Abstract
Objectives
Elevated hip fracture incidence is a major public health problem looming to aggravate in industrialized countries due to demographic developments. We report hip fracture incidence and expected future cases from Vorarlberg, the westernmost province of Austria, results potentially representative of Central European populations.
Methods
Crude and standardized hip fracture incidence rates in Vorarlberg 2003–2013 are reported. Based on the age-specific incidence in 2013 or trends 2003–2013, we predict hip fractures till 2050.
Results
Female age-standardized hip fracture incidence decreased 2005–2013, whereas for men, the trend was rather unclear. Uncorrected forecasts indicate that by 2050, female and male cases will each have more than doubled from 2015 in all demographic core scenarios. Corrected by incidence trends before 2013, cases are expected to drop among women but rise among men.
Conclusions
We anticipate rising hip fracture numbers in Vorarlberg within the next decades, unless prevention programs that presumably account for decreasing incidence rates, particularly among women since 2005, take further effect to counteract the predicted steady increase due to demographic changes. Concomitantly, augmented endeavors to target the male population by these programs are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis, a systemic skeletal disease characterized by low bone mass and architectural derangements (Sambrook and Cooper 2006), is a significant medical health problem due to the resulting elevated risk for skeletal fractures, particularly in developed countries (Johnell and Kanis 2006). Hip fractures, 90 % of which occur after the age of 50 (Sambrook and Cooper 2006), their vast majority being low trauma fragility fractures (Hernlund et al. 2013), are the most devastating consequence of osteoporosis. Known risk factors for osteoporosis include biological ones like female sex, older age, and low body mass index, but also behavioral factors like limited physical activity, smoking, and alcohol consumption, and nutritional factors like low dietary calcium (Hernlund et al. 2013; Zhu and Prince 2015; Peterlik et al. 2009). Importantly, also environmental influences like restricted sun exposure impinging upon vitamin D status (Holick 2011; Peterlik et al. 2009), and exposure to cadmium (James and Meliker 2013) have been associated with osteoporosis.
Hospitalization is required for virtually all hip fractures, sometimes followed by a long recovery or permanent disablement, which contributes to an enormous osteoporosis-related financial burden (Becker et al. 2010). For Austria, the total annual financial burden incurred by osteoporotic fractures for the year 2008 was estimated to amount to 685.2 million € (Dimai et al. 2012). Prevention of osteoporosis-related fractures is, thus, an important public health issue. Whereas primary prevention aims at the protection against bone loss, secondary prevention measures are targeted at inhibiting advanced bone loss to avoid fractures (Grossman 2011). Since most osteoporotic fractures occur with a fall, efficient fall prevention is an additional measure to reduce the burden of fragility fractures (El-Khoury et al. 2013).
To date in Austria, little is known about the epidemiology of osteoporosis and its impact on skeletal fractures on population level (Dorner et al. 2009). Geographic trends reveal much higher hip fracture incidence rates in Austria than in the surrounding countries, being in line with those in Scandinavian countries (Cheng et al. 2011): For example, compared to Germany, hip fracture incidence in Austria was reported to be 30 % higher with a slight increase between 1995 and 2004 (Mann et al. 2010). However, a decrease of the age-standardized incidence among the entire Austrian population has been observed by mid of the last decade (Dimai et al. 2011), and several other international studies have reported a recent decline of hip fracture incidence rates, in particular for women (Cooper et al. 2011).
The Vorarlberg Health Monitoring & Prevention Program (VHM&PP) (Concin et al. 2013) is a population-based risk factor surveillance program in Vorarlberg, the westernmost and second smallest province in Austria, inhabited by approximately 370,000 residents (2013), with a long-standing tradition of health surveillance and disease prevention. The VHM&PP is implemented by the Agency for Social and Preventive Medicine, its primary purpose being prevention of foremost chronic diseases and cancer. As part of the program, by the end of the 1990s prevention campaigns were initiated to reduce osteoporosis-related disease burden, including fall prevention measures like widely offered osteoporosis gymnastics, as well as advanced screening and treatment of osteoporosis. To survey the success of such public health-related programs, epidemiological studies monitoring fracture incidence are needed. Moreover, due to the ongoing change of demographic structure in industrialized countries towards aging populations, forecasting future trends that account for the expected demographic alterations are helpful in assessing how current measures that usually imply latency periods of many years until they take effect will affect future outcomes and, therefore, costs of disease burden as well as of prevention programs. As a result, certain population segments identified as future high-risk groups could be specifically targeted by today’s preventive measures.
