Abstract
Purpose
Increased retropatellar pressure and altered kinematics are associated with anterior knee pain and unsatisfied patients after total knee arthroplasty (TKA). Since malposition of the implant is believed to contribute to postoperative pain, we performed this in vitro study to evaluate the influence of mediolateral femoral component position on retropatellar pressure as well as tibio-femoral and patella kinematics.
Methods
For the test, a fixed-bearing TKA was implanted in eight fresh frozen cadaver specimens. To determine the impact of mediolateral (ML) position, three variants of femoral components (3-mm medialization, neutral position and 3-mm lateralization) were produced using rapid prototyping replicas. In a knee rig, a loaded squat from 20° to 120° of flexion was applied. Retropatellar pressure distribution was measured with a pressure-sensitive film. Additionally, an ultrasonic-based three-dimensional motion analysis system was used to register patello- and tibio-femoral kinematics.
Results
ML translation of the femoral component by 3 mm did not lead to a significant alteration in retropatellar peak pressure (medial 6.5 ± 2.5 MPa vs. lateral 6.0 ± 2.4 MPa). Following the ML translation of the femoral component, the patella was significantly shifted and tilted in the same directions. Varying the ML femoral component position also led to a significant alteration in femoral roll-back.
Conclusion
In day-by-day use, ML position should be chosen with care since there is a significant influence on patella shift and femoral roll-back. Retropatellar pressure is not significantly altered, so there is no clear evidence of an impact on anterior knee pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For decades, total knee arthroplasty (TKA) has been the procedure of choice for patients with progressive osteoarthritis [1, 5]. Although materials, implant design and surgical techniques were continuously improved, up to 18% of patients are unsatisfied after TKA [12, 27, 29, 41]. As a consequence, chronic pain is the cause of 9% of TKA revisions [30]. A substantial number of patients with pain after TKA report anterior knee pain. This isolated condition affects up to 12% of patients [6, 40] and is associated with increased postoperative retropatellar pressure [14, 21].
Several studies have proven that component position influences postoperative knee kinematics with possible impact on stability, increased PE wear, accompanied by aseptic loosening, as well as anterior knee pain [17, 18, 23, 24, 26, 35, 36, 42]. Therefore, adequate implant positioning is crucial in order to increase the percentage of satisfied patients. Unfavourable results in vitro as well as in clinical studies are especially caused by increased internal malrotation of the femoral as well as the tibial component [11, 24, 38, 42]. According to several in vitro studies, the reason is assumed to be patella maltracking and increased retropatellar pressure [2, 28, 35].
Femoral component size is mainly determined by anterior–posterior (AP) dimension, because this element is decisive for the flexion and extension gap and hereby for the joint line [4, 9, 15, 32]. Proper AP sizing though often leads to an oversized femoral component in mediolateral (ML) dimension resulting in ML overhang [10, 25]. Additionally, the recommended slight external rotation (3°) of femoral component causes a further increase in AP size [20].
In vitro studies addressing the impact of ML positioning of femoral component are very rare. Armstrong et al. [3] examined the influence of ML position on patello-femoral kinematics. In the given study, only patella shift was significantly altered by ML position. The impact of ML position on retropatellar pressure and tibio-femoral kinematics is still not clear. It can only be hypothesized that a medialization could lead to a relatively more lateral position of the patella on the trochlear of the femoral component associated with higher pressure on the lateral retropatellar facet [2, 31]. This could result in a higher incidence of anterior knee pain [14, 21]. To our knowledge, there are no in vitro studies which have investigated this matter. Therefore, the purpose of this study was to examine the in vitro influence of a medialized and lateralized femoral component on tibio-femoral and patella kinematics as well as retropatellar pressure after TKA using a knee rig.
