Abstract
Osteoporosis constitutes a major public health problem through its association with age-related fractures, most notably those of the proximal femur. Substantial geographic variation has been noted in the incidence of hip fracture throughout the world, and estimates of recent incidence trends have varied widely. Studies in the published literature have reported an increase, plateau, and decrease in age-adjusted incidence rates for hip fracture among both men and women. Accurate characterisation of these temporal trends is important in predicting the health care burden attributable to hip fracture in future decades. We therefore conducted a review of studies worldwide, addressing secular trends in the incidence of hip and other fractures. Studies in western populations, whether in North America, Europe or Oceania, have generally reported increases in hip fracture incidence through the second half of the last century, but those continuing to follow trends over the last two decades have found that rates stabilise with age-adjusted decreases being observed in certain centres. In contrast, some studies suggest that the rate is rising in Asia. This synthesis of temporal trends in the published literature will provide an important resource for preventing fractures. Understanding the reasons for the recent declines in rates of hip fracture may help understand ways to reduce rates of hip fracture worldwide.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis constitutes a major public health problem through its association with age-related fractures, most notably those of the hip, vertebrae and distal forearm. However, prospective studies have shown a heightened risk of almost all types of fracture in individuals with low bone mineral density (BMD). In the year 2000, there were an estimated 9 million osteoporotic fractures worldwide, of which 1.6 million were at the hip, 1.7 million at the forearm and 1.4 million were clinical (symptomatic) vertebral fractures. The combined annual cost of all osteoporotic fractures has been estimated to be $20 billion in the USA and €30 billion in the European Union [1]. As life expectancy rises around the world along with the number of elderly individuals in every geographic region, the incidence of hip fractures is estimated to reach 6.3 million in 2050, assuming a constant age-specific rate of fracture in men and women [2]. However, substantial variation has been reported in hip fracture incidence rates around the world [1]. Age-adjusted rates seem to be highest in Scandinavia and in North American populations, with almost seven fold lower rates in southern European countries [3]. Hip fracture incidence is also lower in Asian and Latin American populations [4, 5] and rates seem to be lower in rural than in urban areas [6, 7].
In order to estimate the future global burden of hip and other age-related (or fragility) fractures in a more robust manner, it is important to analyse changes in fracture incidence rates adjusted for demographic changes in the world population. Projections of the future numerical burden of hip fracture are known to be highly sensitive to secular changes in age-adjusted incidence rates [8]. Temporal trends in the age- and sex-adjusted incidence of hip fracture around the world were initially explored by Melton et al. [9], over the period 1928–1980 (Fig. 1). Incidence rates appeared to be rising steeply in the USA, as well as in other European centres. These increases were confirmed in subsequent studies from the UK [10] and Scandinavia [11, 12]. The protracted follow-up period available in Rochester, MN, however, also suggested the intriguing possibility that age-adjusted incidence rates might have begun to plateau in women from around 1955 onwards [9]. These findings suggest an important role for environmental factors in the aetiology of hip fracture. However, the extent to which the risk factors studied to date (including smoking, alcohol consumption, physical activity levels, obesity and migration status), as well as the changing rates of risk assessment and treatment contribute to these temporal trends remains uncertain.
Secular trends in the incidence of hip fracture: 1928–1982. Adapted from [9]
This review will update the secular trends for hip fracture in Europe, North America, Oceania and Asia. The limited data on long-term incidence trends for vertebral, distal forearm and other fractures will also be covered. The review was conducted using the PubMed database and MeSH terms/keywords that were employed included “fracture”, “incidence”, “osteoporosis”, “secular” or “trends”. Two co-authors (ZAC and CRH) conducted separate searches to ensure comprehensive identification of studies. All abstracts were reviewed to identify manuscripts of interest. Articles were chosen if they: (1) included incidence rates of fracture at any site over a defined time period; (2) reported directly estimated age-adjusted incidence rates from defined, broadly representative population samples; (3) used statistical tests to evaluate temporal trends; and (4) were published in the English language literature. The reference lists of these articles were examined for any other potentially relevant articles. Quality criteria included prospective ascertainment of fracture, appropriate definition of fracture site (ICD or other validated recording system) and determination of incidence over at least a 1-year period. Studies were considered eligible for review regardless of year of publication. In all, 51 articles were included and reviewed to ascertain the secular changes in osteoporotic fracture by country (Table 1). The majority of studies provided information on changes in hip fracture rates for men and women, but the data for secular trend in each gender were inconsistently supplied. Where available, trends in men generally resembled those in women. We therefore provide information in the table for both genders combined (age-standardised where possible). In those instances where data were only available for women, these are included in the table.
Secular trends in hip fracture
North America
The earliest study to examine hip fracture incidence trends was based in Rochester, MN [9, 13]. This investigation examined all fractures of the proximal femur occurring among residents over the 65-year period, 1928–1992 (Fig. 1). Incidence rates increased exponentially with age in both men and women. Annual age-adjusted incidence among women rose rapidly until 1955 only to fall slowly thereafter. Age-adjusted rates in men rose more steadily before beginning a downturn after 1980. The magnitude of the decline in incidence rates when both genders were analysed together was substantial: 9% between 1973 and 1992, with an incidence of 612.7 per 100,000 person-years at the end of the period. There was also a 13.7-year increase in the age at first hip fracture over the study period. In the most recent analysis of the Rochester data, a follow-up extended between 1980 and 2006 [14], the overall incidence of hip fractures declined by a further 1.42% per year in women and 0.44% per year in men (Fig. 2). The incidence of first hip fracture declined in women by 1.37% per year but remained unchanged in men. Among those with a previous history of hip fracture, the cumulative incidence of recurrence after 10 years was 11% in women and 10% in men. Accounting for the reduction in first hip fracture rates over time, hip fracture recurrence also appeared to decline after 1997.