The aims of the present study include determining hip fracture incidence rates in Vorarlberg 2003–2013, examining secular trends, and predicting future hip fracture cases in a population-based sample, representative of a Central European population living in rural and urban areas alike. Results are, therefore, expected to be valuable for future health policy decisions also beyond Vorarlberg and Austria.
Methods
Study design and data retrieval
In this population-based study within the framework of the VHM&PP, data were collected of 5842 patients with discharge diagnosis hip fracture between January 1st, 2003 and December 31st, 2013 from all hospitals in Vorarlberg (Landeskrankenhaus Bregenz, Landeskrankenhaus Bludenz, Krankenhaus Dornbirn, Landeskrankenhaus Feldkirch, Landeskrankenhaus Hohenems, and Sanatorium Schruns). Hip fracture was defined by the ICD-10 codes S32.4, S32.5 (acetabular fractures), as well as S72.0, S72.1, S72.2, S72.7 and S72.9 (femoral fractures). To obtain incidence rates 2003–2013, yearly cases were related to corresponding figures of the average annual resident population retrieved from the Statistical Database of Statistics Austria (http://www.statistik.at). Likewise, predicted average annual hip fracture incidence rates until 2050 were related to a main demographic scenario of medium fertility, life expectancy, and immigration, which is most likely to occur (Hanika 2015; http://www.statistik.at) and served as our base case. For comparability, the two other available demographic core scenarios, the “growth scenario” (high fertility, life expectancy, and immigration), and the “ageing scenario” (low fertility and immigration but high life expectancy) were accounted for, characterized by an aging population with different birth and immigration rates (Hanika 2015): Assumptions of fertility are based on a total fertility rate of 1.61 births per woman in 2014 that in 2060 is expected to amount to 1.62 anticipating medium fertility, to drop to 1.12 in 2030 and rise to 1.44 in 2060 assuming low, and to reach 2.12 in 2060 assuming high total fertility. Life expectancy at birth is projected to constantly rise until 2060 from 80.0 years among men and 85.1 years among women in 2014 to 88.0 and 91.3 years, respectively, in the medium variant, to 85.0 and 89.1 years, respectively, in the low variant, and to 90.4 and 93.0 years, respectively, in the high variant. Annual immigration in Vorarlberg is expected to exceed that of 2014 (6808 persons) in the coming years, at least until 2018 in the low immigration variant. Compared with 2014, immigration is predicted to change by +1.8 % in 2030 and −4.8 % in 2060 in the medium, by −12.1 % in 2030 and −21.3 % in 2060 in the low, and by +10.4 % in 2030 and +9.1 % in 2060 in the high variant. Numerical representations of the predicted demographic developments according to each of the scenarios are shown in Supplemental Table 1.
