. Orthopade 40(10):907–911
Kulkarni SK, Freeman MA, Poal-Manresa JC, Asencio JI, Rodriguez JJ (2000) The patellofemoral joint in total knee arthroplasty: is the design of the trochlea the critical factor? J Arthroplasty 15(4):424–429
Hauf W, Mittlmeier T, Hagena FW, Plitz W (1992) Method for in vivo measurement of intraosseous pressure of the patella. Biomed Tech (Berl) 37(11):263–272
Stukenborg-Colsman C, Ostermeier S, Burmester O, Wirth CJ (2003) Dynamic in vitro measurement of retropatellar pressure after knee arthroplasty. Orthopade 32(4):319–322
Fuchs S, Skwara A, Tibesku CO, Rosenbaum D (2005) Retropatellar contact characteristics before and after total knee arthroplasty. Knee 12(1):9–12
Fuchs S, Schutte G, Witte H (1999) [Effect of knee joint flexion and femur rotation on retropatellar contact of the human knee joint]. Biomed Tech (Berl) 44(12):334–338
Ahmed AM, Duncan NA (2000) Correlation of patellar tracking pattern with trochlear and retropatellar surface topographies. J Biomech Eng 122(6):652–660
Barink M, Meijerink H, Verdonschot N, van Kampen A, de Waal Malefijt M (2007) Asymmetrical total knee arthroplasty does not improve patella tracking: a study without patella resurfacing. Knee Surg Sports Traumatol Arthrosc 15(2):184–191
Rhoads DD, Noble PC, Reuben JD, Tullos HS (1993) The effect of femoral component position on the kinematics of total knee arthroplasty. Clin Orthop Relat Res 286:122–129
Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT (1993) The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 287:170–177
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
Murakami AM, Hash TW, Hepinstall MS, Lyman S, Nestor BJ, Potter HG (2012) MRI evaluation of rotational alignment and synovitis in patients with pain after total knee replacement. J Bone Joint Surg Br 94(9):1209–1215
Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE (2001) Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res 392:38–45
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Steinbrück A, Schröder C, Woiczinski M, Fottner A, Müller PE, Jansson V (2013) Patellofemoral contact patterns before and after total knee arthroplasty: an in vitro measurement. Biomed Eng Online 12:58
Victor J (2009) Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res 95(5):365–372
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Hauschild O, Muenzberg M, Knothe D, Konstantinidis L, Helwig P, Sudkamp NP, Thielemann FW (2013) Rotational limb alignment changes following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21(10):2346–2354
Acknowledgments
The authors thank the Dr. Auguste Schaedel-Dantscher Foundation for their financial support of this study. The authors also thank the Aesculap Company for providing the prosthesis system, construction of the replicas of the femoral component and set of tools. We also thank Dr. Alexander Crispin (Institute for Biometry and Bioinformatics, LMU München) for his help in generating the statistical tests in this study. Additionally the authors thank Moritz von Holst for his technical help in preparing this paper.
conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Steinbrück, A., Schröder, C., Woiczinski, M. et al. The effect of trochlea tilting on patellofemoral contact patterns after total knee arthroplasty: an in vitro study. Arch Orthop Trauma Surg 134, 867–872 (2014). https://doi.org/10.1007/s00402-014-1956-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-1956-1