Age-adjusted incidence rates for hip fracture in Rochester, MN, USA: 1928–2006. Adapted from [14]
A second study from the USA used the National Hospital Discharge Survey (which covers 0.6% of all patient discharges) to analyse secular trends in hip fracture incidence among the white population from 1970 to 1983 [15]. An overall increase of 9.3% in age- and sex-adjusted hip fracture incidence rates was observed over the 14-year period. Another study using the same database addressed age-specific rates between 1965 and 1993 [16]. Incidence increased linearly for men in the age groups 80–84 years and 85 years and older but for women and young men, rates did not change significantly over the time period. There was an overall improvement in hospital survival rates among men aged over 85 years and women over 75 years.
The Framingham study, a population-based cohort study from 1948 to 1996, also confirmed the progressively rising incidence rates in hip fracture during the second half of the last century [17]. In addition, this carefully assembled study suggested a birth cohort effect on hip fracture risk, with rates 20% and 40% higher among women born from 1901 to 1910 and from 1911 to 1921, respectively, compared with those born in the decade prior to this (Fig. 3). These findings are consistent with birth cohort effects on hip fracture incidence noted in the UK [10] and Finland [18]. They point to aetiological factors which might act early in the lifecourse that reflects themselves in rising fracture rates in successive later generations (see below).
Age-specific incidence rates of hip fracture (per 100,000 person-years) in men and women by birth cohort. Adapted from [17]
These data have been augmented recently by two large studies. In the first study [19], temporal trends in hip fracture incidence were examined over 20 years in the US Medicare database. A 20% sample of patients aged 65 years and older registered in this resource over the period 1986–2005 identified 786,717 hip fractures. The age-adjusted incidence in women increased by 9% from 1986 to 1995, with a remarkable subsequent decline of 24.5% between 1996 and 2005. A similar pattern was observed among men, with a 16.4% rise over the initial decade studied, followed by a 19.2% decline in the second 10-year period. The decline appeared to be collinear with an increasing use of bisphosphonates among the enrolled patients studied, and estimates of the impact of pharmacotherapy on fracture incidence rates was calculated to be as high as 40%. This estimate is substantially higher than that obtained from incidence trends in Canada.
The second study [20] utilised nationwide hospitalisation data for Canada over the period 1985–2005. In this analysis, age-specific hip fracture rates decreased continuously over the entire study period, with an inflexion in the trend line such that the annualised decline in incidence from 1985 to 1996 was 1.2% (95% CI 1.0–1.3%), while that from 1996 to 2005 was substantial steeper (2.4%; 95% CI 2.1–2.6%; p < 0.001).
Studies have also addressed the variation in hip fracture rates among different ethnic groups within the US population as a whole. A Californian analysis explored incidence between 1983 and 2000 with particular emphasis on the Hispanic population, the fastest growing ethnic minority in the USA [21]. Hip fractures were identified using a hospital discharge database. Among non-Hispanic white men and women in California, the standardised annual hip fracture rate for those aged 55 years and over declined steadily over each of the past two decades (0.5% among men and 0.6% among women). No such change was observed among Black or Asian women. By contrast, annual fracture rates among the Hispanic population increased significantly (4.2% in men and 4.9% in women). Alternative explanations proposed by the authors included differences in the lifestyle (nutrition and physical activity) of different ethnic groups, as well as variations in the environments they experienced during growth and development. The rise in US Hispanic rates is paralleled by early observations from Mexico. Data from one of the largest health systems in the country were used to evaluate trends in incidence between 2000 and 2006. Age-adjusted rates increased by around 1% per year among both men and women [22].
Smaller regional studies undertaken in Canada have generally reported similar patterns of hip fracture incidence to those observed in the recent national study [20] and in the USA. The first of these, undertaken using a hospital discharge register in Ontario between 1981 and 1992, showed no significant change in age- and sex-adjusted rates over the period [23]. As with many studies in western populations, the absolute number of hip fractures increased over the observation period along with the growing elderly population, and predictions suggested a doubling of this number by 2010. A second Ontario study [24] reported that age-adjusted rates had remained stable through to 1996 with a subsequent decline of around 0.9% each year among women. The decline was less steep among men. Finally, a study from Quebec revealed unchanged age-adjusted hip fracture rates among men and women between 1981 and 1992 [25]. Cervical femur fractures predominated at younger ages among women, but above the age of 70 years, trochanteric hip fracture incidence increased and the pattern was reversed. Summarising the data for Canada as a whole, data are scarce over the second half of the twentieth century but there seems no reason to suppose that age-adjusted increases did not parallel those observed in the northern USA. Since 1981, age-adjusted rates achieved a plateau and subsequently began to fall, with a progressive acceleration in this decline since the turn of the millennium.
Europe
European data on hip fracture incidence are available for Scandinavia, central and southern Europe (Fig. 4). Table 1 provides information for both genders combined (age-standardised where possible). In those instances where data were only available for women, these are included in the figure.