Statistical analysis
Age-standardized incidence rates per 100,000 person years (PY) are based on the exact European population (ESR, European Standard Rate) with a 95 % confidence interval (95 % CI) using the direct method in 5 years age categories. Based on crude incidence rates 2003–2013 and the population predictions of the Statistics Austria database, hip fracture cases were estimated up to 2050. Incidence time trends observed from annual rates 2003–2013 for both genders in different age groups (i.e., 0–49 years, 50–64 years, 65–79 years, and 80+ years) were approximated by an exponential graph that proved the best fit to the data relative to others like a linear one, and projections up to 2050 were conducted using a log-linear model (Stevens and Rudd 2013). Since peak incidences occurred between 2004 and 2006, incidence rates of year(s) preceding the year of peak incidence were excluded from the model, otherwise all available data points were accounted for. Predicted female and male annual cases of all age groups were added up for total numbers of forecast cases, around which 95 % prediction intervals (95 % PIs) were constructed. PIs, like confidence intervals, take account of slope and intercept variability of the regression line, but they characterize the range of single unknown observations rather than the distribution of sample means as confidence intervals do, thus more appropriately capturing the uncertainty inherent to forecasts. Estimates of predicted cases up to 2050, including corresponding 95 % PIs, based on hip fracture incidence 2003–2013, were obtained using the formula
in which PP denotes the predicted population of year Y, and int and a are the intercept and slope, respectively, of the exponential model; required for calculation of 95 % PI upper and lower bonds are furthermore t 0.05 which is the two-sided critical t statistic value for a probability of 95 %; n which is the number of data points 2003–2013 which are used in the model (between 8 and 11); \(\bar{y}\) which is the mean year date from 2003 to 2013 (“2008”, if all 11 data points are used); SS y which is the sum of squares of deviations from \(\bar{y}\); and SE which is the standard error of the ln of incidence 2003–2013.
Prerequisite for validity of these estimates was the assumption of a constant medical supply situation (i.e., prevention and access to health care) until 2050. For comparison of gender groups, Wilcoxon test was applied. All statistical analyses were performed using SAS 9.3 (SAS Institute, Cary, NC, USA), SPSS version 19 (SPSS Inc., Chicago, IL, USA), and Mathematica 5.2 (Wolfram Research, Champaign, IL, USA).
Results
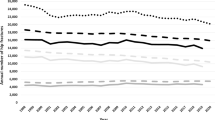
From 2003 through 2013, 5842 hip fractures (21.9 % fractures of the acetabulum and 78.1 % fractures of the femur) were identified in total, occurring in 1707 (29.2 %) men and in 4135 (70.8 %) women. Number of cases, target population, and incidence by gender for the years 2003–2013 are shown in Table 1 and Fig. 1.
Crude hip fracture incidence rates (a) and age-adjusted European standardized rates (ESR) of hip fractures (b) in all age groups and at ≥50 years for both genders combined and separately; error bars in b span the 95 % confidence intervals (Vorarlberg Health Monitoring & Prevention Program, Austria 2003–2013)
Crude male hip fracture incidence rates were significantly lower than female ones (p < 0.01) but without clear temporal trend, displaying fluctuation of the age-standardized incidence rates between 89.4 per 100,000 PY in 2013 and 143.6 per 100,000 PY in 2006 (Table 1; Fig. 1). Female hip fracture incidence adjusted to the ESR increased from 220.2 per 100,000 PY in 2004 to 225.8 per 100,000 PY in 2005. After that year, the trend was inverted and the age-standardized incidence decreased to 152.9 in 2013, corresponding to an average annual decrease of 4.7 % between 2005 and 2013. This was similarly reflected in the group of women ≥50 years with an average decrease of 4.5 % from 617.0 in 2005 to 426.0 in 2013. By age groups, the largest percentagewise drop in crude incidence rates 2003–2013 was observed for both women and men <50 years, from 14.6 to 5.9 per 100,000 PY and from 35.4 to 8.2 per 100,000 PY, respectively. Crude incidence for women at age groups 50–64 years, 65–79 years, and 80+ years ranged from 105.8 (in 2004) to 74.4 (in 2012), from 665.2 (in 2005) to 364.5 (in 2013), and from 3094.0 (in 2004) to 2052.6 (in 2013) per 100,000 PY, respectively. For men, crude incidence rates at age groups 50–64 years, 65–79 years, and 80+ years ranged from 129.4 (in 2004) to 52.5 (in 2012), from 350.3 (in 2005) to 235.3 (in 2013), and from 1379.5 (in 2006) to 745.3 (in 2004) per 100,000 PY, respectively (not shown).
Age-specific incidence rates by gender for 2013 appear in Supplemental Fig. 1. Hip fractures and age-specific incidence rates increased with age in both men and women, the highest age-specific incidence of 3107 per 100,000 PY in women aged 90+ years. For males and females combined at ≥50 years, the highest crude and age-adjusted incidence of hip fractures, respectively, 455.2 and 516.4 per 100,000 PY, was observed in 2004 (Table 1; Fig. 1).