Materials and methods
Specimens
Eight fresh frozen human knee specimens (age 58.9 ± 11.7 years; height 176.9 ± 5.9 cm; weight 81.5 ± 10.6 kg; 3 females, 5 males) were shortened 20 cm proximal and 15 cm distal to the joint line of the knee. Specimens with distinct bone deformity like valgus or varus deviations ≥10° were excluded. Surrounding soft tissue of the knee, like capsule, ligaments and tendons, was preserved. Metallic finger traps (Bühler-Instrumente Medizintechnik GmbH, Tuttlingen, Germany) were attached to the tendons with suture material (FibreWire, Arthrex, Munich, Germany) to simulate muscle forces. The fibula head was fixed to the proximal tibia using a 4.5-mm screw. After preparation, tibial and femoral bone ends were incorporated into metallic pots using epoxide resin (Rencast FC53, Huntsman, Basel, Switzerland).
To exclude specimens with severe bone deformities and to evaluate the extent of osteoarthritis radiographs in two plains with skyline view were taken before implantation. The same radiographs were performed postoperatively to ensure the correct positioning of implants.
Prostheses
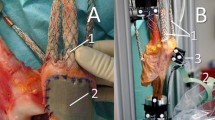
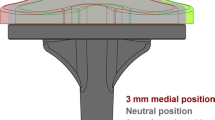
The in vitro tests were conducted with the cruciate retaining fixed-bearing knee system Columbus CR (Aesculap AG, Tuttlingen, Germany). The original tibial components as well as UHWMPE inlays were utilized. To evaluate the impact of ML femoral component position, the neutral implant and two modifications with 3-mm medialization and lateralization were produced for the most frequently used sizes 2–6 (Fig. 1). For the construction of 30 variations in total, the manufacturer provided the original CAD data. The medialized and lateralized modifications were constructed with the CAD software CATIA V5R19 (Dassault Systems, Vélizy-Villacoublay Cedex, France). For the three variations per size, the femoral cuts and the two femoral posts were maintained at the same place. Therefore, the trochlea and the condyles were medialized or lateralized relative to the posts.
Afterwards, these femoral models were produced using a professional 3D printer (Object Eden 350, Rehovot, Israel). Implants were printed in thin layers (down to approximately 50 µm) of a liquid photopolymer resin (Objet VeroBlue RGD840, consisting of several acrylate oligomers, acrylic monomer, isobornyl acrylate and a photoinitiator) polymerizing under UV light. The resulting components were polished under water with fine-grained sandpaper (up to grain size 1000). This method of photopolymerized rapid prototyping TKA replicas was already evaluated for in vitro testing by Schröder et al. [33].
Implantation
All implantations were performed by two experienced surgeons (A.S. and A.F.) in tibia first technique for ligament balancing using a subvastus approach. Tibial resection was perpendicular to the bone axis using an intramedullary rod. As defined as the best rotational position, all tibial components were oriented to the medial third of the tibial tuberosity [24]. For the rotational alignment of the femoral component, a K-wire was drilled through the medial and lateral epicondyle of the femur to define the anatomical transepicondylar axis. Additionally, the Whiteside line was marked with an electronic cauter [22]. Afterwards, the femoral bone cuts were performed parallel to the defined transepicondylar axis to achieve neutral rotation of the femoral component. The femoral component was positioned centrally on the femur with the same distance to the medial and lateral osseous border at the middle of the distal bone cut using a ruler. The TKA was implanted with a 10-mm polyethylene inlay in all cases.
Biomechanical test set-up
After removing peripatellar osteophytes, a pressure-sensitive film (K-Scan 4000, Tekscan Inc., Boston, USA) with a maximal pressure capacity of 1500 PSI (~10 MPa) and a resolution of 62 sensels per cm2 (totally 572 sensels) was attached to the retropatellar surface for measurement of retropatellar pressure distribution. To avoid shear forces, a 0.125-mm Teflon tape (PTFE tape) was glued onto the film. The sensor was fixed to the retropatellar surface with subcutaneous 1.0 suture material. After the tape was glued and before suturing, the sensor film was calibrated by applying a two-point load using a material testing machine (Z010, Zwick, Ulm, Germany).