Scandinavia
Scandinavia has the highest reported incidence of hip fracture worldwide. A plethora of studies have addressed secular tendencies in fracture incidence throughout this northern European region. One of the earliest studies from Uppsala, Sweden (1965–1980), found an increase in the age- and sex-adjusted hip fracture rate from 430 per 100,000 person-years in 1965 to 650 in 1980 [12]. The authors estimated an annual increase of 2.2% over the study period. The rise in fracture rates was most pronounced among men and women aged 85 years and older, for whom fractures were three times more common in 1980 than in 1965. Subsequent studies from Malmo, Sweden revealed similarly steep increases in hip fracture incidence from 1950 to 1985 among men and women [26]. Thus, the annual age-adjusted incidence of 150 per 100,000 men in 1950 had risen to 390 per 100,000 men in 1985. The incidence rates in women had risen from 300 to 830 per 100,000 over the same period. Increased incidence was observed for both trochanteric and cervical femur fractures. A more recent study from the same city [27] suggests a plateau in hip fracture incidence between 1992 and 1995, a finding which is in accordance with several observations made in North America.
Studies have also explored hip fracture incidence in Norway, Denmark and Finland. Using diagnostic registers maintained between 1979 and 1999, a similar plateau in the incidence of hip fracture has been observed in Oslo, Norway to that seen in Sweden [28].
In Vyborg County, Denmark [29], the age-adjusted incidence of hip fractures increased by around 18 per 100,000 per year among women and 8 per 100,000 per year among men between 1987 and 1997. The increase appeared to be more pronounced for trochanteric than for cervical fractures. This general pattern was also observed in Helsinki using the Finnish National Hospital discharge register [18, 30, 31]. Over the period, 1970–1997, age-adjusted hip fracture rates increased among both women and men. In marked contrast, age-adjusted rates fell between 1992 and 2004. The decline was around 2.4% per year among women and 0.9% per year among men. This decline has been verified in a recent study based on national Danish registration data [32].
To summarise the epidemiological data from Scandinavia as a whole, increases in hip fracture incidence were observed from 1950 to around 1990, even after allowance for demographic changes in the population. Over the last two decades, rates appear to have fallen with declining rates more apparent among women than among men.
Northern and Central Europe
The largest number of studies has been undertaken in the UK. The first of these utilised national hospital discharge statistics between 1968 and 1985 (Fig. 5) [33]. Age- and sex-specific rates increased steadily over the first decade of this period but reached a plateau between 1979 and 1985. A similar pattern was observed in the Oxford Record Linkage Study [10], which also explored underlying contributors to these incidence trends using age-period-cohort modelling. A clear birth cohort effect was observed with differences in rates apparent for births from 1883 to 1917. The data resembled analyses from the Framingham study, which also revealed progressive increases in fracture rate for birth cohorts between 1887 and 1921 [17]. The most recent study from the UK echoes findings in North America and Scandinavia, with stabilisation of age-standardised hip fracture incidence rates over the period 1989–1998 [34].
Trends in hospitalisation for hip fracture in England and Wales: 1968–1985. Adapted from [33]
In The Netherlands, the age-adjusted incidence of hip fracture increased in a linear manner between 1972 and 1987 [35], but a later study suggested a stabilisation of rates between 1993 and the turn of the century [36]. This stabilisation in hip fracture incidence was also observed in Geneva, Switzerland between 1991 and 2000 [37], where age-adjusted rates in women actually decreased by around 1.4% each year. In a similar manner, stabilisation in incidence rates for hip fracture has been observed between 1990 and 2000 in Austria [38], Germany [39] and Hungary [40]. In Austria and Germany, significant decreases in age-adjusted rates were reported between 2000 and 2005. Thus, although early studies from Central Europe reported an increase in the age-adjusted incidence of hip fracture among both men and women, more recent studies have reported a plateau and, most recently, a decline [41, 42].
Southern Europe
Southern European studies have been confined to Italy and Spain. In Italy [43], the incidence of hip fracture rose dramatically between 1980 and 1991 among men, but no such trend was observed among women. Overall incidence rates in this study from Siena [43] were substantially lower than those observed in Northern or Central European nations. In Cantabria, Spain [44], the number of hip fractures increased between 1988 and 2002, reflected in an increase in age-adjusted incidence rates among men and women, over the same period.
Oceania
Hip fracture incidence rates in New Zealand and Australia have followed similar patterns to those observed in North America and Europe. A nationwide study in New Zealand observed significant increases in age-adjusted rates between 1950 and 1987 [45], but a follow-up study using the New Zealand Health Information Service between 1988 and 1999 reported that the number of men and women aged 65 years and over with a hip fracture did not meet previous predictions [46]. Furthermore, age-specific hip fracture rates were found to have declined significantly among women over this later period.
Two Australian studies also appear to confirm the recent declines in hip fracture incidence. The Dubbo Osteoporosis Epidemiology Study [47] based in a suburban centre northwest of Sydney, reported significant reductions in fracture incidence between 1989 and 2000 (4% each year among women and 6% among men). A larger study evaluating hospital admissions for hip fracture in New South Wales, suggested stable age-adjusted rates between 1990 and 2000 [48].
Asia
Around 30% of the hip fractures occurring worldwide are thought to arise in Asian populations, most notably that of China. Studies of temporal trends are available for several Asian countries including China, Singapore and Japan. In contrast, trend data are not available for Russia or India.
In Hong Kong, China, the age-adjusted incidence of hip fracture using hospital discharge statistics from all public hospitals was compared in 1966 [49], 1985 [50] and 1991–1995 [51]. Steep increases in incidence were observed among men and women between 1966 and 1985 (1.7-fold among men and 2.5-fold among women). Rates stabilised between 1985 and 1995, by which time they had become very similar to those observed contemporaneously in the UK, after age and sex standardisation.
