Abstract
Purpose
Our study sought to address four issues: (1) the relationship between postoperative overall anatomical knee alignment and the survival of total knee prostheses; (2) the relationship between postoperative coronal alignment of the femoral and tibial component and implant survival; (3) the relationship between postoperative sagittal alignment of the femoral and tibial components and implant survival; and (4) the relationship between postoperative rotational alignment of the femoral and tibial component and implant survival.
Methods
We reviewed 1,696 consecutive patients (3,048 knees). Radiographic and computed tomographic examinations were performed to determine the alignment of the femoral and tibial components. The mean duration of follow-up was 15.8 years (range, 11–18 years).
Results
Thirty (1.0 %) of the 3,048 total knee arthroplasties failed for a reason other than infection and periprosthetic fracture. Risk factors for failure of the components were: overall anatomical knee alignment less than 3° valgus, coronal alignment of the femoral component less than 2.0° valgus, flexion of the femoral component greater than 3°, coronal alignment of the tibial component less than 90°, sagittal alignment of the tibial component less than 0° or greater than 7° slope, and external rotational alignment of the femoral and tibial components less than 2°
Conclusion
In order to improve the survival rate of the knee prosthesis, we believe that a surgeon should aim to place the total knee components in the position of: overall anatomical knee alignment at an angle of 3–7.5° valgus; femoral component alignment, 2–8.0° valgus; femoral sagittal alignment, 0–3°; tibial coronal alignment, 90°; tibial sagittal alignment, 0–7°; femoral rotational alignment, 2–5° external rotation; and tibial rotational alignment, 2–5° external rotation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interest in the accurate positioning and alignment of total knee components has been the subject of controversy, particularly following the development of computer-navigation surgery [1]. Proper alignment of total knee components is strongly associated with greater stability, a lower rate of loosening, and higher clinical scores [2–9]; however, the current literature lacks a precise range of values for postoperative overall anatomical knee alignment or coronal, sagittal and rotational alignment of the femoral and tibial components to achieve the best possible long-term prosthesis survival.
Our study sought to address four issues: (1) the relationship between postoperative overall anatomical knee alignment and the survival of total knee prosthesis; (2) the relationship between postoperative coronal alignment of the femoral and tibial components and implant survival; (3) the relationship between postoperative sagittal alignment of the femoral and tibial components and implant survival; and (4) the relationship between postoperative rotational alignment of the femoral and tibial components and implant survival.
Materials and methods
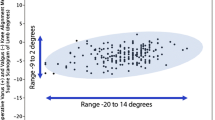
We prospectively followed up and retrospectively reviewed 1,747 consecutive patients (3,150 knees) who underwent primary total knee arthroplasties (TKAs) from May 1994 to June 2001. Fifty-one patients (102 knees) were lost to follow-up. The remaining 1,696 consecutive patients (3,048 knees) formed our study cohort. The study group consisted of 1,584 women and 112 men with a mean age of 61.2 ± 9.6 years (range, 23–79 years) at the time of the index surgery. The preponderance of women in this series was due to the specific ethnic group of these patients. The mean height of the patients was 154.5 ± 6.6 cm (range 138–176 cm), the mean weight was 63.0 ± 8.9 kg (range 40–86 kg), and the mean body mass index was 26.4 ± 3.6 kg/m2 (range 17.0–37.8 kg/m2). The preoperative diagnosis was osteoarthritis in 1,616 patients (2,896 knees), osteonecrosis in 70 patients (133 knees), and rheumatoid arthritis in ten patients (19 knees). The mean preoperative overall anatomical (femorotibial) knee alignment was 10.0° ± 6.9° varus (range 8–20° varus) on the basis of long-leg X-ray including femoral head and ankle.