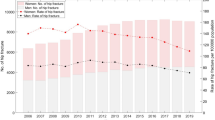
Based on age-specific incidence rates in 2013, we calculated expected hip fracture cases for the years 2015–2050 in the base case scenario (Table 2; Fig. 2). In this scenario, the overall number of hip fractures per year is predicted to increase by an average of 2.2 %, which is roughly the same for both women and men (Supplemental Table 2). In both the growth and aging scenarios, an average annual increase of approximately 2.4 % is expected, likewise equal for both genders (Supplemental Table 2).
Projections of annual hip fracture cases until 2050 assuming the main demographic scenario (see “Methods” and Supplemental Table 1) in all age groups for both genders (a), and for women (b) and men (c) separately. Dotted curves indicate annual cases predicted from incidences in 2013 irrespective of incidence trends 2003–2013. Solid lines represent predictions of future hip fracture cases considering incidence trends 2003–2013, and dashed lines represent the upper and lower limits of the 95 % prediction intervals (PIs) of these forecast cases (Vorarlberg Health Monitoring & Prevention Program, Austria 2003–2013)
Considering incidence trends 2003–2013, overall annual cases are likely to moderately decrease from 516 (95 % PI 361–738) in 2015 to 463 (95 % PI 149–1692) in 2050 in the base case scenario (Table 2; Fig. 2), corresponding to a drop of 0.32 % each year (Supplemental Table 2). However, gender-wise projections differ distinctly. Whereas male annual hip fracture cases are predicted to marginally rise from 153 (95 % PI 77–274) in 2015 to 175 (95 % PI 13–890) in 2045 and drop thereafter, female cases are projected to clearly decline from 363 (95 % PI 284–464) in 2015 to 295 (95 % PI 140–632) in 2050 (Table 2; Fig. 2), corresponding to a decrease of 0.61 % each year (Supplemental Table 2). By comparison, in the growth and aging scenario, overall cases are expected to slightly increase from 510 (95 % PI 356–730) and 509 (95 % PI 355–729), respectively, in 2015 to 524 (95 % PI 249–1052) and 521 (95 % PI 248–1045), respectively, in 2030, and then drop to 492 (95 % PI 156–1818) and 487 (95 % PI 155–1793), respectively, in 2050 (not shown). Gender-wise, male cases are predicted to increase from 153 in both the growth and aging scenarios (95 % PIs 76–273 and 76–272, respectively), to 187 (95 % PI 13–956) and 186 (95 % PI 13–945), respectively, in 2045, and drop until 2050 (not shown). Constantly decreasing female cases are expected in both scenarios, from 357 (95 % PI 279–457) and 356 (95 % PI 279–457) in 2015 following the growth and the aging scenario, respectively, to 308 (95 % PI 146–664) and 306 (95 % PI 145–656), respectively, in 2050 (not shown), which corresponds to an annual decrease of 0.43 and 0.45 %, respectively (Supplemental Table 2).
Supplemental Table 2 lists predicted changes in hip fracture cases 2015–2050 in Vorarlberg in different age groups for each core demographic development and assumption of future incidence. Cases among male and female patients <50 years are predicted to remain constant ignoring the incidence trend 2003–2013, or follow a considerable decline if the incidence trend of the past years is considered. At more advanced age, unsurprisingly, the largest percentagewise increase in hip fractures will be seen at ≥80 years in all scenarios if the incidence trend 2003–2013 is not factored in. If so, however, decreasing numbers of cases are expected up to 79 years for women and up to 64 years for men, and the highest increases are predicted among males over 80 years at an annual rate of 1.81 %.