Hip fracture incidence was also estimated in all 76 hospitals of Beijing, China in 1988–1992 [52]. The age standardised incidence for hip fracture was markedly lower in Beijing than observed in Hong Kong in 1985 or in US Caucasians. The Beijing rates were among the lowest in the world at the time that they were reported but appear to be rising (around 33% between 1988 and 1992). It is likely that part of this apparent increase in incidence was due to changes in the completeness and accuracy of reporting cases from hospitals.
In Singapore, incidence rates estimated in 1991 to 1998 [53] suggested increases of around 1% each year when compared with rates derived in 1965. The incidence of hip fracture in Singapore is now among the highest in Asia and resembles to that observed in Hong Kong, China. During the earliest period covered by these studies, increases in hip fracture rates predominated among Chinese and Malay subsets of the population, while rates in Indians appeared to decrease. The studies in Singapore and Hong Kong both suggest that urbanisation with attendant changes in physical activity and nutrition are associated with the rapidly rising fracture trends during the period 1960–1980. However, the study from Beijing suggests that changes in the accuracy of case reporting might also have contributed to these apparent increases in age-specific incidence.
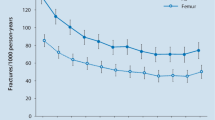
The third group of Asian studies have been undertaken in Japan. These include a detailed evaluation of the incidence of hip fracture in Tottori Prefecture between 1986 and 2001. Significant increases in the age-specific incidence rate of fracture were observed in both men and women over this period (Fig. 6) [54]. These increases appear to have continued to the most recent follow-up (2006), at which time age- and sex-specific rates were rising by around 3.8% per year [55].
Age- and gender-specific hip fracture incidence in Tottori Prefecture, Japan: 1986–2001. Adapted from [54]
In summary, Asian studies have pointed more clearly towards increasing age-adjusted incidence rates of hip fracture among men and women, but these are complicated by the potential for ascertainment bias. The most recent studies from Hong Kong and Singapore suggest that temporal trends may have reached a plateau but those from Japan suggest continuing age-adjusted increases. Further Asian studies are clearly needed to better characterise secular trends in hip fracture incidence for the region as a whole.
Secular trends in the incidence of other fragility fractures
Vertebral fracture
Population-based studies of vertebral fracture have been few and far between, due in part to the variable clinical presentation attributable to vertebral deformity, as well as to variation in opinion as to the extent of deformity which constitutes a significant vertebral fracture. The advent of morphometric and semi-quantitative visual techniques has enabled a number of studies to characterise both the prevalence and incidence of vertebral fracture. The prevalence tends to increase with age among men and women, although the gradient is steeper among women [56]. In contrast with hip fractures, the prevalence and incidence of vertebral deformities appear relatively homogeneous across different regions of the world. Although variation has been observed between centres in individual countries, the extent to which this represents sampling bias remains uncertain. Thus, the risk of vertebral fracture among postmenopausal women in Southeast Asia [57] is only 25% lower than that observed in the USA, despite a marked disparity in hip fracture rates between the two nations.
Studies addressing temporal trends in the incidence of vertebral fracture have only been undertaken in the USA and Sweden. The incidence of clinically ascertained vertebral fractures among residents of Rochester, MN was evaluated between 1950 and 1989 [58]. No overall increase in the incidence of vertebral fracture was observed over this 40-year period, although age-adjusted incidence rates increased by around 80% during the first 15 years of the follow-up period (Fig. 7). This apparent increase was principally attributable to an increasing rate of moderate trauma fractures among postmenopausal women. A second study [59] used an insurance claims database to estimate the changes in vertebral fracture incidence over the quinquennium 2000 to 2005. Rates were again stable over this period [60].
Secular change in the incidence of vertebral fracture in Rochester, MN. Adapted from [58]
Finally, age- and sex-specific incidence rates for radiologically diagnosed thoracic and lumbar vertebral compression fractures have been studied among men and women residents of Malmo, Sweden over the age of 60 years [61]. When the years 1950 to 1952 and 1982 to 1983 were contrasted, age- and sex-specific incidence rates were found to have increased significantly among both women and men, with the steepest rise observed among women aged 80 years and over.
Distal forearm fracture
Fractures of the distal forearm almost always arise following a fall from standing height onto an outstretched arm. Unlike vertebral and hip fractures, distal forearm fractures do not appear to have any discernible influence on survival. Among women, the incidence of distal forearm fracture tends to rise steeply during the perimenopausal period, and then rises more gently thereafter. Among men, incidence rates remain relatively constant between ages 20 and 80 years. A greater female to male ratio has been observed for fractures at this site than for hip and vertebral fracture (with most studies suggesting a female to male ratio of four to one).
Secular trends in the incidence of distal forearm fracture have been evaluated in North America, Australia, Scandinavia and The Netherlands. Unlike vertebral fracture, rates of distal forearm fracture due to low trauma appear relatively stable in most of these studies. In Rochester, MN [62], age-adjusted incidence rates increased gradually (0.5% per year) between 1945 and 1994. When men and women were evaluated separately, the age-adjusted incidence in women reached a peak in 1975, with declining rates thereafter. The pattern broadly resembles that observed for hip fracture over the same time span in the same population. A decline in age-adjusted wrist fracture incidence has also been observed in Canada [22] and Australia [63] where rates were found to be constant between 1992 and 1996, but declined between 1997 and 2000. European data on secular trends in forearm fracture are available for Sweden [64], The Netherlands [65] and Denmark [66]. In general, rates increased significantly until around 1980, but then fell back over the ensuing two decades.