All total knee arthroplasties were performed by the senior author (YHK). The procedure was carried out through a midline skin incision of ten to 12 cm in length using a medial parapatellar arthrotomy. Extramedullary instrumentation was used for the tibial component and intramedullary for the femoral side. The femoral valgus angle for the intramedullary guide was determined preoperatively on standardised long-leg weight-bearing radiographs. The anterior and posterior cruciate ligaments were resected in all knees. Ligamentous balance was restored and ten millimetres of tibial bone was resected to achieve a surface which was perpendicular to the shaft of the tibia in the coronal plane with a posterior slope of 7° in the sagittal plane. Resection of the distal femur (nine to 11 mm) and the posterior femoral condyles (nine to 11 mm) was attempted to remove a thickness of bone which was equal to that of the femoral component to be implanted. During femoral and tibial resection the tibia was prepared first in all knees. Anterior cortical reference was used for the anterior-posterior cut of the distal femur. Femoral component rotation was determined using three reference axes: (1) the transepicondylar axis, (2) the mid-trochlear line (Whiteside line), and (3) 3˚ of external rotation relative to the posterior aspect of the condyles. Tibial component rotation was determined using the medial 1/3 of the tibial tuberosity and attachment site of posterior cruciate ligament and posterior margin of the tibial implant. The low contact stress mobile-bearing rotation platform (LCS RP; DePuy, Warsaw, Indiana) prosthesis was used in all knees.
The knee was placed in a continuous-passive motion machine after the splint was removed (on the second day after the operation). All patients began walking with crutches or a walker and started active and passive range-of-motion exercise on the second day after the operation. The patients used the crutches or walker, with full weight-bearing, for six weeks and a cane when necessary thereafter.
Clinical and radiographic reviews were carried out at three months, one year, and yearly thereafter. The mean duration of follow-up was 15.8 years (range, 11–18 years). All of the clinical data analysis and the radiographic and computed tomographic (CT) scanning measurements were performed and compiled by one research associate (SML) who was not involved in the surgery. Pre- and postoperative scores were obtained for all patients with the use of the Knee Society [10] knee-scoring system.
Radiographic evaluation
All patients had complete radiographic follow-up examinations. All of the radiographs were reviewed by one research associate (SML) who had no knowledge of the patients. Full-length anteroposterior radiographs of the knee, including the femoral head and the ankle made with and without weight-bearing, and lateral and skyline patellar radiographs were made preoperatively and at each follow-up. The overall anatomical knee alignment and the position of the femoral and tibial components in the coronal and sagittal planes were determined (Figs. 1 and 2). The location of radiolucent lines at the cement-bone or cement-implant interfaces was scrutinised as recommended by the Knee Society [10]. The intra-observer kappa statistics for the radiographic examinations was 0.95.
The overall anatomical alignment in the coronal plane was defined as the angle between the femoral anatomical axis and the tibial anatomical axis. The tibial alignment was defined as the angle between the proximal portion of the tibial component and the tibial anatomical axis. The femoral alignment was defined as the angle between the distal portion of the femoral component and the femoral anatomical axis (α = coronal femoral angle, and β = coronal tibial angle)
A lateral radiograph of the right knee shows the measurement of the sagittal alignment of the femoral and tibial components (x = sagittal femoral angle, and y = sagittal tibial angle). The posterior femoral condylar offset (CO) was evaluated by measuring the maximum thickness of the posterior condyle projected posteriorly to the tangent of the posterior cortex of the femoral shaft
Computed tomographic measurements
Postoperative CT scans (at one week after the operation and at final follow-up) were obtained using a multislice scanner (General Electric Light Plus; GE Medical Systems, Milwaukee, Wisconsin). Routine CT scan was obtained at one week after the operation to determine the rotational alignment of the femoral and tibial component. Routine CT scan was obtained at the final follow-up to determine the presence of osteolysis. This was an ethically approved project. The scan sequence was started at the superior pole of the patella and ended at the tibial tuberosity, in contiguous slices of 2.5 mm. The rotation of the femoral component was determined in relation to the transepicondylar axis [9]. An axial image of the distal femur was chosen which most clearly demonstrated the medial epicondylar sulcus, when present, or the central point of the medial epicondyle when no sulcus was found, and the lateral epicondylar prominence. A line was drawn between these two points, thereby establishing the surgical epicondylar axis. A second line was drawn across the posterior condyles of the femoral component. The angle between these represented the rotation of the femoral component. Because the mobile nature of the tibial bearing may affect the true rotational alignment of the tibial component, the rotational alignment of the tibial component was determined relative to the posterior margins of proximal tibia and the tibial bearing. A line was drawn along the posterior margin of the tibial plateau. A second line was drawn along the posterior margin of the tibial bearing. The angle between these represented the rotation of the tibial component. Rotational alignment of the tibial component was defined as neutral when the two lines were converged. When the line along the posterior margin of the tibal bearing diverged posteriorly, relative to the line along the posterior margin of the tibial plateau, the tibial component was defined as externally rotated. When the reverse of this finding was seen, the tibial component was defined as internally rotated (Fig. 3). The intraobserver kappa statistics for the CT examinations was 0.93.