Measurements were taken using a well-established knee rig with six degrees of freedom (DOF) [33, 34, 36,37,38] (Fig. 2). A loaded squat from 20° to 120° of flexion followed by extension back to 20° with a velocity of 3°/s was mediated by a linear drive (Driveset M150, Systec GmbH, Muenster, Germany). Constant angle velocity was ensured by controlling the linear velocity of the stepper respecting the first derivation of the cosine law. For the registration of flexion angle of the knee joint, two angle sensors (8820 Burster, Gernsbach, Germany) installed in the “hip unit” and the “ankle unit” were used. A further linear drive (Driveset M180, Systec GmbH, Muenster, Germany) was applied to build up flexion moment inducing the ground reaction force. The registration of actual quadriceps force was achieved with a force sensor (8417-6002 Burster, Gernsbach, Germany) installed near the tendon. Additionally, the tension of the medial vastus, lateral vastus, semitendinosus and biceps femoris muscle was simulated with 2 kg weights attached to each tendon. For registration of the generated ground reaction force, a six-DOF force moment sensor (FN 7325-31 FGP Sensors, Cedex, France) was mounted under the ankle unit. The linear drives for motion generation and for quadriceps force simulation were driven by a personal computer using a LabVIEW code (Version 8.6, National Instruments, Austin, Texas, USA) with Real-Time and PID-Control Packages to maintain a constant ground reaction force of 50 N.
Kinematics of the tibio-femoral and the patello-femoral joint were recorded using an ultrasonic-based three-dimensional motion analysis system (Zebris CMS 20, Isny, Germany). The measurement system persists of three miniature ultrasonic transmitters attached to the femur, the tibia and the patella. This way it was possible to register the relative rotation and translation of the three parts of the knee joint to each other. The definitions of Bull et al. [7] (flexion, rotation, tilt and shift) were applied to describe the relative motion of the patella.
The study was approved by the ethical committee of the University of Munich (LMU), Germany.
Statistical analysis
The results are given in mean ± standard deviation. The impact of mediolateral femoral component position was statistically evaluated using mixed-effects models with a random intercept per specimen. The cosine of the flexion angle (FA in radian), the squared cosine of the FA, the cubed cosine of the FA, moving direction (flexion or extension) as well as the different femoral component positions (3-mm medialized/neutral/3-mm lateralized) were assumed to be fixed factors. After consultation of the Institute of Medical Informatics, Biometry and Epidemiology (IBE) of the University of Munich, we decided for a mixed-effects model with a random intercept per specimen for this study. For this type of statistical test, a sample size calculation is not applicable, respectively, common. Therefore, we did not perform a sample size calculation. For the mixed-effects models, results were presented as main of regression coefficients and 95% confidence interval. All statistical analyses were calculated with SPSS software (SPSS release 21.0, IBM, New York, USA). All differences were considered significant with p < 0.05.
Results
The maximum quadriceps load was 737 ± 67 N for the lateral, 744 ± 72 N for the neutral and 751 ± 75 N for the medial position (n.s.), which resulted in a nonsignificant different ground reaction force between the variants (n.s.) (Table 1). The difference regarding retropatellar peak pressure was also not significant (n.s.). However there was a slight increase of retropatellar peak pressure after medialization of femoral component to 6.5 ± 2.4 MPa compared to 6.2 ± 2.5 MPa for the neutral position. For the lateralized variant, the decrease was also only minor with 6.0 ± 2.5 MPa. The differences and absolute values for retropatellar peak pressure increased with rising flexion angles. Concerning the distribution of retropatellar pressure, there was not a significant difference between the three tested variants (Fig. 3).
Regarding patello-femoral kinematics, ML position of femoral component led to a significant alteration in patella shift and tilt (Table 1). The differences in patella flexion and patella rotation were not significant. For the fully examined loaded squat, the patella was shifted following the translation of the femoral component (Fig. 4). As a consequence of altered shift, the patella was also significantly tilted in the same direction in 20° of flexion. With increasing flexion angels, the patella was tilted medially for all three variants (Fig. 5).