Pelvis, rib and other fractures
Most epidemiological studies have focussed on fractures at the hip, vertebra and distal forearm. However, incidence trends are available for low trauma fractures of the pelvis [67], calcaneus [67], ribs [68], distal humerus [69], distal femur [70] and proximal tibia [70].
These data have all been gathered in the National Hospital Discharge registration system of Finland, and have all increased in age-adjusted incidence between 1970 and 1990. In most instances, rate increases have been greater among women than men, and age-adjusted rates have increased more steeply in older than in younger subjects. Confirmatory data for pelvic fracture have also been obtained from New South Wales, Australia [71], where the age-standardised hospitalisation rate for pelvic fracture increased from 59.3/100,000 person-years to 89.2/100,000 person-years between 1988 and 2000. In contrast, a US claims database [59] documented stable age-adjusted incidence rates for pelvic fracture over the 5 years between 2000 (8/100,000 person-years) and 2005 (12/100,000 person-years).
Mechanisms which might explain secular trends in fracture incidence
There are several potential contributors to the observed changes in age-adjusted incidence of osteoporotic fracture observed over a period of several decades. These include: (a) a change in the frequency of risk factors for fracture which act relatively late in the lifecourse; (b) a change in the frequency of risk factors influencing bone strength and propensity to trauma during early life, which feed through as altered fracture rates in successive birth cohorts; and (c) alterations in the demographic structure of the populations studied, within age and sex strata. All three of these mechanisms are likely to contribute, but most attention has been focussed on the changing prevalence of later life risk factors. Among such factors, changes in patterns of physical inactivity, vitamin D insufficiency and increasing survival of the frailest elderly are likely to contribute significantly to the age-adjusted increases in the rate of hip fracture observed during the second half of the last century. The reasons for a plateau or decrease in rates of hip fracture since the mid-1990s are not clear. The first bisphosphonate that effectively reduced the risk of hip fracture was approved for use in North America and Europe at around this time. However, the uptake and compliance with therapy has been quite limited and would not fully explain the temporal decreases in hip fracture that have been observed [20, 72]. In Geneva, Switzerland, the reversal of the hip fracture secular trend (observed in women only) was explained by a decrease in the incidence in institution-dwelling elderly women [73]. The increasing prevalence of obesity in the general population might also have blunted the age-specific increases in hip fracture incidence seen over the last two decades. Alterations in nutritional pattern and in tobacco consumption might also have contributed, but cigarette smoking in elderly women has always been very low and would have little impact on rates in the general population. Similarly, there is little evidence for changes in the prevalence of very heavy alcohol intake. The use of postmenopausal oestrogen has declined in North America and Europe, but this would tend to decrease, rather than increase, fracture risk. Finally, it is also important to exclude artefactual reasons for changes in rates of fracture, such as changes over time in the methods and accuracy of coding and reporting hip fractures to central databases and health registries. No single explanation appears to account for the different patterns seen among men and women, nor the timing of increasing rates among women in different regions.
The only direct evidence for a secular increase in the frequency of low BMD in the general population comes from comparison of skeletons obtained from a London church over the period 1729 to 1852, with BMD measurements made contemporaneously [74]. The rate of bone loss as judged by DXA in samples retrieved from the nineteenth century, both pre- and post-menopausal, was significantly greater than that observed in modern-day women. Thus, differences in rates of bone loss, as well as in peak bone mass, may contribute to the increasing incidence of hip fracture in the last half century [75].
The significant birth cohort effects observed in both Oxford and Framingham, suggest the need to consider influences during intrauterine and childhood development. One such example is that observed from the Dutch famine of 1944–1945 [76]. Exposure to famine during gestation resulted in increases in impaired glucose tolerance, obesity, coronary heart disease, atherogenic lipid profile, hypertension and affective disorders. To date, it is not known whether BMD values in the offspring of mothers who experienced a famine are reduced when compared with controls who did not. However, other examples (the Spanish Civil War and concentration camp survivors in Israel) suggest that profound insults of this type might reduce BMD values in the offspring. However, the incidence trajectories for hip fracture have been observed in several countries (Canada, Australia and the USA) that have experienced no major population-wide environmental stressors. Evidence is also accruing that less severe environmental factors during early life might influence the peak bone mass achieved and later risk of fracture. Studies on populations in the UK, USA and Scandinavia, have revealed that low birth weight and weight in infancy predict adult bone mass. Mother offspring cohorts have demonstrated that maternal vitamin D insufficiency during late pregnancy influences the bone mass of the offspring in later childhood [77–79].
Conclusions
This review reveals that there have been substantial temporal trends in the age-specific rates of hip fracture during recent decades. Although there are a few exceptions, age-specific incidence rates rose in western populations until around 1980 and have subsequently reached a plateau or decreased. The trends have been more pronounced in women than in men. There are fewer data from Asia and rates may still be rising in some regions. The temporal patterns for distal forearm fractures in northern Europe seem similar to those for hip fracture in that region. While rates of vertebral fracture may have increased in Sweden and the northern USA until the 1980s, there are no comparative studies of more recent temporal trends which have used standardised and population-based methods. Studies from Finland indicate that the rates of other types of fracture also increased from 1970 to 1990, but again, there are few data beyond that time. Age-period-cohort models suggest that all three of these influences operate on the temporal trend observed for hip fracture. Attempts to reduce the burden of fractures at this site should therefore be directed throughout the lifecourse. Data on continuing trends in hip fracture incidence, and on the changes in age- and sex-adjusted incidence rates of fractures at other sites, need to be collected prospectively and evaluated in a rigorous manner, as these trends will impact substantially on economic evaluations of the future burden of osteoporosis and its related fractures worldwide.