CT scan shows measurement of axial rotation of the femoral component in relation to the transepicondylar axis (A–A) and posterior femoral condylar line. CT scan shows measurement of axial rotation of the tibial component in relation to the posterior margins of the tibial plateau (A–A) and the tibial bearing (B–B)
Statistical analysis
Cox regression analysis was performed with forward, backward, and stepwise selection in order to determine the variables most strongly predictive of failure. The variables analysed were postoperative overall anatomical knee alignment, and postoperative coronal, sagittal, and rotational alignment of the femoral and tibial components. The postoperative overall anatomical knee alignment was highly linked to the tibial alignment and with the femoral alignment; consequently, analysis of covariates was first performed by including overall tibiofemoral alignment and excluding both femoral and tibial alignment variables, then repeated by including both femoral and tibial alignment and excluding overall anatomical knee alignment.
An extended Cox model based on generalised estimating equation theory was used to compare survival by risk factor and to perform a multivariate analysis of the survival of implants [11]. These analyses were used in all univariate and multivariate significance tests and for the calculation of all 95 % confidence intervals [11].
Neutral (optimal) alignment was determined using an algorithm that examined the range of angles associated with the lowest failure rate and selected the narrowest range that had the greatest significance in the full model. Neutral alignment was determined separately for the overall anatomical knee alignment, the coronal and sagittal alignment of the femoral component, the coronal and sagittal of the tibial component, and the rotational alignment of the femoral and tibial components by Cox regression analysis. All statistical tests were two-sided, and p values of < 0.05 were considered significant. Kaplan-Meier survival analysis [12] of the time to failure was performed with revision for any reason other than infection and periprosthetic fracture.
Using the approach of Dupont and Plummer [13], a post hoc power analysis was conducted to estimate the minimum sample size needed to observe a significant difference between the neutrally aligned group and the malaligned group. With regard to the revision for aseptic loosening, the study was adequately powered to detect a significant difference (α < 0.05) with 80 % power if the malaligned group had a two-fold increased risk of failure (a hazard ratio of 2.0). This degree of power would be achieved from study groups comprising at least 1,485 neutrally aligned knees and 551 malaligned knees (total 2,036 knees).
Results
As expected there were significant differences (Student’s t-test, p < 0.05) between intact and revised groups with regard to: postoperative Knee Society knee scores (96.0 ± 8.4 points; range, 74–100 points versus 88.3 ± 6.6 points; range, 79–88 points); Knee Society function scores (82.4 ± 18.7 points; range, 20–100 points versus 61.7 ± 35.5 points; range, 10–80 points); and ranges of motion (120.7° ± 19.9°; range, 70–145° versus 117.5° ± 16.7°; range, 90–130°).
Thirty (1.0 %) of the 3,048 TKAs failed for a reason other than infection and periprosthetic fracture. The mean time to failure was 9.8 ± 3.2 years (range, eight to 12.8 years). In the univariate exploratory analysis, age, anatomical femorotibial alignment and coronal, sagittal and rotational alignments of femoral and tibial components were the factors significantly associated with survival of the implants. Sex, body mass index and preoperative deformity did not have a substantial effect on survival on the implants.