Discussion
Our study provides current population-based data on hip fractures in the period of 2003–2013 in the westernmost Austrian province Vorarlberg and predicts hip fracture cases till 2050. Contrasting with previous publications on hip fracture incidence in the Austrian population aged ≥50 years that analyzed annual data of 1994–2006 and 1995–2004 (Mann et al. 2008, 2010), we observed lower age-standardized incidence rates among both genders. Our figures are, however, more consistent with an investigation by Dimai et al. (2011), also with respect to the notion of an annual decrease in particularly female hip fracture incidence in Austria from 2005 until the final year of that study. A plausible explanation for these divergent findings could be the lack of exclusion of multiple registrations due to re-admissions for the same fracture in the studies by Mann et al. (2008, 2010), whereas Dimai et al. (2011) applied a correction factor, and for the present investigation anonymized information on the patient level was available. In an international context, incidence rates herein are moderate to low according to the categorization used in a previous meta-analysis that compared age-standardized hip fracture incidence rates among studies in general populations worldwide (Kanis et al. 2012) (data therein are, however, reported as standardized to the world population and not to the ESR). We tentatively explain this finding by effective regional prevention programs: Since the early 1990s, in Vorarlberg broad public awareness has been created by area-wide activities for fall prevention in the context of “Safe Communities”, and osteoporosis gymnastics, advanced screening and treatment of osteoporosis (women 50 PLUS) were offered (Concin et al. 2002).
It is these measures and prevention programs that may have contributed likewise to the decline of hip fractures by the mid of the last decade, particularly among women. This trend has previously been observed in Austria from 2006 to 2008 in a study based on the national hospital discharge register for the population ≥50 years (Dimai et al. 2011), and declining hip fracture incidence during previous years has been reported from other countries as well: Using register-based hospital data from Oslo/Norway, the age-standardized hip fracture incidence rate for women but not men ≥50 years was significantly decreased in 2007 as compared to incidence rates from the 1970s, 1980s, and 1990s (Støen et al. 2012). Also in Belgium 2000–2007, using the national hospital database, age-adjusted annual incidence rates were found to have significantly declined for women but not for men ≥50 years (Hiligsmann et al. 2012). A decrease in age-adjusted rates for both genders was reported for the Norwegian population ≥50 years 1999–2008 using a nationwide hip fracture database (Omsland et al. 2012), from the Canadian province of Québec among people ≥50 years 1993–2004 based on the local hospital discharge register (Vanasse et al. 2012), and from The Netherlands for the population ≥65 years 1994–2008 using the national hospital discharge registry (Hartholt et al. 2011); moreover, using data from the Swiss national statistics database, age-standardized hospitalizations due to hip fractures significantly decreased for both genders ≥45 years 2000–2008 (Lippuner et al. 2012). Furthermore, in France 2002–2008, based on the national hospital database, a decreasing incidence trend was described for both genders ≥75 years, yet over 40 years, women displayed declining, and men increasing incidence trends (Maravic et al. 2011). Similarly in Spain, with fracture data obtained from a governmental database, annual age-adjusted incidence rates 2007–2010 rose for male but declined for female hip fractures since the period of 1997–2000 for the population ≥65 years (Azagra et al. 2014). By contrast, while crude incidence rates in Germany increased 1995–2010 using data from the national hospital discharge register, no significant trend was observed upon adjustment for age and sex; however, for males ≥40 years, incidence rates increased whereas those for women over 60 years decreased in areas of former Western Germany only (Icks et al. 2013). In fact, mixed results were also reported in a previous review on secular trends of hip fracture incidence (Cooper et al. 2011). Such variation can be explained by differences in the investigated age groups, observation periods, outcome measures (crude, age- and/or sex-adjusted incidence), and data resources.
Gender-specific differences in hip fracture incidence may be reflective of a faster decrease among women than among men (Cawthon 2011; Lippuner et al. 2012). In our study, we observed a decline in female hip fracture incidence, but, despite a local maximum 2005 and 2006, no clear further trend for men, whereas elsewhere an increase among older men ≥80 years was stated (Hartholt et al. 2011). Since osteoporosis is more prevalent in women, many prevention programs have targeted mainly those, while male osteoporosis is likely to be underdiagnosed and accordingly undertreated (Geusens et al. 2009). Consistent with more previous data from Austria (Dimai et al. 2011), we observed a reversal of the trend in female hip fracture incidence, suggesting that prevention programs are effective. There is no clear impact on male hip fracture incidence, indicating that measures for male osteoporosis prevention should be intensified.