References
Cummings SR, Melton LJ III (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Cooper C, Campion G, Melton LJ III (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2:285–289
Johnell O, Gullberg B, Allander E, Kanis JA (1992) The apparent incidence of hip fracture in Europe: a study of national register sources. MEDOS study group. Osteoporos Int 2:298–302
Yan L, Zhou B, Prentice A, Wang X, Golden MH (1999) Epidemiological study of hip fracture in Shenyang, People’s Republic of China. Bone 24:151–155
Morales-Torres J, Gutierrez-Urena S (2004) The burden of osteoporosis in Latin America. Osteoporos Int 15:625–632
Kaastad TS, Meyer HE, Falch JA (1998) Incidence of hip fracture in Oslo, Norway: differences within the city. Bone 22:175–178
Sanders KM, Nicholson GC, Ugoni AM, Seeman E, Pasco JA, Kotowicz MA (2002) Fracture rates lower in rural than urban communities: the Geelong Osteoporosis Study. J Epidemiol Community Health 56:466–470
Gullberg B, Johnell O, Kanis J (1997) Worldwide projections for hip fracture. Osteoporos Int 7:407–413
Melton LJ III, O’Fallon WM, Riggs BL (1987) Secular trends in the incidence of hip fractures. Calcif Tissue Int 41:57–64
Evans JG, Seagroatt V, Goldacre MJ (1997) Secular trends in proximal femoral fracture, Oxford record linkage study area and England 1968–86. J Epidemiol Community Health 51:424–429
Frandsen PA, Kruse T (1983) Hip fractures in the county of Funen, Denmark. Implications of demographic aging and changes in incidence rates. Acta Orthop Scand 54:681–686
Zain Elabdien BS, Olerud S, Karlstrom G, Smedby B (1984) Rising incidence of hip fracture in Uppsala, 1965–1980. Acta Orthop Scand 55:284–289
Melton LJ III, Therneau TM, Larson DR (1998) Long-term trends in hip fracture prevalence: the influence of hip fracture incidence and survival. Osteoporos Int 8:68–74
Melton LJ III, Kearns AE, Atkinson EJ, Bolander ME, Achenbach SJ, Huddleston JM et al (2009) Secular trends in hip fracture incidence and recurrence. Osteoporos Int 20:687–694
Rodriguez JG, Sattin RW, Waxweiler RJ (1989) Incidence of hip fractures, United States, 1970–83. Am J Prev Med 5:175–181
Bacon WE (1996) Secular trends in hip fracture occurrence and survival: age and sex differences. J Aging Health 8:538–553
Samelson EJ, Zhang Y, Kiel DP, Hannan MT, Felson DT (2002) Effect of birth cohort on risk of hip fracture: age-specific incidence rates in the Framingham study. Am J Public Health 92:858–862
Kannus P, Niemi S, Parkkari J, Palvanen M, Vuori I, Jarvinen M (1999) Hip fractures in Finland between 1970 and 1997 and predictions for the future. Lancet 353:802–805
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB (2009) Incidence and mortality of hip fractures in the United States. JAMA 302:1573–1579
Leslie WD, O’Donnell S, Jean S, Lagace C, Walsh P, Bancej C, Morin S, Hanley DA, Papaioannou A, For the Osteoporosis Surveillance Expert Working Group (2009) Trends in hip fracture rates in Canada. JAMA 302:883–889
Zingmond DS, Melton LJ III, Silverman SL (2004) Increasing hip fracture incidence in California Hispanics, 1983 to 2000. Osteoporos Int 15:603–610
Johansson H, Clark P, Carlos F, Oden A, McCloskey EV, Kanis JA (2010) Increasing age and sex specific rates of hip fracture in Mexico: a survey of the Mexican Institute of Social Security. Osteoporos Int. doi:10.1007/s00198-010-1475-z
Jaglal SB, Sherry PG, Schatzker J (1996) The impact and consequences of hip fracture in Ontario. Can J Surg 39:105–111
Jaglal SB, Weller I, Mamdani M, Hawker G, Kreder H, Jaakkimainen L et al (2005) Population trends in BMD testing, treatment, and hip and wrist fracture rates: are the hip fracture projections wrong? J Bone Miner Res 20:898–905
Levy AR, Mayo NE, Grimard G (1995) Rates of transcervical and pertrochanteric hip fractures in the province of Quebec, Canada, 1981–1992. Am J Epidemiol 142:428–436
Sernbo I, Gullberg B, Johnell O (1993) Hip fracture in Malmo over three decades. Bone 14(Suppl 1):S19–S22
Rogmark C, Sernbo I, Johnell O, Nilsson JA (1999) Incidence of hip fractures in Malmo, Sweden, 1992–1995. A trend-break. Acta Orthop Scand 70:19–22
Lofthus CM, Osnes EK, Falch JA, Kaastad TS, Kristiansen IS, Nordsletten L et al (2001) Epidemiology of hip fractures in Oslo, Norway. Bone 29:413–418
Giversen IM (2006) Time trends of age-adjusted incidence rates of first hip fractures: a register-based study among older people in Viborg County, Denmark, 1987–1997. Osteoporos Int 17:552–564
Kannus P, Niemi S, Parkkari J, Palvanen M, Vuori I, Jarvinen M (2006) Nationwide decline in incidence of hip fracture. J Bone Miner Res 21:1836–1838