Postoperative overall anatomical femorotibial alignment
A postoperative overall anatomical femorotibial alignment conferred an advantage in terms of survival of the implants in the multivariate analysis, after adjusting for age and body mass index. In 1,928 knees the postoperative overall anatomical femorotibial alignment was 3–7.5° valgus (neutrally aligned group), in 664 knees the postoperative alignment was less than 3° valgus (varus aligned group), and in 456 knees the alignment was greater than 7.5° valgus (valgus aligned group). Eleven out of 1,928 knees (0.6 %) required revision of the femoral and tibial components in the neutrally aligned group, 15 out of 664 knees (2.3 %) required revision of both components in the varus aligned group, and four out of 456 knees (0.9 %) required revision of both components in the valgus aligned group (Table 1).
Postoperative coronal alignment of the femoral component
A postoperative coronal alignment of the femoral component conferred an advantage in terms of survival of the implants in the multivariate analysis, after adjusting for age and body mass index. In 2,858 knees the postoperative coronal alignment of the femoral component was 2.0–8.0° valgus (neutrally aligned group), in 160 knees the postoperative alignment was less than 2.0° valgus (varus aligned group), and in 58 knees the alignment was greater than 8.0° valgus (valgus aligned group). Twenty-one out of 2,858 knees (0.7 %) required revision of both components in the neutrally aligned group, eight out of 160 knees (5.0 %) required revision of both components in the varus aligned group, and one out of 58 knees (1.7 %) required revision of both components in the valgus aligned group (Table 2).
Postoperative sagittal alignment of the femoral component
A postoperative sagittal alignment of the femoral component conferred an advantage in terms of survival of the implants in the multivariate analysis, after adjusting for age and body mass index. In 1,735 knees the postoperative femoral sagittal alignment was 0–3° (neutrally aligned group), in 748 knees the postoperative alignment was greater than 3° flexion (flexion group), and in 565 knees the postoperative alignment was greater than 1° extension (extension group). No knees required revision of the component in the neutrally aligned group, 25 out of 748 knees (3.3 %) required revision of both components in the flexion group, and five out of 565 knees (0.9 %) required revision of both components in the extension group (Table 3).
Postoperative coronal alignment of the tibial component
A postoperative coronal alignment of the tibial component conferred an advantage in terms of survival of the implants in the multivariate analysis, after adjusting for age and body mass index. In 2,168 knees the postoperative coronal tibial alignment was 90° (neutrally aligned group), and in 880 knees the alignment was less than 90° (varus aligned group). No knees in the neutrally aligned group required revision of the components, and 30 out of 880 knees (3.4 %) required revision in the varus aligned group (Table 4).
Postoperative sagittal alignment of the tibial component
A postoperative sagittal alignment of the tibial component conferred an advantage in terms of survival of the implants in the multivariate analysis, after adjusting for age and body mass index. In 2,495 knees the postoperative sagittal tibial alignment of the tibial component was 0–7° (normally aligned group), and in 553 knees the alignment was less than 0° or greater than 7° (abnormally aligned group). Five out of 2,495 knees (0.2 %) required revision of both components in the normally aligned group, and 25 out of 553 knees (4.5 %) required revision of both components in the abnormally aligned group (Table 5).
Postoperative rotational alignment of the femoral component
A postoperative rotational alignment of the femoral component conferred an advantage in terms of survival of the implants in the multivariate analysis, after adjusting for age and body mass index. In 2,490 knees the postoperative rotational alignment of the femoral component was 2–5° external rotation, in 401 knees the rotational alignment was less than 2° external rotation, and in 157 knees the external rotation was greater than 5°. No knee required revision of the components in the group with 2–5° external rotation, 27 out of 401 knees (6.7 %) required revision of both components in the group with less than 2° external rotation, and three out of 157 knees (1.9 %) required revision of both components in the group with an external rotation greater than 5° (Table 6).
Postoperative rotational alignment of the tibial component
A postoperative rotational alignment of the tibial component conferred an advantage in terms of survival of the implants in the multivariate analysis, after adjusting for age and body mass index. In 2,490 knees the postoperative rotational alignment of the tibial component was 2–5° external rotation, in 413 knees the rotational alignment was less than 2° external rotation, and in 145 knees the rotational alignment was greater than 5° external rotation. One out of 2,490 knees (0.04 %) required revision of both components in the group with 3–5° external rotation, 27 out of 416 knees (6.5 %) required revision of both components in the group with less than 2° external rotation, and two out of 145 knees (1.4 %) required revision of both components in the group with an external rotation greater than 5° (Table 7).