Concerning tibio-femoral kinematics, only translation of the femoral epicondylar axis, also called “roll-back”, was affected significantly. Tibio-femoral rotation was not significantly influenced by ML position of the femoral component (Table 1). For all three variants, roll-back was more prominent at the lateral compartment (Fig. 6). Concerning the roll-back of the lateral condyle between 20° and 120° flexion angle, there were only slight differences between the three tested variations. Compared to the neutral position with 8.2 ± 5.5, 3-mm lateralization revealed slightly more roll-back with 8.8 ± 6.1, 3-mm medialization, slightly less with 7.2 ± 5.7 mm.
Discussion
The most important finding of this study was the impact of femoral component ML position on patella shift. The patella followed directly the ML translation (Fig. 4). In terms of patella shift, this study could confirm the results of Armstrong et al. [3]. Therefore, it seems to be obvious that the trochlea determines the ML position of the patella. As a side effect of the altered shift, the patella was also significantly tilted in the same direction. The reason could be seen in the unchanged insertion of the patella tendon and the quadriceps muscle. This effect was most prominent between 20° and 40° flexion angle. With more relevant increase of flexion, the patella tilt of all three variations assimilated (Fig. 5). Even though these two parameters of patella kinematics were significantly influenced, retropatellar peak pressure was not significantly altered. There was only a slight decrease in peak pressure to 6.0 ± 2.5 MPa when testing the variant with 3-mm lateralization of the femoral component. Therefore, the hypothesis that a medialized femoral component would lead to significantly increased retropatellar pressure was not confirmed. The second aspect of the hypothesis with higher pressure at the lateral facet for a medialized femoral component could also not be proven since pressure distribution was unchanged for all three variants (Fig. 3).
Comparing the results of retropatellar peak pressure with former studies conducted with the same knee rig under the same loaded squat reveals a significant influence for rotation of the femoral as well as the tibial component [36, 38]. Regarding maximal peak values, the difference between 3° internal and 6° external rotation of the femoral components trochlea was 1.1 MPa (7.3 ± 2.3 vs. 6.2 ± 1.8 MPa). These alterations are more than two times higher compared to medialization and lateralization by 3 mm with an increase of 0.5 MPa (6.0 ± 2.5 vs. 6.5 ± 2.4 MPa). ML translations of the femoral or tibial [34] components have both only a minor effect on retropatellar pressure. The range of maximal peak value differences induced by 3-mm medialization versus 3-mm lateralization is in both cases about the same (0.5 MPa for the femoral component and 0.3 MPa for the tibial baseplate). Since decreased retropatellar peak pressure is clinically relevant to reducing anterior knee pain [14, 21], rotational alignment seems to be more important than the ML position.
The influence of femoral ML position on tibio-femoral kinematics with a significant increase in femoral roll-back especially for the variation with 3-mm lateralization was unexpected. This effect was more prominent for the lateral compartment (Fig. 4). The extent of roll-back for the lateralized variant is in tendency closer to the kinematical findings in the physiological tibio-femoral joint [13]. But the absolute values of roll-back at the lateral compartment of the lateralized femoral component were with 8.8 ± 6.1 mm still much less than determined in the native knee with about 15 mm [13]. A similar extent of roll-back was measured for a 3-mm medialized tibial baseplate (9.7 ± 4.7 mm) [37] using the same knee rig. But actually it is not proven that a more natural kinematic of the knee after TKA also comes along with superior clinical results [16, 19].
A comparison with the variant with 3-mm medialization of the baseplate is particularly interesting since in both cases the relative alteration in the femoral and tibial component to each other is the same. Hence, the reason for the increased lateral roll-back seems to be the same for both variations. An explanation could be seen in modified tensions of the collateral ligaments. Similar to registrations of ligament tension in tibial components with malrotation, the lateralization of the femoral component could result in increased tension of the medial collateral ligament and reduced tension of the lateral collateral ligament [22]. This alteration in tension could lead to a stabilization of the medial rather than the lateral compartment, resulting in a pronounced lateral roll-back.