Lonnroos E, Kautiainen H, Karppi P, Huusko T, Hartikainen S, Kiviranta I et al (2006) Increased incidence of hip fractures. A population based-study in Finland. Bone 39:623–627
Abrahamsen B, Vestergard P (2010) Declining incidence of hip fractures and the extent of use of anti-osteoporotic therapy in Denmark 1997–2006. Osteoporos Int 21:373–380
Spector TD, Cooper C, Lewis AF (1990) Trends in admissions for hip fracture in England and Wales, 1968–85. BMJ 300:1173–1174
Balasegaram S, Majeed A, Fitz-Clarence H (2002) Trends in hospital admissions for fractures of the hip and femur in England, 1989–1990 to 1997–1998. J Public Health Med 23:11–17
Boereboom FT, de Groot RR, Raymakers JA, Duursma SA (1991) The incidence of hip fractures in The Netherlands. Neth J Med 38:51–58
Goettsch WG, de Jong RB, Kramarz P, Herings RM (2007) Developments of the incidence of osteoporosis in The Netherlands: a PHARMO study. Pharmacoepidemiol Drug Saf 16:166–172
Chevalley T, Guilley E, Herrmann FR, Hoffmeyer P, Rapin CH, Rizzoli R (2007) Incidence of hip fracture over a 10-year period (1991–2000): reversal of a secular trend. Bone 40:1284–1289
Mann E, Icks A, Haastert B, Meyer G (2008) Hip fracture incidence in the elderly in Austria: an epidemiological study covering the years 1994 to 2006. BMC Geriatr 8:35
Icks A, Haastert B, Wildner M, Becker C, Meyer G (2008) Trend of hip fracture incidence in Germany 1995–2004: a population-based study. Osteoporos Int 19:1139–1145
Pentek M, Horvath C, Boncz I, Falusi Z, Toth E, Sebestyen A et al (2008) Epidemiology of osteoporosis related fractures in Hungary from the nationwide health insurance database, 1999–2003. Osteoporos Int 19:243–249
Dimai HP, Svedbom A, Fahrleitner-Pammer A, Pieber T, Resch H, Zwetter E, Chandran M, Borgstrom F (2010) Epidemiology of hip fractures in Austria: evidence for a change in the secular trend. Osteoporos Int. doi:10.1007/s00198-010-1271-9
Maravic M, Taupin P, Landais P, Roux C (2010) Change in hip fracture incidence over the last 6 years in France. Osteoporos Int. doi:10.1007/s00198-010-1255-9
Agnusdei D, Camporeale A, Gerardi D, Rossi S, Bocchi L, Gennari C (1993) Trends in the incidence of hip fracture in Siena, Italy, from 1980 to 1991. Bone 14(Suppl 1):S31–S34
Hernandez JL, Olmos JM, Alonso MA, Gonzalez-Fernandez CR, Martinez J, Pajaron M et al (2006) Trend in hip fracture epidemiology over a 14-year period in a Spanish population. Osteoporos Int 17:464–470
Rockwood PR, Horne JG, Cryer C (1990) Hip fractures: a future epidemic? J Orthop Trauma 4:388–393
Fielden J, Purdie G, Horne G, Devane P (2001) Hip fracture incidence in New Zealand, revisited. N Z Med J 114:154–156
Chang KP, Center JR, Nguyen TV, Eisman JA (2004) Incidence of hip and other osteoporotic fractures in elderly men and women: Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res 19:532–536
Boufous S, Finch CF, Lord SR (2004) Incidence of hip fracture in New South Wales: are our efforts having an effect? Med J Aust 180:623–626
Chalmers J, Ho KC (1970) Geographical variations in senile osteoporosis. The association with physical activity. J Bone Joint Surg Br 52:667–675
Lau EM, Cooper C, Wickham C, Donnan S, Barker DJ (1990) Hip fracture in Hong Kong and Britain. Int J Epidemiol 19:1119–1121
Lau EM, Cooper C, Fung H, Lam D, Tsang KK (1999) Hip fracture in Hong Kong over the last decade—a comparison with the UK. J Public Health Med 21:249–250
Xu L, Lu A, Zhao X, Chen X, Cummings SR (1996) Very low rates of hip fracture in Beijing, People’s Republic of China the Beijing Osteoporosis Project. Am J Epidemiol 144:901–907
Koh LK, Saw SM, Lee JJ, Leong KH, Lee J (2001) Hip fracture incidence rates in Singapore 1991–1998. Osteoporos Int 12:311–318
Hagino H, Katagiri H, Okano T, Yamamoto K, Teshima R (2005) Increasing incidence of hip fracture in Tottori Prefecture, Japan: trend from 1986 to 2001. Osteoporos Int 16:1963–1968
Hagino H, Furukawa K, Fujiwara S, Okano T, Katagiri H, Yamamoto K et al (2009) Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos Int 20:543–548
O’Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ (1996) The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 11:1010–1018
Ling X, Cummings SR, Mingwei Q, Xihe Z, Xioashu C, Nevitt M et al (2000) Vertebral fractures in Beijing, China: the Beijing Osteoporosis Project. J Bone Miner Res 15:2019–2025
Cooper C, Atkinson EJ, Kotowicz M, O’Fallon WM, Melton LJ III (1992) Secular trends in the incidence of postmenopausal vertebral fractures. Calcif Tissue Int 51:100–104