Discussion
Although the roles of overall anatomical knee alignment and/or femoral and tibial component alignment in the coronal plane in total knee replacement failures [2–9] are well documented, little has been reported regarding the effect of the sagittal and rotational alignment of the femoral and tibial components. The results of our study confirm that attaining neutrality of all coronal, sagittal and rotational alignments of the femoral and tibial components is vital in maximising implant longevity.
Although three recent studies have found little correlation between anatomical femorotibial alignment in the coronal plane and revision rates [7, 8, 14], the majority of studies have shown increased revision rates with coronal malalignment, particularly in the varus [2–4, 6, 15, 16]. In our study, a coronal femorotibial alignment of less than 3° valgus probably contributed to aseptic loosening of the components. Moreover, less than 2.0° valgus or greater than 8.0° valgus of the femoral component and any varus alignment of the tibial component (less than 90°) contributed to an increased failure rate of the components.
It has been claimed that it is more difficult to achieve good sagittal than coronal alignment of the femoral and tibial components [17, 18], yet the impact of sagittal malalignment has been studied relatively little. However, sagittal instability does occur [19] and has been associated with an excessive tibial slope [20]. Since variations in tibial slope produce reciprocal alterations in flexion and extension gaps, the complications of sagittal malalignment are probably the consequence of flexion-extension match. In our study, sagittal alignment of the femoral component of more than 3° flexion increased femoral component failure significantly. Additionally, sagittal alignment of the tibial component (posterior tibial slope) of less than 0° or greater than 7° increased tibial component failure significantly.
Alignment in the coronal plane does not guarantee the accurate position of each component in flexion/extension, valgus/varus or balanced tibio-femoral rotation. The effect on implant survival of accurate positioning of each individual component in 6° of freedom is not clearly established. There is anecdotal evidence that early mechanical failure is more likely when there is a mismatch of the femoral and tibial components in rotation [9]. However, reliable evidence of the effect of rotational alignment on implant survival is limited because intra- and postoperative measurement techniques are often inaccurate and the optimal rotational alignment target has not been defined [21–23]. In our study, rotational alignment of the femoral component less than 2° external rotation or greater than 5° external rotation increased component failure significantly. Furthermore, rotational alignment of the tibial component less than 2° external rotation or greater than 5° external rotation increased component failure significantly.
The survival rate of the components in our series at 15.8 years was 99 % (95 % confidence interval, 0.96–1.00) as the end point of revision other than infection and periprosthetic fracture. Advances in implant design, polyethylene processing, and cementing technique might improve the survival of implants.
Our study has some strengths. The study focused on the overall anatomical knee alignment, and coronal, sagittal and rotational alignment of the femoral and tibial components. However, our study has some limitations. First, we cannot exclude the possibility of bias owing to the single-observer unblinded measurements of the X-rays and CT scans. Second, this was a retrospective study and the patients were followed up prospectively. Third, as the number of revision cases were only 30, they could reach the significant statistic level because of type II error. Fourth, we did not investigate the dynamic alignment of the limb in either the coronal, sagittal or rotational plane after TKA [24–26]. Finally, although our measurement of the rotational alignment of the tibial component was not as precise as the technique employed by Bell et al. [27], we believe our technique suffices to apply for the measurement of the rotational alignment of the mobile bearing tibial component. Despite these limitations, our study is, to our knowledge, the largest study to investigate the impact of postoperative coronal, sagittal and rotational alignment of an implant on 15.8-year implant survival following modern TKA.
In summary, in order to improve the survival rate of the knee prosthesis, we believe that a surgeon should aim to place the total knee components in the position of: overall anatomical knee alignment at an angle of 3–7.5° valgus; femoral coronal alignment, 2–8.0° valgus; femoral sagittal alignment, 0–3°; tibial coronal alignment, 90°; tibial sagittal alignment, 0–7°; femoral rotational alignment, 2–5° external rotation; and tibial rotational alignment, 2–5° external rotation.