Mediolateral position of the femoral component needs to be chosen with care and translation is limited to some mm. The main problem is ML overhang. Since AP dimension determines the size of femoral component, ML overhang of ≥3 mm is common [4, 9, 10, 15]. Especially in women the incidence can be up to 68% [25]. As a consequence, these patients have a higher risk of postoperative knee pain. To reduce the incidence of overhang, several implants with reduced ML dimensions were introduced [9]. But a clinical benefit of these “gender-specific” implants could not be proven [8]. Since medialization or lateralization of the femoral component could lead to increased medial or lateral overhang, there would be a higher risk of soft tissue irritation and unfavourable postoperative results.
There is one clinical study examining the impact of ML malpositioning of the femoral component [39]. Against the hypothesis of the authors medialization of ≥5 mm resulted in a better postoperative outcome. The authors tried to explain these findings by the lateral trochlear orientation of the femoral component. These results cannot be proven by this in vitro study since medialization did not lead to decreased retropatellar pressure or more physiological femoral roll-back.
This study has several limitations. First of all, there are the typical limitations of all in vitro studies using cadaver specimens examined in a knee rig. The specimens were loaded following a simulated squat. With this experimental set-up, most activities of daily living (e.g. walking, rising from a chair or stair climbing) cannot be simulated. But similar to other studies using a knee rig, the influence of implant position on kinematics and retropatellar pressure might be transferrable to daily activities.
To evaluate different ML positions of the femoral component using the same femoral cuts and femoral pegs, it was necessary to produce rapid prototyping TKA replicas. Even if the materials are different compared with the original implant, both prostheses reveal similar in vitro test results [33].
It must also be taken into account that the results only apply for TKA with a fixed-bearing design like the one used for this study (Columbus CR, Aesculap AG, Tuttlingen, Germany). Other TKA designs like mobile-bearing or posterior stabilized TKA would result in different roll-back and probably also different patella kinematics.
Conclusion
Mediolateral positioning of the femoral component has an impact on patellar as well as tibio-femoral kinematics and should therefore be addressed with care. Since ML position has no significant influence on retropatellar peak pressure, the risk of anterior knee pain seems to remain rather unchanged. ML malpositioning should be limited to avoid implant overhang resulting in postoperative pain. Adequate rotational alignments of the femoral as well as the tibial component are more relevant during implantation of TKA to decrease retropatellar pressure and therefore the incidence of anterior knee pain.
References
Anderson JG, Wixson RL, Tsai D, Stulberg SD, Chang RW (1996) Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty 11(7):831–840
Anglin C, Brimacombe JM, Wilson DR, Masri BA, Greidanus NV, Tonetti J, Hodgson AJ (2010) Biomechanical consequences of patellar component medialization in total knee arthroplasty. J Arthroplasty 25(5):793–802. doi:10.1016/j.arth.2009.04.023
Armstrong AD, Brien HJ, Dunning CE, King GJ, Johnson JA, Chess DG (2003) Patellar position after total knee arthroplasty: influence of femoral component malposition. J Arthroplasty 18(4):458–465
Babazadeh S, Dowsey MM, Swan JD, Stoney JD, Choong PF (2011) Joint line position correlates with function after primary total knee replacement: a randomised controlled trial comparing conventional and computer-assisted surgery. J Bone Joint Surg Br 93(9):1223–1231
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63
Boyd AD Jr, Ewald FC, Thomas WH, Poss R, Sledge CB (1993) Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am 75(5):674–681