Islam S, Liu Q, Chines A, Helzner E (2009) Trend in incidence of osteoporosis-related fractures among 40- to 69-year-old women: analysis of a large insurance claims database, 2000–2005. Menopause 16:77–83
Lad SP, Patil CG, Lad EM, Boakye M (2007) Trends in pathological vertebral fractures in the United States: 1993 to 2004. J Neurosurg Spine 7:305–310
Bengner U, Johnell O, Redlund-Johnell I (1988) Changes in incidence and prevalence of vertebral fractures during 30 years. Calcif Tissue Int 42:293–296
Melton LJ III, Amadio PC, Crowson CS, O’Fallon WM (1998) Long-term trends in the incidence of distal forearm fractures. Osteoporos Int 8:341–348
Boufous S, Finch C, Lord S, Close J, Gothelf T, Walsh W (2006) The epidemiology of hospitalised wrist fractures in older people, New South Wales, Australia. Bone 39:1144–1148
Jonsson B, Bengner U, Redlund-Johnell I, Johnell O (1999) Forearm fractures in Malmo, Sweden. Changes in the incidence occurring during the, 1950s, 1980s and 1990s. Acta Orthop Scand 70:129–132
Oskam J, Kingma J, Klasen HJ (1998) Fracture of the distal forearm: epidemiological developments in the period 1971–1995. Injury 29:353–355
Lauritzen JB, Schwarz P, Lund B, McNair P, Transbol I (1993) Changing incidence and residual lifetime risk of common osteoporosis-related fractures. Osteoporos Int 3:127–132
Kannus P, Niemi S, Palvanen M, Sievanen H, Parkkari J, Jarvinen M (2008) Rising incidence of low-trauma fractures of the calcaneus and foot among Finnish older adults. J Gerontol A Biol Sci Med Sci 63:642–645
Palvanen M, Kannus P, Niemi S, Parkkari J (2004) Hospital-treated minimal-trauma rib fractures in elderly Finns: long-term trends and projections for the future. Osteoporos Int 15:649–653
Palvanen M, Kannus P, Niemi S, Parkkari J (1998) Secular trends in the osteoporotic fractures of the distal humerus in elderly women. Eur J Epidemiol 14:159–164
Kannus P, Niemi S, Parkkari J, Sievanen H, Palvanen M (2009) Declining incidence of low-trauma knee fractures in elderly women: nationwide statistics in Finland between 1970 and 2006. Osteoporos Int 20:43–46
Boufous S, Finch C, Lord S, Close J (2005) The increasing burden of pelvic fractures in older people, New South Wales, Australia. Injury 36:1323–1329
Siris ES, Selby PL, Saag KG, Borgstrom F, Herings RM, Silverman SL (2009) Impact of osteoporosis treatment adherence on fracture rates in North America and Europe. Am J Med 122(Suppl 2):S3–S13
Guilley E, Chevalley T, Herrmann F, Baccino D, Hoffmeyer P, Rapin CH, Rizzoli R (2008) Reversal of the hip fracture secular trend is related to a decrease in the incidence in institution-dwelling elderly women. Osteoporos Int 19:1741–1747
Lees B, Molleson T, Arnett TR, Stevenson JC (1993) Differences in proximal femur bone density over two centuries. Lancet 341:673–675
Hui SL, Slemenda CW, Johnston CC Jr (1990) The contribution of bone loss to postmenopausal osteoporosis. Osteoporos Int 1:30–34
Kyle UG, Pichard C (2006) The Dutch Famine of 1944–1945: a pathophysiological model of long-term consequences of wasting disease. Curr Opin Clin Nutr Metab Care 9:388–394
Dennison E, Hindmarsh P, Fall C, Kellingray S, Barker D, Phillips D et al (1999) Profiles of endogenous circulating cortisol and bone mineral density in healthy elderly men. J Clin Endocrinol Metab 84:3058–3063
Javaid MK, Crozier SR, Harvey NC, Gale CR, Dennison EM, Boucher BJ et al (2006) Maternal vitamin D status during pregnancy and childhood bone mass at age 9 years: a longitudinal study. Lancet 367:36–43
Mahon P, Harvey N, Crozier S, Inskip H, Robinson S, Arden N et al (2009) Low maternal vitamin D status and fetal bone development: cohort study. J Bone Miner Res 25:14–19
Acknowledgements
This study was supported by the Medical Research Council, International Osteoporosis Foundation and NIHR Musculoskeletal Biomedical Research Unit, Oxford. The manuscript was prepared by Vivienne Cresdee and Gill Strange. It is endorsed by the Committee of Scientific Advisors of the IOF.
Conflicts of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The IOF CSA Working Group on Fracture Epidemiology: Adachi J., Borgström F., Dimai H.P., Clark P., Lau E., Lewiecki E.M., Lips P., Lorenc R., McCloskey E., Ortolani S., Papaioannou A., Silverman S., Wahl D.A., and Yoshimura N.
Rights and permissions
About this article
Cite this article
Cooper, C., Cole, Z.A., Holroyd, C.R. et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22, 1277–1288 (2011). https://doi.org/10.1007/s00198-011-1601-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1601-6