References
Laskin RS, Beksac B (2006) Computer-assisted navigation in TKA: where we are and where we are going. Clin Orthop Relat Res 452:127–131
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Fang DM, Ritter MA, Davis KE (2009) Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty 24(6 suppl):39–43
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg Br 73(5):709–714
Ritter MA (2009) The anatomical graduated component total knee replacement: a long-term evaluation with 20-year survival analysis. J Bone Joint Surg Br 91(6):745–749
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res 299:153–156
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92(12):2143–2149
Bonner TJ, Eardley WG, Patterson P, Gregg PJ (2011) The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg Br 93(9):1217–1222
Sikorski JM (2008) Alignment in total knee replacement. J Bone Joint Surg Br 90(9):1121–1127
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Petrie A (2006) Statistics in orthopaedic papers. J Bone Joint Surg Br 88(9):1121–1136
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Dupont WD, Plummer WD Jr (1998) Power and sample size calculations for studies involving linear regression. Control Clin Trials 19:589–601
Morgan SS, Bonshahi A, Pradhan N, Gregory A, Gambhir A, Porter ML (2008) The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int Orthop 32(5):639–642
Lewallen DG, Bryan RS, Peterson LF (1984) Polycentric total knee arthroplasty. A ten-year follow-up study. J Bone Joint Surg Am 66(8):1211–1218
Tew M, Waugh W (1985) Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg Br 67(4):551–556
Chauhan SK, Clark GW, Lloyd S, Scott RG, Breidahl W, Sikorski JM (2004) Computer-assisted total knee replacement. A controlled cadaver study using a multi-parameter quantitative CT assessment of alignment (the Perth CT protocol). J Bone Joint Surg Br 86(6):818–823
Sikorski JM, Blythe MC (2005) Learning the vagaries of computer-assisted total knee replacement. J Bone Joint Surg Br 87(7):903–910
Clarke HD, Scuderi GR (2003) Flexion instability in primary total knee replacement. J knee Surg 16(2):123–128
Sah AP, Scott RD, Iorio R (2008) Angled polyethylene insert exchange for sagittal tibial malalignment in total knee arthroplasty. J Arthroplasty 23(1):141–144
Rienmüller A, Guggi T, Gruber G, Preiss S, Drobny T (2012) The effect of femoral component rotation on the five-year outcome of cemented mobile bearing total knee arthroplasty. Int Orthop 36(10):2067–2072
van der Linden-van der Zwaag HM, Bos J, van der Heide HJ, Nelissen RG (2011) A computed tomography based study on rotational alignment accuracy of the femoral component in total knee arthroplasty using computer-assisted orthopaedic surgery. Int Orthop 35(6):845–850
Daniilidis K, Tibesku CO (2013) Fronatal plane alignment after total knee arthropalsty using patient-specific instruments. Int Orthop 37(1):45–50
Scuderi GR, Komistek RD, Dennis DA, Insall JN (2003) The impact of femoral component rotational alignment on condylar lift-off. Clin Orthop Relat Res 410:148–154
Komistek RD, Scott RD, Dennis DA, Yasgur D, Anderson DT, Hajner ME (2002) In vivo comparison of femorotibial contact positions for press-fit posterior stabilized and posterior cruciate-retaining total knee arthroplasties. J Arthroplasty 17(2):209–216
Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB (2003) Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res 416:37–57
Bell SW, Young P, Drury C, Smith J, Anthony I, Jones B, Blyth M, McLean A. Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee 160(12)163–169
Acknowledgments
The authors thank Sang-Mi Lee, MA for her data analysis of clinical and radiographic findings.
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was approved by our institutional review board, and all patients provided informed consent.
Rights and permissions
About this article
Cite this article
Kim, YH., Park, JW., Kim, JS. et al. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. International Orthopaedics (SICOT) 38, 379–385 (2014). https://doi.org/10.1007/s00264-013-2097-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2097-9