Assuming a constant standard in prevention and care of hip fractures in Vorarlberg till 2050, forecasts up to 2050 show an increase in both male and female hip fractures if incidence trends 2003–2013 are not accounted for. If these trends are accounted for, we predict slightly rising male but decreasing female cases, however, precaution is due because of the wide 95 % prediction intervals for male cases. As observed elsewhere, demographic changes towards an augmented proportion of older age groups substantially contribute to increasing numbers of hip fractures (e.g., Hartholt et al. 2011). If, however, the trend of decreasing female incidence continues in the coming years, it will antagonize the predicted increment in the number of cases. Brown et al. (2012) accounted for past decreasing trends in hip fracture incidence in the United States among individuals ≥45 years between 1990 and 2006; using data from the National Hospital Discharge Survey on hip fractures, they found that conservative estimates may result in levelling-off of all cases and even a reduction of male cases 2010–2050. With data from the same database likewise 1990–2006 for people ≥65 years, considering past incidence trends, a rise of 11.9 % of total hip fractures from 2010 until 2030 was anticipated (Stevens and Rudd 2013); gender-wise, however, a small reduction of 3.5 % was predicted for female cases counteracted by an almost 52 % increase of male cases. Similar conclusions can be drawn from our results herein that cases will increase until 2050 if incidence trends before 2013 are not factored in. If they are considered based on gender- and age-specific incidence rates, our scenario for male cases 2015–2050 is similar to that described by Brown et al. (2012) resulting in a slight rise to a constant level followed by a reduction. Our prognosis for female hip fractures matches the finding of Stevens and Rudd (2013) that cases are on a moderate decrease.
Lifestyle changes such as weight gain, enhanced physical activity or improved prevention (anti-osteoporotic drugs, hip protectors) may have contributed to differential fracture risks across populations. Possible reasons for the decrease in (female) hip fracture incidence observed in our study could include improvements in general health that are mostly unrelated to prevention programs, such as changes in risk factors (smoking, alcohol consumption, low physical activity) over time, effects on bone health in birth cohorts, and changes in population structure. But also preventive measures could play a significant role encompassing effects of augmented bisphosphonate administration, which entails benefits particularly for postmenopausal women (Gallacher and Dixon 2010). This conjecture is supported by studies demonstrating that a marked increase in bisphosphonate prescriptions during the 2000s coincided with reduction of primarily female hip fracture incidence (Alves et al. 2013; Fisher et al. 2009; Hiligsmann et al. 2012). Further observation of our study population can clarify the impact of prevention programs, including administration of bisphosphonates and fall prevention strategies, on future hip fracture incidence. Increase of longevity has an eminent influence on the future number of cases, since hip fractures occur predominantly at more advanced age, which is evident in the group of those over 50 years. Furthermore, today’s preventive measures can have an effect until 2030 if one assumes a latency period of 10 years. Prognosis for subsequent years is, therefore, speculative, also because possible behavioral changes in the population cannot be known today. Further observations of incidence trends are required to verify the predictions and possibly to adjust for expected future risk factor constellations such as obesity and physical activity.
Our study might harbor several limitations: Assuming validity and reliability of the reported hip fracture numbers and population projections, possible future changes in osteoporosis prevalence as a result of improvements in prevention or treatment are unknown to date and could, therefore, not be accommodated by our model. It should, furthermore, be borne in mind that misclassification of the diagnosis of hip fracture is theoretically possible, though it is usually clearly diagnosed. Moreover, our estimates are based on the discharge diagnoses of regional hospitals and, therefore, reflect the health care situation in Vorarlberg. However, since hip fractures are treated almost exclusively on a stationary basis, completeness of the data can be assumed (Wildner and Clark 2001). Major strengths of our investigation include the availability of data on hip fractures covering a period of 11 years on individual level, whereas most previous analyses on osteoporosis and hip fractures in Austria rely on aggregated data from the national hospital diagnosis discharge register (Icks et al. 2008; Mann et al. 2008, 2010). Beyond that, owing to the geographic situation but also political factors (extensive mountain ranges and non-EU countries constitute the borders), exhaustive capture of hip fracture cases in the target population is likely, since treatment of local hip fractures in adjacent regions is practically very limited.