Bull AM, Katchburian MV, Shih YF, Amis AA (2002) Standardisation of the description of patellofemoral motion and comparison between different techniques. Knee Surg Sports Traumatol Arthrosc 10(3):184–193
Cheng T, Zhu C, Wang J, Cheng M, Peng X, Wang Q, Zhang X (2014) No clinical benefit of gender-specific total knee arthroplasty. Acta Orthop 85(4):415–421
Dai Y, Scuderi GR, Penninger C, Bischoff JE, Rosenberg A (2014) Increased shape and size offerings of femoral components improve fit during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(12):2931–2940
Dennis DA (2004) Evaluation of painful total knee arthroplasty. J Arthroplasty 19(4 Suppl 1):35–40
Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A (2004) A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 428:180–189
Dunbar MJ, Robertsson O, Ryd L, Lidgren L (2001) Appropriate questionnaires for knee arthroplasty. Results of a survey of 3600 patients from The Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br 83(3):339–344
Freeman MA, Pinskerova V (2005) The movement of the normal tibio-femoral joint. J Biomech 38(2):197–208
Fuchs S, Skwara A, Tibesku CO, Rosenbaum D (2005) Retropatellar contact characteristics before and after total knee arthroplasty. Knee 12(1):9–12
Incavo SJ, Beynnon BD, Johnson CC, Churchill DL (1997) Knee kinematics in genesis total knee arthroplasty. A comparison of different tibial designs with and without posterior cruciate substitution in cadaveric specimens. Am J Knee Surg 10(4):209–215
Ishida K, Matsumoto T, Tsumura N, Iwakura T, Kubo S, Iguchi T, Akisue T, Nishida K, Kurosaka M, Kuroda R (2014) No difference between double-high insert and medial-pivot insert in TKA. Knee Surg Sports Traumatol Arthrosc 22(3):576–580
Keshmiri A, Maderbacher G, Baier C, Zeman F, Grifka J, Springorum HR (2016) Significant influence of rotational limb alignment parameters on patellar kinematics: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24(8):2407–2414
Keshmiri A, Springorum HR, Baier C, Zeman F, Grifka J, Maderbacher G (2016) Changes in sagittal component alignment alters patellar kinematics in TKA: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24(3):823–829
Kim YH, Yoon SH, Kim JS (2009) Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin Orthop Relat Res 467(2):493–503
Koninckx A, Deltour A, Thienpont E (2014) Femoral sizing in total knee arthroplasty is rotation dependant. Knee Surg Sports Traumatol Arthrosc 22(12):2941–2946
Kulkarni SK, Freeman MA, Poal-Manresa JC, Asencio JI, Rodriguez JJ (2000) The patellofemoral joint in total knee arthroplasty: is the design of the trochlea the critical factor? J Arthroplasty 15(4):424–429
Kuriyama S, Ishikawa M, Furu M, Ito H, Matsuda S (2014) Malrotated tibial component increases medial collateral ligament tension in total knee arthroplasty. J Orthop Res 32(12):1658–1666
Lutzner J, Kirschner S, Gunther KP, Harman MK (2012) Patients with no functional improvement after total knee arthroplasty show different kinematics. Int Orthop 36(9):1841–1847
Lutzner J, Krummenauer F, Gunther KP, Kirschner S (2010) Rotational alignment of the tibial component in total knee arthroplasty is better at the medial third of tibial tuberosity than at the medial border. BMC Musculoskelet Disord 11:57
Mahoney OM, Kinsey T (2010) Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am 92(5):1115–1121
Merican AM, Ghosh KM, Iranpour F, Deehan DJ, Amis AA (2011) The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19(9):1479–1487
Moran CG, Horton TC (2000) Total knee replacement: the joint of the decade. A successful operation, for which there’s a large unmet need. BMJ 320(7238):820
Nagamine R, Whiteside LA, White SE, McCarthy DS (1994) Patellar tracking after total knee arthroplasty. The effect of tibial tray malrotation and articular surface configuration. Clin Orthop Relat Res 304:262–271
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Bohler N, Labek G (2013) Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty 28(8):1329–1332