Conclusions
Our results indicate that in Vorarlberg past preventive programs against osteoporosis-related (hip) fractures have been effective after all in the female population and should be continued focusing on women ≥80 years in particular, but more efforts are required regarding the male population, especially ≥65 years. In aging societies, such programs will be the more successful the more efficiently they reach the fastest growing elderly age groups.
References
Alves SM, Economou T, Oliveira C, Ribeiro AI, Neves N, Gómez-Barrena E et al (2013) Osteoporotic hip fractures: bisphosphonates sales and observed turning point in trend. A population-based restrospective study. Bone 53:430–436
Azagra R, López-Expósito F, Martin-Sánchez JC, Aguyé A, Moreno N, Cooper C et al (2014) Changing trends in the epidemiology of hip fracture in Spain. Osteoporos Int 25:1267–1274
Becker DJ, Kilgore ML, Morrisey MA (2010) The societal burden of osteoporosis. Curr Rheumatol Rep 12:186–191
Brown CA, Starr AZ, Nunley JA (2012) Analysis of past secular trends of hip fractures and predicted number in the future 2010–2050. J Orthop Trauma 26:117–122
Cawthon PM (2011) Gender differences in osteoporosis and fractures. Clin Orthop Relat Res 469:1900–1905
Cheng SY, Levy AR, Lefaivre KA, Guy P, Kuramoto L, Sobolev B (2011) Geographic trends in incidence of hip fractures: a comprehensive literature review. Osteoporos Int 22:2575–2586
Concin H, Ulmer H, Hefler L (2002) Mental well-being in 5000 women participating in the ‘Women-Plus’ preventive medicine program. Maturitas 41:S9–S12
Concin H, Nagel G, Ulmer H (eds.) (2013) Modern Prevention Research in Vorarlberg. 50 Years of Preventive Medicine and Research in the Agency for Preventive and Social Medicine. aks Gesundheit GmbH, Bregenz
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM et al (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22:1277–1288
Dimai HP, Svedbom A, Fahrleitner-Pammer A, Pieber T, Resch H, Zwettler E et al (2011) Epidemiology of hip fractures in Austria: evidence for a change in the secular trend. Osteoporos Int 22:685–692
Dimai HP, Redlich K, Peretz M, Borgström F, Siebert U, Mahlich J (2012) Economic burden of osteoporotic fractures in Austria. Health Econ Rev 2:12
Dorner T, Weichselbaum E, Lawrence K, Stein KV, Rieder A (2009) Austrian osteoporosis report: epidemiology, lifestyle factors, public health strategies. Wien Med Wochenschr 159:221–229
El-Khoury F, Cassou B, Charles MA, Dargent-Molina P (2013) The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ 347:f6234
Fisher AA, O´Brien ED, Davis MW (2009) Trends in hip fracture epidemiology in Australia: possible impact of bisphosphonates and hormone replacement therapy. Bone 45:246–253
Gallacher SJ, Dixon T (2010) Impact of treatments for postmenopausal osteoporosis (bisphosphonates, parathyroid hormone, strontium ranelate, and denosumab) on bone quality: a systematic review. Calcif Tissue Int 87:469–484
Geusens P, Sambrook P, Lems W (2009) Fracture prevention in men. Nat Rev Rheumatol 5:497–504
Grossman JM (2011) Osteoporosis prevention. Curr Opin Rheumatol 23:203–210
Hanika A (2015) Zukünftige Bevölkerungsentwicklung Österreichs und der Bundesländer 2015 bis 2060 (2075). Statistische Nachrichten 70:917–935
Hartholt KA, Oudshoorn C, Zielinski SM, Burgers PTPW, Panneman MJM, Van Beeck EF et al (2011) The epidemic of hip fractures: are we on the right track? PLoS One 6:e22227
Hernlund E, Svedbom A, Iversgård M, Compston J, Cooper C, Stenmark J et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. Arch Osteoporos 8:136