Saranathan A, Kirkpatrick MS, Mani S, Smith LG, Cosgarea AJ, Tan JS, Elias JJ (2012) The effect of tibial tuberosity realignment procedures on the patellofemoral pressure distribution. Knee Surg Sports Traumatol Arthrosc 20(10):2054–2061
Schotanus MG, Schoenmakers DA, Sollie R, Kort NP (2016) Patient-specific instruments for total knee arthroplasty can accurately predict the component size as used peroperative. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4345-1
Schroder C, Steinbruck A, Muller T, Woiczinski M, Chevalier Y, Weber P, Muller PE, Jansson V (2015) Rapid prototyping for in vitro knee rig investigations of prosthetized knee biomechanics: comparison with cobalt-chromium alloy implant material. Biomed Res Int. doi:10.1155/2015/185142
Steinbruck A, Fottner A, Schroder C, Woiczinski M, Schmitt-Sody M, Muller T, Muller PE, Jansson V (2015) Influence of mediolateral tibial baseplate position in TKA on knee kinematics and retropatellar pressure. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3843-x
Steinbruck A, Schroder C, Woiczinski M, Fottner A, Muller PE, Jansson V (2013) Patellofemoral contact patterns before and after total knee arthroplasty: an in vitro measurement. Biomed Eng Online 12:58
Steinbruck A, Schroder C, Woiczinski M, Fottner A, Muller PE, Jansson V (2014) The effect of trochlea tilting on patellofemoral contact patterns after total knee arthroplasty: an in vitro study. Arch Orthop Trauma Surg 134(6):867–872
Steinbruck A, Schroder C, Woiczinski M, Fottner A, Pinskerova V, Muller PE, Jansson V (2016) Femorotibial kinematics and load patterns after total knee arthroplasty: an in vitro comparison of posterior-stabilized versus medial-stabilized design. Clin Biomech 33:42–48
Steinbruck A, Schroder C, Woiczinski M, Muller T, Muller PE, Jansson V, Fottner A (2015) Influence of tibial rotation in total knee arthroplasty on knee kinematics and retropatellar pressure: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24(8):2395–2401
van de Groes SA, Koeter S, de Waal Malefijt M, Verdonschot N (2014) Effect of medial-lateral malpositioning of the femoral component in total knee arthroplasty on anterior knee pain at greater than 8 years of follow-up. Knee 21(6):1258–1262
Vince KG (2003) Why knees fail. J Arthroplasty 18(3 Suppl 1):39–44
Wylde V, Learmonth I, Potter A, Bettinson K, Lingard E (2008) Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br 90(9):1172–1179
Zihlmann MS, Stacoff A, Romero J, Quervain IK, Stussi E (2005) Biomechanical background and clinical observations of rotational malalignment in TKA: literature review and consequences. Clin Biomech 20(7):661–668
Acknowledgements
We kindly thank the Aesculap B. Braun company for donating the prostheses used in this study. Sincere thanks are given to Moritz von Holst for his help in translating our text into English and to Dr. Alexander Crispin (Institute of Biometry and Epidemiology, LMU Munich) for his statistical council.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Aesculap B. Braun has donated the prostheses used in this study. They had no influence on the study design nor on the results or interpretation of data. Furthermore they had no involvement in writing the manuscript and no influence in the decision to submit the article to this journal. AS, CS, PEM and VJ are consultants for the B. Braun Aesculap Company. All authors declare that they have no conflict of interest.
Funding
No funding was received.
Ethical approval
The study was approved by the ethical committee of the University of Munich (LMU), Germany.
Informed consent
For this type of article informed consent is not required.
Rights and permissions
About this article
Cite this article
Steinbrück, A., Schröder, C., Woiczinski, M. et al. Mediolateral femoral component position in TKA significantly alters patella shift and femoral roll-back. Knee Surg Sports Traumatol Arthrosc 25, 3561–3568 (2017). https://doi.org/10.1007/s00167-017-4633-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4633-4