Hiligsmann M, Bruyère O, Roberfroid D, Dubois C, Parmentier Y, Carton J et al (2012) Trends in hip fracture incidence and in the prescription of antiosteoporosis medications during the same time period in Belgium (2000–2007). Arthritis Care Res 64:744–750
Holick MF (2011) Vitamin D: a d-lightful solution for health. J Investig Med 59:872–880
Icks A, Haastert B, Wildner M, Becker C, Meyer G (2008) Trend of hip fracture incidence in Germany 1995–2004: a population-based study. Osteoporos Int 19:1139–1145
Icks A, Arend W, Becker C, Rapp K, Jungbluth P, Haastert B (2013) Incidence of hip fractures in Germany, 1995–2010. Arch Osteoporos 8:140
James KA, Meliker JR (2013) Environmental cadmium exposure and osteoporosis: a review. Int J Public Health 58:737–745
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Lippuner K, Grifone S, Schwenkglenks M, Schwab P, Popp AW, Senn C et al (2012) Comparative trends in hospitalizations for osteoporotic fractures and other frequent diseases between 2000 and 2008. Osteoporos Int 23:829–839
Mann E, Icks A, Haastert B, Meyer G (2008) Hip fracture incidence in the elderly in Austria: an epidemiological study covering the years 1994 to 2006. BMC Geriatr 8:35
Mann E, Meyer G, Haastert B, Icks A (2010) Comparison of hip fracture incidence and trends between Germany and Austria 1995–2004: an epidemiological study. BMC Public Health 10:46
Maravic M, Taupin P, Landais P, Roux C (2011) Change in hip fracture incidence over the last 6 years in France. Osteoporos Int 22:797–801
Omsland TK, Holvik K, Meyr HE, Center JR, Emaus N, Tell GS et al (2012) Hip fractures in Norway 1999–2008: time trends in total incidence and second hip fracture rates. A NOREPOS study. Eur J Epidemiol 27:807–814
Peterlik M, Boonen S, Cross HS, Lamberg-Allardt C (2009) Vitamin D and calcium insufficiency-related chronic diseases: an emerging world-wide public health problem. Int J Environ Res Public Health 6:2585–2607
Sambrook P, Cooper C (2006) Osteoporosis. Lancet 367:2010–2018
Statistik Austria (2015). http://www.statistik.at. Accessed 16 Nov 2015
Stevens JA, Rudd RA (2013) The impact of decreasing US hip fracture rates on future hip fracture estimates. Osteoporos Int 24:2725–2728
Støen RO, Nordsletten L, Meyer HE, Frihagen JF, Falch JA, Lofthus CM (2012) Hip fracture incidence is decreasing in the high incidence area of Oslo, Norway. Osteoporos Int 23:2527–2534
Vanasse A, Orzanco MG, Dagenais P, Ouarda T, Courteau J, Asghari S et al (2012) Secular trends of hip fractures in Québec, Canada. Osteoporos Int 23:1665–1672
Wildner M, Clark DE (2001) Hip fracture incidence in east and west Germany: reassessment 10 years after unification. Osteoporos Int 12:136–139
Zhu K, Prince RL (2015) Lifestyle and osteoporosis. Curr Osteoporos Rep 13:52–59
Acknowledgments
We thank all physicians and participants in the Vorarlberg Health Monitoring and Prevention Program (VHM&PP) for completing the study examinations and providing data. The VHM&PP is supported by the State of Vorarlberg, Austria. We thank Markus Wallner, Christian Bernhard, and Gabriela Dür from the Vorarlberg State Government, and Hans-Peter Dimai for valuable advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors declare conflicts of interest.
Ethical standards
The study was performed according to the Declaration of Helsinki in compliance with Austrian law.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Concin, H., Brozek, W., Benedetto, KP. et al. Hip fracture incidence 2003–2013 and projected cases until 2050 in Austria: a population-based study. Int J Public Health 61, 1021–1030 (2016). https://doi.org/10.1007/s00038-016-0878-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-016-0878-9